Although biological methods of treatment for mental illnesses were available before the Second World War, it was not until the 1950s that effective and safe psychoactive drugs became available. As a consequence of the introduction of chlorpromazine and reserpine, the number of mental hospital in-patients fell markedly, even though admission rates increased, because length of stay was substantially reduced and patients were increasingly managed as out-patients. However, the progress made since then – which continues today – should not be perceived solely in terms of the number of hospital patients and the economic benefits of out-patient treatment. The very real reduction in human suffering, of patients and their families, must never be forgotten. Furthermore, the ability to treat mental illness has removed some of the fear of it and the associated stigma (Reference Ghodse and KhanGhodse & Khan, 1988). Since then, there has been huge progress and an explosion in the drugs available to us. In much of the world, this has been accompanied by growing concern about what is perceived as their excessive use, although there are also parts of the world where suffering goes largely unrelieved.
Background
There are five principal symptoms for which psychoactive drugs are commonly prescribed – inability to cope, depression, anxiety, sleeplessness and pain – and they have a number of features in common: they are all symptoms that everyone has experienced at some time or other; the point at which they are regarded as sufficiently severe to warrant medical intervention and treatment is somewhat arbitrary and varies from one country to another; they are concomitants of other symptoms and may arise as a consequence of them (e.g. an individual patient may be anxious because of a lump and may be unable to sleep because of being in pain – so it is difficult to disentangle any one symptom from the much wider range of symptoms from which the patient is suffering concurrently); and they are all normal and reasonable responses to common situations and, even when they are severe, may still be reasonable responses to very difficult situations.
Although these symptoms are familiar and common occurrences, the scale of the associated suffering for the world as a whole still comes as something of a shock because it is so huge. For example, an estimated 450 million people alive today suffer from some form of mental or brain disorder, including alcohol and substance use disorders, with 121 million suffering from depression. Projections suggest that the proportion of the global burden of disease attributable to mental and brain disorders will rise to 15% by the year 2020. At a more homely level, these huge figures translate into the fact that one in four families has at least one family member who is affected by mental or brain disorder (World Health Organization, 2001a ; World Health Assembly, 2002).
The costs of mental disorders are correspondingly huge in terms of health care costs and loss of productivity at home and in the workplace. For example, just in the UK aggregate costs of mental illness have been estimated to be £32 billion, with reduced ability to work and associated productivity losses accounting for about 45% of this sum (World Health Assembly, 2002).
Fortunately, today there are effective medications and psychosocial interventions to treat mental disorders and pain. Although these are within the reach of all countries and are widely used, there is a global shortage of resources for mental health, which results in stark disparities in the provision of care.
These disparities are illustrated by a World Health Organization study of mental health resources (ATLAS; Abuse Trends Linkage Alerting System), which collected information from 185 countries (World Health Organization, 2001b ). It found that:
-
(a) 41% do not have a mental health policy;
-
(b) 25% do not have mental health legislation;
-
(c) 25% do not have basic psychotropic drugs in primary care settings;
-
(d) 40% do not have treatment facilities for severe mental disorders at primary care level;
-
(e) about half of the countries in the world have fewer than one psychiatrist and one psychiatric nurse per 100 000 population.
There is thus a huge gap between the burden of mental disorders in the world and the available resources, with 28% of countries lacking a specific budget for mental health and, of those countries that do report mental health expenditure, 36% spend less than 1% of their total health budget in this field. Indeed, figures for global consumption of licit drugs show that the bulk of medicine continues to be consumed in a handful of countries, and the proportion is even higher for narcotic drugs and psychotropic substances. In other words, economically weak countries and the poorer segments of society continue to have little or no access to medicines and medical care and even less access to health care for mental disorders.
INTERNATIONAL DISPARITIES IN THE USE OF ANALGESICS
The treatment of pain – severe pain such as that occurring in the course of cancer – illustrates these international disparities. It is estimated that by 2020 there will be 20 million new cancer cases each year, of which approximately 70% will occur in developing countries (World Health Organization, 2000). Seventy to eighty per cent of cancer patients suffer severe pain in the later stages of disease (World Health Organization, 1996) and there is a broad consensus that, for the treatment of such pain, opioids (specifically morphine) are indispensable because of their affordability and analgesic efficacy. Research conducted in several countries has shown that opioid treatment can be effective in 75–90% of patients with cancer-related pain, and of course opioids are also used to relieve acute or chronic pain not related to cancer (World Health Organization, 1986). Indeed, long-term, persistent and debilitating pain is a major public health problem, accounting for untold suffering and lost productivity (Reference Gureje, von Korff and SimonGureje et al, 1998; World Health Organization, 2001a ).
As one of the oldest drugs known to man, and with credentials as an analgesic stretching over hundreds of years, one might expect morphine and similar drugs to be used universally for the treatment of pain. In one sense it is widely used and, in addition to morphine, a variety of semi-synthetic and synthetic opioids have been developed in an attempt to improve on the well-established therapeutic qualities of morphine by separating its desirable properties – analgesic, cough suppressant, anti-diarrhoeal – from its undesirable, addictive properties.
Unfortunately that goal has not been achieved and several opioids, initially welcomed as safer alternatives to older drugs, have failed to live up to early expectations. Morphine and codeine, however, have remained as essential therapeutic tools with a range of applications. Both have been on the World Health Organization's Model List of Essential Drugs since its inception in 1977 and morphine is among the drugs proposed by the World Health Organization for the New Emergency Health Kit (World Health Organization, 1998).
In this context, Fig. 1 presents an uncomfortable, if not shocking, picture: North America, with 7% of the world's population, consumes 47% of the total world's supply of morphine, and Europe, with 12% of the world's population, uses a further 37%. Africa, on the other hand, which has 13% of the world's population, uses only 1% of the world's licit supply of morphine. The same situation pertains in relation to the collective use of the main narcotic drugs, with the USA by far the largest consumer (Fig. 2). There are similar disparities within Europe, with the wealthy countries of Western Europe consuming far higher quantities of opioid analgesics than their neighbours in Eastern Europe. Interestingly, it is the Nordic countries, with only 3% of the European population, whose level of consumption seems particularly high. From such statistics it can be demonstrated that the ten largest opioid-consuming countries in the world account for as much as 80% of morphine consumption (International Narcotics Control Board, 2000, 2002a ).
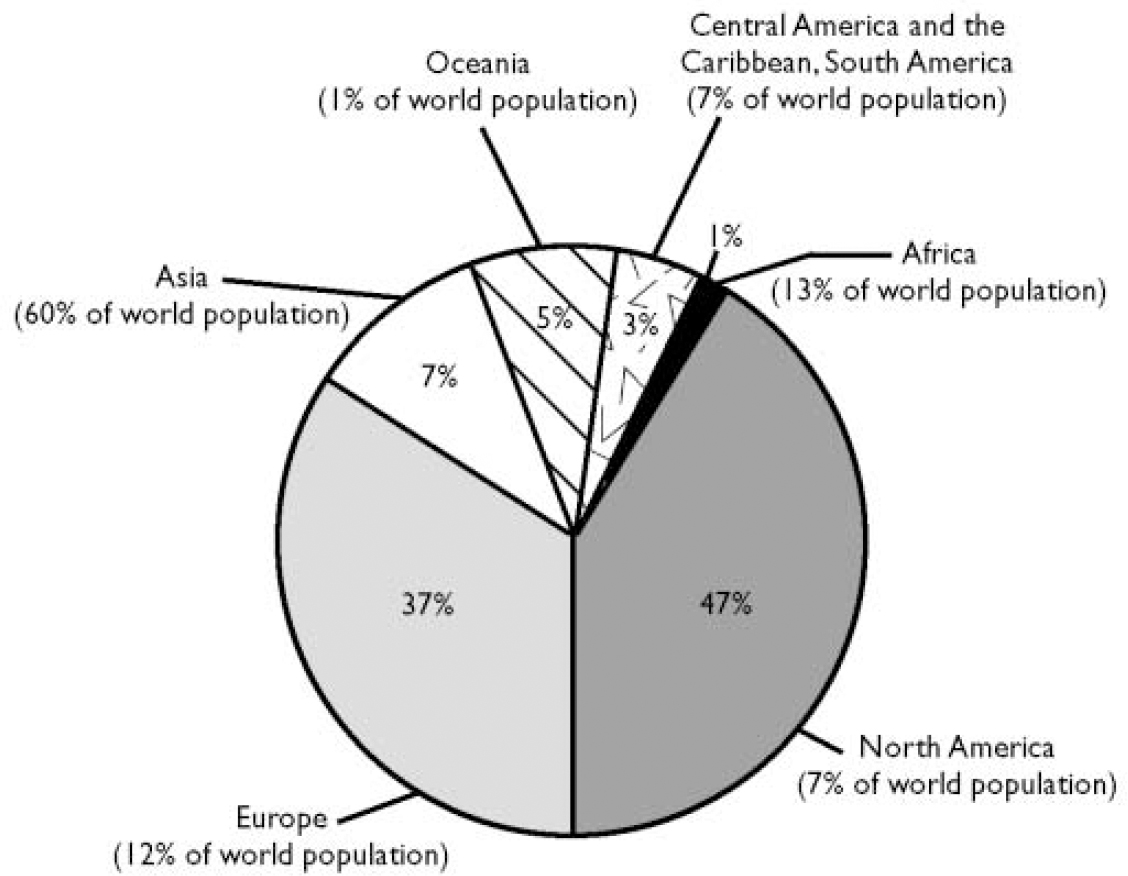
Fig. 1 Disparities in the medical consumption of morphine by region (1996–2000). Data supplied by the International Narcotics Control Board.
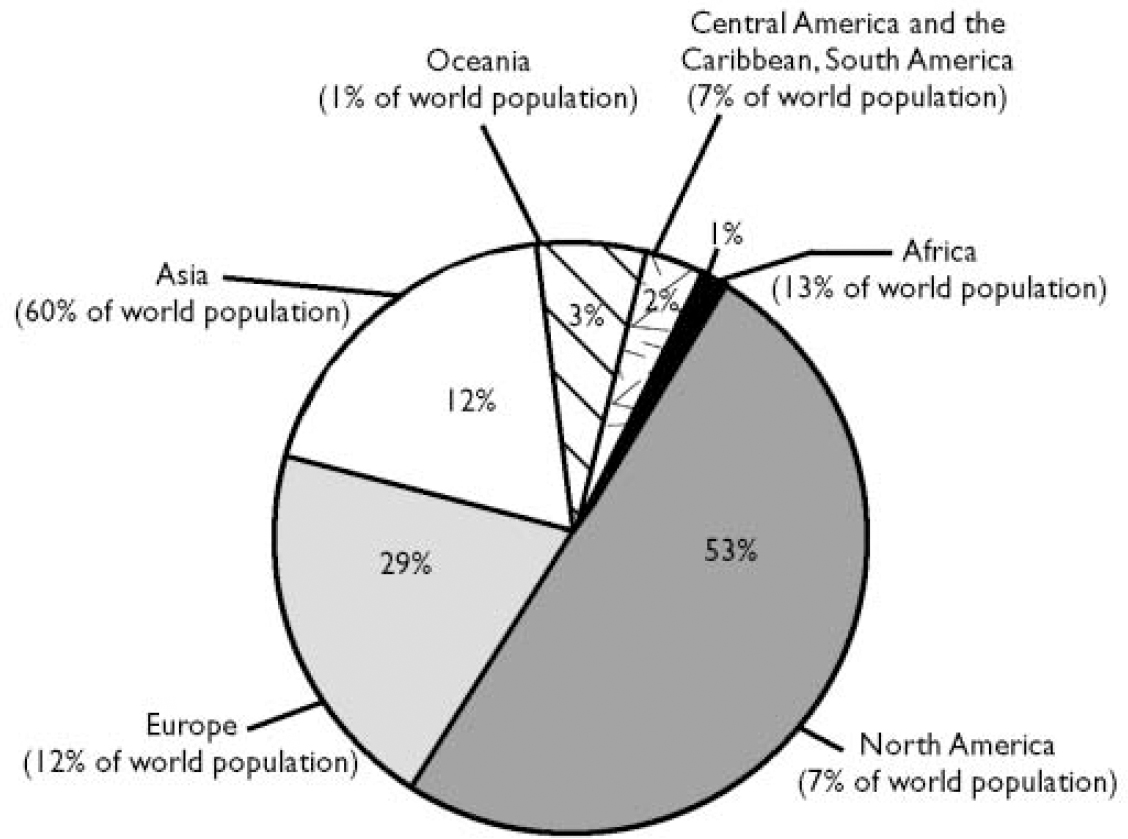
Fig. 2 Disparities in the medical consumption of the main narcotic drugs by region (codeine, dextropropoxyphene, dihydrocodeine, fentanyl, hydromorphone, ketobemidone, morphine, oxycodone, pethidine, tilidine and trimeperidine) by region (1996–2000). Data supplied by the International Narcotics Control Board.
In terms of individual consumption, the average per capita consumption of morphine in 1998 in the ten countries with the highest consumption levels was 31 g per 1000 inhabitants. In the ten countries with the next highest consumption levels, the corresponding figure was 16 g per 1000 inhabitants. In the next 60 countries with a total morphine consumption of more than 1 kg, it was only 2 g per 1000 inhabitants. In the remaining 120 countries, there was little or no opioid consumption, with several African countries reporting no morphine consumption at all. In a few countries there is now a small improvement because they have recently initiated programmes for the relief of cancer pain, but there has been no such improvement in most developing countries (International Narcotics Control Board, 2000).
In a world where the excessive use of controlled drugs tends to dominate discussions, the lack of such drugs receives comparatively little attention. However, the most frequently mentioned causes of inadequate availability of opioid drugs are: restrictive regulations and cumbersome administrative procedures; concerns about diversion and the consequences of inadvertent errors; concerns about iatrogenic addiction; and inadequate or insufficient training of health personnel. Clearly, there are issues here that must be addressed both by the governments concerned and by the medical profession but, in the interim, the net result is that only 10–30% of patients suffering from severe cancer-related pain may be receiving adequate treatment even in many technologically advanced countries, with an even lower rate in developing countries (Reference BonicaBonica, 1985; World Health Organization, 1986, 1993, 2000; International Narcotics Control Board, 2000). Although non-opioid, or indeed non-pharmacological, interventions may be utilised for a proportion of cases, it is widely acknowledged that severe pain requires opioids and, according to the World Health Organization Expert Committee and other reports, the worldwide medical need for opioids is not being fully met, particularly in relation to patients with cancer who may require large doses of opioids to obtain optimal pain relief (Reference Twycross and LackTwycross & Lack, 1984; Reference JoransonJoranson, 1993; World Health Organization, 1993). Because the manufacture, import and export of opioids are highly regulated both nationally and internationally, it is unlikely that populations within countries reporting very low statistics in all of these areas have easy access to these drugs. It is similarly unlikely that large quantities of illicit opioids are available for analgesic purposes in these very poor countries, when such big profits can be made from the illicit market in more affluent countries. There is, therefore, no reason to doubt the conclusions of the relevant international organisations about the woeful provision of effective analgesia to the developing nations of the world.
INTERNATIONAL DISPARITIES IN THE USE OF PSYCHOTROPIC SUBSTANCES
Interesting differences in the consumption of psychotropic substances can be detected in otherwise similar countries. For example, the USA and, to a lesser extent, Canada are by far the greatest consumers of amphetamine-type stimulants, primarily methylphenidate, amphetamine and various anorectics. Indeed, in recent years the USA has accounted for over 80% of global methylphenidate consumption, and per capita consumption of anorectics is the highest in the world – ten times more than the average for countries in Western Europe (Figs 3 and 4). However, the trend towards rapidly growing consumption, already seen in North America, is now occurring in other parts of the world such as Latin America and in certain countries in Asia and Europe as well (International Narcotics Control Board, 2001, 2002b ).
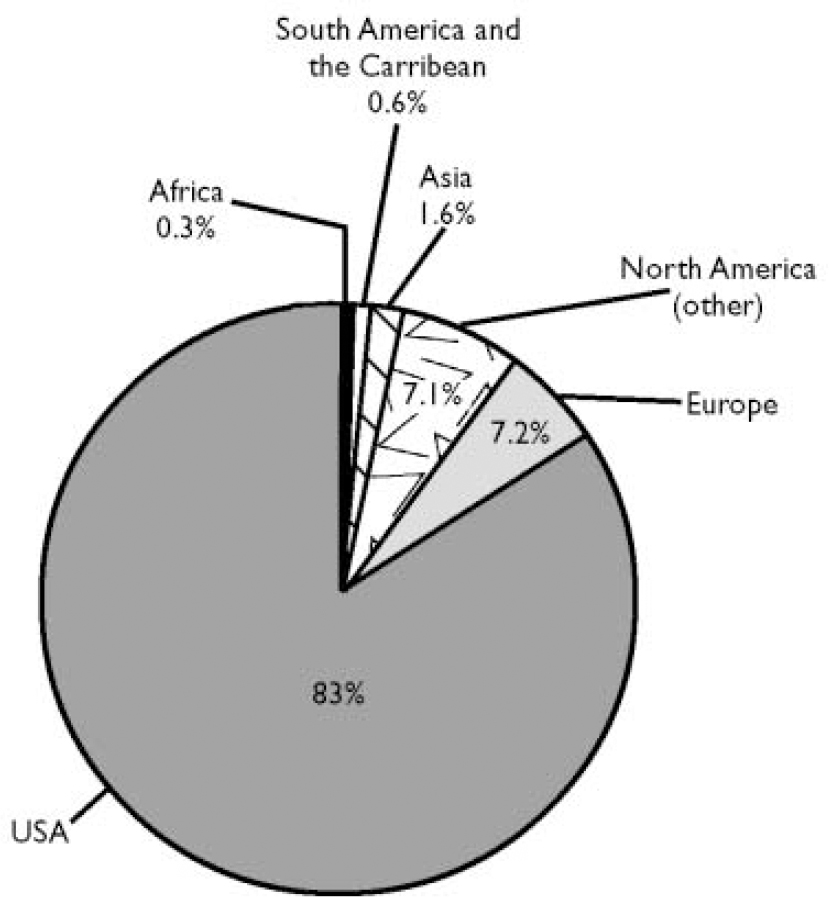
Fig. 3 Average consumption of methylphenidate (1996–2000). Data supplied by the International Narcotics Control Board.
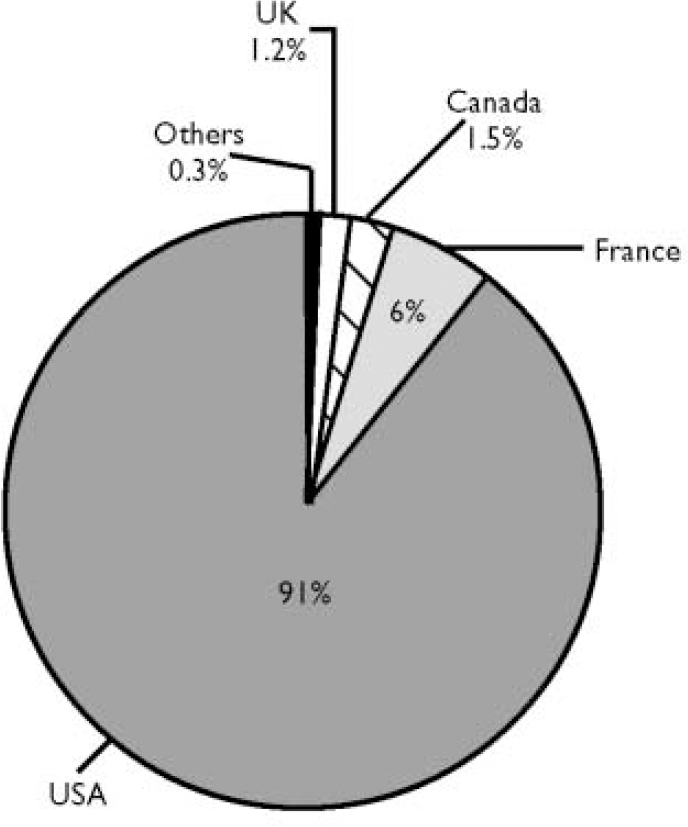
Fig. 4 Average consumption of dexamphetamine (1996–2000). Data supplied by the International Narcotics Control Board.
By way of contrast, many European countries consume relatively high amounts of benzodiazepine-type hypnotics, sedatives and anxiolytics, the European average for such drugs being three times higher than that of the USA (Figs 5 and 6). Indeed, in many countries, diazepam is among the 10–20 most prescribed drugs and among the 20–30 medicines with the highest sales figures. Against this background, there are still considerable variations between European countries, with doctors in France prescribing about four times more sedatives, hypotics and anxiolytics than doctors in Germany and the UK (International Narcotics Control Board, 2001, 2002b ).
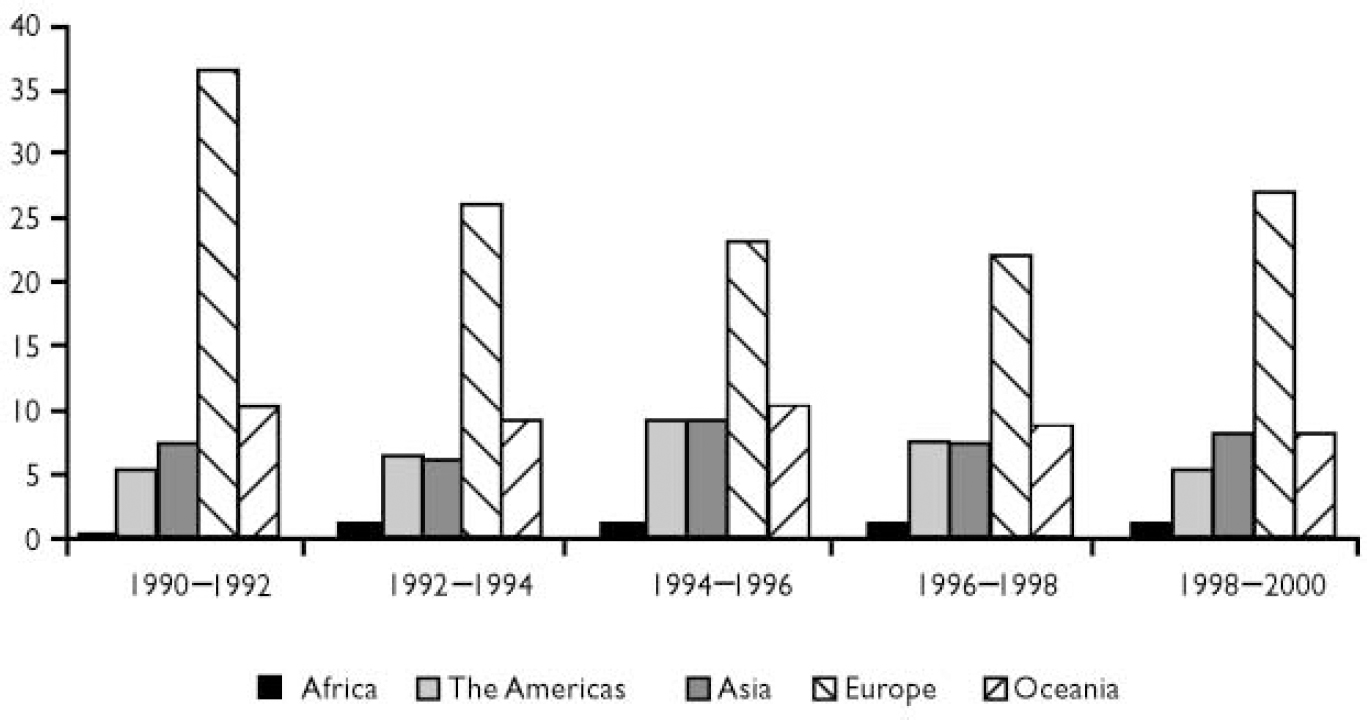
Fig. 5 Average consumption of benzodiazepine-type sedative hypnotics. Defined daily doses per 1000 inhabitants per day. Data supplied by the International Narcotics Control Board.
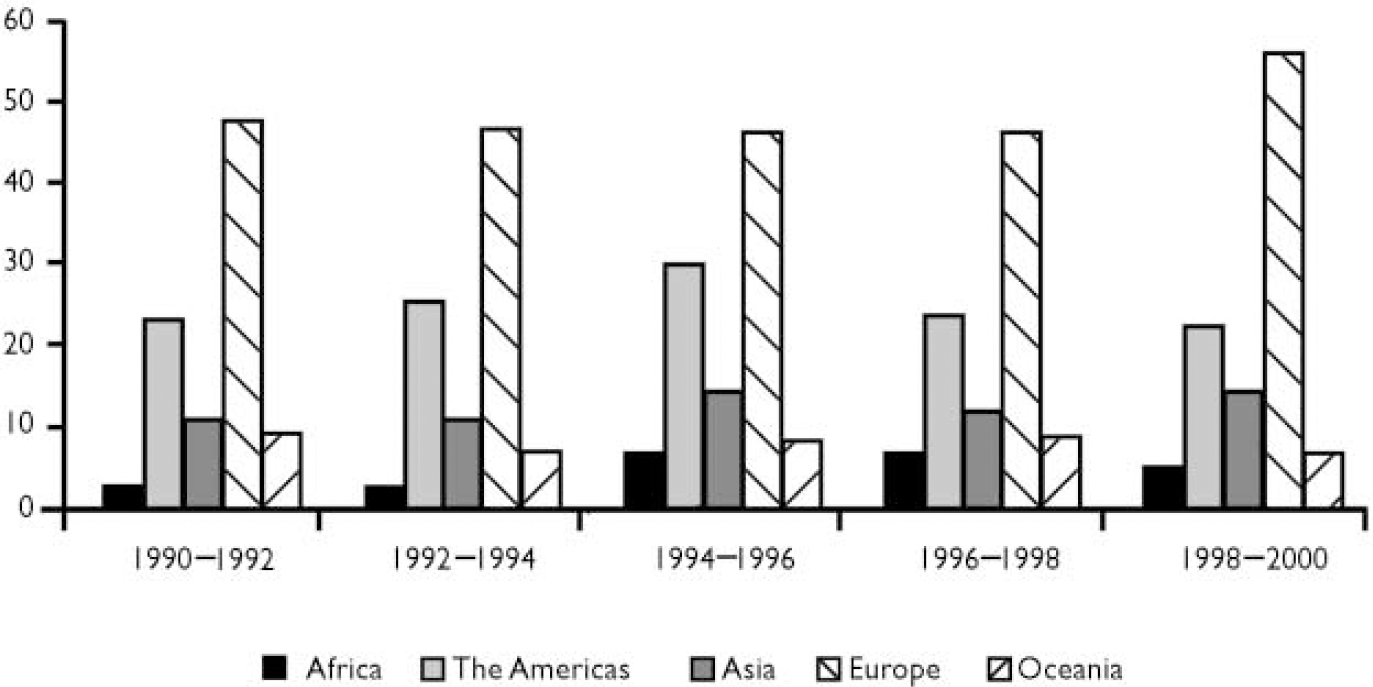
Fig. 6 Average consumption of benzodiazepine-type anxiolytics. Defined daily doses per 1000 inhabitants per day. Data supplied by the International Narcotics Control Board.
When consumption is measured in terms of the number of defined daily doses (DDDs) per 1000 individuals per day, these international differences are immediately apparent. For example, the average consumption of benzodiazepine-type sedatives during the period 1998–2000 was 27 DDDs in Europe, 5 in the Americas, 8 in Asia and Oceania and 1 in Africa (Fig. 5). The figures for consumption of anxiolytics, as measured by DDDs during the same period, were also disproportional: 56 DDDs per 1000 inhabitants per day in Europe, 23 in the Americas, 15 in Asia, 7 in Oceania and 5 in Africa, confirming that the differences are real and not due to inconsistencies in how use is reported (Fig. 6) (International Narcotics Control Board, 2001, 2002b ).
AVAILABILITY OF DRUGS AND ACCESS
Stepping back from these comparisons for a moment, it is worth remembering that during the past several decades the availability of increasingly effective, safe therapeutic agents has made an important contribution to improving health care throughout the world. The development of better medicines combined with better management of their availability could, and should, make the relief of pain and suffering more universally available as well as qualitatively better. Unfortunately, there are shortfalls in availability and there is evidence that in many countries these drugs do not necessarily reach those who need them most.
At the same time, excessive – sometimes apparently unlimited – availability of addictive medicines on national or international markets is as much a cause of concern as insufficient supplies. Although the unavailability of medicines deprives patients of their fundamental right to, and opportunities for, relief of pain and suffering, the excessive availability of such medicines frequently results in unjustified overconsumption and dependence. It may also lead to the diversion of such drugs to illicit trafficking and drug misuse (United Nations, 1991; World Health Organization, 2001a ).
Assessing the medical need for drugs and ensuring sufficient but not excessive supplies is therefore important. Unfortunately, most developing countries lack the necessary resources and expertise and the problem is compounded because there is no universal consumption standard that is applicable to all countries regardless of their social, demographic and economic situations. What constitutes optimum availability in one country may not be optimal in another. Furthermore, there is no country or region in which the status of the availability of a medicine can be considered as a standard for the rest of the world.
For developed countries, the most immediate problems are predominantly related to overconsumption. This is a trend that can be observed in many parts of the world, particularly in technologically advanced countries, but is not restricted to them. Excessive drug consumption that is medically unjustified has a number of general and sometimes country-specific causes and driving forces, of which the most significant are the commercial, sociocultural and educational environments in those countries. For example, newly gained wealth or affluence appears to be the origin of quickly growing drug consumption in countries experiencing rapid economic growth, especially if such consumption is perceived to be part of a new fashion.
One of the features of developed countries is an increasing consumption of sedative hypnotics for the treatment of anxiety and insomnia. It is not clear whether this reflects a true increase in the prevalence of these conditions but some surveys show that clinically significant anxiety affects up to 15% of the population (Reference Regier, Boyd and BurkeRegier et al, 1988; Reference Tohen and BrometTohen & Bromet, 2000; International Narcotics Control Board, 2001). In part, this can be attributed to the growing population of older people, who are the main consumers of these classes of drugs. Demographic change, therefore, may be a significant factor contributing to growing psychotropic consumption in many countries.
Other conditions too are increasing in prevalence and are demanding a pharmacological solution. Obesity is one such condition and it appears to be spreading at such a rate that it is now often referred to as an epidemic – and with prevalence rates as high as 30%, this does not appear to be an overstatement of the problem (Reference BjorntorpBjorntorp, 1997; Reference Rosenbaum, Leibel and HirschRosenbaum et al, 1997; International Narcotics Control Board, 2001). Its treatment increasingly involves the use of anorectic drugs, many of which are amphetamine-type stimulants or are closely related to these drugs.
As well as obesity there is growing awareness and diagnosis of attention-deficit hyper-activity disorder (ADHD), which is also treated symptomatically with stimulants, mostly methylphenidate. These two factors together account for the fact that the USA consumes far greater quantities of stimulants than other countries (Reference GhodseGhodse, 1999).
In addition to these conditions, a considerable proportion of patients is also reported to be suffering from personal, interpersonal and social problems rather than from real mental or physical disease. Indeed, in some countries as many as 25–35% of all patients were prescribed psychotropic drugs without being diagnosed as having a mental disorder (Reference Fombonne, Mousson and DassonvilleFombonne et al, 1989).
In view of the underlying conditions for which psychotropic substances are being prescribed, it is perhaps not surprising that there is an increasing tendency towards extended periods of use, with some individuals taking them for more than one year and some taking them more or less indefinitely. Indeed, it has been estimated that up to 4% of the population of many developed countries are regular long-term consumers of benzodiazepine-type sedative hypnotics (International Narcotics Control Board, 2001).
In one sense there is nothing wrong with long-term treatment – chronic conditions usually require chronic treatment. But chronic administration of substances with known dependence potential and/or other serious side-effects carries its own risks that may not outweigh the assumed benefits of treatment, particularly if there is no diagnosed mental disorder in the first place. Such concerns are heightened when psychotropic substances are prescribed for children. This used to be a comparatively rare occurrence but, with the increased recognition of ADHD, prescriptions of methylphenidate to children have increased very sharply, particularly in the USA (Reference GhodseGhodse, 1999). Although not wishing to deny the potential benefit of treating children with ADHD, it is natural to feel some unease about the liberal use of a drug with the specific intention of modifying a child's behaviour such that he/she becomes more compliant and less troublesome. Furthermore, treatment is initiated in the certain knowledge that it will be long-term treatment with a drug with a known dependence potential. The need for excellent research, so that treatment is based on a sound knowledge base, has never been greater. Similar concerns arise in relation to the treatment of obesity but the fact that the patients are usually adult means that they can participate in the decision-making process and share responsibility for that decision.
ATTITUDES AND EXPECTATIONS
Most of the above relates to developed countries (i.e. those that are technologically advanced). However, similar tendencies are now being observed in developing countries and in younger age groups. In other words, correcting mood and behaviour through controlled drugs is becoming ever more widespread. Within this environment of medicine-taking behaviour and of medicine-taking to manage behaviour, an expanding self-care culture is also becoming more socially acceptable. For example, recent surveys indicate that 70–95% of illnesses are managed by self-care in many countries (Reference FischFisch, 1979; Reference Vuckovic and NichterVuckovic & Nichter, 1997). This tendency has an important influence on medical practice in general and on the clinician–patient relationship but gives rise to particular concern when it involves the long-term use of psychotropic drugs to treat psychological reactions to personal and social problems.
There are also some interesting contrasts in attitudes and expectations. For example, the inappropriate use of sedative drugs by professionals as a ‘chemical strait-jacket’ for disturbed, often elderly patients is rightly condemned by public opinion. Yet, at the same time, patients’ demands for the relief of symptoms related to personal and social problems may be vociferous – not just for themselves but for their child if he/she suffers from ADHD. Furthermore, self-care using psychotropic substances is often perceived as quite acceptable and indeed as the legitimate and valued involvement of the patient in decisions about his/her care. It is these individual and population attitudes towards the treatment of a range of symptoms that are reflected in the drug consumption figures discussed earlier. They impose a considerable burden on national economies and infrastructures. For governments, keeping the supply and consumption of drugs, especially controlled drugs, in line with medically justified levels is not only an important public health issue but an economic issue too.
RESPONSIBILITIES OF THE MEDICAL PROFESSION
It is, therefore, worthwhile to consider the important determinants of the world's response to pain, anxiety and human suffering, in terms of achieving the appropriate availability of the appropriate drugs. The medical profession bears enormous responsibility in this area. It is the prescriber who determines the choice of drug and its dosage, duration and termination, and in this process exercises a great deal of professional freedom and discretion. A well-founded therapeutic decision is based on a good, trusted clinician–patient relationship, accurate assessment and diagnosis by the clinician and careful consideration of the therapeutic options, including expected benefits and risks.
Inappropriate prescription of controlled psychoactive medicines, which can lead to the excessive availability and overconsumption discussed earlier, includes: uninformed prescribing; inconsistent or lax prescribing; wilful and consistent misprescribing for misuse; self-prescribing and self-administration. The principal underlying causes of such behaviour appear to be: inadequate training; shortage of information; lenient or lax attitudes; lack of a sense of professional responsibility; unethical behaviour; personal drug addiction; criminal behaviour or direct financial interest. The therapeutic relationship between patient and clinician is also important and involves responsibilities on the part of both, but the nature and the extent of these responsibilities are heavily influenced by the culture of the country in question.
For all clinicians, however, the aim should be to ensure that drugs are prescribed only for the condition(s) for which they have been shown to be effective and not for any others, and that they are prescribed in the correct dosage and for the correct period of time. Although this may seem self-evident, some of the figures about drug consumption suggest that it is worthwhile to re-state the obvious. In particular, it is worth emphasising that prescription of the optimum dose is very important. If many patients receive too small or too large a dose, then a high proportion of the drug being prescribed is effectively wasted. In contrast, if most patients receive the correct dose of a drug that has been shown to be efficacious, then the total amount prescribed, even if large, will be used for its intended purpose. Amid concerns about the excessive consumption of psychotropic substances, it seems strange that, even in countries with well-developed health care systems and good access to psychotropic medication, it is estimated that fewer than 50% of those suffering from depression receive treatment. In developing countries, treatment rates for depression may be as low as 5% (World Health Assembly, 2002). In addition to lack of resources, other obstacles to care include fear, lack of information, stigmatisation and discrimination.
ROLE OF THE PHARMACEUTICAL INDUSTRY
Among other, wider influences on the availability of drugs, the role of the pharmaceutical industry and its regulation are clearly significant. Drug manufacture and trade are important dynamic sectors of the global economy subjected to an elaborate international regulatory mechanism for the protection of consumers. It is worth noting that this requires the collection of relatively reliable information about drug consumption worldwide, which forms the basis of the analysis presented here (Reference Ghodse and KhanGhodse & Khan, 1988).
However, globalisation of the economy, to the extent that is now occurring, affects the capacity of governments to monitor the activities of the pharmaceutical industry. The growing intensity and volume of free trade and multinational firms operating across national borders tends to weaken the power of governments to control trading in and access to drugs, their price and marketing practices. Ultimately, the safeguards are in the hand of governments. Each participant in the chain between manufacturer and consumer has particular interests, opportunities and obligations, but the ultimate beneficiaries should be the patient and society as a whole. Excessive availability occurs when the relative influence of these constituents is out of balance, for example as a result of weak government regulation or unethical or illegal drug promotion. For example, aggressive advertising and marketing by pharmaceutical firms strongly affects prescribing and consuming behaviour and, contrary to the provisions of the 1971 Convention on Psychotropic Substances (United Nations, 1971), in some countries such as the USA, some drugs are directly advertised to the consumer. There is also continuous pressure to reclassify drugs for ‘over-the-counter’ sale, which permits them to be advertised and sold directly to the public. In this context it is worth noting that a number of over-the-counter medications are familiar substances of misuse and dependence (Reference GhodseGhodse, 2002).
In summary, it is important that the pharmaceutical industry demonstrates its social responsibility as well as loyalty to shareholders. It is reasonable to expect it to play its part in curbing excessive consumption. Simultaneously, by exerting its influence on determining the price of drugs, many of which are beyond the reach of poorer countries, it can ease their availability where they are desperately needed.
THE IMPACT OF NEW TECHNOLOGIES
Electronic communication is a comparatively new variable in this scenario. Tele-medicine and internet prescribing may greatly facilitate access to medical and pharmaceutical services for large segments of society at lower cost. At the same time, the potential for error and intentional misuse is considerable. Substituting direct doctor–patient contact by electronic communication is problematic, particularly in relation to the diagnosis of psychiatric disorders and the prescription of controlled drugs. Efforts to regulate this quickly developing technical area will require close cooperation between countries and the relevant international bodies.
The internet also provides wide access to a huge amount of health-related information for professionals (clinicians) and for non-professionals (patients and their families). This alters the balance of knowledge and power in the therapeutic alliance and therefore changes its very nature. It has the potential to enhance the patient's role in the therapeutic alliance, empowering him/her to contribute more fully to joint decision-making.
CONCLUSION
To summarise, innovations in science and pharmaceutical development have gradually opened the way for safer, more selective and equally potent medicines for alleviating pain and other forms of human suffering. However, there are gross disparities in the availability of these medicines in different parts of the world and it is clear that, for much of the world, much suffering goes untreated. In developed countries, although the assessment of needs is often based on professional evaluation, actual availability tends to be in excess of actual needs and is strongly influenced by new cultural trends and expectations and the marketing practices of pharmaceutical companies. These factors, together with a weak regulatory system and improper medical practice, may result in unjustified and excessive consumption. This has serious implications in terms of the development of dependence on drugs with addictive potential and concerns about the way that human behaviour is being controlled by medicines. These concerns should not be allowed to undermine the value of modern psychotropic substances in alleviating human pain and suffering. There is a continuing challenge to ensure that such substances are available to all who need them, while reducing the potential for overconsumption where this exists.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ There are large disparities in the licit consumption of narcotic analgesics and psychotropic medications in different continents and in different countries in the same region.
-
▪ The excessive per capita consumption of psychotropic drugs is associated with adverse consequences, including misuse and dependence.
-
▪ There is a need for concerted efforts to promote the rational use of psychotropic drugs and narcotic analgesics.
LIMITATIONS
-
▪ Absence of evidence-based assessment of the need for narcotic analgesics and psychotropic drugs in many countries.
-
▪ Lack of information on the treatment of pain and mental disorders in countries with limited access to narcotic analgesics and psychotropic drugs.
-
▪ The cost of drugs in different countries has not been studied.
Acknowledgements
I am grateful to Mr P. Pachta, Mr N. Katkhouda, Ms G. Wieser-Herbeck, Ms Li-Qin Zhu and Ms C. Selva-Elizalde of the International Narcotics Control Board for their help in providing data for this paper.









eLetters
No eLetters have been published for this article.