The assertion that British psychiatry faces an identity crisis and a devaluation of medical expertise Reference Craddock, Antebi, Attenburrow, Bailey, Carson and Cowen1 has prompted wide discussion about the future of the profession. Reference Bullmore, Fletcher and Jones2-Reference Oyebode and Humphreys4 However, a solution capable of addressing the complex and wide-ranging issues involved seems elusive. What is clear is that the next generation of psychiatrists need to be strong medical leaders and pioneers for change that results in better patient care. In order to achieve this, it is necessary to consider whether postgraduate training in psychiatry is capable of shaping the psychiatrists of the future and what changes need to be put in place to achieve this.
Changes to postgraduate medical education
Current attention on the future of postgraduate medical education make it timely to consider what reforms could be beneficial to psychiatry specifically. Postgraduate medical training has undergone a significant period of change over the past 5 years under the Modernising Medical Careers (MMC) programme (www.mmc.nhs.uk) and is likely to undergo further change under the Shape of Training review. Reference Moore5 The current structure and delivery of postgraduate training in psychiatry is summarised in Fig. 1.

Fig 1 Current structure and delivery of postgraduate training in psychiatry.
FY1, foundation year 1; CT1, core trainee year 1; ST4, specialty trainee year 4; CASC, Clinical Assessment of Skills and Competencies.
Government proposals for changes in postgraduate medical training have recently been outlined in an initial White Paper and subsequent policy accompanying the health bill. 6,7 Under new arrangements, postgraduate training of doctors, as well as all other health professionals, will be administered by Local Education and Training Boards (LETBs), with national oversight being provided by the newly formed Health Education England (HEE). Health Education England will replace Medical Education England (MEE), which is the independent advisory non-departmental body set up following Sir John Tooke's inquiry into MMC. Reference Tooke8 Health Education England will provide national leadership and oversight as well as being responsible for the allocation of education and training resources. 7,9 It should be noted that the HEE arrangements will apply only in England and not in the devolved administrations of the UK, although HEE state that because education and training issues operate within a UK-wide context they will build strong relationships with partners in Scotland, Wales and Northern Ireland to ensure consistency and coherence. 9
The future picture is likely to be one of greater involvement of provider organisations (namely National Health Service (NHS) trusts and other organisations delivering healthcare) in the commissioning and provision of postgraduate training under the new LETB/HEE arrangements; with postgraduate medical education and training becoming more closely aligned with the training of other healthcare professionals. The risks are plain. Trusts and healthcare providers may have little incentive to commission the appropriate number of psychiatrists and may opt for the training of other cadres of staff instead. Indeed, it is probable that trusts may wish to influence the content and structure of training without reference to the long-term needs of patients with mental illness in the light of the scientific literature.
It has recently been suggested that postgraduate medical education in England should be more closely linked to universities Reference Ovseiko and Buchan10 and under new arrangements universities are likely to play an increasingly important role through representation on the LETBs. This move would be welcome, as it will reinforce the role of universities in both undergraduate and postgraduate medicine. This may result in better access to research opportunities, and the chance to tailor training programmes to local research and service needs. Although variation in training programmes can be problematic if certain experiences are not available to obtain core clinical competencies, variation could also allow promotion of excellence and innovation by allowing universities to offer unique training opportunities in their own areas of particular expertise.
The present apparent disinterest of most universities in the clinical practice of medicine in the UK in favour of the basic sciences is problematic. The design of psychiatry residency programmes in North America is in stark contrast to this, where a very large number of these programmes are run by medical schools in conjunction with regional healthcare providers. As a result there is greater variability in the nature of residency programmes, however, opportunities for participation in research and the rapid implementation of research evidence into clinical practice are likely to be greater. Interestingly, the national accreditation body for North American residency programmes, the Accreditation Council for Graduate Medical Education, is moving towards a competency-based model of training for residents, which will set out ‘milestones’ that will need to be reached by certain points of the programme. This is not dissimilar to what is expected of UK trainees, and may go some way to reducing the variability of the North American programmes.
Reaffirming our ideals
The role of the Royal Colleges in postgraduate medical education is likely to evolve given the extent of the changes described above. The Royal College of Psychiatrists will need to pay close attention to the development of future education and training delivery arrangements in order to ensure that the training ideals of the profession are safeguarded for the future generation of psychiatrists and their patients. There is already a danger that long-held ideals of postgraduate education in psychiatry have been side-lined by recent pressing needs of implementing MMC, and may now again come under threat in the light of further likely reform. It has been argued that past changes, including the introduction of workplace-based assessments, have led to a damaging preoccupation with competence rather than expertise or excellence. Reference Oyebode11 As emphasised in Tooke's dissection of MMC, it is imperative to aspire to excellence Reference Tooke8 and not have a culture of merely accepting satisfactoriness. To cultivate trainees who pursue excellence and who are not simply preoccupied with ticking boxes, it is of course necessary to have training schemes delivered by trainers who also aspire to excellence. To be a supervisor is a privilege, not a right, for those who are appropriately trained and work within a robust quality assurance system. The General Medical Council (GMC) has recently consulted on suggestions for the approval and recognition of specialty trainers to bring these arrangements in line with those for general practice, where trainers already require specific GMC approval. 12
Suggested changes to psychiatric training
It has been suggested that the psychiatrists of the future should develop expertise in the management of physical illnesses that are so commonly comorbid with psychiatric disorder and decrease life expectancy, with benefits both for patients and the medical image of the specialty. Reference Craddock, Antebi, Attenburrow, Bailey, Carson and Cowen1 We believe the importance of the relationship between mental illnesses and physical illnesses has been overlooked in the development of psychiatric training in the UK. Several European countries have placements in general medicine or neurology available as part of their postgraduate training in psychiatry. Reference Oakley and Malik13 There is a particular need for an excellent mutual understanding between the disciplines of psychiatry and neurology, with several common core clinical competencies but also differing skills that can be shared. We propose that, in the first year of training, a 4-month placement in neurology becomes an integral part of core training in psychiatry, in order to consolidate clinical examination skills and provide experience in the interface between neurological and psychiatric disorders. In addition, advanced training should routinely include medical placements in paediatrics for child and adolescent psychiatrists and elderly medicine for old age psychiatrists.
It has been argued that there is no psychiatry without psychopharmacology and that the considerable benefit patients can derive from medication cannot be maximised safely without more thorough training in psychopharmacology than is suggested by its one mention in the curriculum. Reference Harrison, Baldwin, Barnes, Burns, Ebmeier and Ferrier3 We entirely support the argument made in that paper for greater prominence of psychopharmacology in psychiatric training and do not repeat it here, Reference Harrison, Baldwin, Barnes, Burns, Ebmeier and Ferrier3 other than to emphasise that these skills are absolutely core to the psychiatrist's role as a medical doctor. There has been considerable focus in recent years on the lack of availability of psychotherapy experience for all trainees Reference Denman14-Reference Siddiquee and Qaadir16 and although we whole-heartedly support the need for all psychiatrists to learn essential psychotherapeutic skills, it is time the same attention is given to providing structured training in the breadth of psychopharmacology rather than learning prescribing by the apprenticeship model. We propose that all training schemes have at least one joint psychiatry and clinical pharmacology placement, which trainees can rotate into during core training. Such a placement could be run jointly between a clinical pharmacologist and a psychiatrist with an interest in clinical psychopharmacology. A proposed pilot involves a trainee spending 3 days a week in clinical pharmacology attending ward rounds, clinics, drug and therapeutics committees, reviewing and auditing the use of treatments in particular areas of practice and conducting a relevant systematic review or meta-analysis. The 2 days working in psychiatry includes attendance at National Institute for Health and Clinical Excellence (NICE) technology appraisal meetings, clinics dealing with complex cases and offering second opinions.
Recent years have seen the degradation of three particular aspects of training: emergency psychiatry, breadth of experience and opportunities for research. First, a combination of New Ways of Working, the European Working Time Directive and NHS financial pressures have led to concerns about the quantity and quality of trainees’ exposure to the acute emergencies that occur out of hours and the unique training opportunities they present. 17 Indeed, one study highlighted the reduction in the number of emergency assessments conducted by trainees in psychiatry since the introduction of a primarily nurse-led home treatment team. Reference Waddell and Crawford18 The College guide to specialist training in psychiatry contains a clear statement about core trainees’ participation on a first on-call rota, with acute management plans conceived and implemented for a range of conditions - unfortunately no such guidance for advanced trainees remains, with only a vague statement that emergency psychiatry is important. 19 It is essential that trainees have exposure to a range of emergency assessments and are properly supervised to conduct risk assessments and implement appropriate management plans; this is critical to learning to manage complexity and becoming a consultant who supervises others doing such assessments. Training programmes must ensure this experience is available, despite potential financial disincentives for mental health trusts.
Second, in considering the breadth of training experience available, the principle that placements reflect the trainees’ learning needs and are not driven by service need is crucial. Concerns have previously been expressed about the implementation of service changes without consideration of the effect on training Reference Malik, White, Mitchell, Henderson and Oakley20 and this has led to a lack of breadth of experience on offer in placements in training programmes. Reference Oyebode and Humphreys4 With ‘functionalisation’ of provision of general adult psychiatry it is possible for trainees to have very little exposure to in-patient treatment. In order to achieve a well-rounded training experience it is critical to carefully consider the skills the trainee needs to obtain and how different placements may deliver these.
Third, valuing research and using evidence have been identified as core attributes of a psychiatrist, with it being considered extremely important that psychiatrists are involved in high-quality research into the causation and treatment of mental illness. Reference Craddock, Kerr and Thapar21 Concerns have been expressed that changes to the structure of training following MMC have made it more difficult for trainees to undertake research. Reference Jauhar22 A lack of flexibility in the current training system and difficulties matching clinical training in psychiatric specialties with academic training structures have led to concerns about training the academic psychiatrists of the future. Reference Garralda23 However, although the limited evidence indicates that undertaking research as a psychiatric trainee predicts pursuing an academic career, it has also been emphasised that such experience is also invaluable for those pursuing a clinical career. Reference Fogel24 Therefore, it is necessary to promote the flexibility needed to allow trainees to undertake research and ensure access to research supervisors for trainees in training programmes distant from academic psychiatry departments.
The role of leadership and management experience within psychiatric training has received increasing attention over recent years, and rightly so. This has recently culminated in the establishment of the Faculty of Medical Leadership and Management. Development of the Medical Leadership and Competency Framework 25 by the Academy of Medical Royal Colleges and the NHS Institute for Innovation and Improvement and its subsequent incorporation into the Royal College of Psychiatrists’ curriculum has formalised this aspect of postgraduate training. Any new postgraduate training structure would need to take this into account and provide appropriate opportunities. In particular, there is a need for good careers advice and support throughout training so that trainees are signposted at an early stage to the myriad of opportunities now available to them within this field.
Quality of training
There has long been a tension between service provision and training, with discussions about how much of their time trainees should be providing service to the NHS and how much time they should be training, and indeed under what circumstances service provision constitutes training. Too great an emphasis on service provision can compromise training, with the long-term effect of compromising the quality of future service provision due to inadequately trained consultants. Recent suggestions to reduce the total number of medical training posts, with a reduction in hospital-based doctors and an increase in community-based doctors, include discussions about whether the consultant workforce of the future will be delivering more of the service, partly driven by the fact that there will be fewer trainees to provide such service. 26 One possible benefit of universities becoming more involved in postgraduate training, as discussed above, is that they are independent of the NHS and can help safeguard the quality, depth and breadth of training that can sometimes be adversely effected by service pressures.
Current arrangements see the Royal College of Psychiatrists devising the curriculum and competencies, for approval by the GMC, with these being enforced by the deaneries via the process of trainees’ Annual Review of Competency Progression (ARCP). The quality control of training programmes, previously monitored by external College visits, has been taken on by the deaneries via their own internal inspection processes. The national GMC survey does provide a formalised way for trainees to raise concerns about training programmes and following consultation this has been developed over the past year to improve the quality of data and speed of reporting. The current reorganisation of delivery of postgraduate training offers an opportunity to introduce a more robust system of quality control. Curricula should be more powerful in terms of providing a means for the quality control of training programmes; if competencies as outlined by a robust curriculum cannot be obtained within a training programme, this should be a lever for its improvement. By being explicit in the requirements for broad experience, out-of-hours experience and participation in research, a curriculum that has its delivery as a quality metric could safeguard the experiences essential for training.
Recommendations
Our recommendations to enhance the structure of post-graduate training in psychiatry are illustrated in Fig. 2. They should be underpinned by the principles of a focus on excellence and expertise, more opportunities for research and better access to emergency psychiatry experience. Implementation of these recommendations will involve some changes by those planning the curriculum and training at the College and a commitment to these ideals by those delivering training on the ground. To achieve the appropriate breadth of experience, including neurology and psychopharmacology placements as outlined earlier, core training should be extended to 4 years. This will allow a full range of placements to be undertaken as shown in Fig. 2 and ensure thorough experience of the full range of psychiatric presentations. Although longer core training would be unique among medical specialties, a total length of psychiatry training of 7 years would be comparable to postgraduate training in medical and surgical specialties. Alternatively, there are also ways in which the experience we propose could be incorporated instead into an extended advanced training and a debate about such issues would be welcomed.
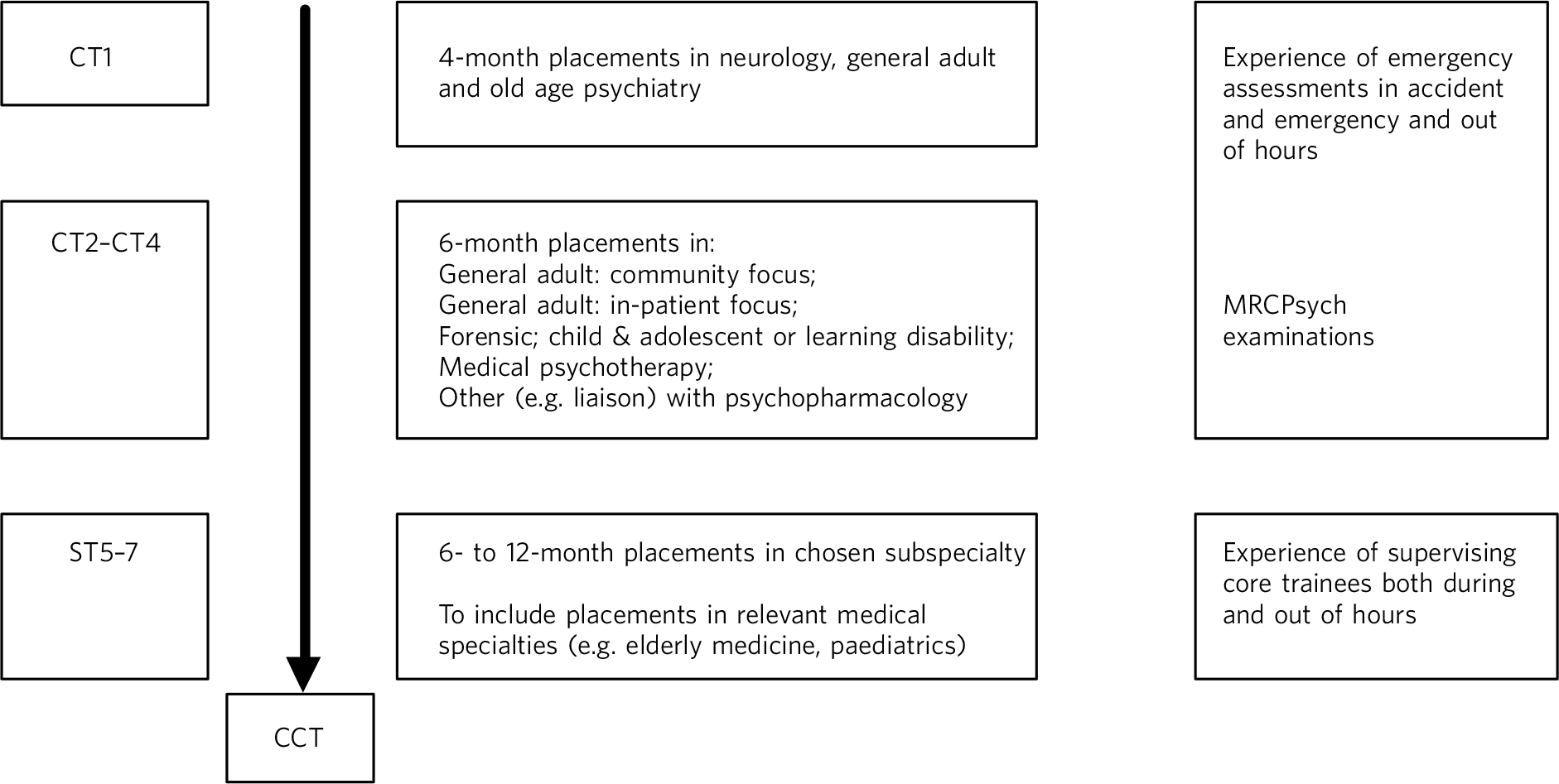
Fig 2 Proposed structure of postgraduate training in psychiatry.
CT1, core trainee year1; ST5, specialty trainee year 5.
Adopting these recommendations may have further benefits for future generations by means of a potential impact on recruitment to the specialty, which continues to be of concern for the profession and is the focus of a 5-year strategy for the College. 27 Strengthening research training may assist in combating the perceived lack of scientific rigour that it has been suggested reduces enthusiasm among medical students for choosing a career in psychiatry. Reference Curtis-Barton and Eagles28 The difficulty of functionalised or specialised training placements is mirrored in undergraduate experience, being exacerbated by the short time the students are exposed to psychiatry, potentially giving them a very narrow view of the specialty. Finally, more explicit links with, and placements in, medical specialties may begin to address the perception that psychiatry is very distant from the rest of medicine and reduce the stigma from other doctors that has been identified as such a barrier to recruitment into psychiatry. Reference Curtis-Barton and Eagles28-Reference Korszun, Dharmaindra, Koravangattu and Bhui30
We recognise that our proposals present significant practical challenges that would need to be overcome, for example the presence of both 4- and 6-month placements during core training would necessitate a change from the current norm where training posts may variously be used as core trainee year 1 (CT1) or CT2, or even CT3 placements depending on circumstances. It would be necessary to designate some placements as being specifically for CT1 trainees and hence of 4, rather than 6, months’ duration. However, we would argue that deciding which posts are most suitable for the learning needs of trainees at different years of training and structuring the rotation of trainees in this way has its advantages. We seek to present our vision of the future of psychiatric training and suggest that these aspirations and ideals should drive the development of training, while accepting that a pragmatic compromise may be the result.
Acknowledgements
We are grateful to Dr Sheldon Benjamin for his perspective on the North American training system.





eLetters
No eLetters have been published for this article.