Covid-19 in South Africa
The first case of COVID-19 in Africa was reported in Egypt on February 14, 2020, 1 followed by the first case in South Africa (SA) on March 5, 2020. 2 After the World Health Organization (WHO) declared the Coronavirus disease 2019 (COVID-19) a pandemic, SA implemented a nationwide 21- day lockdown at the end of March 2020, which was later extended. This period marked a significant shift in healthcare systems globally. This was achieved by lockdown strategies and de-escalation of routine healthcare services. This included postponing clinic visits for chronic diseases and elective surgical procedures. Other mitigation strategies included telephonic medical consultations; provision of set appointment times; and convincing patients with non-urgent concerns not to visit healthcare facilities. Reference Vallabhjee, Gibson and Davies3 The pandemic was characterized by a rise and fall pattern in the number of confirmed cases over time, colloquially referred to as the “waves” of the pandemic.
Laboratory medicine plays an integral role in the screening, diagnosis, and monitoring of non-communicable diseases (NCD), and reportedly, up to 70% of clinical decisions are based on laboratory results. Reference Forsman4 Glycated hemoglobin (HbA1c) measurement is recommended in international and local guidelines for the screening, diagnosis, and monitoring of diabetes mellitus. 5,6 The diagnosis and management of dyslipidemia is based on lipid profile results; consisting of total cholesterol, triglycerides, low-density lipoprotein, and high-density lipoprotein. Thyroid-stimulating hormone (TSH), free thyroxine, and free triiodothyronine (fT3) are used to assist with the diagnosis of various thyroid disease states and to evaluate response to treatment. Reference Kahaly, Bartalena and Hegedüs7 Serum Protein Electrophoresis (SPE) and Serum Free Light Chains (SFLC) are laboratory tests essential in the diagnosis of monoclonal gammopathies and to assess response to therapy, Reference Fazel8,Reference Rajkumar9 while prostate specific antigen (PSA) is useful in the screening, risk stratification, and monitoring of patient response to the treatment of prostate cancer. Reference Duffy10
A laboratory-based study illustrated an objective decline in the number of requests for several analytes received at a tertiary hospital in South Africa (SA). Reference Kruger, Banderker and Erasmus11 However, this study only analyzed data during the initial months of the pandemic and was limited to a single center. The aim of this study was to determine the impact of the COVID-19 pandemic on laboratory requests for tests used in the routine care of patients with various NCD at multiple outpatient departments (OPDs) and primary healthcare facilities (PHF) across SA.
Methods
Study Design
This national, multicenter, retrospective descriptive audit collected data on laboratory requests used for the diagnosis, and monitoring of NCD received from OPDs, and PHF across SA. OPDs, located in secondary and tertiary hospitals, provide medical services to patients who do not require hospital admission. In contrast, PHFs serve as the initial level of healthcare services for ambulatory patients and are an integral component of primary healthcare. Serious or complex health conditions may be further referred to secondary or tertiary care, and patients are downreferred to primary care for ongoing management once their conditions are stable.
Eight testing panels namely: HbA1c, lipid profile, TSH, and fT4, as well as fT3, SPE, SFLC, and PSA were used as a proxy for the screening, diagnosis, and monitoring of the following NCDs: diabetes mellitus, dyslipidemia, thyroid disease, and monoclonal gammopathies, as well as prostate cancer. Monoclonal gammopathies and prostate cancer were included since SPE, SFLC, and PSA are established tumor markers for these conditions in a laboratory-based screening approach. In SA, prostate cancer accounts for 22% of all new cancers in males and has an age-standardized rate (ASR) of 39.46 per 100 000. In contrast, the ASR for multiple myeloma is 1.03 per 100 000 for males and 0.7 per 100 000 for females. 12
The study included test requests from January 1, 2017 to December 31, 2021. Test requests from the immediate pre-pandemic period (January 2019 – February 2020) were used as a baseline and were compared to test requests during the pandemic period (March 2020 – December 2021). To ensure that any observed changes from the 2019 baseline were not caused by random variation, an average baseline was calculated from the 3-year pre-pandemic period (January 2017 – December 2019). The pandemic period was subdivided into wave 1 (April – June 2020) (W1); wave 2 (December 2020 – February 2021) (W2); and wave 3 (June – September 2021) (W3). The average test request volume for each wave (calculated by dividing the sum of the requests received during the wave by the duration of the wave in months) was calculated to compare the impact during each wave. The region and site of facility (rural or urban) was also noted.
Data was collected from Chemical Pathology Laboratories within the National Health Laboratory Service (NHLS) across SA. The NHLS is a public health laboratory service, serving approximately 80% of the South African population. 13 According to the organizational structure of the NHLS, the 9 provinces of SA are merged into 6 service regions and include the Eastern Cape (EC); Free State and North-West (FS&NW); Gauteng (GP); KwaZulu Natal (KZN); Limpopo and Mpumalanga (LP & MP); Western Cape and Northern Cape (WC & NC).
Statistical Analysis
Stata release 14 (Stata Corp., College Station, Texas, USA) was used to analyze data and Excel (Office 365; Microsoft, Redmond, Washington, USA) was used to construct graphs. Requests for HbA1c; lipid profiles; TSH, fT4 and fT3; SPE and SFLC; PSA were grouped per month, year, region, and site of specimen collection. The number of requests during 2017, 2018, and 2019 were compared to the number of requests during the pandemic (W1, W2, W3). The percentage difference in requests for all analytes was calculated for each month of 2020 – 2021 and for W1 – W3, then compared to 2019. The average of 3 years (2017 – 2019) of pre-pandemic data was used as a comparator for pandemic data, to ensure that the baseline values were not influenced by chance occurrences.
Ethical Considerations
This study was approved by the Faculty of Medicine and Health Science Ethics committee at Stellenbosch University. Research was conducted according to the Declaration of Helsinki (2013). A waiver of informed consent was obtained for retrospective data collection.
Results
In 2020, the NHLS received 3 281 939 requests for the analytes of interest (HbA1c; lipid profiles; TSH, fT4 and fT3; SPE and SFLC; PSA); 2 728 120 of the requests were received from OPD and PHF, 9% less than in 2019. In 2021 the request volume surpassed both 2019 and 2020; request volumes increased by 11% compared to 2019, and 22% compared to 2020. The regions that made the biggest contribution towards the request volumes were GP (30%), KZN (25%) and WC & NC (19%). The WC & NC region observed the largest reduction in request volumes from 2019 to 2020 (− 20%), while the FS & NW region experienced the smallest reduction (−1%) (Table 1).
Table 1. The number of requests received from each region from 2019 to 2021

NHLS, National health laboratory service; GP, Gauteng; KZN, KwaZulu Natal; WC, Western Cape; NC, Northern Cape; FS, Free State; NW, North-West; EC, Eastern Cape; LP, Limpopo; MP, Mpumalanga.
* Average baseline: (2017 + 2018 + 2019)/3.
The decrease in request volumes during 2020 occurred from April to July, compared to the same period in 2019. The largest reduction was seen during April, when all tests except PSA, had a 30% or greater reduction in volumes. The tests with the biggest reduction were SPE (−45%), fT4 (− 42%), TSH (− 39%), and HbA1c (− 36%). Although the volumes were reduced from May – June 2020 compared to 2019, it was to a lesser degree than during April 2020; most tests had a reduction of less than 30%, except for SPE (− 36%) and TSH (− 30%). In July 2020 the decrease in volumes was like those observed in April 2020; SPE (−39%), TSH and PSA (− 31%), and fT4 (− 30%) had the largest reductions (Figure 1).

Figure 1. Number of requests received for each analyte from 2019 – 2021.
Dashed lines represent the 3 waves of the pandemic. (A) illustrates high volume tests, (B) illustrates low volume tests. W1 = wave 1; W2 = wave 2; W3 = wave 3. HbA1c = Glycated hemoglobin; TSH = Thyroid-stimulating hormone; fT4 = free thyroxine; fT3 = free triiodothyronine; SPE = Serum protein electrophoresis; SFLC = serum free light chains; PSA = prostate specific antigen.
During W1, all analytes showed a decrease in request volumes compared to the same period in 2019 (Table 2). In W2, the reduction in request volumes persisted but to a lesser degree than W1; the only test that did not decrease in volume was SFLC. In W3, there was an increase above the baseline in request volumes for all tests, except SPE that showed a 13% reduction.
Table 2. Requests for each test received during wave 1, wave 2, and wave 3

HbA1c, Glycated hemoglobin; TSH, Thyroid-stimulating hormone; fT4, free thyroxine; fT3, free triiodothyronine; SPE, Serum protein electrophoresis; SFLC, serum free light chains; PSA, prostate specific antigen.
Overall, the percentage difference in request volumes from urban facilities reflected the total OPD and PHF numbers, while the request volumes from rural facilities did not change to the same degree, apart from PSA and fT3 (Table 3). These observed differences were not consistent throughout the 3 waves, with W1 demonstrating the most substantial variations (Figure 2).
Table 3. Differences in request volumes in urban and rural facilities
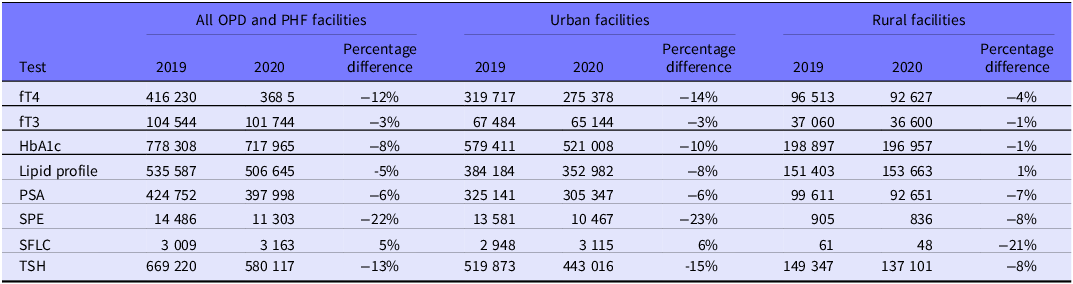
HbA1c, Glycated hemoglobin; TSH, Thyroid-stimulating hormone; fT4, free thyroxine; fT3, free triiodothyronine; SPE, Serum protein electrophoresis; SFLC, serum free light chains; PSA, prostate specific antigen.

Figure 2. Comparison of percentage differences in the high volume laboratory tests between urban and rural facilities.
HbA1c = Glycated hemoglobin; TSH = Thyroid-stimulating hormone; fT4 = free thyroxine; fT3 = free triiodothyronine; PSA = prostate specific antigen.
Discussion
This national laboratory-based study investigated the impact of the COVID-19 pandemic and lockdown measures on the routine care of patients in SA with NCD’s, namely diabetes mellitus, dyslipidemia, and thyroid disease, as well as monoclonal gammopathies, and prostate cancer. The laboratory tests routinely requested for the management of these conditions were used as a proxy for patient management in OPDs and PHF. We noted a significant reduction in test request volumes during 2020, with request volumes from urban facilities showing a greater decrease than rural facilities. This reduction was more noticeable during April and July 2020. In 2021, the test request volumes increased above the 2019 baseline.
Over the last decade, SA has seen an increase in the prevalence of NCDs. In 2019, ischemic heart disease, stroke, and diabetes were amongst the top 5 causes of death in the adult South African population. 14 Screening programs to ensure early detection and regular follow-up of confirmed cases are essential in the management of NCDs. Reference Bigna and Noubiap15 The South African national government implemented a rigid lockdown regimen in response to the WHO declaration. During the initial lockdown period, routine healthcare services were de-escalated, and included the postponement of clinic visits for chronic diseases. Reference Vallabhjee, Gibson and Davies3 To ensure continued treatment for NCDs, home delivery of medication (HDM) was introduced for patients on chronic medication with repeat prescriptions. Reference Vallabhjee, Gibson and Davies3 David et al. Reference David, Bresick and Moodaley16 investigated the potential benefit of HDM services on a cohort of patients with DM from a PHF in Cape Town. They studied a group of 461 DM patients returning to PHC after the first wave of the pandemic; 331 (72%) received HDM. The follow-up HbA1c results in both the HDM and non- HDM groups increased on return to the PHC, however the observed increase in HbA1c was smaller in the HDM group when compared to the non-HDM group. This illustrates the positive contribution that HDM made towards improved glycemic control, and strengthens the argument made by Low that medication should be delivered to patients unable to visit pharmacies due to lockdown measures. Reference Low and Yap-Tan17 In addition to the re-organization of healthcare services, provision of NCD care was further limited by the perception of community members that healthcare workers were carriers of COVID-19, leading to violence against healthcare workers in certain communities. Reference Delobelle, Abbas and Datay18
A survey conducted in May 2020 by the WHO in 155 countries (unspecified) reported that 49% of participants experienced a disruption in the management of diabetes. 19 Our group saw a significant reduction (− 36%) in HbA1c requests in April 2020, however it was less than that of the United Kingdom where a reduction of 80% was observed, Reference Holland, Heald and Stedman20 and in North America where request volumes decreased by 70%. Reference Sharma, Greene and Chambliss21
PSA is used as a screening test for prostate cancer. During W1, PSA requests dropped by 18% when compared to 2019. Van Wyk et al. examined the number of histopathology specimens that were received from April to June 2020 at an anatomical pathology laboratory in the Western Cape. They reported that the number of new prostate cancer diagnoses made in their laboratory decreased by 58%. Reference Van Wyk, De Jager and Razack22 The sample collection for a PSA test is less invasive and specialized than the collection of histopathology samples, and this could possibly account for the differences observed between the studies.
Pillay et al. analyzed data from routine primary healthcare services across SA during May – December 2020, compared to 2019. They reported that all provinces experienced a decrease in the number of visits to primary healthcare facilities in 2020, with the WC having the largest decline (− 30%) in visits and the FS the smallest decline (− 8.7%). Reference Pillay, Pienaar and Barron23 This is in keeping with our findings that the WC & NC region had a 20% decrease in test request volumes, and the FS & NW had a 1% decrease; this possibly reflects the de-escalation of routine healthcare services, which included postponing clinic visits for chronic diseases and elective surgical procedures. This disruption of medical services might have contributed towards the increase in natural deaths that was observed between May and June, 2020. During this time, the South African Medical Research Council reported that there were 28 329 more deaths compared to the same period in earlier years, of which 7 527 were confirmed COVID-19 cases. 24 The re-organization of healthcare services and the resulting lack of patient follow-up could have contributed to the excess of non-COVID-19 deaths. While it is possible that unconfirmed cases of COVID-19 may have played a role, our primary concern centers on the impact of healthcare service disruptions.
At the end of W1, routine medical services were re-escalated, and as the pandemic progressed, adjustments were made primarily in response to the number of confirmed cases and the corresponding lockdown levels. These adjustments included permitting patient visits to healthcare facilities when lockdown levels allowed. Reference Vallabhjee, Gibson and Davies3 This could explain the smaller decrease in request volumes during W2. During W2, we found that request volumes for 7 of the included analytes decreased compared to 2019, although to a lesser degree. A study in South Korea compared the number of visits at Internal Medicine departments and found the decrease in visits were more significant during the earlier months of the pandemic, but returned to baseline during subsequent waves. Reference Byun, Kang and Go25 In the study by Sharma et al., the HbA1c request volumes from 11 institutions across the United States and Canada, decreased during March – May 2020 compared to 2019, and returned to baseline in June 2020. Reference Sharma, Greene and Chambliss21 Lum et al. reviewed cancer cases from a large cancer registry in the United States. They compared the number of new cancer diagnoses made in 2020 to the case number in 2019. They report a 14% reduction in new cancer diagnoses from March to May 2020, with a partial recovery in June 2020, but it remained lower than in previous years. Reference Lum, Browner and Palis26 Unexpectedly, we saw that W3 test request volumes for all testing panels, apart from SPE, surpassed the volumes of 2019. This increase coincides with the roll out of COVID-19 vaccines to the South African public; the peak of vaccine administration was reached at the end of August 2021. 27 The rise in testing demand may have been influenced by the relaxation of stringent lockdown measures and the re-opening of healthcare facilities.
The movement of people between provinces and regions after the implementation of the lockdown could account for the difference in the percentage decrease in request volumes between rural and urban facilities. A social impact survey conducted by Stats SA (Stats SA, Pretoria, South Africa) reported that 6% of respondents, who were mostly from Gauteng, Western Cape, and Eastern Cape, moved between provinces after the announcement of the national lockdown; 25% stated that the reason for moving was to be closer to family. 28 This suggests that during W1, some individuals may have returned to their rural hometowns, potentially contributing to the greater reduction in request volumes observed in urban areas. Subsequently, it is possible that these individuals returned to the urban areas after W1, which could have influenced the observed patterns.
This study distinguishes itself with its exceptional scale and comprehensive approach, encompassing both a global and local (sub-Saharan Africa) perspective. It involves an exhaustive examination of national data collated from a multitude of laboratories dispersed across various strata of public healthcare. To secure a robust baseline, 3 years of pre-pandemic data (2017 - 2019) were utilized, thus minimizing the probability of skewness induced by stochastic events. Substantial studies have been undertaken in Europe, the United States and Asia, but the distinctiveness of this research arises from its concerted effort to elucidate the impact of COVID-19 on Sub-Saharan Africa; an area that has remained relatively understudied. Consequently, this research contributes essential perspectives regarding the repercussions of pandemics on the healthcare systems within developing nations, thereby qualifying it as one of the most substantial studies conducted on a global scale.
Limitations
Despite its profound scope, the research methodology did not incorporate data on population differences or a review of clinical files, instead relying exclusively on laboratory tests as indicators for disease screening, and diagnosis, as well as clinical care monitoring. Although sub-dividing laboratory requests into first-time and follow-up categories would enhance the accuracy of our analysis regarding the pandemic’s impact on distinct patient groups, regulatory restrictions in SA prevent access to patient identifiers, rendering this approach unfeasible. The potential for increased dependence on point-of-care devices during the pandemic and lockdown periods, which fall outside the recording capabilities of the laboratory information system, is also acknowledged as a potential variable not accounted for. Furthermore, the merging of provinces into regions could conceal diverging trends over time between amalgamated provinces. It should be acknowledged that our assessment of the potential impact of healthcare service re-organization and the associated lack of patient follow-up on the excess of non-COVID-19 deaths remains speculative, as precise quantification of these effects is challenging. This study did not account for potential variation in the rates of NCDs over time, which could be influenced by factors such as changes in demography, social determinants of health, and the impact of COVID-19 infection itself. Yet, the study’s size reinforces its position as a significant milestone within the global scientific community’s ongoing discourse on healthcare dynamics during pandemics.
Conclusion
The findings of this study are inescapable: the COVID-19 pandemic had a significant impact on the South African population receiving care in public healthcare facilities. While some countries resorted to telemedicine to ensure uninterrupted care, it may not be a viable solution in resource-limited settings due to challenges such as smartphone access, connectivity issues, data costs, and communication barriers. These findings will be used to model the impact of the pandemic on such settings and provide recommendations for more effective responses in future pandemics or other emergencies. It remains to be seen how the pandemic affected individual patient care. Nonetheless, these results shed light on the crucial need to find innovative solutions to mitigate the impact of pandemics on healthcare systems, especially in developing countries.
Acknowledgement
We acknowledge NHLS for assisting with data collection.
Author contribution
Conceptualization (ECK, AEZ); Data collection (ECK, DJW); Data analysis (ECK, DJW); Graph/ table construction (ECK, DJ); Assessment of findings (DJW, APK, RTE, AEZ); Literature review (ECK, DJ, NM, UN); Original draft writing (ECK, RBB); Final draft writing (ECK, DJW, RBB, DJ, NM, UN); Proofreading prior to submission (RTE, APK, AEZ).
Abbreviations
WHO, World Health Organization; COVID-19, Coronavirus disease 2019; NCD, Non-communicable disease; HbA1c, glycated hemoglobin; TSH, Thyroid-stimulating hormone; fT4, Free thyroxine; fT3, Free triiodothyronine; SPE, Serum protein electrophoresis; SFLC, Serum free light chains; PSA, Prostate specific antigen (PSA); SA, South Africa; OPD, Outpatient departments; PHF, Primary healthcare facilities; NHLS, National Health Laboratory Service; EC, Eastern Cape; FS, Free State; NW, North West; GP, Gauteng; KZN, KwaZulu Natal; LP, Limpopo; MP, Mpumalanga; WC, Western Cape; NC, Northern Cape
Competing interests
None.







