Introduction
In this report, a 15-year-old adolescent completed a course of cognitive behavioural therapy (CBT) for obsessive compulsive disorder (OCD). Although he experienced obsessions and compulsions with a range of themes, his most troubling concern involved sexual obsessions – in the form of intrusive, visual mental imagery – depicting unwanted same-sex sexual acts. Following evidence-based guidelines (National Institute for Health and Care Excellence, 2005), exposure and response prevention (ERP) was initially employed and later augmented with imagery-based techniques, inspired by innovations in the CBT literature in adults (Hackmann et al., Reference Hackmann, Bennett-Levy and Holmes2011; Holmes et al., Reference Holmes, Hales, Young and Di Simplicio2019).
Literature review
OCD is characterised by the experience of persistent and uncontrollable obsessional thoughts alongside compulsive acts, which are aimed at reducing the distress associated with obsessions (American Psychiatric Association, 2013). While individuals with OCD experience fears around key themes such as contamination, harm, need for symmetry and so forth, sexual obsessions (e.g. paedophilia, unwanted homosexual acts, incest, etc.) are also common (Gordon, Reference Gordon2002; Pinto et al., Reference Pinto, Greenberg, Grados, Bienvenu, Samuels, Murphy, Hasler, Stout, Rauch, Shugart, Pauls, Knowles, Fyer, McCracken, Piacentini, Wang, Willour, Cullen, Liang and Nestadt2008; Rachman, Reference Rachman2007; Ruscio et al., Reference Ruscio, Stein, Chiu and Kessler2010; Williams et al., Reference Williams, Slimowicz, Tellawi and Wetterneck2014; Williams and Farris, Reference Williams and Farris2011). Adolescence is a period marked by the development of sexual feelings and sexual identity, yet there is limited literature on sexual obsessions in youth OCD. Up to a quarter of young people (aged 8–17 years) with OCD are estimated to experience sexual obsessions, with an increased likelihood associated with being male and higher OCD severity (Fernández De La Cruz et al., Reference Fernández De La Cruz, Barrow, Bolhuis, Krebs, Volz, Nakatani, Heyman and Mataix-Cols2013). Sexual obsessions can be associated with shame and stigma, leading to symptom concealment and thus potential mis-identification (Glazier et al., Reference Glazier, Wetterneck, Singh and Williams2015). Relative to other symptom dimensions of OCD, the presence of sexual obsessions has been linked with poorer treatment outcomes (Williams et al., Reference Williams, Farris, Turkheimer, Pinto, Ozanick, Franklin, Liebowitz, Simpson and Foa2011b).
The gold-standard treatment for OCD across the lifespan is CBT (National Institute for Health and Care Excellence, 2005). CBT for youth OCD has also been shown to be effective beyond traditional face-to-face settings, rapidly expanding into other delivery formats, including via the internet (Lenhard et al., Reference Lenhard, Andersson, Mataix-Cols, Rück, Vigerland, Högström, Hillborg, Brander, Ljungström, Ljótsson and Serlachius2017). This development is crucial to meet the increasing demand for evidence-based psychological treatments to tackle youth mental health globally (Patel et al., Reference Patel, Flisher, Hetrick and McGorry2007). When sexual obsessions are present, however, it remains contested whether CBT for OCD is as effective (Fernández De La Cruz et al., Reference Fernández De La Cruz, Barrow, Bolhuis, Krebs, Volz, Nakatani, Heyman and Mataix-Cols2013; Mataix-Cols et al., Reference Mataix-Cols, Marks, Greist, Kobak and Baer2002) and whether it requires longer treatments (Grant et al., Reference Grant, Pinto, Gunnip, Mancebo, Eisen and Rasmussen2006) and more specialist clinicians (Fernández De La Cruz et al., Reference Fernández De La Cruz, Barrow, Bolhuis, Krebs, Volz, Nakatani, Heyman and Mataix-Cols2013),
CBT for youth OCD is based on clinical models developed with adult populations (Turner, Reference Turner2006). Contrary to the adult literature, however, CBT protocols for youth OCD prioritise the ‘behavioural’ component (i.e. ERP) and place less emphasis on traditional ‘cognitive’ techniques (March, Reference March1995). ERP is thought to be the ‘active ingredient’ for treating OCD, but its underlying mechanisms warrant further research (Turner, Reference Turner2006). Specifically to sexual obsessions, there is very little clinical guidance on how to conduct ERP appropriately in young people. Some relevant clinical case descriptions involving adults have included exposure to sexual materials such as pornography (Williams et al., Reference Williams, Crozier and Powers2011a), which raises ethical issues in young people.
Traditional cognitive techniques are often perceived as too ‘complex’ for young people, who can struggle to verbalise their thoughts (Turner, Reference Turner2006). In addition to verbal-based thinking, however, cognitions can also take the form of mental imagery, especially for emotionally charged experiences (Hackmann et al., Reference Hackmann, Bennett-Levy and Holmes2011; Holmes et al., Reference Holmes, Hales, Young and Di Simplicio2019). Sexual obsessions are often imagery-based (Rachman, Reference Rachman2007), and the centrality of images is acknowledged in the diagnostic criteria for OCD (American Psychiatric Association, 2013). Nevertheless, direct work with images in OCD (beyond conventional imaginal exposure) by manipulating imagery content and/or properties is still in its infancy and is primarily limited to adults thus far (Maloney et al., Reference Maloney, Koh, Roberts and Pittenger2019; Veale et al., Reference Veale, Page, Woodward and Salkovskis2015). From a neuroscientific perspective, imagery is a hypothesised preferred mode of thinking in young people (Burnett Heyes et al., Reference Burnett Heyes, Lau and Holmes2013). If so, treatment innovation for youth OCD can leverage clinical science on imagery in established areas such as trauma (Ehlers and Clark, Reference Ehlers and Clark2000), alongside other rapidly evolving imagery-focused approaches specific to youth mental health (Pile et al., Reference Pile, Williamson, Saunders, Holmes and Lau2021; Schwarz et al., Reference Schwarz, Grasmann, Schreiber and Stangier2020).
Introduction to the case
Tom is a 15-year-old White British young person from a middle-class family living in England. He was referred to a Child and Adolescent Mental Health Service by his GP, who described that Tom is spending 6–12 hours a day with obsessions causing significant impairments to his quality of life.
Presenting problems
Tom and his mum Ruth attended the assessment together. Initially, he was too anxious to be seen alone. Tom reported experiencing thoughts that were frequent, vivid and distressing. Content of the images included setting fire to his house, stabbing someone, seeing Ruth sick in hospital and so forth, which he found deeply upsetting. Because these thoughts were repeated in his mind, Tom tried to ‘get rid of them’ or ‘say the opposite thing’. Tom also reported needing to complete a number of overt compulsions at home and school. For example, he would wash his hands throughout the day and had a particular washing routine. Tom found it hard to resist the compulsions even though he recognised the thoughts were ‘silly’. Tom also described increased palpitations, which made him think ‘am I having a heart attack?’. He had developed involuntary eye twitches when he experienced ‘bad thoughts’. Ruth said that Tom can be quite snappy at home when he is stressed. Ruth also recalled that Tom used to display ‘strange’ behaviours when he was younger, such as having to say goodbye five times when she left him in the playground at school. No thoughts of suicide or self-harm were reported, which remained the case throughout treatment. Sexual obsessions were not reported at this stage.
Method
Case conceptualisation
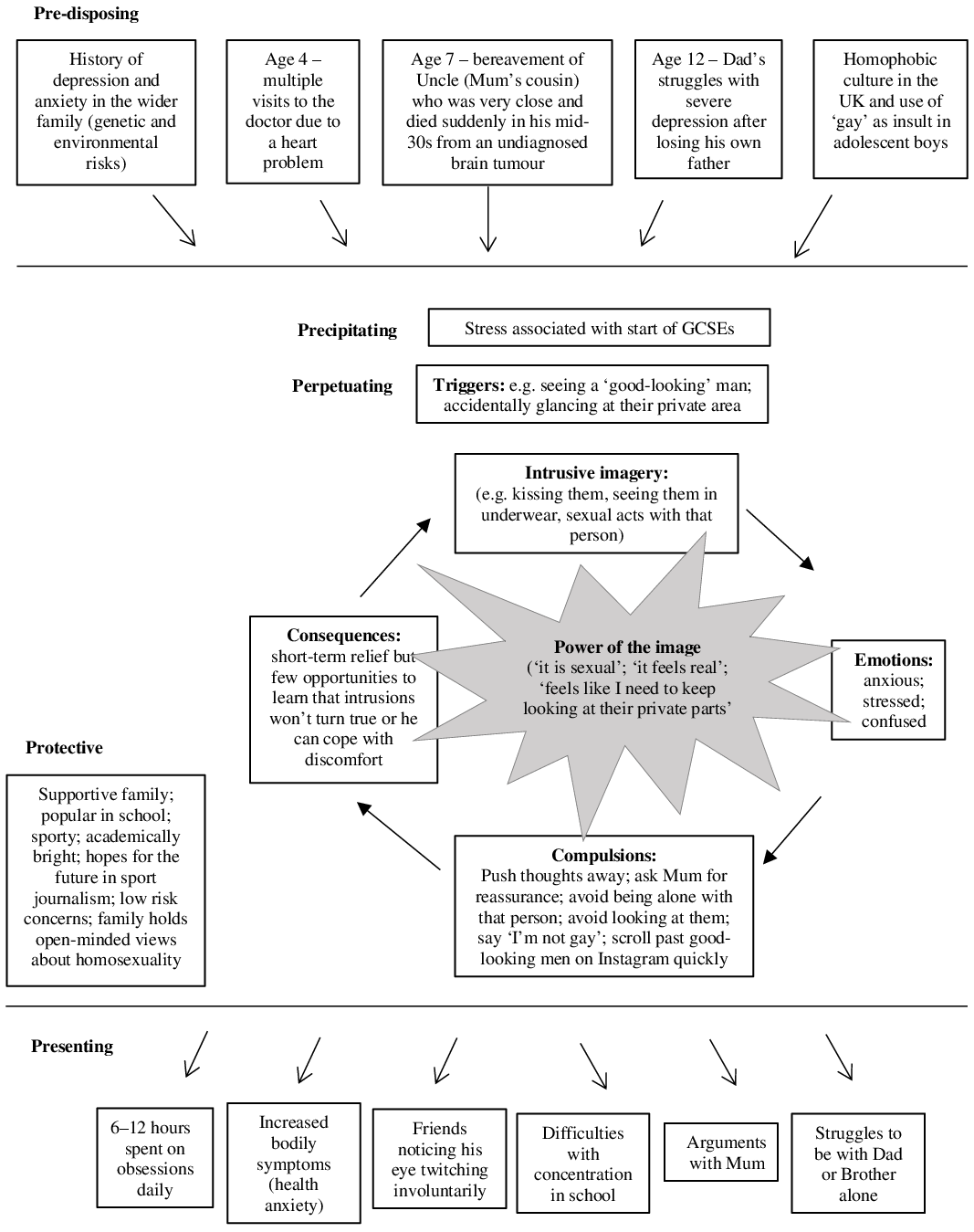
A 5-P’s framework (Macneil et al., Reference Macneil, Hasty, Conus and Berk2012) was used to (i) help Tom and Ruth make sense of Tom’s ‘story’ (shared verbally but depicted here visually; Fig. 1); (ii) inform suitability for a CBT-based approach; and (iii) aid the therapist in holding in mind the developmental context. A finer-grained cognitive behavioural formulation for OCD (Fig. 1), developed collaboratively later with Tom, informed the core therapeutic tasks targeting maintenance factors only. The exposition of the broader/longitudinal formulation is therefore necessarily brief, and the interested reader can refer to further details (Fig. 1).
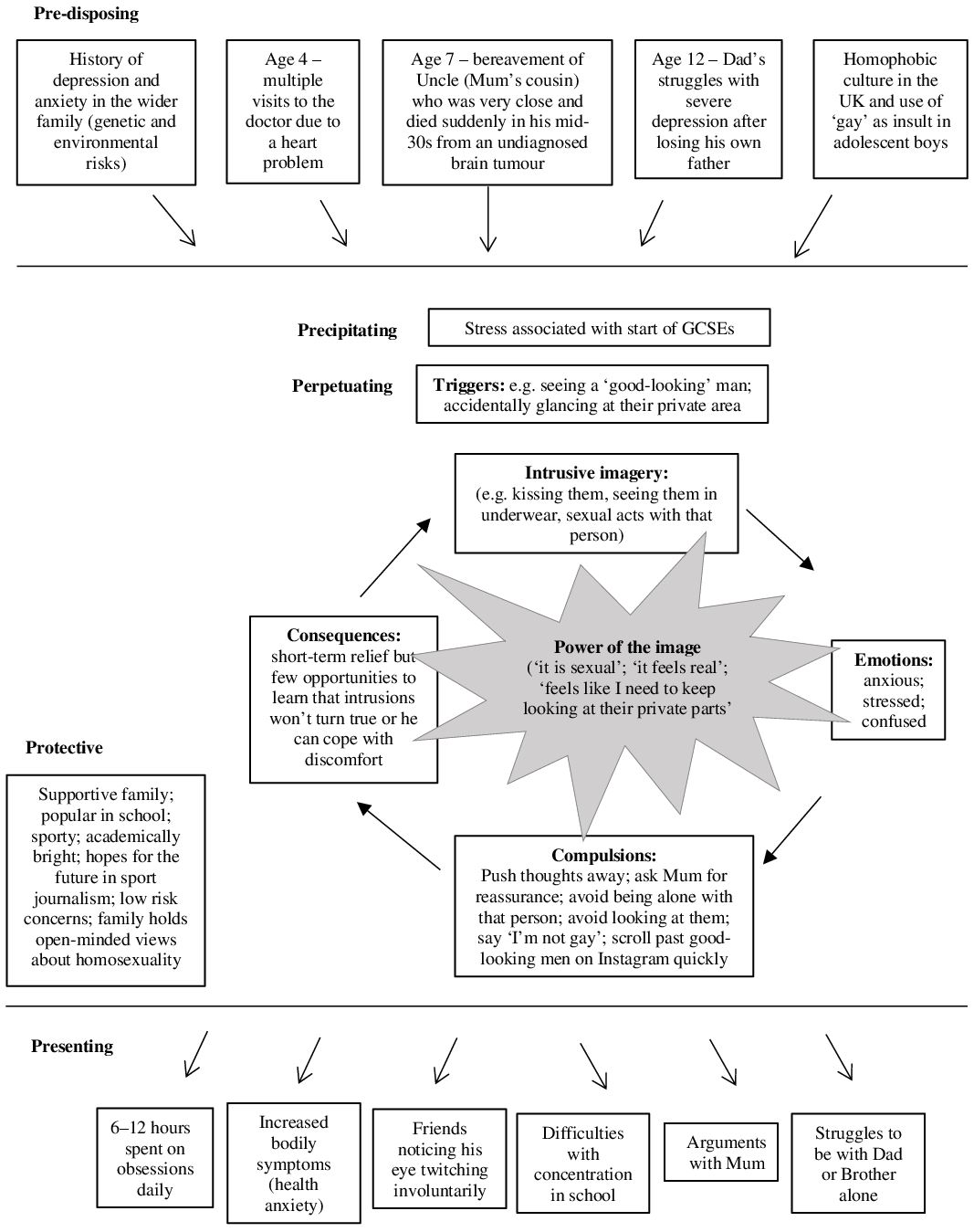
Figure 1. Developmental formulation for obsessive compulsive disorder with a focus on intrusive, unwanted, sexual mental imagery.
Key family factors and life events throughout Tom’s upbringing, particularly key bereavements (predisposing factors), might have enhanced Tom’s perception that ‘bad things will happen’. Tom’s heart problems as a child (including frequent hospital visits and family stress) appeared to have contributed to his vulnerabilities to anxiety (DeMaso et al., Reference DeMaso, Calderon, Taylor, Holland, Stopp, White, Bellinger, Rivkin, Wypij and Newburger2017; Gonzalez et al., Reference Gonzalez, Kimbro, Cutitta, Shabosky, Bilal, Penny and Lopez2021), as exemplified by some of his earlier ‘OCD-like’ rituals. Additionally, the homophobic culture in the UK (for example, the use of ‘gay’ as an insult) may have reinforced the idea that sexual obsessions are ‘unacceptable’ when adolescents seek to ‘fit in’.
The onset of Tom’s difficulties coincided with him starting GCSEs (General Certificate of Secondary Education) and during a developmental stage with the increased importance of peers and sensitivity to peer rejection (precipitating factors). Tom experienced obsessions as uncontrollable and negative; he performed compulsions to relieve distress, but which were counterproductive (perpetuating factors; described in more detail later). As OCD expanded over Tom’s life, it inevitably had a detrimental impact on his academic, social and home situation (presenting factors). Despite these difficulties, Tom has many individual and family strengths (protective factors), harnessed later in therapy. For example, he was highly motivated with ERP homework, which was further supported by his parents who would perform spontaneous ERP tasks alongside him at home (e.g. Ruth would lick the bottle of bleach and show Tom nothing deadly would happen; Tom would be suddenly asked by his dad if he could touch a table that has just been wiped with cleaning products).
OCD ‘traps’ (Derisley et al., Reference Derisley, Heyman, Robinson and Turner2008) were formulated for two identified core fears. For the fear of harming others, he explained that seeing a knife would trigger the image of ‘stabbing Mum’, leading to anxiety and stress; to relieve the distress, he would reassure himself ‘he would never do this’ and put the knife away. For the fear of contamination, wearing a jacket that has just been put on the floor would make him think’this is dirty’, leading to anxiety; to relieve the distress, he would avoid zipping his jacket all the way up so there is no contact with his mouth and he would apply hand gel multiple times a day. In both ‘traps’, compulsions and avoidant behaviours led to a short-term reduction in anxiety, but his feared predictions were unchallenged, and his perceived inability to cope was reinforced, maintaining distressing intrusions.
In the first session on his own, Tom revealed for the first time that he also experienced sexual obsessions of same-sex acts – in fact, this core fear was the most troubling of all. Therefore, the ‘trap’ concerning sexual obsessions is depicted as central in the formulation (Fig. 1). Sexual obsessions were normally triggered by seeing other men, such as male friends, family members or ‘good-looking’ people in the media. His intrusive images involved sexual acts, such as kissing them. Tom found them confusing and stressful. Tom would avoid looking/glancing at the ‘crotch’ area of other men, avoid being with them on his own, and self-reassure that he is straight, all of which only strengthened the sexual obsessions. As sexual exploration and identity forming is a normative task in adolescence, it seemed important to ascertain whether Tom found pleasure in experiencing such sexual images and whether there was a perceived judgement from self/others if he were gay.
As treatment progressed, the ‘power of the image’ (Holmes et al., Reference Holmes, Hales, Young and Di Simplicio2019) was later incorporated to fully understand the persistence of the sexual obsessions, unlike the non-sexual counterparts (Fig. 1). This simple but targeted formulation provided the clinical rationale for boosting ERP with imagery-based techniques to dissolve the image’s perceived power and fully tackle sexual obsessions.
Goals
Tom’s goals were to (i) have fewer and less distressing sexual obsessions in the presence of other ‘good-looking’ men; (ii) spend less time completing compulsions (e.g. excessive handwashing); and (iii) to improve his sleep.
Treatment delivery
Tom attended 13 60-minute sessions of individual CBT. Two appointments were in person with the remaining sessions over videoconferencing due to safety measures imposed by the COVID-19 pandemic. Ruth attended the initial session only, as Tom expressed preference for sessions on his own, consistent with potential issues of shame surrounding sexual obsessions (Gordon, Reference Gordon2002). Ruth was involved in brief check-ins at mid- and post-treatment. Tom agreed to share his learning with Ruth at the end of each session to ensure that the family was ‘on the same page’.
Content of sessions
In agreement with Tom, non-sexual obsessions were addressed first (sessions 1–7) to build his confidence prior to tackling sexual obsessions (sessions 8–12). Topics covered per session were as follows:
Sessions 1–2: Review of OCD symptoms; psychoeducation about anxiety; externalising OCD as a ‘bully’; normalising intrusions; behavioural experiment to show the counterproductive effects of imagery suppression (Table 1); goal setting.
Table 1. Imagery-based techniques used to target sexual (and other) obsessions
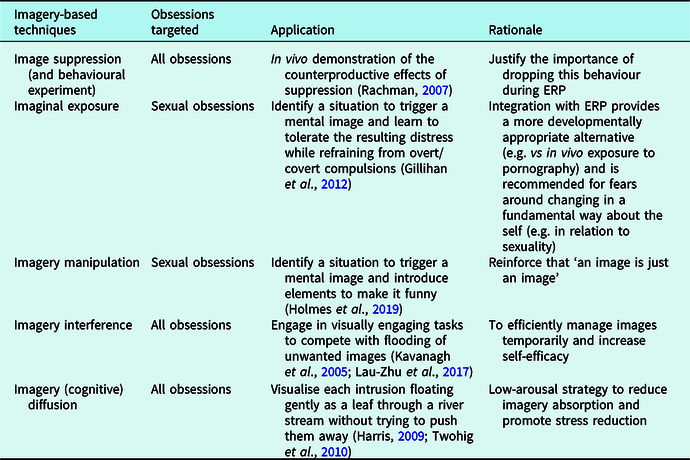
Sessions 3–7: Microformulation of OCD ‘traps’ for two non-sexual OCD themes (fear of harming others and fear of contamination); collaboratively developing the exposure hierarchy (and anxiety ratings 0–10 per step); in vivo ERP (e.g. holding a knife against his palm; wiping his mouth after touching a bottle of bleach); daily ERP homework.
Sessions 8–10: Microformulation on OCD ‘trap’ for sexual obsessions; psychoeducation (e.g. anxiety vs arousal; normalising sexual obsessions); ERP incorporating imaginal exposure, which involved holding in mind and tolerating the unwanted sexual obsession imagery (Table 1); Tom identified triggering situations for the exposure hierarchy: (i) sharing details of the obsessions in therapy; (ii) looking at the face of a male model; (iii) looking at a shirtless model; (iv) staring at the model’s underwear.
Although Tom’s intrusions became less distressing, they remained frequent and continued to disrupt his schoolwork. Thus, he was introduced to the notion of imagery interference (Table 1). He identified easily accessible and visually engaging activities (e.g. playing a videogame; scrolling through Instagram on his phone) to cut his attention off the obsessive visual-based images and then return to his homework.
Sessions 11–12: Tom progressed much slower through the ERP hierarchy for sexual (vs non-sexual) obsessions. He was unable to dismiss the image because it was ‘sexual’ and seemed ‘real’. Imaginal exposure was hence substituted with imagery manipulation (Table 1) to reduce the image’s ‘power’. Tom was introduced to the idea that he can modify what happens in the image (of ‘seeing a male underwear model in bed’) to whatever he wanted (akin to a ‘film director’) to make it less ‘sexual’. He first followed the therapist’s lead to imagine dressing up the model in a clown outfit. Tom then introduced his own ‘funny’ ideas. He brought two of his best friends in, and they all started jumping on trampolines, while the model rode a unicycle around the room with all of them shooting paint of multiple colours at each other. He later reported being able to apply the same ‘film director’ idea to sexual images involving other people.
Tom also reported being troubled by intrusions at nights, particularly when he was tired. As imagery interference strategies using his phone may be counterproductive for sleeping, an imagery defusion technique (see Table 1) was added to help him mindfully distance himself from his thoughts and help alleviate stress.
Session 13: Written relapse prevention plan; ideas for ‘overlearning’ were discussed, including ways to show he has ‘conquered’ the sexual obsessions (e.g. watching an age-appropriate gay-themed romantic film); working on endings.
Design and outcomes
Primary measures
The Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) was used to measure the severity of OCD at both the start and end of treatment. The CY-BOCS is a semi-structured interview for youth OCD that covers frequency, interference, distress, resistance and control of OCD symptoms (Scahill et al., Reference Scahill, Riddle, McSwiggin-Hardin, Ort, King, Goodman, Cicchetti and Leckman1997). It has good internal consistency, inter-rater reliability and convergent validity (Scahill et al., Reference Scahill, Riddle, McSwiggin-Hardin, Ort, King, Goodman, Cicchetti and Leckman1997). The CY-BOCS was administered by the treating clinician with both Tom and Ruth present each time.
Child and parent versions of the Revised Children’s Anxiety and Depression Scale (RCADS) were used at initial assessment and start, mid and end of treatment. The RCADS (Chorpita et al., Reference Chorpita, Yim, Moffitt, Umemoto and Francis2000) is a self-report questionnaire with six subscales to assess symptoms of depression and anxiety. It has good internal consistency (Chorpita et al., Reference Chorpita, Moffitt and Gray2005), test–re-test reliability (Chorpita et al., Reference Chorpita, Yim, Moffitt, Umemoto and Francis2000), convergent validity (Esbjørn et al., Reference Esbjørn, Sømhovd, Turnstedt and Reinholdt-Dunne2012) and concurrent validity (Chorpita et al., Reference Chorpita, Moffitt and Gray2005).
Secondary measures
Goal-based outcomes were used to track progress towards individualised goals at both start and end of treatment, each on a scale from 0 (not achieved at all) to 10 (fully achieved; Law and Jacob, Reference Law and Jacob2015). The Experience of Service Questionnaire (ESQ) was used to assess Tom’s satisfaction with the service at the end of treatment (Brown et al., Reference Brown, Ford, Deighton and Wolpert2014). Idiosyncratic ratings were used to track belief related to the power of sexualised images (‘It is sexual’) from 0 (not true at all) to 100 (extremely true).
Results
CY-BOCS scores dropped from 22 (moderate) to 5 (below the clinical cut-off of 16) from start to end of treatment. This corresponds to a 77% reduction in OCD symptoms, which is considered remission (Skarphedinsson et al., Reference Skarphedinsson, De Nadai, Storch, Lewin and Ivarsson2017).
According to the RCADS (Fig. 2), Tom’s self-reported symptoms of anxiety and depression were above the clinical threshold (t-score > 70) at assessment, start of and mid-treatment but had dropped below this threshold at end of treatment. Tom’s symptoms, as reported by Ruth, were generally higher. Ruth, however, reported symptom reduction earlier than Tom – with scores already below the clinical threshold by mid-treatment.
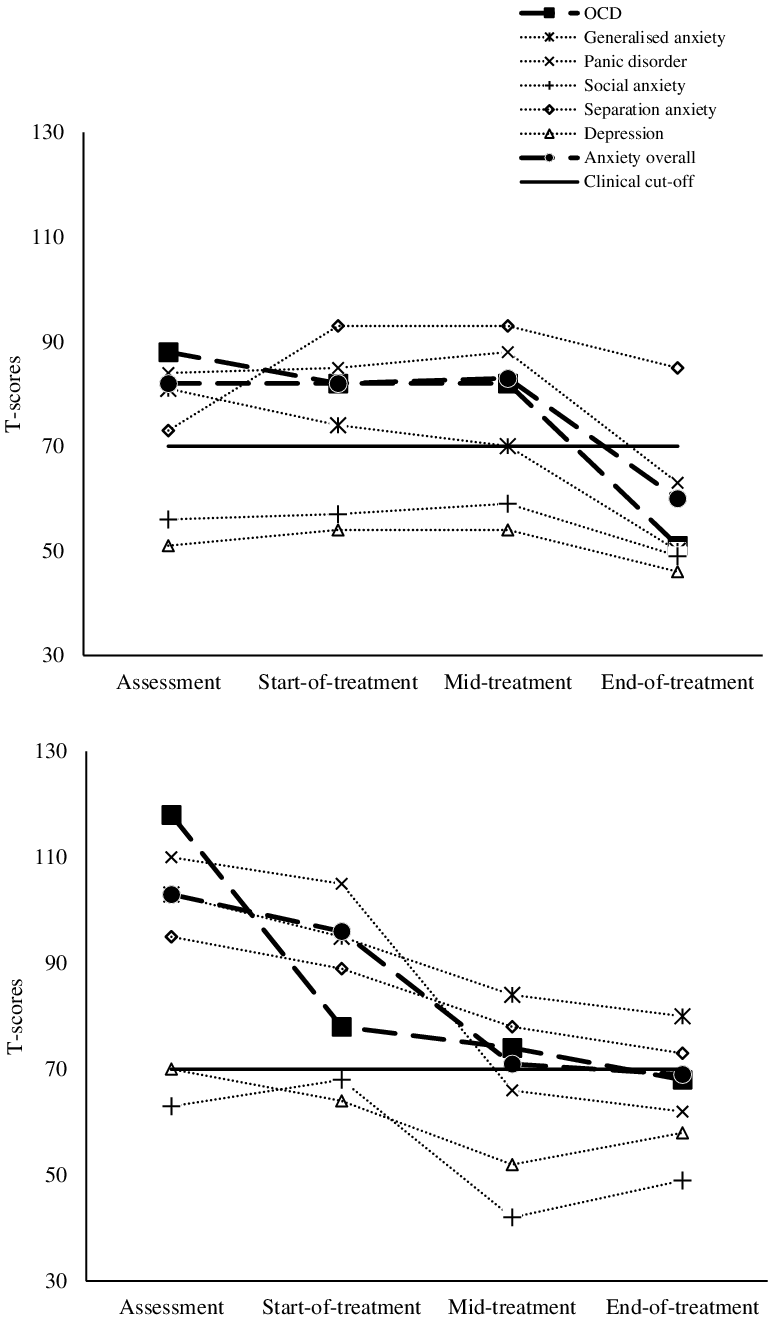
Figure 2. T-scores for the Revised Children Anxiety and Depression’s Scale rated by the child (top panel) and the parent (bottom panel) from assessment through to treatment. OCD, obsessive compulsive disorder.
The belief that his mental image ‘was sexual’ dropped from 90% to 0% after introducing the image manipulation technique in session 10.
Tom’s goals were rated as 1, 2 and 3 at the start of treatment, but 10, 9 and 8 at the end of treatment, reflecting high ratings of goal attainment. For the ESQ, he rated all items on satisfaction with care (e.g. ‘If a friend needed similar help, I would recommend that they come to the service’) as ‘certainly true’ and wrote in the free-text box ‘for me everything was pretty perfect’.
Discussion
This report presented the case of a 15-year-old adolescent, Tom, who underwent 13 sessions of weekly CBT for OCD with unwanted sexual obsessions as his most distressing symptoms. This was delivered by videoconferencing precipitated by a national lockdown in the UK due to the COVID-19 pandemic. The treatment protocol began with ERP – the conventional approach for youth OCD – and was later augmented with imagery-based techniques. Tom’s scores on all primary outcome measures (CY-BOCS and RCADS) indicated symptom reduction throughout treatment, with scores indicative of remission towards the end.
There are important issues to consider with our key outcome measures. While Tom’s RCADS scores declined throughout treatment, his scores were overall higher when rated by Ruth. Such informant discrepancies are common (De Los Reyes et al., Reference De Los Reyes, Augenstein, Wang, Thomas, Drabick, Burgers and Andres2015). Higher parental ratings of adolescent anxiety have been associated with higher maternal anxiety (Fjermestad et al., Reference Fjermestad, Nilsen, Johannessen and Karevold2017), which could partly reflect Ruth’s heightened concerns about Tom’s wellbeing (e.g. given his early experiences in the hospital) but possibly also her own ongoing worries related to the COVID-19 pandemic. Moreover, the CY-BOCS was administered by the treating clinician, which could have introduced a bias, although this is standard in routine care. Note, however, that this clinical interview was supplemented by the use of parent ratings and child self-reports producing converging results. Our multi-method assessment strengthened the observation that our intervention indeed successfully led to symptom reduction.
The ‘power’ of sexual imagery was understood as a key maintenance factor when ERP did not appear to produce treatment gains as rapidly as it had done for Tom’s non-sexual obsessions. While conventional ERP does consider imagery somewhat (e.g. imaginal exposure), here, further imagery-based techniques were drawn from the CBT literature for adults (Hackmann et al., Reference Hackmann, Bennett-Levy and Holmes2011; Holmes et al., Reference Holmes, Hales, Young and Di Simplicio2019), targeting both the content and properties of the image. Image manipulation was used as an alternative to ERP, whereas imagery defusion and interference techniques provided Tom with tools for day-to-day symptom relief in relation to all obsessive images, which Tom reported as especially helpful for his sleep (goal 3). Overall, the imagery-based approach was associated with full goal attainment for reducing sexual obsessions (goal 1). Note that the image manipulation approach differed from recent descriptions of imagery rescripting in adults with OCD (Maloney et al., Reference Maloney, Koh, Roberts and Pittenger2019; Veale et al., Reference Veale, Page, Woodward and Salkovskis2015), where aversive memories (from which intrusive images stemmed) were modified rather than the intrusive images per se. This memory-based approach was not employed here, as there was no indication that Tom’s sexual obsessions were linked to early experiences.
What could have been the mechanisms underlying these imagery techniques? Of all the techniques used, image manipulation was key, as it was linked to in-session changes in belief ratings of the ‘sexual’ nature of the image. Changing the content of a specific image served as a springboard for Tom to understand the power of images and to modify his relationship to sexual images in general. Such change could be thought to occur at a meta-cognitive level (Fisher and Wells, Reference Fisher and Wells2008) because Tom was able to generalise this technique to other unwanted sexual images outside of sessions (e.g. other men), perhaps learning that ‘an image is just an image’.
Mechanistic changes may have also occurred at the representational level, where new, non-threatening images were formed to compete with the original sexual image, resulting in ‘retrieval competition’ (Brewin, Reference Brewin2006) as Tom encountered triggers. What might be the exact nature of these competing representations? Inhibitory learning models (Craske et al., Reference Craske, Treanor, Conway, Zbozinek and Vervliet2014) posit the original association, where a conditioned stimulus (e.g. picture of a man) predicting an unconditioned stimulus (e.g. sexual intrusion) is later inhibited by a newly formed association, where the conditioned stimulus (e.g. picture of a man) predicts something else instead (e.g. humorous imagery). An alternative view suggests that concepts within semantic networks in OCD are biased towards OCD-based concerns (e.g. linking ‘man’ with ‘sex’) so that the creation of novel, more positive, and OCD-irrelevant associations dampens the activation of the original OCD-relevant associations (Moritz et al., Reference Moritz, Jelinek, Klinge and Naber2007), for example, through a technique called Associations Splitting in which alternative connections (e.g. linking ‘man’ with ‘humour’) could be introduced (Ching and Williams, Reference Ching and Williams2018). These hypothesised mechanisms could have been targeted with traditional verbal techniques, but the saliency of the imagery-based nature of Tom’s sexual obsessions lent itself naturally to the creative use of imagery-based approaches. Speculations about the mechanisms of our imagery-based approach and whether using imagery strengthens retrieval competition warrant further research.
Alternative cognitive behavioural approaches are worth considering. Tom could have persisted with conventional ERP, taking inspiration from existing protocols (Williams et al., Reference Williams, Crozier and Powers2011a; Williams and Wetterneck, Reference Williams and Wetterneck2019) where a variety of creative imaginal and in vivo exposure tasks have been suggested and could have been adapted for adolescents (e.g. watching a gay-themed teen movie; going to an LGBT-space for youth; imagining the consequences of being gay, and so forth). Note that for this ERP-based approach, more sessions might have been needed; the current case using imagery-based techniques needed 13 sessions, which is only average for paediatric OCD (Fernández De La Cruz et al., Reference Fernández De La Cruz, Barrow, Bolhuis, Krebs, Volz, Nakatani, Heyman and Mataix-Cols2013), rather than longer treatments as clinically indicated for sexual obsessions (Grant et al., Reference Grant, Pinto, Gunnip, Mancebo, Eisen and Rasmussen2006). Tom could have also explored a more verbal-based cognitive approach that is more commonly used in adult OCD, but its applicability for youth OCD remains unclear (Turner, Reference Turner2006). Tom explained that while he ‘knew’ that his parents would ultimately accept him regardless of his sexuality and that being gay did not mean he was ‘bad’, he continued to ‘feel’ uncomfortable with these sexual obsessions. A more fine-grained analysis of appraisals (Rachman, Reference Rachman1997; Salkovskis, Reference Salkovskis1985) could have been pursued, bearing in mind the balance between exploring meaning and providing counterproductive reassurance as therapists (Williams et al., Reference Williams, Farris, Turkheimer, Pinto, Ozanick, Franklin, Liebowitz, Simpson and Foa2011b).
Developmentally appropriate parental involvement can be important in CBT for youth OCD (National Institute for Health and Care Excellence, 2005). Minimal parental involvement may be more suitable when sexual obsessions are present in adolescents to facilitate disclosure. Nevertheless, there was still some parental involvement at brief check-ins at key timepoints, and Tom took the lead in summarising the session content for Ruth. This enhanced Tom’s autonomy in treatment. Interestingly, scores on the RCADS showed a discrepancy in the timing when marked symptom improvements were reported, which was by mid-treatment review for Ruth but not until end of treatment for Tom. Sexual obsessions were not targeted until after mid-treatment review, so possibly Tom’s persisting distress linked to his more private OCD symptoms was perhaps less perceptible by others. This underscores the importance of assessing and addressing sexual obsessions while respecting the privacy of an adolescent.
Although the treating clinician was also male, Tom denied experiencing sexual intrusions during therapy in response to the clinician, even when this was discussed explicitly. It remains possible that Tom felt embarrassed and thus concealed his intrusions (Glazier et al., Reference Glazier, Wetterneck, Singh and Williams2015), but this is unlikely, as efforts were made to normalise such experiences. Regardless, having a male therapist could have constituted an exposure task in itself in a safe, non-judgemental space that minimised the need for compulsions.
Clinical implications
This case raises the tantalising possibility that treatment innovation for youth OCD, specifically for sexual obsession, could leverage an imagery-based approach, bringing together ongoing developments in other clinical areas and translational work (see Table 1). This is consistent with evidence that imagery could provide privileged access to emotions in CBT and therefore a powerful vehicle for therapeutic change (Hackmann et al., Reference Hackmann, Bennett-Levy and Holmes2011; Holmes et al., Reference Holmes, Hales, Young and Di Simplicio2019). The improved developmental fit of using imagery is also in line with cognitive and neuroscientific studies (Burnett Heyes et al., Reference Burnett Heyes, Lau and Holmes2013; Pile et al., Reference Pile, Williamson, Saunders, Holmes and Lau2021; Schwarz et al., Reference Schwarz, Grasmann, Schreiber and Stangier2020). Indeed, service-user feedback pointed to the immediacy of treatment gains using imagery-based techniques and suggested a high degree of engagement, perhaps due to the more ‘playful’ nature (especially when the image’s content is transformed as a ‘film director’). The approach was also well-tolerated digitally by videoconferencing – a preferred modality for many young people.
Some may argue that the imagery-based techniques distracted from exposure and thus were additional forms of compulsion/avoidance (Gillihan et al., Reference Gillihan, Williams, Malcoun, Yadin and Foa2012). Concurrent activities during exposure, however, can be helpful if these facilitate approach to exposure (Parrish et al., Reference Parrish, Radomsky and Dugas2008). Careful psychoeducation took place to emphasise the importance of experiencing anxiety during exposure. Imagery interference and defusion were introduced to promote Tom’s sense of self-efficacy (important for ERP) in everyday symptom management. Imagery manipulation introduced fantasy elements to the sexual obsessions while still enabling Tom to engage with their content and thus was not fully ‘distracting’. Critically, Tom understood that these strategies were additional to, and not in lieu of, ERP homework, as demonstrated by his diligence with it. Had these imagery-based techniques become compulsions/avoidance, Tom would have experienced short-term relief only (e.g. within minutes or within the day), whereas he observed sustained improvements in symptom severity (e.g. averaging a whole week).
The imagery-based approach was used as an adjunct to traditional ERP for OCD; the possibility of using this as a stand-alone intervention could be tested in the future, at least where imagery is central to the formulation. As imagery-based techniques have yet to be fully exploited in CBT in youth, the current case can guide imagery-based applications across emotional disorders in youth. Assessments/formulations in youth OCD – and beyond – may benefit from direct and routine enquiry of imagery and its perceived power.
Limitations
The imagery-based approach consisted of a package of techniques, hence limiting the ability to compare their relative importance. Further replication is needed to ascertain our treatment’s effectiveness beyond a single adolescent and a single form of sexual obsessions. Underlying mechanisms were also under-explored, although there were indications of ‘metacognitive’ changes (about imagery’s power). Future work could consider more robust research designs (e.g. multiple baselines within the same participant; comparison of different techniques across participants), larger samples, more extended follow-ups (to confirm maintenance of treatment gains), and process measures of hypothesised mechanisms.
Key practice points
-
(1) Consider assessing sexual obsessions in adolescents privately.
-
(2) Look out for the presence of imagery in sexual obsessions and its perceived ‘power’.
-
(3) Use imaginal exposure within ERP as first-line treatment, and if needed, it could be augmented with other imagery techniques to reduce the imagery’s ‘power’.
-
(4) Imagery techniques can be suitable for young people and provide alternatives to more traditional ‘verbal’ cognitive techniques.
-
(5) Imagery techniques can be delivered in vivo and practised as homework.
Acknowledgements
We are grateful to the young person and the family for the opportunity to do this work with them, and for the three anonymous reviewers for their helpful comments.
Author contributions
Alex Lau-Zhu: Conceptualization (lead), Formal analysis (lead), Investigation (lead), Writing – original draft (lead); Alice Farrington: Supervision (supporting), Writing – review & editing (supporting); Clarence Bissessar: Conceptualization (supporting), Supervision (supporting), Writing – review & editing (supporting).
Financial support
A.L.Z. was supported by funding for professional clinical psychology training by Oxford Health NHS Foundation Trust.
Conflicts of interest
The authors declare none.
Ethics statements
The Authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the British Association of Behavioural and Cognitive Therapies and the British Psychological Society. The treatment ran as part of routine clinical cases within a Child and Adolescent Mental Health Service in the UK. Parental and child consent were obtained for the study, and names/ages used have been changed to preserve confidentiality.
Data availability statement
The data that support the findings of this study are available from the corresponding author, A.L.Z., upon reasonable request.





Comments
No Comments have been published for this article.