Recent studies from various countries have indicated that patients with substance use disorder have a greater risk of suicidal ideation and suicide attempts compared with the general population.Reference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 Alcohol use disorder was found to be associated with a tenfold increase in risk of dying by suicide in a meta-analysis of 42 different cohort studies; those who injected drugs were about 14 times more likely to complete suicide.Reference Wilcox, Conner and Caine2 Moreover, 58% of those with polysubstance dependence report suicide attempts.Reference Landheim, Bakken and Vaglum3 A study in Spain among patients who sought treatment for substance use disorder reported that the lifetime suicidal ideation rate was 43.7% and the lifetime suicide attempt rate was 17.7%, with 1 month prevalence of 8.7% and 1.5% for suicide attempt and ideation, respectively.Reference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 The prevalence of suicidal ideation and attempt have also been reported by studies in different countries; for instance, 21% in Turkey for suicidal attempts,Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 34% and 13% in Australia for lifetime and recently attempted suicide among patients with heroin dependence,Reference Darke, Ross, Lynskey and Teesson5 44.7% for suicidal ideation and 26.8% for suicide attempts in the past 6 months in China,Reference Gu, Lau, Li, Li, Gao and Feng6 6.3% for suicidal ideation and 2.1% for suicide attempt in MoroccoReference Agoub, Moussaoui and Kadri7 and 20% for suicidal ideation over the past month in Kenya.Reference Ongeri, McCulloch, Neylan, Bukusi, Macfarlane and Othieno8 The prevalence of suicidal ideation and attempts in Ethiopia has been reported among individuals with various diagnoses of mental disorders; 23.3% of those with a diagnosis of major depression, 23.8% of those diagnosed with bipolar disorder and 13.1% of those diagnosed with schizophrenia had made a suicide attempt.Reference Shibre, Hanlon, Medhin, Alem, Kebede and Teferra9 In another study from Ethiopia among adult psychiatric out-patients, rates of 64.8% and 19.2% for suicidal ideation and attempt were reported, respectively.Reference Mekonnen and Kebede10 There were multiple risk factors for suicidal ideation and attempt in patients with substance use disorders, including beginning use of a substance at a younger age, being female, being less educated, unemployment, and having a diagnosis of depression, bipolar disorder, anxiety or polysubstance use.Reference Darke, Ross, Lynskey and Teesson5,Reference Arias, Miller, Camargo, Sullivan, Goldstein and Allen11–Reference Miller, Borges, Orozco, Mukamal, Rimm and Benjet13 No published research in Ethiopia has yet examined the prevalence of suicidal ideation and suicidal attempts and the associated risk factors among substance use disorder patients. This study aimed to fill this gap.
Method
Study design and setting
We followed the methods of Molla et al (2019).Reference Molla, Mengesha, Derajew and Kerebih14 A cross-sectional study was conducted on patients with substance use disorder who visited the out-patient department of any of three public hospitals (Saint Amanuel Mental Specialised Hospital, Saint Paul's Millennium Medical College and Zewditu Memorial Hospital) in Addis Ababa, Ethiopia, from 5 May to 13 June 2019. Saint Amanuel Mental Specialised Hospital is the only mental health hospital in the country. The hospital has 300 beds, of which 14 are for substance use disorder patients. Saint Paul's Millennium Medical College provides psychiatry services and has 15 beds for substance use disorder patients. Zewuditu Hospital provides psychiatry services and has substance use disorder out-patient and in-patient services with five beds.
Sample size determination and patient selection procedure
The total number of participants needed to conduct this study was calculated using a single population proportion formula with the following considerations: a standard normal distribution (z = 1.96) with 95% confidence interval (α = 0.05) and P = 50% (0.5), since there has been no study of the prevalence of suicidal ideation and attempt specifically in this population. The absolute precision or tolerable margin of error (d) was taken to be 5%. Ten per cent for non-respondents was added, bringing the total sample size to 423. Study participants from each hospital were allocated proportionally.
A systematic sampling technique was applied to select 423 patients with substance use disorders. The sampling interval (k) was calculated by dividing the total study population during the 1 month data collection period by the total sample size: k = N / n = 890 / 423 = 2.1. Therefore, participants were selected from patients every two intervals. The first study subject was selected by a lottery method from the first two participants. All patients with substance use disorder attending the out-patient department in the addiction psychiatry unit during the study period were included in the study. Those who were severely ill and difficult to interview were excluded from the study if they were not suitable owing to illness or if it was considered not to be in their best interests to participate.
Outcome variables and independent variables
The outcome variables were suicidal ideation and attempt, assessed using the suicidality module of the World Mental Health Survey Initiative version of the World Health Organization's Composite International Diagnostic Interview (CIDI). There is a version of this assessment tool in the Amharic language, which has been validated for use in Ethiopia in both clinical and community settings.Reference Rashid, Kebede and Alem15,Reference Gelaye, Williams, Lemma, Deyessa, Bahretibeb and Shibre16
The study questionnaire had five components. Sociodemographic characteristics were collected using structured questions, clinical factors were collected using semi-structured questions, and substance-related factors were collected using substance-related questions. Social support was assessed using the Oslo three-item social support scale (Oslo-3). The total score on the Oslo-3 ranges from 3 to 14, indicating poor support (score of 3–8), moderate support (score of 9–11) or strong support (score of 12–14).Reference Dalgard, Dowrick, Lehtinen, Vazquez-Barquero, Casey and Wilkinson17 Perceived stigma was assessed using the four-point Substance Abuse Perceived Stigma Scale (SAPSS). This is a 12-item Likert scale (strongly disagree, disagree, agree, strongly agree) that assesses the construct of perceived stigma.Reference Luoma, Twohig, Waltz, Hayes, Roget and Padilla18
Operational definition
Substance use disorder
Substance use disorder is the diagnostic term applied to specific substance misuse (e.g. alcohol use disorder or opioid use disorder) that results from the prolonged use of a substance, with a maladaptive pattern of substance use leading to clinically significant impairment or distress occurring within 12 months.Reference Sadock, Sadock and Ruiz19
Suicidal ideation
The respondents who answered ‘yes’ to the question ‘have you seriously thought about committing suicide within the past 1 year’ were considered to have suicidal ideation according to the suicidality module of CIDI.Reference Kessler and Üstün20
Suicidal attempt
The respondents who answered ‘yes’ to the question ‘have you attempted suicide within the past 1 year’ were considered to have had a suicide attempt according to the suicidality module of CIDI.Reference Kessler and Üstün20
Social support
The Oslo-3 social support scale was used to assess whether the participant had poor, moderate or strong support.Reference Dalgard, Dowrick, Lehtinen, Vazquez-Barquero, Casey and Wilkinson17
Perceived stigma
Participants who scored less than or equal to the mean (≤24) on the 12-item SAPSS were considered to have perceived stigma related to substance misuse.Reference Luoma, Twohig, Waltz, Hayes, Roget and Padilla18
Chronic medical illness
A participant was considered to have chronic physical illness if such an illness had previously been diagnosed and was currently being followed up.
Past and current mental illness
We noted previously and currently diagnosed mental illness and past and current treatment.
Consent statement
Written informed consent was obtained from all participants.
Data collection procedure
Data were collected by face-to-face interviews using the Amharic version of a pre-tested questionnaire and by reviewing the patient chart. The data was collected by three BSc psychiatry nurses who were supervised by two MSc mental health professionals. The supervisors and the data collectors were assigned to health institutions daily.
Two-day training for data collectors and supervisors was completed to ensure a common understanding of the interview questions. Ethical concerns that might be encountered during data collection, were discussed with the data collectors and supervisors. Pre-testing was conducted on 5%Reference Garlow, Purselle and D'Orio21 of the sample population at Eka-Kotebe General Hospital before the actual data collection to identify potential problems in using the data collection tools and to check the consistency of the data collectors. Data collected for the pre-test were not included in the analysis of the main study. Regular supervision was given by the supervisors and principal investigator to ensure that all necessary data were properly collected.
Ethical statement
The authors assert that all procedures contributing to this work complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects or patients were approved by the joint ethical review committee of the University of Gondar and Saint Amanuel Mental Specialised Hospital (reference UOG/AH/2365).
Data processing and analysis
The collected data were checked for completeness and consistency and coded. The coded data were entered into a computer using EPI data version 3.1 and imported to SPSS for Windows version 20. Descriptive statistics (frequency, percentage and mean) were computed and presented using tables. Bivariate logistic analysis was performed to identify the variables associated with suicidal ideation. Variables with P < 0.2 in the logistic regression analysis were entered into the multivariable analysis to identify independent correlates of suicidal ideation. The Hosmer–Lemeshow test was used to determine the goodness of fit of the model. P-values less than 0.05 were considered to indicate statistical significance, and point estimates are presented with their respective 95% confidence intervals.
Results
Sociodemographic characteristics of the respondents
Of the total 423 patients, 408 participants were assessed and included in the analysis. The median age of participants was 31 years (interquartile range (IQR): 25–38), with age ranging from 18 to 70 years. The majority of the participants were males (352, 86.3%), 286 (70.1%) were single, 170 (41.7%) had completed high school education and 164 (40.2%) were unemployed (Table 1).
Table 1 Distribution of participants by sociodemographic factors (N = 408)
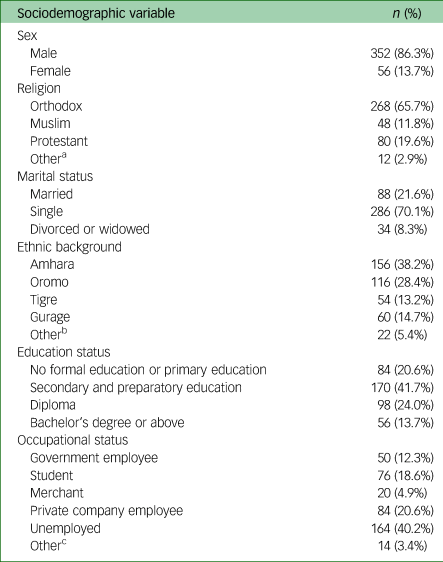
a. Adventist or no religion.
b. Hadiya, Hadere, Welelle or Argoba.
c. Housewife, farmer or daily labourer.
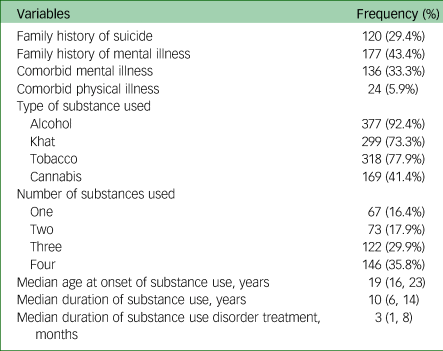
Clinical and substance-use-related factors of the respondents
The majority of participants used alcohol 377 (92.4%), and 16.4%, 17.9%, 29.9% and 35.8% of respondents used one, two, three and four types of substance, respectively; 136 (33.3%) of participants had a comorbid mental illness. The median (IQR) age of onset of substance use was 19 (16–23) years, and the duration of substance use was 10 (6–14) years. Of the total participants, 120 (29.4%) had a family history of suicide (Table 2).
Table 2 Description of clinical and substance-related factors (N = 408)
Psychosocial factors
One-fifth of participants (20.10%) reported that they were getting strong support, and half (206, 50.5%) reported poor social support. The remaining 29.40% received moderate social support. More than half of the respondents (230, 56.37%) reported substance-related perceived self-stigma.
Prevalence of suicidal ideation and attempt among patients with substance use disorder
Nearly half (198, 48.5%) of the respondents reported that they had experienced suicidal ideation at least once in their lifetime; 170 (85.85%) of these were men. Suicidal ideation in the past 12 months was reported by 39.5% of the participants; 83.85% of these were men.
A total of 118 (28.9%) respondents disclosed that they had attempted suicide at least once in their lifetime; 92.4% said they had planned an attempt. Nearly one in five patients (76, 18.6%) reported that they had attempted suicide in the past 12 months. Of the participants who had ever attempted suicide, 32(27.1%), 61(51.7%) and 25 (21.2%) of had attempted suicide once, twice and three or more times, respectively. The most commonly used method was reported to be hanging (65, 55.1%), followed by poisoning (32, 27.1%), and some participants had used more than one methods. The two most frequently mentioned major reasons for suicide attempt were family conflict (35, 29.7%) and poverty (27, 22.9%) (Table 3).
Table 3 Distribution of suicidal ideation and attempt (N = 408)

a. Hopelessness or no reason.
Factors associated with suicidal ideation among patients with substance use disorder
The categorical variables (family history of suicide, family history of mental illness, comorbid mental illness, poor social support, perceived stigma related to substance misuse, alcohol use, khat use, tobacco use, cannabis use and multiple substance use) and continuous variables (age, age at onset of substance use, duration of substance use and duration of treatment) had P-values less than 0.2 for association with suicidal ideation in the bivariate analysis and were included in the subsequent multivariate analysis. In the multivariate analysis, family history of mental illness, comorbid mental illness, perceived stigma related to substance misuse and alcohol use had statistically significant associations with suicidal ideation.
Participants who had family history of mental illness had a nearly four times higher risk of having suicidal ideation compared with people with no family history of mental illness (adjusted odds ratio (AOR) = 3.60, 95% CI: 2.17, 5.97). Participants with comorbid mental illness were 3.61 times more likely to have suicidal ideation compared with patients who had no comorbid mental illness (AOR = 3.61, 95% CI: 2.11, 6.16). Patients reporting perceived stigma related to substance misuse were four times more likely to have suicidal ideation compared with those reporting no such stigma (AOR = 4.00, 95% CI: 2.26, 7.07). Alcohol use had a strong association with suicidal ideation. Respondents who used alcohol had a 7.49 times higher risk for suicidal ideation compared with those who did not use alcohol (AOR = 7.49, 95% CI: 1.99, 28.19) (Table 4).
Table 4 Associations between patient factors and suicidal ideation (N = 408)

AOR, adjusted odds ratio; COR, crude odds ratio.
χ² = 3.88, d.f. = 8; Hosmer–Lemeshow test statistic, 0.86; reference value, 1.
***P < 0.001.
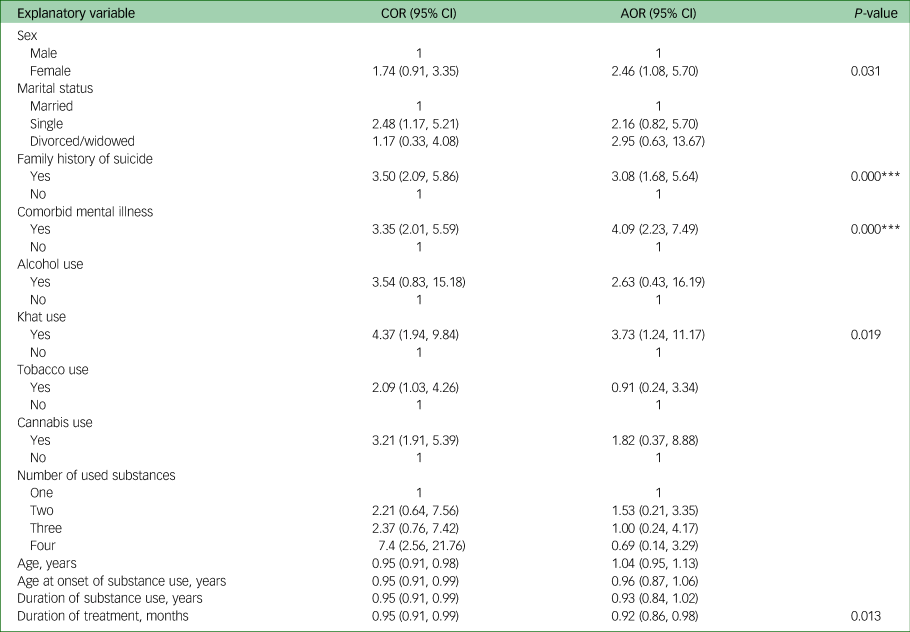
Factors associated with suicide attempt among patients with substance use disorder
The categorical variables (being female, being single, family history of suicide, comorbid mental illness, use of three of four substances, alcohol use, khat use, tobacco use and cannabis use) and continuous variables (age, age at onset of substance use, duration of substance use and duration of treatment) had P-values less than 0.2 for association with suicide attempt in the bivariate analysis. These variables fulfilled the minimum requirements for inclusion in the multivariate analysis. Being female, family history of suicide, comorbid mental illness, duration of treatment and khat use were statistically significantly associated with suicide attempt (P-value less than 0.05) in the multivariate analysis. The odds of a suicide attempt among females were 2.46 times higher compared with males (AOR = 2.46, 95% CI: 1.08, 5.70).
Patients who had a family history of suicide were 3.08 times more likely to have had a suicidal attempt compared with those who had no family history of suicide (AOR = 3.08, 95% CI: 1.68, 5.64). Participants with comorbid mental illness were 4.09 times more likely to have had a suicidal attempt compared with patients who had no comorbid mental illness (AOR = 4.09, 95% CI: 2.23, 7.49). Patients who used khat had 3.73 times higher odds of suicide attempt compared with patients who did not use khat (AOR = 3.73, 95% CI: 1.24, 11.17). For each unit (1 month) increase in duration of treatment, the odds of suicide attempt decreased by 8% (Table 5).
Table 5 Associations between patient factors and suicide attempt (N = 408)

AOR, adjusted odds ratio; COR, crude odds ratio.
χ² = 3.11, d.f. = 8; Hosmer–Lemeshow test statistic, 0.92; reference value, 1.
***P < 0.001.
Discussion
The prevalence of suicidal ideation in our study was 39.5%. Our results regarding suicidal ideation were consistent with those of studies carried out in Spain (43.7%)Reference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 and the USA (35.4%).Reference Garlow, Purselle and D'Orio21 Regarding suicidal ideation, we found a lower prevalence compared with those reported by studies carried out in China (44.7%),Reference Gu, Lau, Li, Li, Gao and Feng6 Barcelona, Spain (50%)Reference Rodríguez-Cintas, Daigre, Braquehais, Palma-Alvarez, Grau-López and Ros-Cucurull22 and Chicago, USA (67%).Reference Berman and Schwartz23 A possible reason for the discrepancy may be related to study design; the study in Spain used retrospective cohorts,Reference Rodríguez-Cintas, Daigre, Braquehais, Palma-Alvarez, Grau-López and Ros-Cucurull22 and the one in the USA was a case–control study.Reference Berman and Schwartz23 Another possible reason for the discrepancy might be differences in the number of substances included; cocaine and opiates users were also included in the study conducted in Spain.Reference Rodríguez-Cintas, Daigre, Braquehais, Palma-Alvarez, Grau-López and Ros-Cucurull22 In addition, the China study used a different sampling method (snowball), a different study population (female and sex workers) and a different sample size (200), all of which may be reasons for the discrepancy.Reference Gu, Lau, Li, Li, Gao and Feng6
Our study found a higher prevalence of suicidal ideation compared with those reported by studies in Australia (13.0%),Reference Darke, Ross, Lynskey and Teesson5 Mexico (22%), Catalonia, Spain (32.7%),Reference Arribas-Ibar, Suelves, Sanchez-Niubò, Domingo-Salvany and Brugal24 Canada (8.0%)Reference Kennedy, Marshall, Hayashi, Nguyen, Wood and Kerr25 and the USA (19.1%).Reference Wong, Zhou, Goebert and Hishinuma26 This discrepancy may have been due to differences in the type of study (a household community-based survey was conducted in Mexico) and in the study population (the USA study was among high school students).Reference Wong, Zhou, Goebert and Hishinuma26 In addition, the study from Australia involved a single-substance user, which could explain the discrepancy.Reference Darke, Ross, Lynskey and Teesson5 Furthermore, the USA study included those who had used substances at least once in their lifetime, which might be a source of discrepancy.Reference Wong, Zhou, Goebert and Hishinuma26 The prevalence of suicide attempts in our study (18.6%) was in line with those reported by studies in Turkey (21%)Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 and Spain (17.7%).Reference López-Goñi, Fernández-Montalvo, Arteaga and Haro1
Regarding factors, patients who had a family history of mental illness were more likely to have suicidal ideation than patients who had no family history of mental illness. This finding is supported by a study in Turkey.Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 This association might be because children with mentally ill parents or family members might not receive good support and may be more likely to have a history of child maltreatment. This in turn may lead to poor mental health and suicidal behavior.Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4
In this study, comorbid mental illness was found to have significant association with suicidal ideation; this is also supported by previous studies conducted in Turkey,Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 SpainReference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 and the USA.Reference Wong, Zhou, Goebert and Hishinuma26 This association might be because of some mental illnesses like depression are more likely to think about suicide.Reference Castiello d'Antonio, Sadock, Sadock and Ruiz27,Reference Bjerkeset, Romundstad and Gunnell28
Patients with perceived stigma related to substance misuse were more likely to have suicidal ideation than their counterparts. This finding is supported by previous studies done in ChinaReference Gu, Lau, Li, Li, Gao and Feng6 and New York, USA.Reference Crapanzano, Hammarlund, Ahmad, Hunsinger and Kullar29 The association might be due to patients with perceived stigma having low self-esteem, depressive symptoms, loneliness and a sense of dissatisfaction with social relationships, which heighten suicidal ideation.Reference Earnshaw, Smith, Cunningham and Copenhaver30 Alcohol use was strongly associated with suicidal ideation. Previous studies conducted in SpainReference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 and CanadaReference Kennedy, Marshall, Hayashi, Nguyen, Wood and Kerr25 reported similar findings regarding the association between alcohol use and suicidal ideation. This association might be due to the fact that alcohol use increases psychological distress and aggressive behaviour, including self-aggression, changes an individual's expectations and helps to propel or trigger suicidal ideation into action; it also constricts attention and inhibits effective coping strategies to avoid suicidal behavior.Reference Cherpitel, Borges and Wilcox31
Regarding factors associated with suicide attempt, females were more likely to experience suicide attempt than males. This finding is supported by previous studies conducted in Australia,Reference Darke, Ross, Lynskey and Teesson5 SpainReference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 and Turkey.Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 The association might be due to the fact that females are more likely to disclose their difficulties than males. This might encourage them to attempt suicide.Reference Rodríguez-Cintas, Daigre, Braquehais, Palma-Alvarez, Grau-López and Ros-Cucurull22 It might also be because females have a twofold greater risk of depression, which increases suicidal behaviour, compared with males.Reference Castiello d'Antonio, Sadock, Sadock and Ruiz27,Reference Bjerkeset, Romundstad and Gunnell28
Patients who had a family history of suicide were more likely to attempt suicide compared with their counterparts. This result is supported by a study conducted in Turkey.Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 A possible reason for this association is that individuals whose parents died by suicide might experience challenges related to child–parent separation and attachment, as well as socioeconomic insecurity, which in turn favour suicidal behavior.Reference Mikolajczak, Brianda, Avalosse and Roskam32,Reference Brodsky and Stanley33
In this study, comorbid mental illness was significantly associated with suicide attempt. This result was in line with those of previous studies conducted in the USA,Reference Wong, Zhou, Goebert and Hishinuma26 Australia,Reference Darke, Ross, Lynskey and Teesson5 SpainReference López-Goñi, Fernández-Montalvo, Arteaga and Haro1 and Turkey.Reference Guvendeger Doksat, Zahmacioglu, Ciftci Demirci, Kocaman and Erdogan4 This association might exist because individuals with certain mental illnesses (for instance, depression) are more likely to attempt suicide.Reference Castiello d'Antonio, Sadock, Sadock and Ruiz27 It could also be due to the unpleasant feelings of experiencing public stigma towards mental illness.Reference Kota, Salazar, Culbreth, Crosby and Jones34
We also found that khat chewing was associated with suicide attempt. This finding is supported a review study of the adverse effects of khat previously conducted in England, which showed suicide attempt has been reported by several authors in the context of the khat withdrawal state.Reference Cox and Rampes35 Our study result regarding khat chewing and the suicidal attempt has also been supported by another study conducted in Jimma high school students which reported as khat chewing has an association with suicidal ideation which might progress to suicidal attempt.Reference Dires, Soboka, Kerebih and Feyissa36 This might also be because of evidences indicated as there is an association between khat chewing and mental distress.Reference Damena, Mossie and Tesfaye37
Furthermore, patients with a longer duration of treatment for substance use disorder were less likely to experience suicidal attempt compared with their counterparts. This finding is supported by the results of a study conducted in Australia.Reference Darke, Ross, Lynskey and Teesson5 This association may exist because when patients receive treatment for an adequate time, they are more likely to develop the skills to cope with adverse life events. It may also be because depressive symptoms, which may increase suicidal behaviour, can be identified and treated earlier while patients are receiving treatment.Reference Cornelius, Clark, Salloum, Bukstein and Kelly38
Limitation of the study
Although this study reports important findings in the under-investigated area of suicidal ideation and attempt in Ethiopia, there were some limitations that need to be considered before generalising from the results. The first limitation is the possibility of underreporting of events, owing to the data collection method and the nature of the conditions. There may have been some recall bias as a face-to-face interview method was used. There could also have been social desirability bias, as disclosing suicide is perceived as a socially sensitive issue in the community. We recommend follow-up studies to clarify the cause–effect relationships among certain factors, including the relationships of comorbid mental illness and perceived stigma related to substance misuse with suicidal ideation and attempt. We also recommend that future studies use data collection techniques other than interview (such as self-administered or web-based questionnaires) to avoid underreporting of substances used owing to fear of legal issues.
Data availability
The data that support the findings of this study are available from the corresponding author (M.S.B.) upon reasonable request.
Acknowledgements
We thank the staff members of Amanuel Mental Specialised Hospital, St Paul's Millennium Medical College and Zewditu Memorial Hospital addiction units and study participants for their cooperation and support during data collection. We also thank Dr Gizat Molla Kassie for his unreserved support and guidance from the commencement to the reporting of this study. Finally, we thank Dr Heather Dipple from England who helped us to review the manuscript for language and grammar.
Author contributions
G.M.K. participated in formulating the research question, designing and carrying out the study, analysing the data and writing the article. Y.M.L., M.S.B., G.T.T., G.M.D., W.M.G. and M.W.B. participated in designing and carrying out the study, analysing the data and writing the article. All authors participated in the review and preparation of the manuscript. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.