Introduction
Caring for an individual with dementia has been associated with poor mental health outcomes, but the mechanisms are less understood [Reference Sallim, Sayampanathan, Cuttilan and Ho1,Reference Sörensen and Conwell2]. Given the increasing number of dementia caregivers globally and potential negative impact on their mental wellbeing [3], identifying modifiable mechanisms that can be targeted through cost-effective interventions is important [Reference Hoff4].
A meta-analysis of 84 studies found that caregivers were more likely to report depressive symptoms compared to non-caregivers [Reference Pinquart and Sörensen5]. The incidence of depressive symptoms depends on the characteristics of both the caregiver and recipient [Reference Covinsky, Newcomer, Fox, Wood, Sands and Dane6]. Recipient characteristics such as younger age (i.e., <65 years old compared to ≥85), lower education, Hispanic ancestry, higher levels of disability, and the presence of challenging behaviors have all been associated with higher depressive symptoms among caregivers [Reference Covinsky, Newcomer, Fox, Wood, Sands and Dane6]. Being the spouse of a care recipient (especially the wife) is also a risk factor for depression compared to other types of caregiver roles, such as caring for grandchildren [Reference Covinsky, Newcomer, Fox, Wood, Sands and Dane6].
Caring for an individual with dementia involves both physical and neurological symptomatology, as well as behavioral and cognitive impairments, which may explain why dementia care incurs a greater burden compared to caring for an individual with only physical (but not neural) impairments [Reference Ory, Hoffman, Yee, Tennstedt and Schulz7]. The demands of dementia care could also lead to loneliness among the caregivers, and it is well documented that loneliness is linked with reduced mental wellbeing as well as physical morbidity and increased mortality [Reference Hawkley and Cacioppo8]. A UK-based prevalence study indicated that over two-thirds of dementia caregivers reported feeling lonely [Reference Victor, Rippon, Quinn, Nelis, Martyr and Hart9]. The study found that greater social isolation and caregiver stress were associated with higher loneliness, while caregiver–recipient relationship quality was protective.
The relationship between loneliness and depression is well established, but few studies have examined this in relation to dementia caregiving. Loneliness was a strong predictor of depressive symptoms among 242 spousal dementia caregivers in the United States [Reference Beeson, Horton-Deutsch, Farran and Neundorfer10], and a cross-sectional study of 49 spousal dementia caregivers found loneliness to explain 49% of the variance depressive symptoms [Reference Beeson11]. Caregiver loneliness might increase in parallel with the increasing severity of dementia, which could elevate the risk of adverse mental health among caregivers over time. However, most previous studies have relied on cross-sectional data and have not addressed potential mechanistic relationships between caregiving and depressive symptoms.
This study considered whether the higher risk of depressive symptoms among those caring for a partner with dementia (compared to noncaregiving partners) could be explained by loneliness. We tested the following hypotheses:
-
1. Individuals providing care for a partner with dementia (“dementia caregiving”) would have increased odds of depressive symptoms at follow-up compared to individuals not providing care for their partner (irrespective of partner dementia diagnosis).
-
2. Individuals caring for a partner with dementia would report higher levels of loneliness compared to other partnered caregivers.
-
3. Loneliness would mediate the relationship between dementia caregiving and subsequent depressive symptoms.
Method
Design, setting, and participants
Data were drawn from the English Longitudinal Study of Aging (ELSA), an ongoing nationally representative sample of approximately 11,000 individuals aged 50 and over living in England [Reference Steptoe, Breeze, Banks and Nazroo12]. Participants were initially recruited in 2002–2003. Refreshment samples of new participants were recruited in 2006–2007, 2008–2009, 2010–2011, 2012–2013, and 2014–2015. All waves took place biennially, consisting primarily of self-completed questionnaires and face-to-face interviews. Only waves 3–7 were used in this analysis due to the lack of caregiving data prior to wave 3. We included in our analysis refreshment samples introduced at waves 3 and 4. We selected 10,813 individuals who had provided care to their partner between wave 3 (2006–2007) and wave 5 (2010–2011) and had available data on loneliness at wave 6 (2012–2013) and depressive symptoms at wave 7 (2014–2015). Participants were only eligible if they had a partner.
Measurements
Caregiving
Caregiving status was assessed by self-report questions at waves 3–5 where participants were asked: “Did you look after anyone in the last week (including your partner or other people in your household)?” Participants responding “No” were classified as “non-caregiving partners.” Those responding “Yes” were then asked what their relation to the care recipient was (e.g., partner, child). Those not providing care to a partner were excluded from the final analytic sample. Individuals who provided care for a partner at least once across waves 3, 4, or 5 were classified as a caregiver. Functional impairments were assessed at waves 3–5, by asking whether household members required support with Activities of Daily Living (ADLs; bathing or showering, walking across a room, dressing, getting in/out of bed, eating, and using the toilet) or Instrumental Activities of Daily Living (IADLs; preparing a hot meal, doing house/garden work, using a map in unknown places, grocery shopping, taking medication, making telephone calls, and managing money) [Reference Torres, Lima-Costa, Marmot and de Oliveira13]. Dementia status was assessed based on self-reported physician-confirmed diagnoses of dementia at waves 3–5.
Based on this information, we derived a four-level caregiving measure: 0 = “Noncaregiving partners,” the reference category; 1 = “Care for partner with dementia”; 2 = “Care for partner with functional impairments (but no diagnosis of dementia)”; and 3 = “Care for partner with other conditions.” For mediation analyses, we created binary dummy variables representing each caregiving category.
Depressive symptoms
Self-reported depressive symptoms were assessed at wave 7 (2014/2015) using the 8-item version of the Center for Epidemiologic Studies Depression Scale (CES-D) [Reference Radloff14], see Supplementary Material, Table S1. This measure had good internal reliability across waves (α = 0.84) and comparable psychometric properties to the full 20-item scale [Reference Rafnsson, Shankar and Steptoe15,Reference Turvey, Wallace and Herzog16]. All items were coded as “Yes” or “No.” The item addressing loneliness was removed to ensure that this item did not overlap with the mediating effect of loneliness [Reference Cacioppo, Hawkley and Thisted17]. The remaining seven items were summed and dichotomized, such that participants with scores of ≥3 were considered with elevated depressive symptoms) [Reference Daly18,Reference White, Zaninotto, Walters, Kivimäki, Demakakos and Biddulph19].
Potential mediator
Loneliness was measured using the 3-item short form of the revised University of California, Los Angeles (UCLA) Loneliness Scale, which has been shown to have acceptable internal reliability (α = 0.78) [Reference Hughes, Waite, Hawkley and Cacioppo20]. Three questions assessed the frequency that an individual had felt a lack of companionship, left out, or isolated from others over the past week. Answers were scored on a 3-point scale ranging from 1 (“Hardly ever or never”) to 3 (“Often”) and summed to create a continuous total score ranging 3–9. Higher scores indicated increased loneliness [Reference Shankar, Hamer, McMunn and Steptoe21].
Covariates
Analyses were adjusted for covariates measured at the first nonmissing interview between waves 3 and 5. Adjustments were made for gender, age, household wealth, marital status, ethnicity, highest educational qualification, employment status, presence of limiting longstanding illness, and poor self-rated health.
To reduce possible confounding, all fully adjusted models were estimated with adjustment for baseline depressive symptoms (CES-D score of ≥3 at wave 3; or wave 4, if missing at wave 3). Please see Supplementary Material for more information on how and why these covariates were chosen/derived.
Statistical analysis
χ 2 and Kruskal–Wallis tests were used to investigate baseline demographic differences between the four caregiving categories, as well as differences in depressive symptoms at follow-up. The association between caregiving and depressive symptoms was assessed using logistic regression models. Three models were estimated (a) unadjusted, (b) adjusted for age, gender, education level, household wealth, marital status, ethnicity, employment status, and (c) additionally adjusted for the presence of longstanding limiting illness, self-rated health, and baseline depressive symptoms. All models were estimated in the overall sample and separately for men and women. We reported the odds ratios (OR) and 95% confidence intervals (CI).
Mediation was assessed by fitting a series of linear regression models for continuous variables (loneliness) and logistic regression models for binary variables (depressive symptoms) using the “medeff” statistical package in Stata 14 [Reference Hicks and Tingley22,23]. Due to differences in sample size across these groups, the sample sizes for assessing mediation vary slightly. The manuscript was written following STROBE guidelines [Reference von Elm, Altman, Egger, Pocock, Gøtzsche and Vandenbroucke24], see Supplementary Material, Table S2.
Sensitivity analyses
To reduce possible confounding, all models were re-estimated after excluding participants meeting criteria for clinically significant depressive symptoms at baseline (7-items CES-D score of ≥3 at wave 3 or wave 4 if missing at wave 3). A second sensitivity analysis was conducted on the main sample using the 8-item CES-D with a threshold of ≥4 at wave 3 or wave 4, if missing at wave 3, instead of the ≥3 threshold used in the main analysis.
Results
Sample characteristics
The analytical sample included 4,672 participants after removal of those with missing information on caregiving status (n = 1), covariates (n = 739), mediators (n = 74), or depressive symptoms (n = 928) (Figure 1).
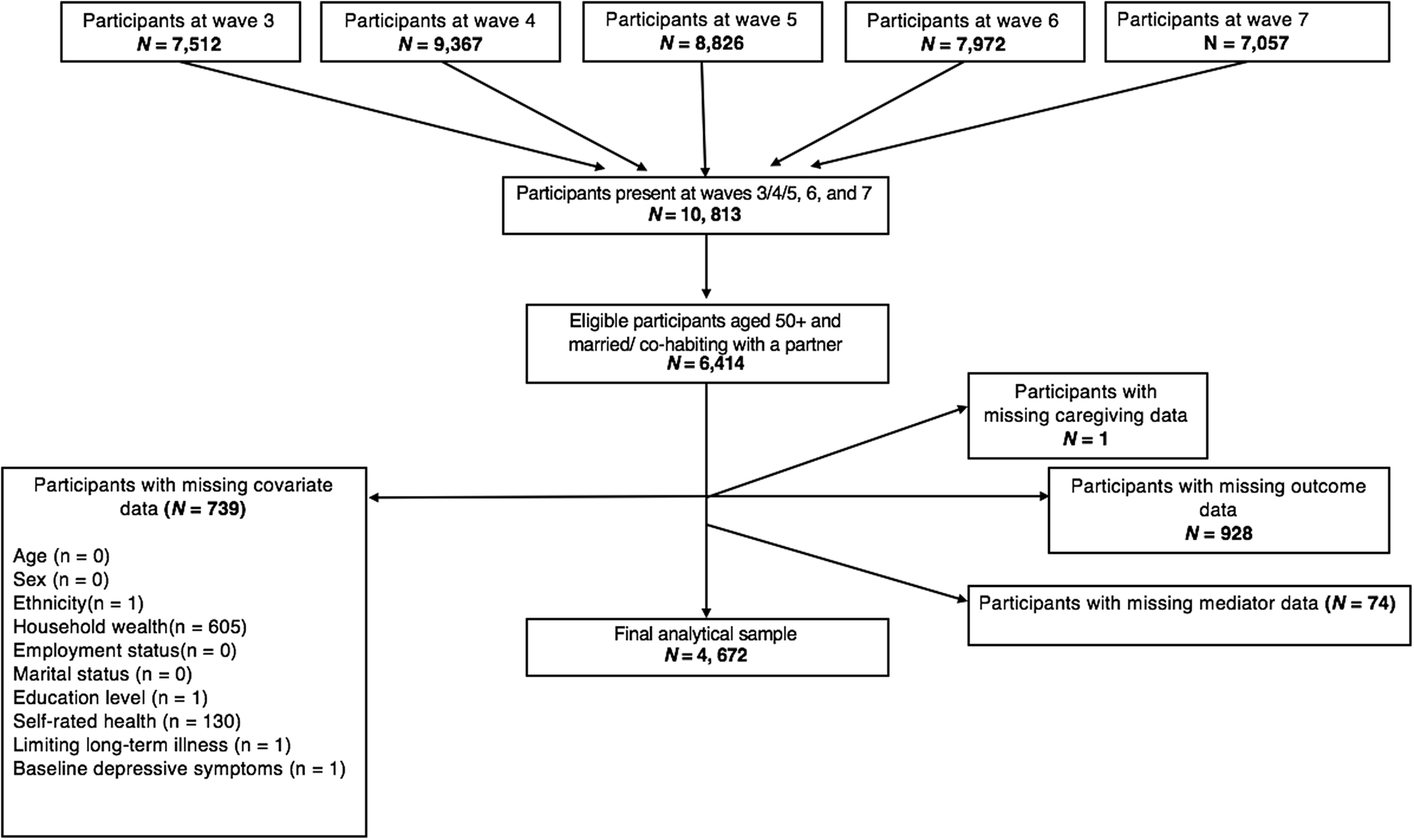
Figure 1. Participant flowchart for the analytical sample.
Compared to the main sample, excluded participants were older (64.8 vs. 61.9 years), more likely to be female (59 vs. 51%), similar in terms of non-White ethnicity (4 vs. 3%), had a higher incidence of longstanding limiting illnesses (37 vs. 26%), were less likely to have completed any formal education (minimum of O-level award or junior/middle high school diploma) (67 vs. 80%), were more likely to be in the lowest quintile of household wealth (25 vs. 8%) and were less likely to be employed (35 vs. 46%).
Table 1 presents the demographic characteristics of the analytical sample stratified by caregiving status. Compared to noncaregiving partners, those caring for a partner were more likely to be female than male (59 vs. 51%), older (63.5 vs. 61.8 years), to be in the lowest quintile of household wealth (18 vs. 9%), less likely to be employed (30 vs. 48%) and more likely to report longstanding limiting illnesses (35 vs. 25%). However, noncaregivers at baseline were less likely to report depressive symptoms (9 vs. 13%) and slightly lower levels of loneliness (mean of 3.8 vs. 4.0) compared to caregivers. All differences were statistically significant at p < 0.005 except for differences in ethnicity (p = 0.413).
Table 1. Demographic characteristics of the analytic sample (n = 4,672).
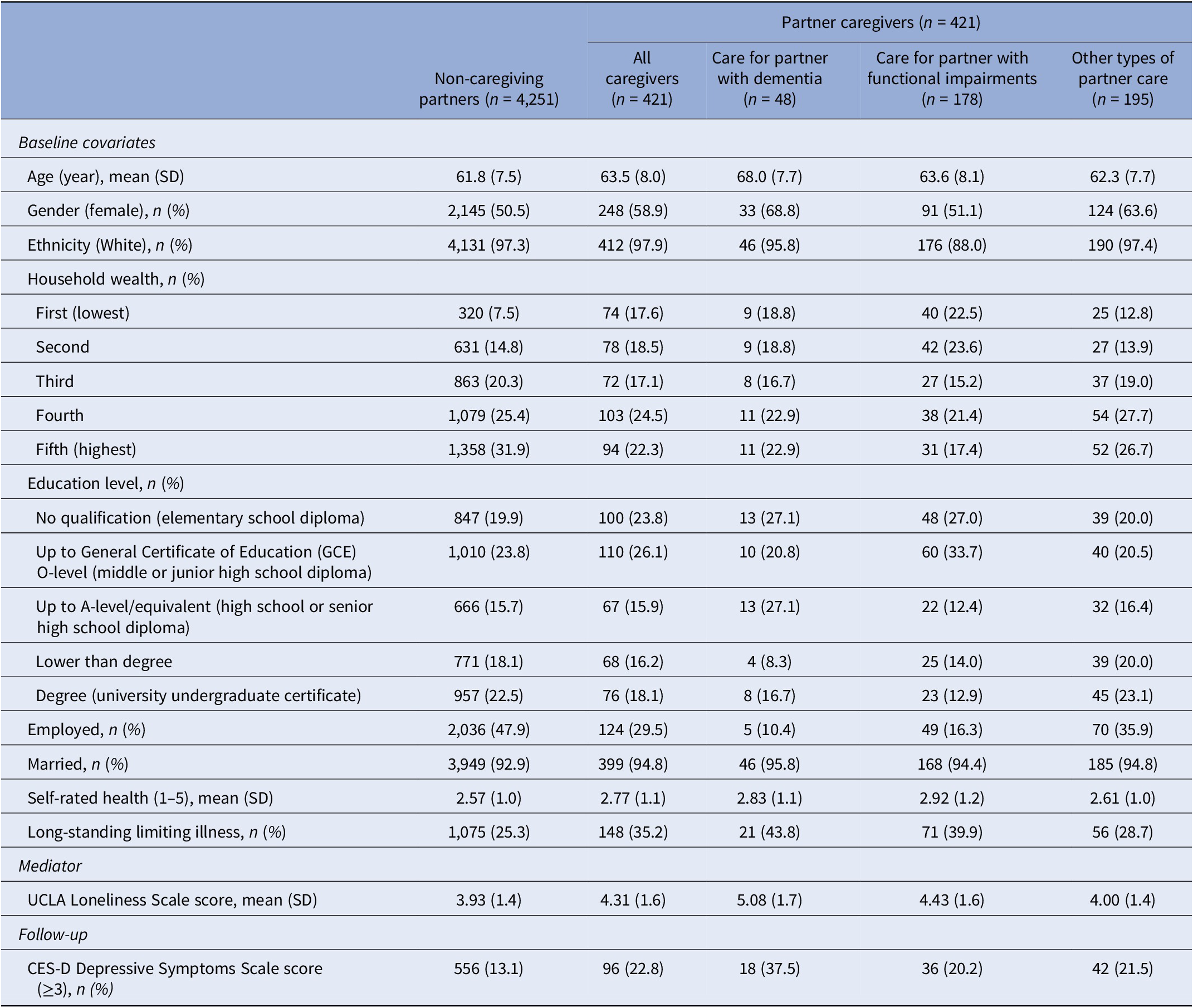
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; n, sample size; SD, standard deviation; UCLA, University of California, Los Angeles.
Dementia caregivers tended to be older (68.0 vs. 61.8 years; p < 0.001), female (69 vs. 51%; p < 0.007) and unemployed (10 vs. 48%; p < 0.001), compared to partners not providing any care. The proportion of dementia caregivers reporting depressive symptoms was higher compared to noncaregiving partners (at baseline: 21 vs. 9%; p < 0.001; at follow-up: 27 vs. 13%; p < 0.001) and when compared to those caring for a partner with functional impairments (baseline: 21 vs. 11%; p = 0.03; follow-up: 38 vs. 20%; p < 0.01). Dementia caregivers were also more likely to report depressive symptoms at follow-up (27 vs. 22%; p < 0.01) compared to those caring for a partner with other conditions, but this difference did not reach statistical significance at baseline (21 vs. 13%; p = 0.09). Dementia caregivers were more likely to report longstanding limiting illnesses at baseline (44 vs. 25%; p < 0.005).
The relationship between caregiving status and subsequent depressive symptoms at follow-up
In the overall sample (n = 4,672), individuals caring for their partner had higher odds of developing depressive symptoms compared with those not caring for their partners. This was especially the case among those providing care to a partner with dementia (Table 2). In unadjusted analyses, caregiving for a partner with dementia (OR = 3.99, 95% CI: 2.21, 7.20), functional impairments (OR = 1.68, 95% CI: 1.16, 2.45), or other conditions (OR = 1.82, 95% CI: 1.28, 2.60) was associated with increased levels of depressive symptoms. This relationship was attenuated after full adjustment and remained statistically significant only for those caring for a partner with dementia or other conditions. Preliminary analyses found no gender differences between various types of caregiving within those with depressive symptoms at follow-up (χ2 = 5.73, p = 0.13).
Table 2. The odds ratios of depressive symptomatology (wave 7) among caregivers (waves 3–5) in the full analytic sample (N = 4,672).
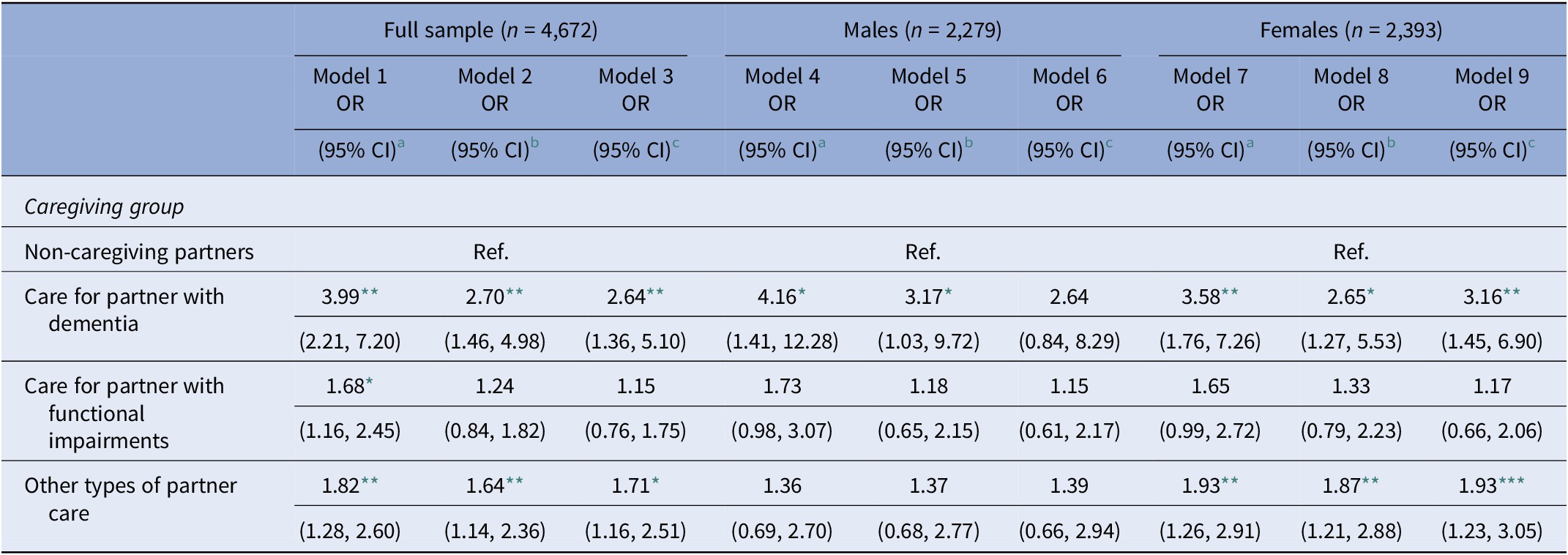
Abbreviations: CI, confidence interval; OR, odds ratio.
a Unadjusted model.
b Model adjusted for demographic factors (age, marital status, ethnicity, socioeconomic status, employment, and education).
c Model adjusted for demographic factors and health-related factors (presence of long-standing limiting illnesses, self-rated health, and baseline depressive symptoms); each caregiving measure was tested in a separate model.
* p < 0.05.
** p < 0.005.
*** p < 0.001.
The mediating role of loneliness (wave 6) on the association between caregiving (waves 3–5) and depressive symptoms (wave 7)
Caring for a partner with dementia was positively associated with loneliness (β = 0.31, 95% CI: 0.15, 0.47), and loneliness was positively associated with depressive symptoms at follow-up (OR = 1.11, 95% CI: 0.92, 1.30). Moreover, caring for a partner with dementia was indirectly related to depressive symptoms via loneliness (β = 0.04, Bias corrected [Bc] CI: 0.02, 0.07), which explained 34% of the total effect (Figure 2).

Figure 2. Mediation analysis of the association between dementia care (waves 3/4/5) on depressive symptoms (wave 7) via loneliness (wave 6) (n = 4,229). *p < 0.05. All models were adjusted for demographics (age, marital status, ethnicity, socioeconomic status, employment and education) and health-related (presence of longstanding limiting illnesses, self-rated health, and baseline depressive symptoms) factors. A bias-corrected bootstrap using 1,000 iterations was applied to all models. Each caregiving measure was tested in a separate model.
Caring for a partner with other conditions was not significantly associated with loneliness (β = −0.004, 95% CI: −0.07, 0.06), and although loneliness was positively related to depressive symptoms (OR = 1.13, 95% CI: 0.94, 1.32), there was no evidence of an indirect effect via loneliness (β = −0.001, Bc CI: −0.008, 0.008). Since caring for a partner with functional impairments was not associated with depressive symptoms after full adjustment (i.e., no “Total effect”), this model was not tested for mediation (Figure 3).

Figure 3. Mediation analysis of the association between “care for a partner with other conditions” (waves 3/4/5) on depressive symptoms (wave 7) via loneliness (wave 6) (n = 4,446). *p < 0.05. All models were adjusted for demographics (age, marital status, ethnicity, socioeconomic status, employment, and education) and health-related (presence of longstanding limiting illnesses and self-rated health) factors. A bias-corrected bootstrap with 1,000 iterations was applied to all models (see Supplementary Materials for details).
Sensitivity analyses
We conducted two sensitivity analyses. Firstly, we excluded all participants who met the criteria for baseline depressive symptoms (N = 423), see Supplementary Material, Table S3. In the second analysis, we re-estimated all models using the original CES-D scale (with a cut-off of ≥4), see Supplementary Material, Table S4. The new results did not substantially alter the strength of the initial associations found between caregiving types and depressive symptoms at follow-up compared to our main analyses.
Moreover, the indirect effect of caregiving on depressive symptoms via loneliness remained statistically significant among dementia caregivers and non-significant among those in the “other care” category in both sensitivity analyses (see Supplementary Material, Figures S1–S4).
Discussion
We found that caring for a partner with dementia was associated with higher odds of depressive symptoms at follow-up compared to noncaregiving partners and that loneliness significantly mediated this association. A similar association was observed for those caring for other conditions than dementia, but the increased odds of depressive symptoms was lower than for those caring for a partner with dementia. We did not find evidence to suggest loneliness mediates the association between care for a partner with other conditions and subsequent depressive symptoms.
Consistent with our first hypothesis, the odds of depressive symptoms were higher among dementia caregivers when compared to non-caregiving partners. This is in line with previous research [Reference Pinquart and Sörensen5,Reference Covinsky, Newcomer, Fox, Wood, Sands and Dane6] and may reflect the caregiving burden associated with increased psychological and mental demands, as well as the physical and behavioral challenges that can present in patients with dementia and the strain these can place on the couple [Reference Ory, Hoffman, Yee, Tennstedt and Schulz7]. However, we did not find evidence of gender differences in the relationships between caregiving and depressive symptoms, consistent with one other previous study [Reference Pöysti, Laakkonen, Strandberg, Savikko, Tilvis and Eloniemi-Sulkava25]. Caring for individuals with dementia requires ongoing care that may impose withdrawal from paid work, which is another determinant of poor mental health [Reference Sefcik, Petrovsky, McPhillips, Hodgon and Gitlin26,Reference Quinn, Clare and Woods27]. While some partners may embrace the caregiving role, some report feelings of “role captivity” which is likely to feed into the development of depressive symptoms [Reference Givens, Mezzacappa, Heeren, Yaffe and Fredman28]. Role captivity refers to a sense of being trapped in a specific social role which limits the individual’s freedom. This might partly be responsible for feelings of loneliness and depressive symptomatology.
Our findings might support the idea that caring for a partner with both mental and functional impairments (i.e., dementia) is more strenuous than caring for a partner with only functional impairments or physical disability [Reference Ory, Hoffman, Yee, Tennstedt and Schulz7]. Although we did not make an active comparison between these groups, this was inferred from the larger odds ratio in the dementia care group compared to the functional impairments group. Notably, caring for a partner with only physical, rather than both mental and physical impairments, as in the case of dementia, was not found to be associated with subsequent higher odds of depressive symptoms. This is thought-provoking because it suggests that caring for partners with physical impairments only is not necessarily linked to poorer mental health. It is also possible that greater support is available to carers for partners with only functional impairments, or that those caring for a partner with dementia have less time and opportunities for social support, and therefore more vulnerable to an increased risk of depressive symptoms. Ultimately, it may be that it is the addition of psychological/behavioral impairments that tips the association towards significance.
Consistent with our second hypothesis, loneliness was highest among dementia caregivers compared to non-caregiving partners. A possible explanation for this is the shift from partnership to the caregiver-patient role, and thus the loss of a previously meaningful relationship. This is consistent with qualitative findings describing the caregiving experience as one of ‘relational deprivation’ [Reference Vasileiou, Barnett, Barreto, Vines, Atkinson and Lawson29]. The burden of caregiving activities may increase loneliness by reducing the opportunities to engage with a wider social circle [Reference Beeson, Horton-Deutsch, Farran and Neundorfer10]. Similarly, the progressive deterioration in cognitive functioning among those with dementia often also results in personality changes, that may precipitate a significant emotional loss in the form of anticipatory grief [Reference Robins Wahlin and Byrne30–Reference Blandin and Pepin32]. Both of these factors may contribute to increased loneliness.
Consistent with our third hypothesis, we found evidence of indirect effects of dementia caregiving on depressive symptoms via loneliness, highlighting the importance of considering loneliness when supporting such individuals. Interestingly, there was a direct effect of caring for other conditions on depressive symptoms; however, we did not find any indirect effect via loneliness. This suggests that policies and/or therapeutic interventions need to be tailored to the specific needs of the couple. Future research could attempt to uncover what are the specific mediating factors of the “other care” category.
Strengths and limitations
Our analysis represents a longitudinal investigation of dementia caregivers living in their community and their subsequent level of loneliness and mental health, using a representative sample of the English population. This is a significant benefit since many studies of caregivers are based on the recruitment of participants who have self-identified as distressed caregivers, a factor likely to inflate the findings and reduce ecological validity [Reference Ask, Langballe, Holmen, Selbæk, Saltvedt and Tambs33]. We also used a superior design compared to past studies where comparison groups have contained both partnered and un-partnered noncaregivers. Being married or having a partner is usually protective of mental health [Reference Akhtar-Danesh and Landeen34], but previous studies may have underestimated the effect of caregiving on depressive symptoms. Furthermore, we used a prospective longitudinal data that allowed us to test potential causal inferences regarding the impact of partner caregiving on subsequent loneliness and depressive symptoms.
However, several potential limitations have been identified. Firstly, caregiving was based on a self-reported measure, and no consideration was given to the intensity of care provided or the duration of the caregiving role (due to sample size limitations). Moreover, our measurement of caregiving did not allow variations in caregiving intensity or transitions in/out of a caregiving role, which previous studies have identified as important for mental health outcomes [Reference Seltzer and Li35]. By not considering the potential transitions in caring roles may have introduced some bias into our findings. However, we assumed that once an individual becomes a carer for a partner with dementia, their role as caregiver is likely to continue for some time (either until the partner dies, or becomes institutionalized). Furthermore, we assumed that even if caregivers transitioned out of the role between waves 3 and 5, the influence on their mental health would be expected to continue to some degree. This would be in line with the relational deprivation hypothesis, which suggests that it is partly the meaning attributed to the caregiving role (i.e., that it acts as a kind of loss of the partner once known) that mediates depressive symptoms (rather than solely the requirements of the role itself).
Secondly, it is also worth noting that although dementia diagnoses were made by a physician, it was still a self-reported physician-based diagnosis reported by either the participant themselves or their carers. This, however, may raise some questions around the reliability of the diagnosis for these analyses, although it is unlikely that such reports will be false positives. In fact, it is estimated that dementia remains undetected in almost 30–50% of primary care patients in the UK [Reference Connolly, Gaehl, Martin, Morris and Purandare36]. Furthermore, it is possible that care-recipients relevant to the “functional impairments” category had dementia during the exposure period but had not yet received a diagnosis by a physician. This may have attenuated differences between each group.
Thirdly, we had no means of knowing whether caregivers were receiving psychological support and the number of individuals with dementia was small, both of which could have affected the results. Similarly, excluding participants with missing data could have diluted the reported effect sizes. For example, based on their characteristics (see “Results” section), excluded participants might be more at risk of depressive symptoms compared to those without missing data. While the reasons for attrition among ELSA participants have been previously explored, it is unclear whether the caregiving role had any influence on this attrition, and what the impact on the results was [Reference Seltzer and Li35].
Fourthly, to maximize the use of available data, our measurement of caregiving captured caring roles at either wave 3, 4, or 5. We took this approach because if an individual entered a caregiving role at waves 4 or 5, we wanted to avoid classifying them as “Not caring” based on wave 3 alone. As discussed above, a caregiving role at any single wave may still be associated with subsequent depressive symptoms. This measurement of caregiving across multiple waves introduced a further limitation whereby for a small minority (less than 5% of the analytical sample) caregiving status and covariates were measured at different waves. However, for most of our covariates with the exception of age, we did not expect a real change over time.
Finally, although we found evidence of an indirect effect of dementia caregiving on depressive symptoms via loneliness, it was unclear whether it was due to the caregiving itself or the death of the care-recipient, for example. Having said that, the specific causes of loneliness are likely to vary between individuals, and this would be explored as part of any therapeutic intervention.
Conclusion
Our findings indicate that partner dementia caregiving is indirectly associated with depressive symptoms via feelings of loneliness. The mental health of dementia caregivers is arguably an essential psychiatric priority, given that it could seriously influence the quality of care provided to their partner and thus impact the rate of care-recipient institutionalization [Reference Ask, Langballe, Holmen, Selbæk, Saltvedt and Tambs33,Reference Coehlo, Hooker and Bowman37].
Acknowledgments
The English Longitudinal Study of Aging is funded by the National Institute on Aging (Grant RO1AG017644) and by a consortium of UK government departments coordinated by the Economic and Social Research Council (ESRC) and the National Institute for Health Research. The English Longitudinal Study of Aging (ELSA) was developed by a team of researchers based at University College London, the Institute for Fiscal Studies and the National Centre for Social Research. The views expressed are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Financial Support
D.C. is funded by the National Institute on Aging (grant RO1AG017644) and ESRC (grants ES/T012091/1 & ES/S013830/1). E.C. is funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, and King’s College London. The views expressed are those of the authors and not of the funding agencies.
Conflict of Interest
On behalf of all co-authors, we have no conflict of interest to declare.
Supplementary Materials
To view supplementary material for this article, please visit http://dx.doi.org/10.1192/j.eurpsy.2021.20.
Data Availability Statement
The ELSA data containing the individual items and the derived scores have been made available via UK Data Service (http://www.esds.ac.uk/longitudinal/access/elsa), and the study number is 5050 (http://doi.org/10.5255/UKDA-SN-8502-2).








Comments
No Comments have been published for this article.