Introduction
People living with HIV (PLHIV) experience high rates of mental illness, including elevated rates of depression and anxiety (Weiser et al., Reference Weiser, Wolfe and Bangsberg2004). In the United States (USA), poverty and social deprivation are concentrated among PLHIV (Pellowski et al., Reference Pellowski, Kalichman, Matthews and Adler2013), and may contribute to poor mental health. An important challenge that low-income PLHIV in the USA frequently face is food insecurity (Palar et al., Reference Palar, Laraia, Tsai, Johnson and Weiser2016; Spinelli et al., Reference Spinelli, Frongillo, Sheira, Palar, Tien, Wilson, Merenstein, Cohen, Adedimeji, Wentz, Adimora, Metsch, Turan, Kushel and Weiser2017), which includes food insufficiency and hunger, poor quality diets, persistent uncertainty around access to food and having to engage in personally or socially unacceptable food procurement (Jones et al., Reference Jones, Ngure, Pelto and Young2013). Food insecurity has been associated with a range of poor mental health outcomes including depression (Whitaker et al., Reference Whitaker, Phillips and Orzol2006; Palar et al., Reference Palar, Kushel, Frongillo, Riley, Grede, Bangsberg and Weiser2015; Tuthill et al., Reference Tuthill, Sheira, Palar, Frongillo, Wilson, Adedimeji, Merenstein, Cohen, Wentz, Adimora, Ofotokun, Metsch, Kushel, Turan, Konkle-Parker, Tien and Weiser2019), anxiety (Whitaker et al., Reference Whitaker, Phillips and Orzol2006; Whittle et al., Reference Whittle, Sheira, Wolfe, Frongillo, Palar, Merenstein, Wilson, Adedimeji, Weber, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019b), symptoms of post-traumatic stress disorder (Golin et al., Reference Golin, Haley, Wang, Hughes, Kuo, Justman, Adimora, Soto-Torres, O'Leary and Hodder2016; Whittle et al., Reference Whittle, Sheira, Wolfe, Frongillo, Palar, Merenstein, Wilson, Adedimeji, Weber, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019b), substance use (Whittle et al., Reference Whittle, Sheira, Frongillo, Palar, Cohen, Merenstein, Wilson, Adedimeji, Cohen, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019a) and suicidality (Alaimo et al., Reference Alaimo, Olson and Frongillo2002; Davison et al., Reference Davison, Marshall-Fabien and Tecson2015). While people who experience mental illness likely face more barriers to accessing healthy food, evidence from longitudinal and qualitative studies indicates that food insecurity contributes to symptoms of common mental illness (Hamelin et al., Reference Hamelin, Beaudry and Habicht2002; Palar et al., Reference Palar, Kushel, Frongillo, Riley, Grede, Bangsberg and Weiser2015; Whittle et al., Reference Whittle, Palar, Seligman, Napoles, Frongillo and Weiser2016; Tuthill et al., Reference Tuthill, Sheira, Palar, Frongillo, Wilson, Adedimeji, Merenstein, Cohen, Wentz, Adimora, Ofotokun, Metsch, Kushel, Turan, Konkle-Parker, Tien and Weiser2019; Whittle et al., Reference Whittle, Sheira, Wolfe, Frongillo, Palar, Merenstein, Wilson, Adedimeji, Weber, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019b). Provision of food support to food-insecure individuals in a manner consistent with the preservation of dignity has been shown to reduce symptoms of depression (Palar et al., Reference Palar, Napoles, Hufstedler, Seligman, Hecht, Madsen, Ryle, Pitchford, Frongillo and Weiser2017; Palar et al., Reference Palar, Frongillo, Riley, Ryle, Madsen, O'Donnell, Napoles, Sheira, Phillips and Weiser2018).
These findings raise questions about how symptoms of common mental illness occurring in the setting of adverse social and structural factors should be addressed. Mental illness and its treatment are often formulated according to a ‘biopsychosocial’ model (Engel, Reference Engel1977) in which multidimensional influences on mental health are addressed concurrently through psychotropic medications, psychological interventions and services aimed at improving social circumstances. Yet, in practice, psychotropic medications often predominate. In the USA, data have shown significant upward trends over the past two decades for the use of psychotropic medications alone, compared to significant downward trends for the use of psychotherapy and psychotropic medications together or psychotherapy alone (Olfson and Marcus, Reference Olfson and Marcus2010). One in six US adults is now prescribed a psychotropic medication, rising to one in five among non-Hispanic White adults and one in four among adults aged 60–85 years (Moore and Mattison, Reference Moore and Mattison2017).
Pharmaceutical drugs are prominent for several reasons. Psychotropic medications have the most extensive evidence base among mental health interventions, as their effects can be measured through randomised controlled trials more easily than other forms of intervention. In meta-analyses of trials, common classes of psychotropic medications including antidepressants and antipsychotics show modest but significant therapeutic effects for their respective indications (Leucht et al., Reference Leucht, Cipriani, Spineli, Mavridis, Orey, Richter, Samara, Barbui, Engel, Geddes, Kissling, Stapf, Lassig, Salanti and Davis2013; Cipriani et al., Reference Cipriani, Furukawa, Salanti, Chaimani, Atkinson, Ogawa, Leucht, Ruhe, Turner, Higgins, Egger, Takeshima, Hayasaka, Imai, Shinohara, Tajika, Ioannidis and Geddes2018). Prescribing drugs is also less labour-intensive than psychological or social interventions, and often more accessible and time-efficient for service users. In the USA specifically, the market-based structure of the healthcare system may contribute to higher rates of psychotropic medications, which have the financial and promotional backing of for-profit pharmaceutical companies (Moncrieff, Reference Moncrieff2008). Conversely, reimbursement rates for non-pharmacological treatments by Medicare (US government health insurance for low-income individuals) have been falling steadily for many years, driving psychologists and other allied professionals away from low-income service users (American Psychological Association, 2015). Furthermore, psychotropic medications adhere to a medical model of intervention that accords with the clinical education of prescribers. The paucity of social science training in clinical curricula leaves clinicians lacking the intellectual tools and frameworks to fully understand how social-structural issues may drive distress (Holmes, Reference Holmes2013; Metzl and Hansen, Reference Metzl and Hansen2014; Hansen et al., Reference Hansen, Braslow and Rohrbaugh2018). Consequently, social interventions may be placed at lower priority than pharmaceutical drugs by default, principally through unfamiliarity and misunderstanding on the part of clinicians.
The vulnerability of public funding for social support to changes in fiscal policies and political ideologies may also contribute to the primacy of pharmacologic interventions. In the USA, public spending on social safety net institutions has undergone a sustained reduction since the 1980s (Harvey, Reference Harvey2005; Wacquant, Reference Wacquant2009; Katz Reference Katz2013; Schram, Reference Schram2015). The welfare reforms of 1996 had a particularly detrimental effect on the provision of social support, significantly curtailing access to government income for non-disabled adults, with the most severe restrictions targeting those without dependent children (Hansen et al., Reference Hansen, Bourgois and Drucker2014; Whittle et al., Reference Whittle, Palar, Ranadive, Turan, Kushel and Weiser2017). Notably, this development has left federal disability income as one of the last forms of substantial government assistance available to many indigent adults in the USA (Whittle et al., Reference Whittle, Palar, Ranadive, Turan, Kushel and Weiser2017). Recent studies have suggested that this shift may be fuelling a ‘medicalisation of poverty’, as diagnoses of chronic illness – and particularly mental illness – play an increasingly important economic role for struggling adults to obtain income security through disability status (Hansen et al., Reference Hansen, Bourgois and Drucker2014; Knight, Reference Knight2015). In this respect, diagnoses of mental illness, accompanied by treatment with psychotropic medications, can act as an important gateway to a level of income stability otherwise unobtainable for many in the current US context of widespread working poverty under welfare reform (Hansen et al., Reference Hansen, Bourgois and Drucker2014; Knight, Reference Knight2015). Identifying these social and economic realities does not imply that disabled individuals are malingering, or that clinicians are prescribing for non-clinical reasons, but suggests instead that we consider the impact, at a population level, of structural factors that incentivise the prescription of psychotropic drugs for socially deprived individuals.
These arguments raise the question of whether social adversity might drive higher rates of psychotropic prescriptions, independent of psychiatric symptoms. Few empirical studies have attempted to investigate this possibility. We used data from the Women's Interagency HIV Study (WIHS), an ongoing prospective cohort study at nine sites across the USA, to investigate the associations between food insecurity and psychotropic medication use among a broadly representative population of women living with HIV in the USA. Our previous studies in the WIHS cohort have demonstrated dose–response relationships between food insecurity and poor mental health outcomes, including depression (Tuthill et al., Reference Tuthill, Sheira, Palar, Frongillo, Wilson, Adedimeji, Merenstein, Cohen, Wentz, Adimora, Ofotokun, Metsch, Kushel, Turan, Konkle-Parker, Tien and Weiser2019), anxiety, stress, symptoms of post-traumatic stress disorder (Whittle et al., Reference Whittle, Sheira, Wolfe, Frongillo, Palar, Merenstein, Wilson, Adedimeji, Weber, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019b), substance use (Whittle et al., Reference Whittle, Sheira, Frongillo, Palar, Cohen, Merenstein, Wilson, Adedimeji, Cohen, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019a) and mental health-related quality of life (Tuthill et al., Reference Tuthill, Sheira, Palar, Frongillo, Wilson, Adedimeji, Merenstein, Cohen, Wentz, Adimora, Ofotokun, Metsch, Kushel, Turan, Konkle-Parker, Tien and Weiser2019). Here we used a cross-sectional sub-sample of the WIHS cohort for which data on psychotropic medication use were available to test two successive hypotheses: (1) food insecurity would be associated with psychotropic medication use in a dose–response relationship among women living with HIV, mirroring the dose–response relationships between food insecurity and symptoms of common mental illness found in previous studies; and (2) if we additionally adjusted for symptoms of common mental illness, any positive associations between food insecurity and psychotropic medication use would remain significant.
Methods
Study design and population
Our study was a cross-sectional analysis of data from the WIHS, a prospective cohort study of HIV-seropositive women and demographically similar HIV-seronegative women in the USA. Cohort recruitment, demographics and retention are described elsewhere (Barkan et al., Reference Barkan, Melnick, Preston-Martin, Weber, Kalish, Miotti, Young, Greenblatt, Sacks and Feldman1998; Bacon et al., Reference Bacon, von Wyl, Alden, Sharp, Robison, Hessol, Gange, Barranday, Holman, Weber and Young2005; Hessol et al., Reference Hessol, Weber, Holman, Robison, Goparaju, Alden, Kono, Watts and Ameli2009; Adimora et al., Reference Adimora, Ramirez, Benning, Greenblatt, Kempf, Tien, Kassaye, Anastos, Cohen, Minkoff, Wingood, Ofotokun, Fischl and Gange2018). WIHS participants undergo structured interviews and physical examinations every 6 months at nine sites across the USA and have blood and other biological samples taken. The WIHS began with baseline recruitment in 1994 and has undergone three recruitment waves since. Beginning in 2009, a standardised and detailed neurocognitive assessment was added to the WIHS Core exams and administered every 2 years.
From April 2013 through March 2016, the Food Insecurity Sub-study collected data every 6 months on food security, nutrition and other key socio-economic variables from all WIHS participants. For the current analysis, women living with HIV who participated in the Food Insecurity Sub-study from April 2013 through March 2015 and also had neurocognitive and psychiatric variables (including psychotropic medication use) during the same time period were included (n = 905). Data collection for psychotropic medication use was staggered across four WIHS visits during this period, at five study sites: San Francisco, CA; Chicago, IL; Washington, DC; Bronx, NY and Brooklyn, NY.
Primary explanatory variable
Food security (FS) was the primary explanatory variable, measured using the Household Food Security Survey Module (HFSSM) (US Department of Agriculture, 2012). The HFSSM is an 18-item survey designed to capture the experience of anxiety around household food supplies, inadequate quality of food and/or reduced food intake. Originally developed from in-depth qualitative and survey data among women in the USA (Radimer et al., Reference Radimer, Olson, Greene, Campbell and Habicht1992; Wehler et al., Reference Wehler, Scott and Anderson1992), it has since been validated in multiple diverse contexts (Jones et al., Reference Jones, Ngure, Pelto and Young2013). Respondents are classified as having high, marginal, low or very low FS. Very low FS corresponds to reduced food intake and hunger, while marginal FS implies persistent anxiety and uncertainty around food. The internal consistency of the HFSSM in this sample was high (Cronbach's α = 0.90).
Outcome variables
The primary outcomes were four categories of prescribed psychotropic medication use (antidepressant use, sedative/hypnotic/tranquiliser/anxiolytic use, antipsychotic use and a pooled outcome of any psychotropic medication use). WIHS participants are asked to bring a list of medications to each visit and are also asked specifically whether they are using any medications ‘for psychological conditions or depression’ and for the name of the medication. Self-reported psychotropic medications were coded as antidepressants (e.g. selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors and tricyclic antidepressants), sedatives/hypnotics/tranquilisers/anxiolytics (hereafter referred to as ‘sedatives’; e.g. benzodiazepines and Z-drugs) or antipsychotics (e.g. typical and atypical neuroleptics) as appropriate. Using these data, we constructed a pooled outcome for any psychotropic medication use (i.e. use of an antidepressant, sedative or antipsychotic) and made three separate binary outcomes corresponding to each individual drug class.
Other outcomes included symptoms of depression, generalised anxiety disorder and mental health-related quality of life. Symptoms of depression were measured using the Center for Epidemiologic Studies Depression (CESD) score, a widely used self-report instrument that asks participants how often they experience symptoms of depression including low mood, low self-esteem, poor concentration, sleeping difficulties, poor appetite and others (Eaton et al., Reference Eaton, Muntaner, Smith, Tien, Ybarra and Maruish2004). Scores range from 0 to 60, with higher scores indicating greater depressive symptoms. CESD score is a core WIHS study measure collected from WIHS participants at each visit. The internal consistency of the CESD in our sample was high (Cronbach's α = 0.93).
We measured symptoms of generalised anxiety disorder (GAD) using the Generalised Anxiety Disorder-7 (GAD-7) scale, a 7-item self-report instrument used to screen for and categorise the severity of GAD in primary care (Spitzer et al., Reference Spitzer, Kroenke, Williams and Lowe2006). Participants were asked how often they experience symptoms of GAD including worry, restlessness, irritability and others, with responses scored from 0 to 21. In the WIHS, collection of GAD-7 data only began in October 2013. GAD-7 data were therefore only available for approximately 75% of the women participating in our study. The internal consistency of the GAD-7 in the sample was high (Cronbach's α = 0.92).
Mental health-related quality of life was measured using the Mental Health Summary (MHS) score of the Medical Outcomes Study HIV Health Survey (MOS-HIV) scale (Revicki et al., Reference Revicki, Sorensen and Wu1998). The MOS-HIV scale, a widely used quality of life measure developed and validated among PLHIV, comprises 35 questions across ten domains, providing a total score out of 100. The MHS is calculated from the total MOS-HIV score by means of a standardised method that transforms the scores of relevant domains into a standardised t-score with a mean of 50 and standard deviation of 10. MHS is a continuous variable composed of four sub-scales where lower scores indicate worse mental health-related quality of life (e.g. feeling nervous and depressed) and higher scores indicate better mental health-related quality of life (e.g. feeling calm and peaceful). WIHS participants undergo the MOS-HIV annually (i.e. every two study visits). Since psychotropic medication data were staggered across four study visits (approximately 2 years), MHS data were only available for approximately 50% of the women contributing data to this study. The internal consistency of the MHS (Cronbach's α) was 0.80.
Other variables
Based on theory and the literature, we identified potential variables that may confound the relationship between food insecurity and psychotropic medication use (Allen et al., Reference Allen, Balfour, Bell and Marmot2014). These were age at visit, race/ethnicity (non-Hispanic White, Hispanic, African-American or other), annual income (⩽$12 000, $12 001–24 000 or ⩾$24 001), education (less than high school education v. at least high school education), heavy drinking (>7 v. ⩽7 alcoholic drinks/week) and illicit substance use (use of any illicit substances not including cannabis since the last visit v. none). All of these variables were measured by self-report.
Ethics statement
Participants provided written informed consent for participation in the WIHS and received compensation for their participation at each visit. The institutional review board of each study site's institution and the WIHS Executive Committee approved this study.
Statistical analysis
Data were obtained from WIHS visits at which women both completed the HFSSM and had coded psychotropic medication data available, creating a cross-sectional sample staggered over four study visits (approximately 2 years). Initially, we examined associations of FS with common mental illness to confirm whether the dose–response relationships found in previous studies were reproduced in this sub-sample. To examine associations of FS with CESD score, GAD-7 score and MHS score, we ran multivariable linear regressions.
Next, we tested associations between FS and psychotropic medication use in two successive models. First, we ran multivariable logistic regressions to examine associations of FS with any psychotropic medication use and antidepressant, sedative and antipsychotic use individually, adjusting for race/ethnicity, income, education, heavy drinking and illicit substance use. For any psychotropic medication use, antidepressant use and sedative use, we then ran multivariable logistic regressions also adjusted for CESD score and GAD-7 score (in addition to the other variables listed above). We did not include antipsychotic use as an individual outcome in this fully adjusted model because depression and anxiety are not clinical indications for antipsychotic use, which would render the outcome difficult to interpret (the WIHS does not include any measure of psychosis). The area under the receiver operating characteristic curve, which ranges from 0.5 (chance) to 1.0 (perfect), was used to quantify how well the models explained the outcomes (Swets, Reference Swets1988). All analyses were completed using Stata version 14 (StataCorp LP, College Station, TX, USA).
Results
There were 905 women in the sample (Table 1). Approximately two-thirds (67.5%) identified as African-American, while just under half (48.6%) reported an annual income less than $12 000. Over one-third (36.8%) were categorised as food-insecure (i.e. marginal, low or very low FS). In total, one-third (33.0%) were taking psychotropic medication. The most common class was antidepressants (taken by 27.6% of women), followed by sedatives (14.0%) and then antipsychotics (9.3%). In adjusted analyses, compared to high FS, marginal, low and very low FS were significantly associated with increasingly higher CESD and GAD-7 scores and with increasingly lower MHS scores, exhibiting a consistent dose–response relationship across all three outcomes (Table 2).
Table 1. Background characteristics of sub-sample (n = 905)

a Heavy drinking defined as ≥7 drinks/week (1 drink defined as 1 can, bottle, or glass of beer; 1 glass of wine; 1 shot of liquor on its own or in a mixed drink; or any other kind of alcoholic beverage).
b Participants were asked if they used cocaine, crack, heroin, methamphetamine, hallucinogens, club drugs, or any other illicit or recreational drugs not including cannabis since the last visit.
Table 2. Multivariable linear regressions to examine the association between FS and symptoms of common mental illness among HIV+ women

∗∗∗p < 0.001, ∗∗p < 0.01, ∗p < 0.05.
a Heavy drinking defined as ≥7 drinks/week (1 drink defined as 1 can, bottle, or glass of beer; 1 glass of wine; 1 shot of liquor on its own or in a mixed drink; or any other kind of alcoholic beverage).
b Participants were asked if they used cocaine, crack, heroin, methamphetamine, hallucinogens, club drugs, or any other illicit or recreational drugs not including cannabis since the last visit.
Of the other variables studied, self-identifying as African-American/Black, having an income ⩾$24 001, and having at least a high school education were all variously associated with better mental health (lower CESD scores, lower GAD-7 scores and/or higher MHS scores). Illicit substance use was associated with higher CESD and GAD-7 scores and lower MHS scores.
For the psychotropic medication use outcomes, we first performed adjusted analyses in the absence of adjustment for CESD and GAD-7 scores. We found that marginal and low FS were associated with 2.06 (p < 0.001; 95% confidence interval [CI] = 1.36–3.13) and 1.99 (p < 0.01; 95% CI = 1.26–3.15) times higher odds of any psychotropic medication use, respectively, compared to high FS (Table 3). While very low FS was associated with 1.50 times higher odds of any psychotropic medication use, this was not statistically significant. Associations between FS and each individual category of psychotropic medication use exhibited a similar pattern of findings, with the adjusted odds ratios (AORs) consistently highest for marginal FS. Marginal FS was associated with 1.82 (p < 0.01; 95% CI = 1.19–2.80) times higher odds of antidepressant use and 1.73 (p < 0.05; 95% CI = 1.01–2.97) times higher odds of sedative use, while low FS was associated with 1.66 (p < 0.05; 95% CI = 1.03–2.65) times higher odds of antidepressant use. There were no significant associations between FS and antipsychotic use in these models, and no significant associations between very low FS and any of the psychotropic medication outcomes.
Table 3. Multivariable logistic regressions to examine the association between FS and psychotropic medication use among HIV+ women
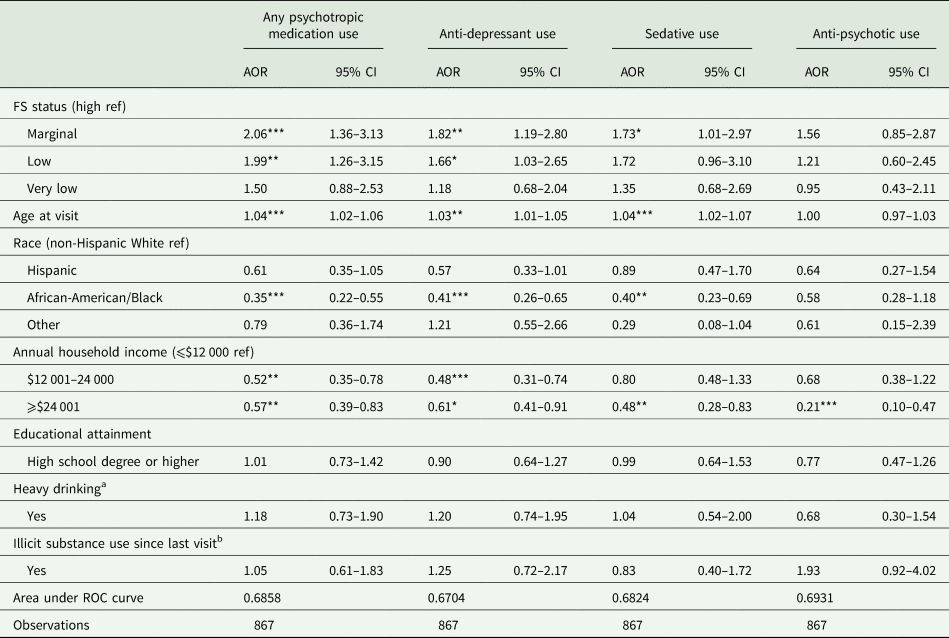
∗∗∗p < 0.001, ∗∗p < 0.01, ∗p < 0.05.
a Heavy drinking defined as ≥7 drinks/week (1 drink defined as 1 can, bottle, or glass of beer; 1 glass of wine; 1 shot of liquor on its own or in a mixed drink; or any other kind of alcoholic beverage).
b Participants were asked if they used cocaine, crack, heroin, methamphetamine, hallucinogens, club drugs, or any other illicit or recreational drugs not including cannabis since the last visit.
We next examined associations of FS with any psychotropic medication use, antidepressant use and sedative use, additionally adjusting for CESD and GAD-7 scores (Table 4). Marginal FS remained associated with 1.93 (p < 0.05; 95% CI = 1.16–3.19) times higher odds of any psychotropic medication use. The AORs for associations of marginal FS with antidepressant and sedative use were 1.64 and 1.42, respectively, although neither reached statistical significance. Associations between low FS and each psychotropic medication outcome were close to 1 (all not statistically significant), while very low FS was associated with lower odds of each outcome, with the association between very low FS and antidepressant use statistically significant (AOR = 0.42; p < 0.05; 95% CI = 0.19–0.96).
Table 4. Multivariable logistic regression models to examine the association between FS and psychotropic medication use among HIV+ women after adjusting for psychiatric symptoms

∗∗∗p < 0.001, ∗∗p < 0.01, ∗p < 0.05.
a Heavy drinking defined as ≥7 drinks/week (1 drink defined as 1 can, bottle, or glass of beer; 1 glass of wine; 1 shot of liquor on its own or in a mixed drink; or any other kind of alcoholic beverage).
b Participants were asked if they used cocaine, crack, heroin, methamphetamine, hallucinogens, club drugs, or any other illicit or recreational drugs not including cannabis since the last visit.
Of the other variables, higher incomes were consistently associated with lower odds of psychotropic medication use prior to adjusting for CESD and GAD-7 scores. Having an annual income of $12 001–24 000 remained significantly associated with lower odds of any psychotropic medication use and antidepressant use after adjusting for CESD and GAD-7 scores, compared to having an annual income ⩽$12 000. Age was positively associated with any psychotropic medication use, antidepressant use and sedative use (but not antipsychotic use), both before and after adjusting for CESD and GAD-7 scores. Self-identifying as African-American/Black was associated with lower odds of any psychotropic medication use, antidepressant use and sedative use, compared to self-identifying as non-Hispanic White (although this was not significant for sedative use after adjusting for CESD and GAD-7 scores). In the fully adjusted model, CESD and GAD-7 scores were positively associated with any psychotropic medication use, antidepressant use and sedative use.
Discussion
In this study of women with HIV in the USA, food insecurity was associated with the symptoms of common mental illness but displayed a complex relationship with psychotropic medication use. Similar to previous studies (Tuthill et al., Reference Tuthill, Sheira, Palar, Frongillo, Wilson, Adedimeji, Merenstein, Cohen, Wentz, Adimora, Ofotokun, Metsch, Kushel, Turan, Konkle-Parker, Tien and Weiser2019; Whittle et al., Reference Whittle, Sheira, Wolfe, Frongillo, Palar, Merenstein, Wilson, Adedimeji, Weber, Adimora, Ofotokun, Metsch, Turan, Wentz, Tien and Weiser2019b), we found a dose–response relationship between food insecurity and symptoms of common mental illness. We hypothesised that associations between food insecurity and psychotropic medication use would reflect this dose–response relationship, but our findings suggest a more complex picture. While marginal FS was associated with significantly higher odds of taking any psychotropic medication, antidepressants and sedatives, the magnitude of the associations decreased as severity of food insecurity increased. Very low FS was associated with lower odds of psychotropic medication use after adjusting for CESD and GAD-7 scores (although this only reached significance for antidepressant use).
While there may be several possible explanations for this pattern of findings, it is most likely that people who experience very low FS find it difficult to engage in mental health care because of competing resource demands. Such individuals may find it difficult to access mental health services and therefore have fewer chances to be prescribed psychotropic medications. Alternatively, they may access care but find it more difficult to adhere to medication regimens and subsequently have prescriptions discontinued. This possibility is supported by previous studies. Food insecurity has consistently been associated with poor engagement in care among PLHIV, including missing clinic visits and suboptimal adherence to medications (Young et al., Reference Young, Wheeler, McCoy and Weiser2014). In qualitative studies, food-insecure PLHIV describe how hunger, exhaustion, pre-occupation with finding food and less money for transport erect major barriers to attending clinics (Whittle et al., Reference Whittle, Palar, Seligman, Napoles, Frongillo and Weiser2016). Similarly, in a nationally representative sample of non-elderly adults in the USA, individuals with severe mental illness who had very low FS were twice as likely to report being unable to afford mental health care, and 25% less likely to be using mental health services, compared to food-secure individuals with severe mental illness (Afulani et al., Reference Afulani, Coleman-Jensen and Herman2018).
Two studies in the USA have found that severe food insecurity was associated with higher rates of acute mental health care utilisation. Among outpatient users of mental health services, severe food insecurity was associated with five times the odds of having any psychiatric emergency room visit (Mangurian et al., Reference Mangurian, Sreshta and Seligman2013); and among a national sample of homeless adults, food insufficiency was associated with three times higher odds of psychiatric hospitalisation (Baggett et al., Reference Baggett, Singer, Rao, O'Connell, Bharel and Rigotti2011). Poor access to ambulatory outpatient mental health services among severely food-insecure individuals may therefore result in inadequate long-term symptom control and, consequently, greater acute mental health care utilisation – which is the same pattern that has been seen in studies of food insecurity and HIV care (Weiser et al., Reference Weiser, Hatcher, Frongillo, Guzman, Riley, Bangsberg and Kushel2013).
Another key finding is that marginal FS remained associated with nearly twice the odds of any psychotropic medication use after adjusting for symptoms of depression and anxiety. This supports our hypothesis that among these women living with HIV, food insecurity, at least in a milder form, may be associated with being prescribed psychotropic medications independent of symptoms of common mental illness. This suggests that people experiencing complex social problems such as food insecurity (but who do not experience such severe levels of social deprivation that they are unable to engage in care) may be prescribed psychotropic medications at a higher rate than those without such problems. This is supported by higher incomes also being associated with lower odds of psychotropic medication use in models additionally adjusted for CESD and GAD-7 scores. These findings indicate that there may be structural incentives and concomitant factors that favour the prescription of psychotropic medications for all forms of distress, regardless of the nature of the dominant contributing factors (e.g. biological v. psychological v. social). As explained above, these factors may include the clinical training of prescribers, the absence of resources for social interventions and/or the relative stability and provision that can accompany a psychiatric diagnosis through disability (Holmes, Reference Holmes2013; Hansen et al., Reference Hansen, Bourgois and Drucker2014; Knight, Reference Knight2015).
Given that the data were cross-sectional, these possible explanations must be interpreted cautiously, and further research is needed. It remains possible that the causality runs in the reverse direction: people with symptoms of common mental illness significant enough to warrant treatment with psychotropic medications may be more likely to be food-insecure, and then may be referred to food assistance services that prevents them from experiencing the most severe form of food insecurity. Longitudinal studies investigating directionality and dominant mediating mechanisms are needed to comprehensively understand this association.
Our study has other limitations. It is not clear from the data who was prescribing psychotropic medications for these women (e.g. HIV specialists v. psychiatrists). Greater clarity on this aspect of the findings would be helpful. Similarly, we have no data on access to mental health services and attendance at clinic appointments, which would clarify some of the mechanisms and explanations behind the findings. Third, we have no data on other mental health treatment modalities among these women, and no data on adherence to treatments, whether pharmacological or non-pharmacological. Measurement of these variables will be important for future studies. Finally, we were unable to adjust for any other symptoms of mental illness besides depression and anxiety because such data were not collected in the WIHS.
Conclusion
Our findings reveal a complex relationship between food insecurity and psychotropic medication use among women living with HIV in the USA. The data tentatively suggest that (1) PLHIV with severe food insecurity may face barriers to engaging in mental health services, and (2) food-insecure PLHIV who are able to engage in mental health services may be more likely to be prescribed psychotropic medications. While these interpretations come with significant caveats owing to limitations of the dataset, they warrant further research, including longitudinal and qualitative studies, examining the relationships of food insecurity (and other forms of social deprivation) with symptoms of common mental illness, access to mental health services, and the prescription of psychotropic medications and other treatment modalities. If further substantiated, our findings support recent calls for incorporating more detailed understandings of the social-structural determinants of health into clinical curricula (Metzl and Hansen, Reference Metzl and Hansen2014; Hansen et al., Reference Hansen, Braslow and Rohrbaugh2018) and for re-examining how the structure of the US social safety net and healthcare system affects the course of different chronic illnesses (Hansen et al., Reference Hansen, Bourgois and Drucker2014; Whittle et al., Reference Whittle, Palar, Ranadive, Turan, Kushel and Weiser2017).
Data
Data for this manuscript were provided by the Women's Interagency HIV Study (WIHS) as part of an Executive Committee (EC) approved concept sheet. These data cannot be provided to other investigators or used for additional projects without the written consent of the WIHS EC. Data are made available to investigators through a formal concept sheet submission and review process or the WIHS Public Use Data Set. Please visit http://www.wihshealth.org for more information on how to obtain WIHS data.
Acknowledgements
We acknowledge the participants of the WIHS for generously sharing their time and information to make this study possible.
Financial support
This study was funded by a Women's Interagency HIV Study (WIHS) sub-study grant from the National Institute of Mental Health, R01MH095683 (Dr. Weiser). Additional salary support was provided by K01DK107335 (Dr. Palar). Publication was made possible in part by support from the UCSF Open Access Publishing Fund. Data in this manuscript were collected by the Women's Interagency HIV Study (WIHS). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). WIHS (principal investigators): UAB-MS WIHS (Mirjam-Colette Kempf and Deborah Konkle-Parker), U01-AI-103401; Atlanta WIHS (Ighovwerha Ofotokun and Gina Wingood), U01-AI-103408; Bronx WIHS (Kathryn Anastos and Anjali Sharma), U01-AI-035004; Brooklyn WIHS (Howard Minkoff and Deborah Gustafson), U01-AI-031834; Chicago WIHS (Mardge Cohen and Audrey French), U01-AI-034993; Metropolitan Washington WIHS (Seble Kassaye), U01-AI-034994; Miami WIHS (Margaret Fischl and Lisa Metsch), U01-AI-103397; UNC WIHS (Adaora Adimora), U01-AI-103390; Connie Wofsy Women's HIV Study, Northern California (Ruth Greenblatt, Bradley Aouizerat, and Phyllis Tien), U01-AI-034989; WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub), U01-AI-042590; Southern California WIHS (Joel Milam), U01-HD-032632 (WIHS I–WIHS IV). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA) and the National Institute on Mental Health (NIMH). Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and other Communication Disorders (NIDCD) and the NIH Office of Research on Women's Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR000454 (Atlanta CTSA) and P30-AI-050410 (UNC CFAR).
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.






