Introduction
Warfarin has been used in the paediatric population since the 1960s. There has been an increase in its use for paediatric cardiac interventions due to advancements in surgical palliation of the univentricular heart, increasing use of mechanical heart valves in childhood/adolescence, and rising prevalence of giant aneurysms secondary to Kawasaki disease. Reference Jain and Vaidyanathan1 The anticoagulant effect of warfarin occurs through its inhibition of the vitamin K epoxide reductase complex in the liver, resulting in impaired coagulant effect of vitamin K-dependent coagulation factors II, VII, IX, and X . Reference Ansell, Hirsh and Hylek2 Due to its narrow therapeutic index, patients on warfarin require frequent drug monitoring through measurement of the international normalised ratio. Labile international normalised ratio values and difficulty achieving a stable international normalised ratio is of particular relevance in paediatric cardiology practice as there is evidence that uncontrolled warfarin therapy is associated with an increased risk of thromboembolic events in children post-Fontan palliation. Reference McCrindle, Manlhiot and Cochrane3 In children, developing systems of metabolism and haemostasis as well as factors including age, body weight, variations in diet, frequent childhood illnesses, and drug interactions contribute to the difficulty in maintaining patients within a target international normalised ratio range. In general, the target international normalised ratio range for paediatric cardiac indications in 2.0–3.0 with the exception of mechanical heart valves which have a higher target of 2.5–3.5. Reference Giglia, Massicotte and Tweddell4 A prospective study of 319 patients found that for those with a target international normalised ratio of 2.0–3.0 and 2.5–3.5 the percentage time in target range (%ITR) was 47 and 61%, respectively. Reference Streif, Andrew and Marzinotto5 Due to the inherent challenges associated with warfarin’s use, strategies for improving time in target range such as predicative models for dosing which include pharmacogenomic data are under evaluation. Reference Hamberg, Friberg and Hanséus6– Reference Al-Metwali, Rivers and Goodyer8 The complexity and interplay of numerous contributing factors in the prediction of warfarin dosage makes the utilisation of artificial intelligence an exciting prospect in this area. There are examples of machine learning models and artificial neural networks to predict warfarin dosing in the literature, and this may play an important role in warfarin usage in the future. Reference Sharabiani, Bress, Douzali and Darabi9,Reference Grossi, Podda and Pugliano10 However, a systematic review of warfarin dosing algorithms demonstrated that most algorithms developed have not been externally validated or assessed for clinical utility. Furthermore, algorithms designed for use in paediatrics made up only 3% of the total algorithms included in the study. Reference Asiimwe, Zhang, Osanlou, Jorgensen and Pirmohamed11
Additionally, the investigation of alternatives to warfarin continues with the ongoing comparison of aspirin versus warfarin in certain indications such as patients post-Fontan palliation, and there is emerging evidence for the use of direct oral anticoagulants for paediatric cardiac indications with the recent publication of a number of randomised clinical trials and a meta-analysis of the studies to date. Reference McCrindle, Michelson and Van Bergen12– Reference Van den Eynde, Possner and Alahdab16
Our study aimed to retrospectively review warfarin management in our centre through evaluation of the indications for warfarin use, international normalised ratio levels, and percentage of time in the desired range (%ITR), as well as the frequency of phlebotomy or point-of-care international normalised ratio monitoring. We planned to use these data for planning of quality improvement initiatives and for optimisation of our anticoagulation programme.
Methods
Paediatric cardiology patients on warfarin therapy telephone international normalised ratio level results to the cardiology department in Children’s Health Ireland (CHI) at Crumlin, the national paediatric cardiology centre for Ireland, for advice regarding dose adjustments. We identified patients undergoing warfarin therapy based on all those who called with an international normalised ratio level over a four-week period. We then excluded patients who were within four weeks of initiating warfarin.
The indication for warfarin in each instance was obtained from the patient’s medical record. International normalised ratio values were reviewed retrospectively by accessing patient specific excel sheets which contained international normalised ratio values from the beginning of their treatment. The first four weeks of treatment were excluded while patients were being established on warfarin. We assessed the target ranges used and calculated the median international normalised ratio values by indication. Warfarin control was assessed by calculating the percentage time in international normalised ratio range (%ITR), as well as the percentage times above and below target. These results were displayed as the median %ITR for all patients and sub-divided by indication. We also used patient records to establish the median frequency of phlebotomy by indication and the proportion of patients using home point-of-care international normalised ratio monitoring. In our cohort of Fontan patients, specifically we established if warfarin therapy had continued long term or discontinued after a period of time. In those who had warfarin discontinued, we calculated the median time to discontinuation. Ethical approval was waived by the Children’s Health Ireland at Crumlin Ethics Committee (CHI/22.10.22).
Results
Indications for warfarin use
A total of 26 patients were included in our study. The most common indication for warfarin therapy was in patients post-total cavo-pulmonary connection (n = 19). The remaining indications were mechanical mitral valve (n = 2), mechanical aortic valve, paediatric inflammatory multi-system syndrome temporally associated with COVID-19 (PIMS-TS), Kawasaki disease with giant coronary aneurysm, cerebrovascular accident post-bidirectional Glenn procedure, and early valve dysfunction post-percutaneous pulmonary valve replacement as shown in Figure 1.

Figure 1. Indications for warfarin use.
Target international normalised ratio range and median international normalised ratio value by indication
The results are displayed in Figure 2. In our centre, there is no published institutional guideline for management of anticoagulation. The target ranges used may vary based on the primary clinician as well as other risk factors for thromboembolic events. In the patients post-total cavo-pulmonary connection, generally two target ranges were used (1.8–2.5 and 2.0–3.0). Notably, those in the 2.0–3.0 group had a higher median international normalised ratio of 2.37 versus a median of 2.21 for the lower target range.
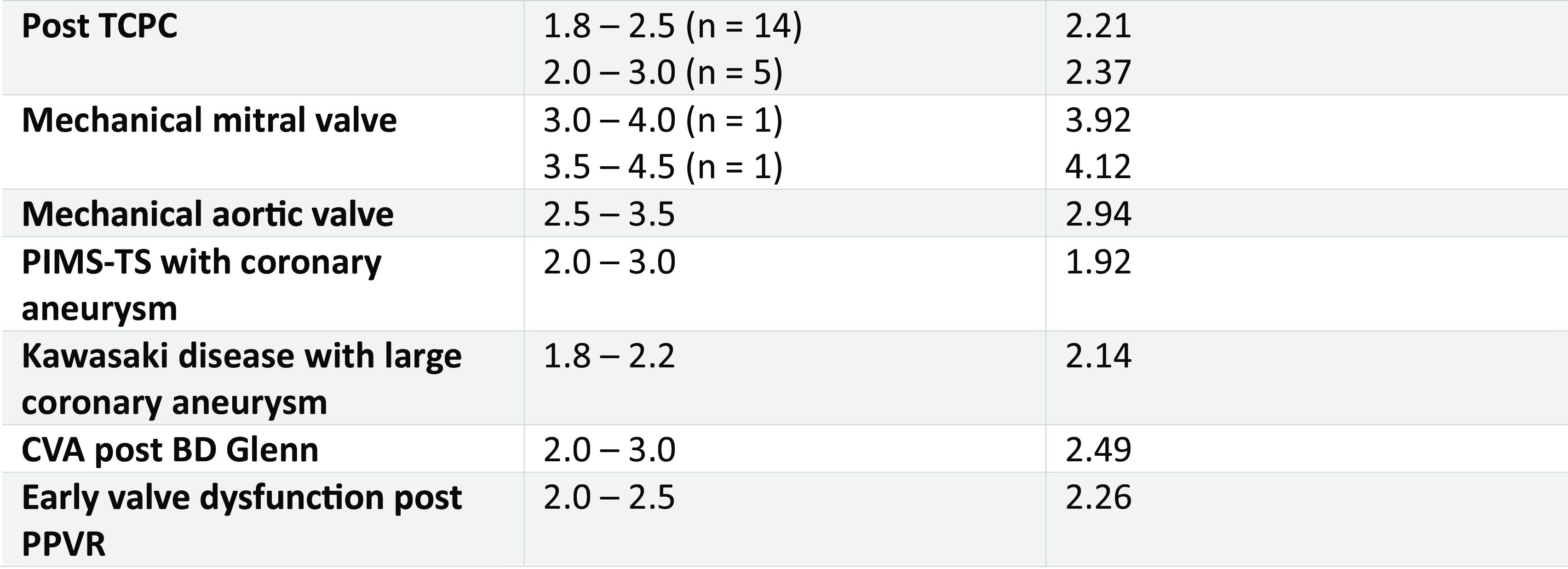
Figure 2. Target international normalised ratio ranges used and median international normalised ratio by indication.
Percentage time in target, above target, and below target range
The %ITR for the entire cohort was 55.4%, with a range between individual patients of 29.7–86.4%. In the post-total cavo-pulmonary connection group, a value of 60 %ITR was noted, although there was a wide range between individual patients (29.7–86.4). Particular note was made of the time under range in the higher risk patients with mechanical valves in situ with the total %ITR in these patients being below 45.6%. The remainder of the results are shown in Figure 3.

Figure 3. %ITR, % under, and % over target range.
Frequency of phlebotomy and point-of-care international normalised ratio
Warfarin therapy in our cohort necessitated frequent drug monitoring as detailed in Figure 4. The patients underwent monitoring once every 10 days either through formal phlebotomy in the hospital setting or through home point-of-care international normalised ratio monitoring. This number varied between individual patients and based on indication. Seventy-three per cent of the patients included had used home point-of-care international normalised ratio monitoring during their treatment on warfarin.

Figure 4. Frequency of phlebotomy.
Duration of warfarin in post-total cavo-pulmonary connection patients
Of the 19 patients post-total cavo-pulmonary connection who were included, 15 had their warfarin discontinued in follow-up. The median time to discontinuation was 11.1 months. Eight patients had their warfarin discontinued within 6–12 months, 6 patients between 12 and 18 months, and 1 patient after more than 18 months. Four patients continued on warfarin for various indications. One patient had an extracardiac conduit placed at the time of the Glenn procedure which was subsequently perforated percutaneously for a Fontan completion, the patient remained on warfarin for the duration of the conduit being in situ and post-percutaneous Fontan completion. One patient was commenced on warfarin post-Glenn due to reduced ventricular function and an increased risk of thrombosis, and this was continued post-Fontan completion. Two patients remained on warfarin post-Fontan due to a patent conduit fenestration.
Discussion
This study of the warfarin data in our national centre shows results for time in target range similar to previous published data. Reference Streif, Andrew and Marzinotto5 The aim of our study was to audit our own centres practice with the aim of instituting quality improvement initiatives for improving overall warfarin management. Particular note was made of the time in range for the patients with mechanical valves in situ with values below target range of 22.5 and 32.2% for mitral and aortic mechanical valves, respectively. The time under range for these patients was of particular concern due to their high risk of thrombosis. While there is no specific guideline for the anticoagulation used in patients post-Fontan palliation in Childrens Health Ireland, generally warfarin therapy is continued for the six months post-operatively where the risk of thromboembolic events is highest. Reference McCrindle, Manlhiot and Cochrane3 After this six-month window, there is a consideration of switching to aspirin monotherapy. In this study, the average time before switching from warfarin to aspirin was 11.1 months. While there is a general consideration at six months post-op to switch to aspirin monotherapy, an individualised approach to anticoagulation in patients post-total cavo-pulmonary connection is necessary with those at higher risk of thrombosis often remaining on longer-term anticoagulation as seen in the patient examples above. Therefore, this potential need for long-term anticoagulation in high-risk patients further emphasises the need to optimise warfarin management or to consider direct oral anticoagulants as an alternative as further evidence emerges as discussed in a recent expert analysis detailing and anticoagulation algorithm for patients post-Fontan. Reference Alsaied T, Van den Eynde and Kreutzer17 The number of international normalised ratio test was high in our study, at a rate of one test every 10 days, as seen in previous studies in the paediatric population. Warfarin use necessitates frequent episodes of phlebotomy for drug monitoring ranging from 1.8 to 8.1 tests per month depending on the age of the patient with younger patients generally requiring more frequent testing. Reference Streif, Andrew and Marzinotto5,Reference Newall, Savoia, Campbell and Monagle18 This was replicated in our study with blood tests being carried out every 8–14 days depending on indication. A method of decreasing the burden of drug monitoring is home international normalised ratio measurement, and 73% of our patients had used the international normalised ratio CoaguChek system. Point-of-care self-testing at home has previously been shown to be safe and efficacious while also positively impacting patient quality of life. Reference Jones, McLoughlin, Piovesan, Savoia, Monagle and Newall19 There is also evidence that robust patient and parent education and empowerment in warfarin self-management can be safe and increase time in therapeutic range. Reference Bauman, Black and Bauman20,Reference Jones, Hislop and Gilmore21 As a consequence of this research, we intend establishing an anticoagulation clinic directed by consistent practitioners with a special interest in anticoagulation. This could include strong patient/parental education with emphasis of patient self-testing and potentially self-management. We plan to develop an updated anticoagulation guideline with specific focus on warfarin adjustment for practitioners and staff education prior to re-examining the data. Additionally, data from this study have been part of a move to the development of a guideline for the use of rivaroxaban in patients post-total cavo-pulmonary connection in our centre which will be introduced in the near future. Ideally, prospective data collection following changes in practice will be carried out in order to assess the impact of these changes in the clinical setting.
This study again highlighted the challenges in maintaining children on warfarin within a therapeutic window. The recent expansion of the use of direct oral anticoagulants in the paediatric population offers an interesting alternative to warfarin use in children. Advantages of direct oral anticoagulants include rapid onset of action, no drug monitoring, fewer drug/food interactions, and oral fixed dosing which can lead to improved patient adherence with the medication. Reference Betensky, Monagle, Male and Goldenberg22 It should be noted that the studies on direct oral anticoagulants demonstrated practicality and safety of use in children but were not designed or powered to show superiority or even non-inferiority. This highlights the significant challenge in carrying out studies investigating prevention of thromboembolism in children due to the underlying rarity of the event. Reference Choueiter23 Therefore, it is essential that data from real-world registries and post-marketing surveillance are used to validate what has been shown in the direct oral anticoagulant clinical trials. Three randomised controlled trials have studied the use of direct oral anticoagulants as prophylaxis in paediatric cardiac patients; UNIVERSE (Rivaraxoban versus aspirin post-Fontan procedure), Reference McCrindle, Michelson and Van Bergen12 ENNOBLE-ATE (Edoxaban versus standard of care), Reference Portman, Jacobs and Newburger13 and SAXOPHONE (Apixaban versus standard of care) Reference Payne, Burns and Glatz14 and a recent systematic review and meta-analysis Reference Giossi, Menichelli and D’Amico24 of randomised controlled trials assessing the safety and efficacy of direct oral anticoagulants in children included these three trials as well as three trials investigating the use of direct oral anticoagulants for the treatment of venous thromboembolism and one trial of primary prophylaxis in children with haematological malignancy. Reference Halton, Brandão and Luciani15,Reference Male, Lensing and Palumbo25– Reference O’Brien, Rodriguez and Lew27 Across the cardiac prophylaxis trials, there were a total of 471 patients. No deaths were reported, and there was a non-significant decrease in thromboembolic events. With regard to safety outcomes, there was a non-significant or no obvious difference noted in major bleeding events, clinically relevant non-major bleeding events, any bleeding, and serious adverse events. There was a non-significant increase in discontinuation of medication in the direct oral anticoagulant group versus standard of care. Overall, the impression derived from this study was that direct oral anticoagulants appear to be at least comparable to Standard of care prophylaxis in children with cardiac disease and that this are warranted further study. Reference Giossi, Menichelli and D’Amico24 An example of real-world use of apixaban in paediatric cardiac patients was shown in a large retrospective single-centre study which described their experience with apixaban use both for prophylaxis and treatment of thromboembolism in paediatric cardiac patients. This study included 219 patients who received apixaban for various indications, including cardiomyopathy, CHD, including single- and two-ventricle circulations, Kawasaki disease, and others. 172 (79%) required prophylaxis and 47 (21%) required treatment for thromboembolic events. Initial dosing was empiric based on the patient’s weight and underlying indication for anticoagulation. Using an in-house assay peak apixaban levels were obtained in this study, and dosing was adjusted in 25 % of the patients following measurement of apixaban levels. In the prophylaxis group, no patients on apixaban has symptoms of or evidence radiographically of new thrombosis and while the numbers were small in the group treated for thrombosis there was a high rate of clot resolution noted. In this large group of complex and heterogeneous patients, it was demonstrated that apixaban use was feasible with a low rate of major and clinically relevant bleeding events. Reference VanderPluym, Esteso and Ankola28
Some clinicians would argue that the requirement of drug monitoring may have its advantages. It is a useful way of assessing compliance in patients and highlighting higher risk patients who may need closer follow-up. However, previous studies have shown that compliance with warfarin can be as low as 41%. Reference Monagle, Cochrane and Roberts29 The compliance rates of the direct oral anticoagulants in their respective clinical trials were significantly higher with those on Edoxaban having rates of 94%, although this may not reflect real-world compliance rates as this number fell to 55% in the study’s extension period. Reference Portman, Jacobs and Newburger13 Furthermore, monitoring in a patient on warfarin with a raised international normalised ratio identifies those at high risk of haemorrhagic complications, and there is a readily available treatment method in the form of vitamin K. It is difficult to predict who will bleed on direct oral anticoagulants treatment, and reversal agents are less readily available. Reference Mullen30 Pharmacokinetic and pharmacodynamic data from the direct oral anticoagulants clinical trials have shown that weight-based adjusted dosing leads to drug levels similar to those seen in adults and that drug monitoring is generally not required in the majority of children receiving direct oral anticoagulants. Reference Betensky, Monagle, Male and Goldenberg22 Interestingly, in the study carried out by VanderPluym et al., peak apixaban levels were measured in order to dose-adjust based on whether the required level was for prophylaxis or treatment of venous thromboembolism and this has become their standard of practice. Reference VanderPluym, Esteso and Ankola28 While further extrapolation of what is the correct or safe level based on weight, age, and indication is required, this does offer a potential solution for clinicians who are reluctant to forego monitoring of drug levels which has been the standard in antithrombosis management for years.
While the data provided from these studies are highly valuable, there are many questions which remain to be answered regarding optimal anticoagulation management in children. In cardiac patients, what is the optimal time to stop anticoagulation prior to procedures? When to use reversal agents? Is usage safe in certain populations who were excluded from the studies, that is, premature infants, those at high risk of bleeding, those with renal/liver dysfunction? Who would benefit from drug monitoring and what is the optimal therapeutic range? Does the use of direct oral anticoagulants improve medication adherence or quality of life? Does the use of direct oral anticoagulants impact longer-term outcomes such as growth or neurodevelopment? Reference Betensky, Monagle, Male and Goldenberg22 These questions among many others may be challenging to answer but data from cohort studies, registries, and real-world data will be vital in furthering the already significant progress that has been made in paediatric thrombosis research.
The study was limited due to overall low numbers of patients on warfarin at the time of auditing and by the fact that the data collection was retrospective. This was a single-centre study and should be representative of the Irish population as children on warfarin for cardiac indications are managed through our centre in Children’s Health Ireland. However, we would ideally carry out a multi-centre study in the future to increase our numbers and widen the indications for warfarin use in the cohort. The method of patient inclusion was done over a four-week period, and only those patients who called our centre for warfarin dosing management during this period were included. As most patients have dose adjustments in this time period, we felt most patients would be captured. However, patients who were very stable on warfarin who had longer intervals between phlebotomy may not have been included. There were low numbers by certain indications with most of the patients in the cohort being post-total cavo-pulmonary connection. For example, only one patient with Kawasaki disease was included during the data collection period which would be unusual in our centre. In a paper on the Irish experience with Kawasaki disease, 32 patients were identified in a four-year period and 15 (47%) of whom had abnormalities on echocardiogram during the acute phase of illness. While all but one of these patients was managed with aspirin, there were very few patients identified treated with warfarin during this period. Reference Flinn, Gavin, McMahon, Oslizok and Disease31 Additionally, our data collection was carried out during the COVID-19 pandemic where the incidence of Kawasaki disease was shown to have declined. Reference Burney, Roberts and DeHaan32
We opted to use the simplest method of measuring time in range, that is, the %ITR which is the proportion of international normalised ratio levels which fall within the desired target range. Alternate methods of measurements include the percentage time within therapeutic range (%TTR) which uses a statistical method called linear interpolation to calculate the percentage time in target range. Reference Rosendaal, Cannegieter, van der Meer and Briët33 This method accounts for time in between international normalised ratio measurements by allocating an international normalised ratio value to each day which is likely to decrease the effect of temporary frequent measurements of international normalised ratio on the long-term anticoagulation control. A study comparing the two methods of measurement for a discrepancy between them showed the %ITR method possibly underestimating the quality of anticoagulation control in children. Reference Biss, Avery, Walsh and Kamali34 However, the authors did note limitations to the linear interpolation method and could not recommend one measure over the other due to the lack of knowledge regarding the impact of these measurements on actual clinical outcomes. Important further research would be examining the methods of assessing control by correlation with clinical outcomes, that is, thromboembolic or bleeding events.
In conclusion, this study of warfarin management in our national centre highlights the challenges of anticoagulation with warfarin in the paediatric population. While recent data show promise in alternative anticoagulant therapies for children with cardiac indications, there is a key role for warfarin use going forward, especially in the management of patients with mechanical valves where there is no evidence for the use of direct oral anticoagulants. Therefore, optimisation of warfarin management through clinical interventions such as specialist anticoagulation clinics with parental education and empowerment will be crucial. Additionally, research into dosing and monitoring optimisation such as dosing algorithms may offer an opportunity to further enhance our management of this high-risk patient group.
Acknowledgements
None
Financial support
None
Competing interests
None







