The prevalence of obesity has doubled in many European countries over the last decades, and the numbers of those affected continue to rise at an alarming rate(Reference Finucane, Stevens and Cowan1–Reference Kumanyika, Obarzanek and Stettler3). In Finland, for example, the prevalence of obesity was found to have nearly doubled from 11·3 to 20·7 % among men, and it rose from 17·9 to 24·1 % in women over a 20-year period(Reference Lahti-Koski, Seppänen-Nuijten and Männistö4). The detrimental consequences of excess adipose tissue depend on its distribution. Abdominal obesity, assessed by waist circumference (WC), is found to be more closely related to health risks than overall obesity(Reference Huxley, Mendis and Zheleznyakov5–Reference Wassink, van der Graaf and van Haeften8). Adverse changes in body shape and fat distribution have already occurred in the general population. Over the last decades, average BMI values have increased, but in recent few years, weight gain has occurred mainly in WC, since the rise of BMI has attenuated and WC has continued to increase steadily(Reference Lahti-Koski, Harald and Männistö9). This change has been substantial particularly among young Finns.
Although diet is recognised as a key determinant in becoming overweight or obese, the role of specific nutrients, especially carbohydrates(Reference van Dam and Seidell10) and fats(Reference Willett11, Reference Bray, Paeratakul and Popkin12), remains controversial due to the large number of candidate foods and the intercorrelation between dietary components. As a consequence, researchers are increasingly investigating obesity in relation to not only specific foods, nutrients and food components, but also overall dietary patterns. These may have a greater effect on health than any individual food item or nutrient and may possibly prove useful in determining public health recommendations(Reference Hu13).
Dietary quality can be studied using cluster and factor analyses or by using indices and scores, such as the Mediterranean Diet Score(Reference Trichopoulou, Kouris-Blazos and Wahlqvist14). The Mediterranean diet, which is high in vegetables, legumes, fruits and nuts, cereals, fish and seafood, and unsaturated fatty acids (from olive oil), together with moderate alcohol consumption (such as red wine) and low intake of meat and meat products, is recognised as a health-promoting diet(Reference Sofi, Cesari and Abbate15, Reference Sofi, Abbate and Gensini16). Due to differences in food culture and resources, however, the Mediterranean diet may not be easily adopted by Nordics. As a counterpart, the SYSDIET study of the University of Eastern Finland, together with the Finnish Heart Association and the Finnish Diabetes Association, released a Baltic Sea Diet Pyramid in January 2011 in order to illustrate the healthier choices of the diet consumed in the Nordic countries (Denmark, Finland, Iceland, Norway and Sweden)(Reference Uusitupa and Schwab17). The diet is rich in foods grown in the Nordic countries, e.g. apples and berries, roots and cabbages, rye, oats and barley, low-fat milk products, rapeseed oil, and fish (salmon and Baltic herring); it is also low in red meat, processed meat products and alcohol.
The main aim of the present study was to investigate whether the Baltic Sea diet is a diet that could be promoted as a healthy-weight diet. First, we created a score based on the Baltic Sea Diet Pyramid to indicate adherence to the Baltic Sea diet. Furthermore, we assessed whether the Baltic Sea Diet Score (BSDS) is associated with general obesity, defined by BMI, and abdominal adiposity, defined by excess WC.
Methods
Selection of study subjects
The study of the Dietary Lifestyle and Genetic Determinants on the Development of Obesity and Metabolic syndrome (the DILGOM Study) included men and women aged 25–74 years who participated in two phases of the National FINRISK Study, with the first phase taking place between January and March 2007(Reference Vartiainen, Laatikainen and Peltonen18). A random sample of 10 000 people was drawn from the Finnish population register in five geographical areas. The sample was stratified by sex, 10-year age group and area. Participants received by mail an invitation to participate in a health examination and a self-administered health questionnaire. Of the invited subjects, 6258 participated in the health examination (response rate 63 %).
To gather more detailed information on obesity, the metabolic syndrome and diabetes, we invited all participants of the first study phase to be a part of the second study phase (DILGOM) between April and June 2007. Of the invited participants, 5024 participated (participation rate 80 %). After exclusions of participants with a missing FFQ or anthropometric data, or those who were pregnant, the sample size for the present study was 2190 men and 2530 women.
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethics Committee of the Hospital District of Helsinki and Uusimaa for both study phases. Written informed consent was obtained from all subjects.
Anthropometric measurements
At the study sites, specially trained nurses measured weight, height, WC and hip circumference using standardised international protocols(Reference Tolonen, Koponen and Aromaa19). Body weight was measured to the nearest 0·1 kg using an electric bioimpedance scale (TANITA TBF-300MA; Tanita Corporation of America, Inc.), with all participants wearing light clothing and no shoes. Pregnant women and subjects with heart pacemakers did not undergo bioimpedance measurement. Height was measured to the nearest 0·1 cm. BMI was calculated as weight in kg divided by the square of height in m2. The BMI values obtained from TANITA were used because the results of the calculated BMI did not differ from the ones measured with the bioimpedance scale. WC was measured at the midpoint between the lowest rib and the iliac crest to the nearest 0·5 cm with the use of a measuring tape. Categorical obesity was defined as overweight or obese (BMI ≥ 25·0 kg/m2)(20). Categorical abdominal adiposity was defined as normal waist < 100 cm for men and < 90 cm for women(21).
Assessment of background variables
At the study visit, participants completed self-administered health questionnaires, which were used to collect information on the participants' socio-economic characteristics, lifestyle variables and medical history. In the present study, age, education, smoking status and leisure-time physical activity (PA) were used as covariables. Education was assessed by inquiring about the total number of school years. Participants were classified into three educational levels (low, middle and high) according to their birth year; this was done to adjust for the extension of the basic education system and the increase of average school years over time. Smoking status was defined by using four categories: never smoker; quit >1/2 years ago; quit < 1/2 years ago; current smoker. Leisure-time PA was assessed by asking the participants to define their activity outside work using four categories: inactive (mainly reading, watching television or other light activities); moderately active (walking, cycling, gardening or other activity at least 4 h/week); active (brisk running, walking cross-country skiing, swimming or other physically demanding activities at least 3 h/week); highly active (competition sports aiming and physically demanding exercising several times in a week).
FFQ
Participants filled in a validated 131-item FFQ that was designed to measure their habitual diet over the previous 12 months(Reference Paalanen, Männistö and Virtanen22–Reference Männistö, Virtanen and Mikkonen24). They were asked to indicate the average consumption frequency of each FFQ item by using nine frequency categories ranging from ‘never or seldom’ to ‘six or more times a day’. The predefined FFQ-item portion sizes appeared as household and natural units (e.g. glass, slice) on the FFQ. The participants were also able to report other frequently consumed foods not listed. They completed the FFQ at the study site, where a trained study nurse reviewed the questionnaire. Nutritionists entered the data and the average daily food, nutrient and energy intakes (EI) were calculated using the Finnish National Food Composition Database (Fineli®; National Institute for Health and Welfare, Helsinki, Finland)(Reference Reinivuo, Hirvonen and Ovaskainen25). Exclusions were made due to incompletely filled out FFQ (n 74). In addition, men and women (n 48) were excluded if their daily EI (cut-offs) corresponded to 0·5 % at both ends of the daily EI distributions.
Baltic Sea Diet Score
We transformed the Baltic Sea Diet Pyramid(Reference Uusitupa and Schwab17) to a BSDS. The final score consists of nine variables, of which six are foods or food groups and three represent nutrients. The six food groups included fruits and berries (Nordic berries, such as bilberries and lingonberries, apples and pears), vegetables (tomatoes, lettuce, cucumbers, different cabbages, legumes and roots – potatoes excluded), cereals (rye, oats and barley), low-fat milk (fat-free milk and milk with fat content under 2 %), fish (salmon, Baltic herring and mackerel) and meat products as a negative component (beef, pork, processed meat products and sausage). We included the total fat of the diet expressed as a percentage of total EI E% to control for the amount of fat in the diet and calculated a ratio of PUFA:SFA and trans-fatty acids to illustrate dietary fat quality (e.g. high use of rapeseed oil and low use of butter). Alcohol consumption was also included in the score.
The score was calculated, with the exception of alcohol, according to the quartiles of consumption of each score component. We used quartiles instead of quintiles to obtain wide ranges between the points. For fruits and berries, vegetables, cereals, low-fat milk, fish and the fat ratio, the lowest quartile was coded as 0, the second lowest as 1, the third one as 2 and the highest quartile as 3. For meat products and total fat, the highest quartile was coded as 0, the second highest as 1, the third one as 2 and the lowest quartile as 3. Alcohol consumption was computed as ethanol intake. Men consuming 20 g or less and women consuming 10 g or less of alcohol per d received 1 point; otherwise, a 0 point was given. The resulting BSDS ranged from 0 to 25. Higher points indicated higher adherence to the Baltic Sea diet.
Statistical analysis
All analyses were conducted separately for men and women, and performed with the R statistical computing program, version 2.13.0(Reference Venables, Smith and Development Core Team26). A P value of < 0·05 was considered as significant. Descriptive statistics generated by BSDS quintiles included means with their standard errors by age, BMI and WC. Variables were considered as normally distributed using probability plots and histograms.
Linear regression was used to estimate linear trend in age, BMI, WC, EI and food groups (BSDS components) according to adherence to the Baltic Sea diet (quintiles) (lm procedure of the Base package in R). The χ2 test was used to estimate differences in smoking habits, education and PA, respectively (χ2 test procedure of the Stats package in R). The association between the adherence to the Baltic Sea diet and the decreased risk of obesity (categorical; BMI ≥ 25·0 kg/m2) and abdominal adiposity (categorical; WC ≥ 100 cm for men and ≥ 90 cm for women) was tested using logistic regression analysis (GLM procedure of the Epicalc package in R). For the risk analyses, we divided the final score into quintiles, where the highest quintile represents high adherence to the Baltic Sea diet. First, we used a simple age- and energy-adjusted model. Furthermore, we fitted multivariable-adjusted models, controlling for the following potential confounders: age (in years, continuous); EI (kJ/d, continuous); PA (categorical: inactive, moderately active, active and highly active). The likelihood ratio test (LRtest procedure of the Epicalc package in R) was used to test the significance of each variable in the model. Education and smoking did not have a significant impact in the model, thus they were not included in the final multivariable analyses. To account for the influence of BMI on WC, analyses of WC were conducted with and without adjustment for BMI (kg/m2, continuous). To take into account possible misreporting of EI, the ratio of reported EI:predicted BMR (EI:BMR) was calculated using the WHO guidelines(27), and participants were classified as either under-reporters (EI:BMR ≤ 1·14) or plausible reporters (EI:BMR >1·14) based on the cut-off points proposed by Goldberg et al. (Reference Goldberg, Black and Jebb28) and revised by Black(Reference Black29). Models were also run after stratification of age using sex-specific median (men: < 54 years and ≥ 54 years; women: < 53 years and ≥ 53 years).
Results
In the highest BSDS quintiles, participants tended to be older than participants in the lowest score quintiles (Tables 1 and 2). Both men and women in the highest BSDS quintiles had a greater intake of energy compared with the lower score quintiles (P< 0·0001). There were more physically inactive participants (P< 0·0001) and fewer highly educated participants (P< 0·01) in the lowest quintile v. highest quintile of the BSDS. About one-fifth of men and women were current smokers (men: 20·8 %; women: 14·5 %). The percentage of current smokers decreased by higher score quintiles in both sexes (P< 0·0001).
Table 1 Selected characteristics of the male participants by Baltic Sea Diet Score quintiles (Mean values with their standard errors or percentages)
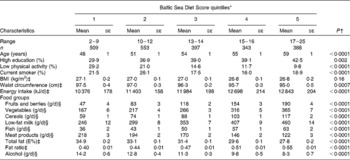
E%, percentage of energy.
* Baltic Sea Score components: fruits and berries (berries, apples, pears), vegetables (tomatoes, cucumbers, cabbages, roots, legumes, lettuce), cereals (rye, oats, barley), low-fat milk (fat-free and < 2 % fat), meat products (beef, pork, processed meat, sausage), fish, fat ratio (PUFA:SFA+trans-fatty acids), total fat content of the diet (E%), alcohol (as ethanol); scoring by quartiles 0–3 points (1st quartile, lowest consumption; 4th quartile, highest consumption); positive scoring (the more consumed, the higher points) was used for the other score components except meat products, which were scored negatively (the more consumed, the lower points). Men consuming 20 g or less of alcohol were given 1 point; otherwise, 0 point was given.
† P value was determined using linear regression for continuous variables and χ2 test for categorical variables. Significance testing was at P< 0·05.
‡ Values are age-adjusted means with their standard errors.
§ Values are age- and energy-adjusted means with their standard errors.
Table 2 Selected characteristics of the female participants by Baltic Sea Diet Score quintiles (Mean values with their standard errors or percentages)
E%, percentage of energy.
* Baltic Sea Score components: fruits and berries (berries, apples, pears), vegetables (tomatoes, cucumbers, cabbages, roots, legumes, lettuce), cereals (rye, oats, barley), low-fat milk (fat-free and < 2 % fat), meat products (beef, pork, processed meat, sausage), fish, fat ratio (PUFA:SFA+trans-fatty acids), total fat content of the diet (E%), alcohol (as ethanol); scoring by quartiles 0–3 points (1st quartile, lowest consumption; 4th quartile, highest consumption); positive scoring (the more consumed, the higher points) was used for the other score components except meat products, which were scored negatively (the more consumed, the lower points). Women consuming 10 g or less of alcohol were given 1 point; otherwise, 0 point was given.
† P value was determined using linear regression for continuous variables and χ2 test for categorical variables. Significance testing was at P< 0·05.
‡ Values are age-adjusted means with their standard errors.
§ Values are age- and energy-adjusted means with their standard errors.
According to the WHO criteria(20), the mean BMI of participants fell into the overweight category (men: 27·0 kg/m2; women: 26·0 kg/m2). In general, 60·8 % of men and 54·0 % of women were overweight or obese (BMI ≥ 25 kg/m2). No linear trend was found for BMI through the score quintiles. WC tended to decrease by higher adherence to the Baltic Sea diet in both men and women (P< 0·001).
The mean total BSDS was 13 points for both men and women. In the age- and energy-adjusted model, men's consumption of positive score components (fruits and berries, vegetables, cereals, low-fat milk, fat ratio and fish) substantially increased, and consumption of negative score components (meat products, total fat and alcohol) decreased due to higher score quintiles (P< 0·001; Table 1). The trend of women's consumption was similar, respectively (P< 0·0001; Table 2).
The results of the logistic regression analyses are presented in Table 3. The results for BMI showed no statistically significant association with the BSDS for either sex. In the age- and energy-adjusted model (model 1), men in the highest score quintile were 43 % (95 % CI 0·42, 0·78) less likely to have high WC compared with the lowest score quintile of the BSDS. For women, respectively, the odds were 30 % (95 % CI 0·52, 0·94) lower. In the multivariable model (model 2), the inverse association with abdominal obesity attenuated, but remained significant for men (95 % CI 0·29, 0·80). For women, the trend was similar, but did not reach statistical significance. After excluding potential under-reporters, the results regarding abdominal obesity remained the same, although the effect of exclusion was stronger in women (Table 3).
Table 3 BMI and waist circumference (WC) for level of adherence to the Baltic Sea diet (Odds ratios and 95 % confidence intervals)
* Baltic Sea Diet Score quintiles for men: 1st, 2–9 points; 2nd, 10–12 points; 3rd, 13–14 points; 4th, 15–16 points; 5th, 17–25 points; for women: 1st, 1–9 points; 2nd, 10–12 points; 3rd, 13–14 points; 4th, 15–17 points; 5th, 18–25 points.
† P value was determined using the likelihood ratio test to examine whether the Baltic Sea Diet Score was a strong predictor in the model. Significance testing was at P< 0·05.
‡ Adjusted for age and energy intake.
§ Adjusted for age, energy intake and physical activity. In waist, model was also adjusted for BMI.
∥ Adjusted for age, energy intake and physical activity excluding under-reporters. In waist, model was also adjusted for BMI.
¶ Cut-off for age is sex-specific median.
We analysed the risk of abdominal obesity separately for the younger and older participants using sex-specific medians of age as cut-offs (Table 3). For men under 54 years, the risk was 77 % (95 % CI 0·08, 0·62) lower in the highest compared with the lowest score quintile. The comparable value for women under 53 years of age was 83 % (95 % CI 0·05, 0·58). For older men and women, no statistically significant associations were found.
We evaluated the associations between WC and the BSDS components to find out which of the score components contributed the most to the risk of abdominal obesity. The participants in the highest quartile of cereal consumption had a lower risk of abdominal obesity compared with those in the lowest cereal consumption quartile (Table 4). Men who consumed 20 g or less of alcohol per d on average had a 43 % lower risk of abdominal obesity compared with men who consumed over 20 g of alcohol per d on average (95 % CI 0·39, 0·85). For women, the trend was similar, but not statistically significant. The other individual BSDS components were not related to WC.
Table 4 Waist circumference for quartiles of the Baltic Sea Diet Score components*† (Odds ratios and 95 % confidence intervals)
E%, percentage of energy.
* Model adjusted for age, energy intake, physical activity and BMI.
† High waist circumference was defined as ≥ 100 cm for men and ≥ 90 cm for women.
‡ Participants in the higher quartiles of presumably beneficial effects were assigned higher points than participants in the lowest quartile. In contrast, participants in the lower quartiles of presumably detrimental effects were assigned higher points than participants in the highest quartile. Cut-off points of the quartiles (1st, 2nd, 3rd cut-off) for men: fruits and berries (g/d) 31·9, 73·4, 147·5; vegetables (g/d) 138·0, 216·3, 323·8; cereals (g/d) 49·1, 77·9, 114·5; fish (g/d) 26·1, 42·9, 61·0; low-fat milk (g/d) 37·5, 214·7, 537·5; meat products (g/d) 105·3, 154·3, 216·5; fat ratio 0·38, 0·46, 0·53; total fat (E%) 27·8, 31·0, 34·4; cut-off points for women: fruits and berries (g/d) 50·4, 115·3, 211·5; vegetables (g/d) 176·6, 271·7, 408·2; cereals (g/d) 45·8, 74·6, 106·8; fish (g/d) 19·2, 30·3, 45·7; low-fat milk (g/d) 28·4, 170·0, 438·4; meat products (g/d) 64·5, 96·3, 135·2; fat ratio 0·38, 0·46, 0·56; total fat (E%) 27·3, 30·4, 33·6.
§ P value was determined using the likelihood ratio test to examine whether each Baltic Sea Diet Score component was a strong predictor in the model. Significance testing was at P< 0·05.
∥ Low-fat milk group included fat-free milk and milk < 2 % of fat.
¶ Ratio of PUFA:SFA and trans-fatty acids.
** Men who consumed 20 g or less and women who consumed 10 g or less of alcohol received 1 point; otherwise, 0 point was given. Thus, for alcohol, the reference group is 0 and adherence to the Baltic Sea diet is 1.
We tested whether the inverse association between the BSDS and WC is driven only by cereal and alcohol components. First, we conducted analyses excluding the cereal and alcohol component from the score. In women, only the cereal component was excluded as alcohol alone did not have an association with WC. In both sexes, the results did not change substantially in the age- and energy-adjusted model (1st v. 5th quintile; men: OR 0·59, 95 % CI 0·26, 0·98, P= 0·01; women: OR 0·71, 95 % CI 0·54, 0·95, P= 0·008) or in the multivariable model (1st v. 5th quintile; men: OR 0·63, 95 % CI 0·38, 1·04, P= 0·019; women: OR 0·73, 95 % CI 0·45, 1·19, P= 0·12). Second, we also conducted the analyses using only cereal and alcohol as components in the score. Again, the results remained significant (1st v. 5th quintile; men: OR 0·42, 95 % CI 0·27, 0·65, P =0·002; women: OR 0·50, 95 % CI 0·31, 0·80, P= 0·025).
Discussion
The present study suggests that the Baltic Sea diet may be related to abdominal fat distribution. Subjects with high adherence to the Baltic Sea diet were less likely to have an excessively large WC, which is independent of BMI, compared with subjects with low adherence to the diet. After adjusting for relevant confounding factors, the association remained significant, although it was no longer statistically significant in women. Participants in the younger age groups were more likely to benefit more from the Baltic Sea dietary pattern than the older age groups. No association was found between the Baltic Sea diet and BMI. The potential mechanisms by which the Baltic Sea diet may have desirable effects on abdominal adiposity could be especially the diet's high fibre content (from rye, oats and barley) together with moderate alcohol consumption.
It is generally considered that excess abdominal fat is more pathogenic than excess subcutaneous fat. Excess abdominal fat is associated with insulin resistance and CVD in both sexes(Reference Wassink, van der Graaf and van Haeften8, Reference Sofi, Cesari and Abbate15, Reference Sofi, Abbate and Gensini16, Reference Canoy30–Reference Vazquez, Duval and Jacobs34). The results from a Spanish population(Reference Salas-Salvado, Bullo and Babio35, Reference Salas-Salvado, Fernandez-Ballart and Ros36) showed that a prevalence of metabolic syndrome and diabetes incidence can be lowered by adherence to the Mediterranean diet without weight reduction and change in PA. This is in line with the present findings on inverse associations between the BSDS and abdominal adiposity. Hyperglycaemia induced by increased release of NEFA from abdominal fat and decreased release of insulin from pancreatic β-cells leads to vascular damage and accelerates the formation of atherosclerotic plaque(Reference Scaglione, Di Chiara and Cariello37–Reference Elks and Francis39). Thus, abdominal fat appears more suitable as a measure of the risk of chronic diseases than does overall obesity (BMI)(Reference Huxley, Mendis and Zheleznyakov5–Reference Schneider, Friedrich and Klotsche7, Reference Qiao and Nyamdorj40).
The health-promoting effects of the Mediterranean diet have been in focus for the last two decades. In cross-sectional and prospective studies, a low Mediterranean Diet Score has predicted obesity and abdominal adiposity(Reference Beunza, Toledo and Hu41–Reference Kastorini, Milionis and Esposito43). In the EPIC-PANACEA (European Propective Investigation of Cancer and Nutrition – Physical Activity, Nutrition, Alcohol, Cessation of smoking, Eating out of home and obesity) study, BMI was not associated with a modified Mediterranean Diet Score, but a significant inverse association was found between WC and the score in both sexes(Reference Romaguera, Norat and Mouw44). In a recent meta-analysis, the combined effects of five cross-sectional studies and fourteen clinical trials revealed that a high adherence to the Mediterranean diet was associated with a reduced risk of WC compared with a low adherence to the Mediterranean diet(Reference Kastorini, Milionis and Esposito43). Most of the individual studies included in the meta-analysis, however, showed no significant associations between WC and the Mediterranean Diet Score. In addition, most of the clinical trials that evaluated the effects of the Mediterranean diet on WC were short-term trials. However, the present study related to the Baltic Sea diet is in line with these findings, although the scoring method and cut-off values were not the same in the BSDS and the Mediterranean Diet Score.
A diverse diet can be constructed in various ways. The Mediterranean diet is one serious diverse diet that has been under wide debate also in Finland. The aim of the Baltic Sea diet is to show that a healthy diverse diet can be constructed also from the local foods. The local resources enable and facilitate gathering the healthy diet from foods that naturally grow in their neighbourhood or which they can cultivate with no substantial costs and support ecological aspects. Furthermore, food culture determinates the social and psychological acceptance of foods, and therefore local well-known foods that are already part of the culture are usually better adopted to the diet than foreign foods.
Hypotheses suggest that the Nordic diet has multiple health effects for Nordics. Recent randomised clinical trial on Swedish hypercholesterolaemic subjects suggested that the Nordic-style diet reduces cardiovascular risk factors(Reference Drake, Gullberg and Ericson45). In addition, results from a Danish cohort of men and women showed a significant inverse association between the Nordic food index (which illustrates high use of apples and pears, cabbages, roots, rye bread, oatmeal and fish) and total mortality(Reference Olsen, Egeberg and Halkjaer46). In Finland, the SYSDIET study, together with the Finnish Heart Association and the Finnish Diabetes Association, created a Baltic Sea Diet Pyramid based on Nordic dietary habits that emphasises high consumption of berries, local vegetables and whole-grain cereals, such as rye, oats and barley, fish, and rapeseed oil, together with a low consumption of red and processed meat. The present results from the BSDS support the hypothesis that it is possible to construct a healthy-weight diet from Nordic foods.
The present results indicate that a whole diet described by a dietary score predicts decreased risk of abdominal obesity. In large population-based studies, it has been observed that several foods have either an independent positive or negative association with long-term weight gain and annual change in WC(Reference Mozaffarian, Hao and Rimm47, Reference Romaguera, Angquist and Du48). Individuals who increased their intake of beneficial foods and decreased the intake of harmful foods gained less weight compared with those who did not change their diet(Reference Mozaffarian, Hao and Rimm47). In other words, if we rely on one healthy food, but the overall quality of the diet is low, it is likely that all unhealthy foods in the diet will compensate for the positive effect, which would make the measurement of only one food item irrelevant. The present study also suggests that some single foods (cereal and alcohol) have a greater effect on abdominal obesity, and the measurement of only these foods might be enough to assess the risk of abdominal obesity. However, most of the dietary scores, such as the BSDS, were developed to illustrate a general healthy diet, and expected to have multiple beneficial effects on health. Other score components than those that predicted abdominal obesity might reveal to be more important when assessing metabolic risk factors, such as markers of inflammation or lipid fractions. Thus, a whole diet-based approach (dietary score) may be a better tool to evaluate the impact of dietary components on overall health (including obesity), even individual foods could be used to assess some specific diseases.
We found that in the younger age groups, a higher adherence to the Baltic Sea diet was more strongly inversely associated with abdominal adiposity. In participants in the younger age groups, there could be more variation from the Baltic Sea-style diet compared with modern-style diets. Younger people are also gaining more weight in Finland(Reference Lahti-Koski, Seppänen-Nuijten and Männistö4). One explanation to the attenuation observed in the trend of the risk between the highest and the lowest score quintile in women could be that there were more older women in the highest compared with the lowest score quintile. Another possible explanation for this is the fairly low number of subjects in the highest score quintile. It is also known that women are generally less likely to have abdominal obesity than men. Furthermore, it is acknowledged that the greatest loss of participants is in the group of young subjects, especially among men. It could be that those young subjects who participated had healthier diets than those who did not.
The strengths of the present study included a large and representative sample with a participation rate at an acceptable level. We used a validated FFQ and internationally standardised anthropometric measurements(Reference Tolonen, Koponen and Aromaa19, Reference Paalanen, Männistö and Virtanen22–Reference Männistö, Virtanen and Mikkonen24). The study included some limitations, too. The FFQ might have influenced the exposure assessment, because the questionnaire measures the habitual diet over the last 12 months, while obesity is generated over several years. Because of the cross-sectional design of the present study, we do not have information on the participants' earlier weights and eating patterns. Thus, reverse causality is also possible. Under-reporting that generally relates to nutrition research can lead to results that are more of an underestimate of the relationship between the Baltic Sea diet and abdominal adiposity. After exclusion of under-reporters, the present results remained significant, though the effect of the exclusions was stronger in women. Furthermore, the phenomenon that health-conscious people are more likely to participate in health surveys may have affected the present results.
A dietary score also has its weaknesses. The selection of the food groups and nutrients, as well as the scoring of the selected components, is made through subjective decisions, although we carefully based our selections on the Baltic Sea diet. As recommended, we did not use single cut-off points, but instead used scoring ranges. We also included total fat in the score to ensure an overall balance of fat intake, and we adjusted the analyses for total EI(Reference Waijers, Feskens and Ocke49). Although a predefined score, such as the BSDS, enables better capture of the exposure of interest and diminishes nutritional confounding, some confounding due to correlations with the intake of various dietary factors and existing nutrient–nutrient interactions still remains.
The present study shows that it is possible to construct a healthy-weight diet from Nordic foods, especially rye, oats and barley together with moderate alcohol intake, which seems to have a beneficial effect on abdominal fat distribution. This finding may be useful for dietary counselling and the prevention of abdominal obesity. Nevertheless, given the limitations of the present cross-sectional study, future prospective studies are needed to confirm these results.
Acknowledgements
This study was supported by the Academy of Finland (136895 and 141005). N. E. K. and S. M. participated in the design and conduct of the research. N. K., S. M. and U. S. were responsible for creating the BSDS. N. K. performed the statistical analyses, wrote the manuscript and had primary responsibility for the final content. S. M. was responsible for the original study idea and revised the manuscript for publication. All authors read and approved the final manuscript. The authors declare that they have no personal or financial conflicts of interest.






