1. Introduction
Bipolar disorder is a chronic illness characterised by episodes of depression and excessive elation. It represents a spectrum from mild mood episodes to severe mood disorders with psychotic symptoms. Bipolar disorder is often associated with other psychiatric disorders (e.g. substance abuse, personality disorder) or physical co-morbidities (e.g. diabetes, cardiovascular disease), and often results in poor social and physical functioning of the patients [1–Reference McIntyre, Soczynska, Beyer, Woldeyohannes, Law and Miranda3].
The lifetime prevalence of bipolar disorder is estimated to be between 1 and 6% in European countries [Reference Pini, de Queiroz, Pagnin, Pezawas, Angst and Cassano4]. Worldwide, it is one of the leading causes of disability with more years of life lost due to premature death and disability than asthma, heart attack, epilepsy and dementia [Reference Mathers, Fat and Boerma5]. People with bipolar disorder are frequent users of health and social care services. In 2007, an estimated 1.14 million people suffered from bipolar disorder in the UK [Reference McCrone, Dhanasiri, Patel, Knapp and Lawton-Smith6]. For the same year, the total societal costs of bipolar and related disorders were calculated at £ 5.2 billion with total service costs (health and social services and informal care) being £ 1.6 billion [Reference McCrone, Dhanasiri, Patel, Knapp and Lawton-Smith6]. A more recent estimate by Young et al. [Reference Young, Rigney, Shaw, Emmas and Thompson7] for the annual UK National Health Service (NHS) cost of bipolar disorder was £ 342 million at 2009/10 prices. Hospitalizations accounted for 60%, outpatient and community mental health for 26.7%, and medication in primary care for 7.4% of the overall direct costs of care [Reference Young, Rigney, Shaw, Emmas and Thompson7]. A recent review suggests that costs in the UK are comparable with other European countries: cost estimates for the USA are much more variable [Reference Kleine-Budde, Touil, Moock, Bramesfeld, Kawohl and Rössler8].
The main objectives of bipolar disorder management are stabilization of mood thereby preventing acute episodes, unwanted hospital admissions and suicides, and improving quality of life by optimising social and physical functioning. Recent guidelines [Reference Goodwin, Haddad, Ferrier, Aronson, Barnes and Cipriani9] have emphasized the potential for improving care by more expert clinical service provision. Specialist care reduced the risk of re-admission to hospital in bipolar disorder in comparison with generic care in Denmark [Reference Kessing, Hansen, Hvenegaard, Christensen, Dam and Gluud10] and this finding can probably be generalized to other developed countries. Monitoring of symptoms should be an essential component of bipolar disease management because it can track the effectiveness of interventions and facilitate early intervention when fluctuations in symptoms are identified to prevent or minimise the impact of episodes [11]. Timely access to specialist care is, however, often limited due to human, financial or geographical constraints resulting in waiting lists, suboptimal treatment and lost opportunities for early intervention or prevention.
Several attempts have been made to implement regular, remote mood monitoring for bipolar disorder to improve clinical outcomes and optimize access to specialist services at low direct intervention costs [12–Reference Saunders, Bilderbeck, Panchal, Atkinson, Geddes and Goodwin17]. However, none of the relevant studies provided information on patients’ real-world achievable compliance with monitoring or investigated the broader impact of monitoring on other costs to the mental health services. Moreover, currently there is no agreement whether remote mood monitoring increases mental health service use due to stricter follow-up or reduces service use as the consequence of less frequent visits and better health outcomes. With the growing number of such services worldwide, it is important to gain more insight into the real-life feasibility and acceptability of remote mood monitoring and to establish its likely wider economic impact on the mental health services. In order to explore these aspects and fill the relevant gaps in evidence, we conducted a retrospective cohort study of bipolar patients’ compliance with monitoring and their mental health service contacts and costs before and during their first year engagement with the True Colours monitoring system at Oxford Bipolar Disorder Research Clinic in Oxford, UK (https://truecolours.nhs.uk).
2. Methods
2.1. The True Colours system
Remote mood monitoring for adults with bipolar disorder has been successfully implemented at the Oxford Bipolar Disorder Research Clinic at the Warneford Hospital, Oxford, UK using the True Colours system since 2006. The clinic provides secondary (for referrals from central Oxford) and tertiary service for around 300 patients with bipolar disorder. The True Colours system combines simple, widely used, convenient and low cost means of communication by SMS/email/internet with sophisticated software engineering. It allows a real-time, remote monitoring of symptoms and clinical outcomes by patients self-rating their mood using validated self-report scales for depressive (the Quick Inventory of Depressive Symptomatology [QIDS-SR16]) and manic symptoms (the Altman Self-Rating Scale for Mania [ASRM]), and their communication by weekly mobile-phone text messages or email [Reference Rush, Trivedi, Ibrahim, Carmody, Arnow and Klein18,Reference Altman, Hedeker, Peterson and Davis19]. Patients using True Colours either receive and reply to two, weekly text messages separately for the monitoring of their QIDS and ASRM scores, or receive one prompting email and log in to the True Colours website via a secure link to enter their relevant scores directly. In case of no reply or faulty response, the system sends additional reminder SMS messages/emails. The chosen method of communication is the preference of the patient and can be changed. The system also produces a graph-based output in a user-friendly format accessible through the web for the patients and their clinicians/care teams, allowing them to track a patient's condition and identify early signs of relapse in a collaborative way. True Colours meets the requirements of patient confidentiality and security as it has been designed to enable compliance with the Data Protection Act 1998 and 2003 [20,21] and the NHS Information Governance Assurance Framework [22].
2.2. Patients and design
A group of 159 potential participants aged 18 and over was obtained from the patient lists of the three consultant psychiatrists initially implementing True Colours at the Oxford Bipolar Disorder Research Clinic. The status of these participants as current or previous True Colours users was confirmed by their responsible clinician and further authenticated through cross-referencing with the True Colours database. Screening of the cohort was conducted to identify: a clinician confirmed diagnosis of bipolar disorder I, II or Not Otherwise Specified (NOS) using the Structured Clinical Interview for DSM-IV (SCID); registration with the True Colours system for a minimum of 12 months; and accessible paper or electronic psychiatric notes covering the full 12-month periods prior to and after enrolment with True Colours (pre-TC and TC periods, respectively) as of 2010.
Compliance with remote mood monitoring was measured for each participant as the proportion of valid SMS/email messages received by the True Colours system in comparison to the expected number of weekly QIDS and ASRM scale messages over the first year monitoring period. Anonymised patient-level data on the number of messages sent and received by the True Colours system were extracted directly by the system manager for the relevant 12-month periods. Individual case notes were screened for contacts with various mental health care staff and psychiatric hospital admissions for the 12 months before and 12 months after engagement with remote mood monitoring by an independent research assistant. Written consent was sought from all participants. The study protocol was approved by the local Research Ethics Committee (Oxfordshire REC A, Reference: 10/H0604/13).
2.3. Analysis
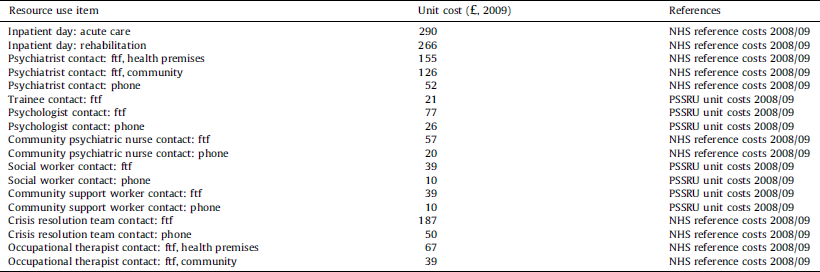
The economic analysis had a before and after study design. Investigated resource use categories included mental health inpatient hospitalisations, face-to-face and phone contacts with psychiatrists (including trainees), psychologists, community mental care staff (community psychiatric nurse, community support worker, crisis team, occupational therapist, social worker) and psychiatric medications. Service costs were calculated in British £s for the last respective year of resource use using UK national-level unit costs [Reference Curtis and Netten23,24]. For medications, we used average mg prices based on the British National Formulary [25]. Applied unit costs are listed in Table 1.
Table 1 Unit costs (GBP (£), year 2009).
A frequency analysis of observed, patient-level mental health service use data and comparison of observed costs in the pre-TC and TC periods were carried out using t-test. In addition, mental health service costs were analysed in a multiple regression analytic framework [26–Reference Mihaylova, Briggs, O’Hagan and Thompson28] to explore the associations with age, gender, duration of illness and period of observation (pre-TC or TC), and to adjust for potential, a priori defined confounders such as the presence of significant manic and/or depressive symptoms at the time of engagement with True Colours, and patients’ referral status to the Oxford Bipolar Disorder Research Clinic during the pre-TC period (newly referred vs. long-term patients). Statistical significance was considered at 5% (two-sided, P = 0.05). All analyses were carried out in STATA 10 (StataCorp. LP, College Station, Texas, USA, 2007).
3. Results
3.1. Patients
Seventy-nine participants (33 male/46 female) aged 18 to 71 years (mean age = 39 years, SD = 13 years) fulfilled all of the specified inclusion criteria and consented to the study. Participants’ history of bipolar I (n = 52), II (n = 9) or NOS (n = 18) varied from 24 to 612 months (mean length = 175 months, SD = 123 months). At the time of engagement with remote mood monitoring, 9% of the patients (7/79) had manic symptoms, 60% of the patients (47/79) had depressive symptoms, 11% of the patients (9/79) had a mixed elevation of manic and depressive symptoms, and 20% of the patients (16/79) were euthymic (Table 2). 57% of the patients (45/79) had been registered with the Oxford Bipolar Disorder Research Clinic for the full 12 months before engaging with remote mood monitoring rather than being referred from another mental health service provider, and are indicated in this publication as long-term patients of the clinic. The socio-demographic characteristics of these long-term patients did not differ significantly from those of the full cohort (Table 2).
Table 2 Socio-demographic and clinical characteristics of the cohort at the time of engagement with True Colours monitoring.

3.2. Compliance with remote mood monitoring
Fifty-two patients (66%) used SMS-based monitoring, 17 patients (22%) used email-based monitoring and 9 patients (11%) used a combination of both over the 12-month TC period. The average compliance rate with monitoring was 82% (median = 91%, IQR: 77–100%) (Fig. 1). Patients using monitoring via SMS had a median compliance rate of 92% (IQR: 83–100%) with a minimum compliance of 16%. Patients using monitoring via email also had a median compliance rate of 92% (IQR: 71–100%) with a minimum compliance of 12%. Those patients who used a combination of both communication methods had a median compliance rate of 87% (IQR: 45–92%) with a minimum compliance of 21%. There were no observable differences between good and bad compliers in terms of their age, gender, duration of illness, presence of manic and/or depressive symptoms at the time of engagement with True Colours, or referral status to the Oxford Bipolar Disorder Research Clinic during the pre-TC period.

Fig. 1 Compliance rate.
3.3. Mental health service use and costs
Mental health service use data were captured for the period Dec 2005-Aug 2010. During the pre-TC period, 6% of the cohort (5/79) was hospitalized on a psychiatric ward for a total of 72 nights. During the TC period, psychiatric hospitalization occurred for 5% of the cohort (4/79) for a total of 133 nights. The mean number of psychiatrist contacts changed from 4.01 (SD = 3.11) to 5.7 (SD = 4.21) between the pre-TC and TC periods, leading to an average £ 291 (95% CI: £ 105 to £ 478) increase in the relevant costs. The average number of different psychiatric medications prescribed over 12 months changed from 2.28 (SD = 1.58) to 2.71 (SD = 1.61) between the pre-TC and TC periods, while the annual cost of psychiatric medications increased by £ 247 per patient (95% CI: £ 108 to £ 386), respectively. Although the types of the five most commonly prescribed psychiatric medications did not differ after monitoring was introduced, all except citalopram had an increase in their usage rates: 41% vs. 38% for lithium, 41% vs. 33% for lamotrigine, 32% vs. 29% for valproate/valproic acid, 48% vs. 20% for quetiapine, and 11% vs. 11% for citalopram. Overall, 38% of the cohort (30/79) had an increase in the number of prescribed psychiatric medications between the pre-TC and TC periods, while 9% (7/79) had a decrease. For the remaining 53% of the patients (42/79), there was no change in the number of prescribed psychiatric drugs. There were no other observable mental health service use differences between the periods (Table 3).
Table 3 Use of mental health services: frequency analysis and observed costs (n indicates the number of patients with a >0 resource use).

The observed increase in the total mental health services costs was an average £ 686 per patient (95% CI: -£ 101 to £ 1473) between the pre-TC and TC periods (Table 3). Observed costs were adjusted for the potential effects of age, gender, duration of illness, significant manic or depressive symptoms at the time of engagement with monitoring and referral status using multiple linear regression analysis (Table 4). Referral status proved of particular importance. Patients newly referred to the Oxford Bipolar Disorder Research Clinic during the pre-TC period showed a tendency for less psychiatrist contact costs during the year prior to engagement with mood monitoring in comparison to long-term patients of the clinic (mean difference = -£ 217, P = 0.075) and had a significant increase in their psychiatrist contact costs between the two observation periods (£ 738, P < 0.01). The same tendency was not present for long-term patients who did not have any significant change in their mean annual cost of psychiatrist contacts between the pre-TC and TC periods (-£ 46, P = 0.615). Annual psychiatric medication costs also increased significantly after the introduction of monitoring (mean difference = £ 235, P < 0.01), but this change was independent from referral status.
Table 4 Multiple regression (OLS) analysis of mental health service costs (£, year 2009).

* P < 0.1.
** P < 0.05.
*** P < 0.01.
In the case of long-term patients, there was no overall trend in total mental health service costs between the pre-TC and TC periods (mean difference = £ 20, P = 0.958). For newly referred patients, the substantial increase in total mental health service costs (mean difference = £ 1547, P = 0.075) showed a tendency towards significance. Excluding hospitalization, costs did not alter these inferences (mean difference = £ 181, P = 0.260 for long-term patients vs. mean difference = £ 859, P < 0.01 for newly referred patients).
Female patients had significantly higher psychologist contact costs (£ 70, P = 0.045) and showed a tendency towards higher community mental health staff contact costs (£ 161, P = 0.075) than male patients. Patients with manic symptoms at the time of engagement with mood monitoring had significantly less annual psychiatric medication costs than those without (-£ 488, P = 0.001). There was also indication of depressive symptoms being associated with more costly hospitalization costs (£ 506, P = 0.061).
4. Discussion
The current study explores the achievable compliance with weekly remote mood monitoring in a real-life, specialist care setting and the impact of such services on the mental health service use of adults with bipolar disorder in the UK. The study found that compliance with remote mood monitoring was high, an average 82% across the whole patient cohort. This compliance rate is comparable or even superior to the average achievable compliance rates found so far in controlled studies of different mobile system applications, respectively, 42% [Reference Depp, Kim, Vergel de Dios, Wang and Ceglowski15], 88% [Reference Faurholt-Jepsen, Frost, Vinberg, Christensen, Bardram and Kessing12] and over 90% [Reference Saunders, Bilderbeck, Panchal, Atkinson, Geddes and Goodwin17]. The results also suggest that the introduction of mood monitoring was not associated with significant changes in mental health service costs except an increase in psychiatric medication costs over the first year of monitoring.
We used regression analysis to account for the most likely confounders of mental health service use (clinical status at the time of engagement with True Colours, and referral status). Due to the sample size and that all patients were outpatients with similar symptom burden, the type of bipolar disorder was not considered separately. The adjusted cost results revealed that the observed tendency towards increased psychiatrist contacts and total mental health service costs were only associated with patients who were newly referred to the clinic during the pre-TC period. Therefore, the increase was likely to be the consequence of a changed care setting for these patients rather than the direct effect of patients’ engagement with weekly remote mood monitoring. On the other hand, a significant increase in psychiatric medication costs between the pre-TC and TC periods was found across all participants. The data indicate that during the monitoring period there were more frequent changes to psychiatric medications and higher levels of polypharmacy as a possible consequence of a more intensively managed medication regimen. In addition, the prescription rate of quetiapine more than doubled during the TC period. These findings are in line with earlier evidence in the field. For example, Simon et al. looked at a multicomponent intervention programme including regular monitoring of mood symptoms and found increased psychotropic medication costs in the intervention group [Reference Simon, Ludman, Bauer, Unützer and Operskalski29]. The significantly lower psychiatric medication costs of patients with manic symptoms are expected to reflect the easier treatability of manic mood episodes. No significant changes could be detected in hospitalizations and the relevant costs, although the study was neither sufficiently large nor long-term to make robust inferences.
A larger prospective study is required to demonstrate whether automated mood monitoring can facilitate the detection and prevention of relapse. There is preliminary evidence that relapse prevention of mania is facilitated by the identification of manic prodromes [Reference Perry, Tarrier, Morriss, McCarthy and Limb30]. It might be expected that self-rating of manic symptoms or identification of relapse signatures would be facilitated by automated registration on a system such as True Colours.
Direct comparisons with other methods for automated symptom monitoring in bipolar disorder are limited. The ChronoRecord system is designed for daily use on a personal computer, and in a selected patient group compliance was very high [Reference Bauer, Grof, Rasgon, Glenn, Alda and Priebe31]. There are also a number of self-monitoring devices for use by individuals using home computers or smart phones [Reference Callan, Wright, Cucciare and Weingardt32]. However, our system is unusual in being integrated into a clinical service and as such, we are not aware of a fully comparable system.
4.1. Limitations
The study has inherent limitations due to its retrospective, non-randomised nature. Although we explored the impact of the most likely confounders, we cannot exclude the possible effect of unknown confounders, which could not be included in the regression analysis. Second, potentially different administration practices between the Oxford Bipolar Disorder Research Clinic and the referring services could have also contributed to the significant increase in psychiatrist contact costs for newly referred patients. Third, the study looked at remote mood monitoring of patients treated at a specialist psychiatric care centre which is likely to limit the external generalisability of the results to other settings or patient populations. For the same reason, the reported average per patient costs of psychiatrist contacts and psychiatric medications are likely to be higher, while the psychologist and community mental health costs lower than any primary care or community care based estimates. Fourth, we were not able to collect information on non-mental health service use or link resource use directly to clinical outcomes. Therefore, the current cost figures do not reflect the total health and social care costs of bipolar disorder and should not be used for estimating the cost-effectiveness of regular remote mood monitoring. In addition, as cost estimates also refer to the last relevant resource use year rather than the latest calendar year, they may not be fully representative of current service prices. Since routine service provision for bipolar patients has not changed over the past few years, this shall not impact the overall validity or the comparative value of the analysis.
In summary, compliance with remote mood monitoring in a specialist outpatient setting was high for patients with bipolar disorder. Given the superiority of specialist care over generic care for bipolar patients [Reference Kessing, Hansen, Hvenegaard, Christensen, Dam and Gluud10], this approach is relevant to improving practice in bipolar disorder in developed countries [Reference Goodwin, Haddad, Ferrier, Aronson, Barnes and Cipriani9]. Improved use of information technology will be key to improving services in the coming years.
Ethical statement
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Funding source
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Reference Number RP-PG-0108-10087)
Disclosure of interest
GMG and JRG are NIHR Senior Investigators. GMG is past president of ECNP, holds a grant from Wellcome Trust, holds shares in P1vital and has served as consultant, advisor or CME speaker for AstraZeneca, MSD, Eli Lilly, Lundbeck (/Otsuka or/Takeda), Medscape, P1Vital, Pfizer, Servier.
J. Simon, K. Budge, J. Price declare that they have no competing interest.
Acknowledgements
Jean Christensen managed the project. JS designed the study with input from JRG, GMG and JP. KB collected the data. The analyses were carried out by JS and KB. All authors were involved in the conduct of the study, interpreting the results, and in revising and correcting the paper, which was drafted by JS. All authors read and approved the final version of the manuscript.
References













Comments
No Comments have been published for this article.