Psychiatric in-patient care is a scarce and expensive resource in healthcare systems across the world. Admission to hospital is usually a last resort for the most acutely unwell patients, and consequently the majority of in-patients have a psychosis diagnosis.1 Patient satisfaction with the care they experience during an in-patient admission is generally low.Reference Csipke, Flach, McCrone, Rose, Tilley and Wykes2, Reference Csipke, Williams, Rose, Koeser, McCrone and Wykes3 A common source of dissatisfaction with acute in-patient care is the lack of access to psychological therapies, as an adjunct to medication.Reference Wood and Alsawy4 Good practice guidelines for in-patient wards recommend access to evidence-based psychological therapies.5 However, it is not clear what constitutes an evidence-based in-patient psychological therapy. International treatment guidelines for schizophrenia recommend cognitive–behavioural therapy (CBT) for psychosis.6–Reference Dixon, Dickerson, Bellack, Bennett, Dickinson and Goldberg8 However, these recommendations are largely based on trials conducted in community settings. At the time of writing the protocol for the current review, no systematic reviews or meta-analyses focusing solely on psychological interventions for psychosis within in-patient settings had been either published or registered on the PROSPERO database. The aim of the current paper was therefore intended mainly as a ‘scoping’ review. This kind of review is used to find out the potential size and scope of the available research literature, and may include ongoing or planned research.Reference Grant and Booth9 Scoping reviews are particularly relevant to areas of healthcare where it is not clear whether the evidence exists to answer a more precise question, such as the effectiveness of a particular therapy within a particular setting. The aim of this review was therefore to explore and map out the evidence base for psychological therapies for psychosis within acute in-patient settings.
Method
A review protocol was written and registered in the public domain before searching and data extraction began (PROSPERO Registration: CRD42015025623). Five review questions were set in advance:
(a) What is the current state of the evidence base for psychological therapies for psychosis within acute psychiatric in-patient settings?
(b) What study designs are used to evaluate psychological therapies for psychosis within acute in-patient settings?
(c) How are psychological therapies for psychosis within acute psychiatric in-patient settings evaluated, and what are considered to be the key outcome measures?
(d) What healthcare professionals are involved in delivering psychological therapies for psychosis, and in which roles (for example sole therapist, group cofacilitator, clinical supervisor)?
(e) How are psychological therapies for psychosis adapted for use within acute psychiatric in-patient settings?
We included only studies published in English, with no date restrictions on searches. Searches were initially run in September 2015, and updated in December 2016. We planned to include a wide range of different study types to address the main review question pertaining to the current state of the evidence base. We anticipated that there would be relatively few eligible randomised controlled trials (RCTs), and the majority of studies would be small-scale, uncontrolled, non-randomised studies. Eligible studies therefore included RCTs, uncontrolled studies, observational studies, case studies, study protocols and qualitative studies. We searched for studies on psychological therapies for psychotic symptoms within acute psychiatric in-patient care (adult wards only).
We defined inclusion based on the care setting, rather than solely the diagnosis of patients, on the basis that acute care is not diagnosis-specific in most countries, and not all patients receiving in-patient care may yet have an established diagnosis. We defined acute psychiatric care as including triage/acute assessment wards, general acute wards and psychiatric intensive care units. Non-acute in-patient care settings were excluded (for example rehabilitation wards, specialist units, residential therapy units). Non-in-patient acute services were also excluded (for example day hospitals, crisis/home treatment teams).
We included any psychological intervention/therapy aimed at alleviating distress or impairment to functioning arising from psychotic symptoms (such as voices, delusions) or aimed at emotional difficulties commonly associated with psychotic symptoms (such as anxiety, depression). This therefore excluded compliance therapy, and any intervention focused primarily on improving psychiatric ‘insight’. We included individual, family and group therapies, delivered by any healthcare professional, of any length, frequency or duration, but not purely staff-based interventions, therapeutic community or milieu therapy. We included any therapies started within the acute in-patient setting, whether or not the therapies continued post-discharge.
We included CBT-based psychological therapies, broadly defined as a talking therapy based on an underlying theoretical model of the relationship between thoughts, emotions and behaviours. So-called third-wave cognitive therapies including mindfulness, acceptance and commitment therapy, meta-cognitive therapy, dialectical–behavioural therapy and compassion-focused therapy were included and classified as subtypes of CBT. Non-CBT-based therapies such as psychodynamic therapy were also included. Cognitive-remediation therapy was excluded on the basis that it is aimed primarily at remediating cognitive deficits rather than emotional difficulties associated with psychotic symptoms (likewise any intervention such as social skills training that is focused primarily on the remediation of functioning). Arts therapies including art, drama and movement therapy were also excluded. Studies with any, or no control conditions, were included. The search strategy and search terms for each resource is available online in Supplementary Table 1 available at https://doi.org/10.1192/bjp.2018.106.
Eligible studies were identified by the primary (P.J.) and secondary (K.H.) reviewer. In the first stage, P.J. independently screened all titles and abstracts identified from searches to determine which met the inclusion criteria. In the second stage, P.J. and K.H. both independently screened full-text articles for inclusion or exclusion, with discrepancies resolved by discussion. For included studies, we linked multiple reports from the same study, so that each study (rather than each report) was the unit of interest in the review. A standard data-extraction template was used to record relevant information from each included study. Data for each study were extracted by either P.J. or K.H., with each reviewer cross-checking each of the other reviewer's forms to ensure consistency and accuracy of data extraction.
In keeping with the range of this ‘scoping’ review, the quality of eligible studies was assessed using the Mixed Methods Appraisal Tool (MMAT).Reference Pluye10 The MMAT is designed to assess quantitative, qualitative and mixed-methods studies using a single integrated tool. The initial stage involved assessing each study according to two standard screening questions (is there a clear research question, and do the data collected address this question). Further assessment with the MMAT was not feasible or appropriate for studies that failed the screening questions, or which did not report any outcomes (whether quantitative or qualitative). The second stage involved assessment under one of five categories, depending on the type of study, each with four assessment criteria. A summary score was calculated by dividing the number of criteria definitely met (i.e. scored as a ‘yes’) divided by four, and expressed as a percentage. Quality scores therefore ranged from 0, 25, 50, 75 to 100%. We additionally assessed the RCTs using the Cochrane Risk of Bias criteria.Reference Higgins, Altman, Gøtzsche, Jüni, Moher and Oxman11
Results
As shown in Fig. 1, we identified 65 studies for inclusion in the review. We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines in summarising the search results (see Supplementary Table 2 for the PRISMA checklist).Reference Moher, Liberati, Tetzlaff and Altman12 Fourteen of the 65 studies were linked to at least one other record (for example Drury et al Reference Drury, Birchwood, Cochrane and MacMillan13 was published as three peer-reviewed journal articles as well as a PhD thesis). In this case, where at least one of the records was a peer-reviewed journal article, this was taken as the ‘primary’ reference. In the case of RCTs, which often published acute-phase and follow-up data in separate journal articles, the paper that had been published first was designated as the primary paper. However, the data extraction form was completed using all relevant information across all linked studies. Overall, 58 out of the 65 studies had a peer-reviewed journal article designated as the primary paper. Of the remaining studies, four were published solely as book chapters, one was published as a PhD thesis and we could not find any subsequent published journal articlesReference Cholet14 and the remaining two existed only as trial registry records – one of these had not yet been published in a peer-reviewed journal because the trial was still ongoing,Reference Gaudiano15 and the other reported results on the trial registry website but we could find no evidence of subsequent publication in a peer-reviewed journal.Reference Boden16
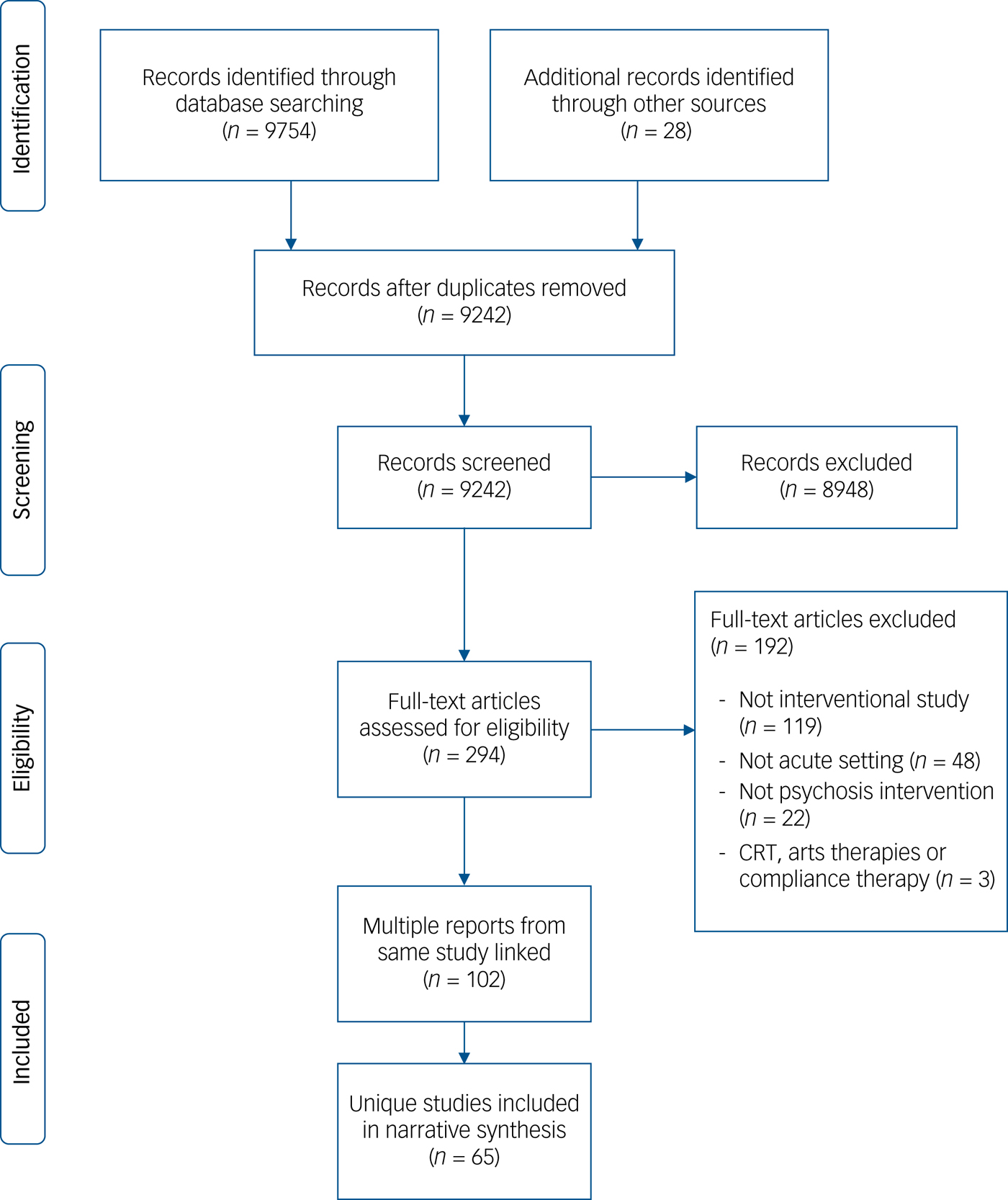
Fig. 1 PRISMA flowchart.
Review question 1: current state of evidence base
Sixty-five studies were included in the review (see online Supplementary Table 3). Overall, 40% of studies failed the initial MMAT screening stage (26/65). Of the remaining 60% (n = 39) which were assessed further, 21.5% (n = 14) were rated as high quality, 20% (n = 13) were medium quality and 18.5% (n = 12) were low quality. We broadly categorised therapies into CBT, and non-CBT models, with subtypes of therapy noted where appropriate. Overall, we found there were slightly more CBT studies (n = 35) than non-CBT therapies (n = 28). We took a broad definition of therapy models, but even so were unable to categorise two studies into a recognisable therapy model (Dichos therapyReference Aviera17 and computer-facilitated therapyReference Ahmed, Bayog and Boisvert18).
Among the CBT studies, there was a noticeable increase in so-called third-wave cognitive therapies in recent years, with 12 studies categorised as either mindfulness, compassion-focused, or acceptance and commitment therapy. The majority of the non-CBT studies were psychodynamic (n = 17). A clear difference emerged between countries in their dominant therapy models. For the UK studies, over 75% were CBT based (16/20). However, the reverse was true for the USA studies, with 62% of studies being non-CBT based (16/26). For other countries (which were predominantly European), CBT and non-CBT studies were more evenly balanced (11 CBT and 8 non-CBT). The first CBT studies did not emerge until the 1980s, but they represent the majority of studies included in the review published since 2000.
In order to provide a broad overview of the main findings of the studies in the review, relevant studies were identified according to four criteria. These were (a) the stated aim of the study was described as evaluating efficacy/effectiveness; (b) the study reported at least one outcome measure; (c) the study stated which was the primary outcome measure, where multiple outcomes were reported; and (d) the study passed MMAT screening stage. Twelve studies in total met all these criteria and are summarised in Table 1, in chronological order.Reference Cholet14, Reference Bookhammer, Meyers, Schober and Piotrowski19–Reference Moritz, Veckenstedt, Randjbar, Vitzthum and Woodward29 No exclusions were made based on study quality, therefore the findings should be interpreted with appropriate caution, and in the context of the associated MMAT quality scores (see Supplementary Table 3).
Table 1 Summary of main findings (efficacy studies with primary outcomes only)
RCT, randomised controlled trial; TAU, treatment as usual; CBT, cognitive–behavioural therapy.
Review question 2: types of study design (including quality assessment)
As expected, a full range of study designs were included in the review, from single case studies to large-scale RCTs. RCTS were more likely to describe CBT, rather than non-CBT interventions and the converse was true for non-RCTs. Service evaluation, case series/studies and qualitative studies were more evenly matched between CBT and non-CBT models. Quality assessment scores were variable across different categories of study designs. For the RCTs (n = 21), there was evidence of an improvement in quality over time, as all studies published pre-2000 were rated as low–medium quality (0–50%), but post-2000 included at least five studies rated as high quality (75–100%). This probably reflects improvements in trial reporting guidelines arising from the first publication of the CONSORT statement in the 1990s,Reference Begg, Cho, Eastwood, Horton, Moher and Olkin30 and its subsequent adoption by most major journals.
In addition to the MMAT, we also assessed RCTs using the Cochrane Risk of Bias (see online Supplementary Table 4). Overall, the risk of bias was lower for attrition and reporting bias, with most RCTs reporting <20% loss to follow-up at trial end-point, and appropriately reporting prespecified trial outcomes. However, randomisation methods, allocation concealment and masking were causes for concern (Fig. 2). Only two of the RCTs clearly stated using the ‘gold standard’ of an independent randomisation service with randomly varying block sizes, with a large number of studies not specifying the randomisation method at all (n = 10). A minority of studies mentioned masking of outcome assessors, and masking of the in-patient and/or community teams potentially involved in treatment decisions. Size of trials was also a concern – out of the 19 RCTs with published results, over half (n = 10) had fewer than 25 people in the treatment arm. Finally, most of the RCTs used treatment as usual (TAU) (or ‘enhanced’ TAU in the Gaudiano and Gaudiano & Herbert trials)15,31 as the control arm (n = 11), and therefore did not control for non-specific therapy factors such as time and attention from a warm, empathic therapist. A minority of trials did use an active control arm. One of the largest trials had a strong design in this respect, and included both a supportive counselling and TAU condition, with over 100 participants in each arm.Reference Lewis, Tarrier, Haddock, Bentall, Kinderman and Kingdon25
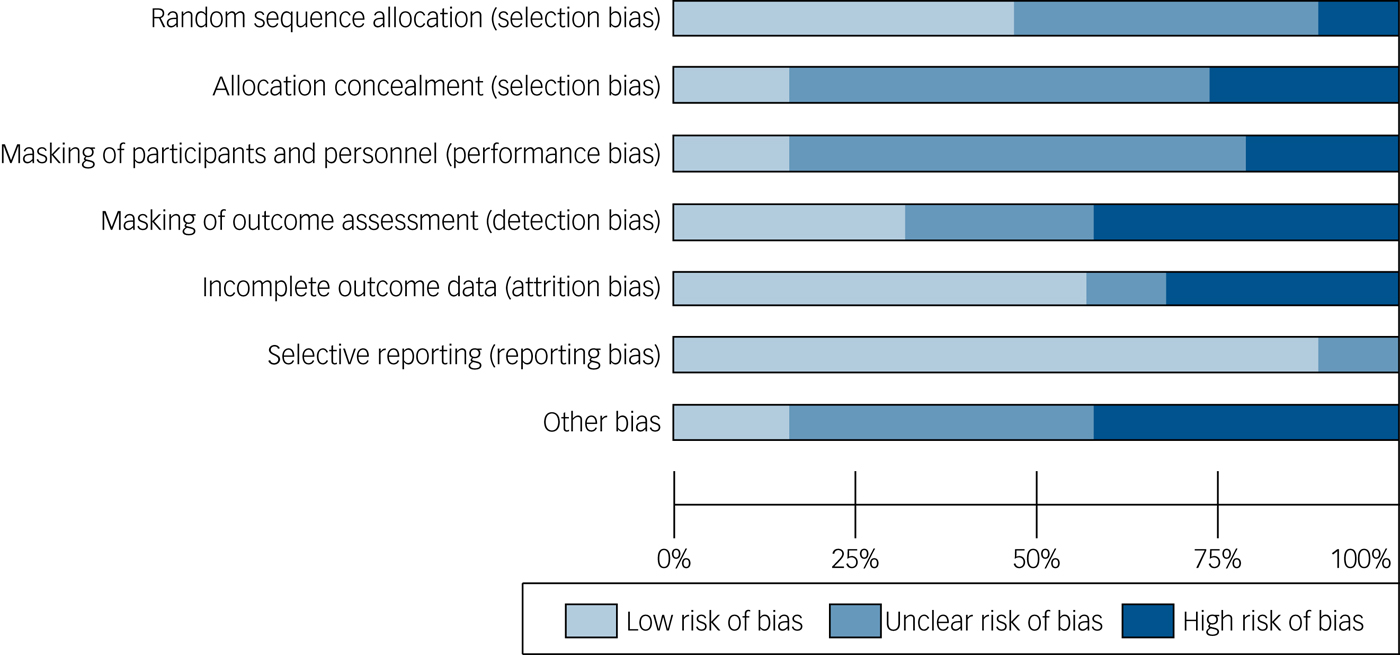
Fig. 2 Risk of bias summary for randomised controlled trials presented as percentages across included studies (n = 19).
Review question 3: evaluation and outcome measures
Most of the studies included in the review reported collecting some kind of outcome measure (n = 48). We categorised the outcome measures used into five main categories (psychotic symptoms, affective symptoms, general/clinical functioning, recovery, and readmission/relapse). The results are summarised in Table 2. Where outcome measures were reported, these were usually focused on assessing psychotic symptoms and/or general functioning. There were relatively few studies that reported assessing affective symptoms, such as depression or anxiety. Only 3 of the 65 studies used self-report recovery measures. Even though they were not usually the primary outcome measure, many studies reported readmission/relapse data. The timing of outcome assessments was variable, and usually included a combination of different time points (for example baseline, discharge and 6-month follow-up). The assessment schedule was not specified in two studies. For the remaining 46 studies, 32 reported data at baseline, 12 reported outcomes session-by-session, 4 at mid-therapy and 26 at discharge/end of therapy. Twenty-one studies reported follow-up data beyond the end of therapy. The longest follow-up point was 6 months or less for 10 studies, and longer than 6 months for the remaining 11 studies.
Table 2 Summary of outcome measures for those studies reporting any kind of outcome (n = 48 studies including 21 randomised controlled trials (RCT))
a. Some studies included more than one scale within the same domain.
Review question 4: delivery of therapies
The most common mode of delivery was group therapy (n = 27), followed by individual therapy (n = 19). There was a notable difference in the types of trial design between group and individual treatment modalities. The majority of the studies describing individual therapies were RCTs (12/19), compared with 3 of 27 of the group therapy studies.
As anticipated, a variety of staff groups were involved with delivering psychological therapies within in-patient settings, including psychologists, psychiatrists, nurses, occupational therapists, social workers, family therapists, CBT therapists and clinical trainees from different disciplines. It was notable, however, that almost a third of the studies included in the review failed to specify the professional group delivering the intervention. This limits the interpretation and replicability of such studies. The primary, or sole, therapist was described as a clinical psychologist in the majority of studies where the profession was specified (n = 14).
Training, supervision and checks on treatment fidelity were generally poorly described or entirely absent. Over 50% of studies included in the review gave no details about training and supervision of therapists. For the 21 RCTs in the review, only a third of studies (n = 7) clearly reported that the staff delivering the intervention were both trained and supervised. An additional third reported either staff training or supervision, but not both. The final third gave no details on either. The majority of RCTs gave no details on checking treatment fidelity. Only eight studies reported fidelity checks – this was usually done by an independent rater reviewing a sample of audiotapes of therapy sessions (n = 6), but the use of direct observation (n = 1) and videotapes (n = 1) was also reported.
Review question 5: adaptations to facilitate delivery within acute settings
After an initial review of the included studies, we identified and categorised studies according to five main adaptations. These were (a) increased frequency of sessions (≥2 sessions a week), (b) briefer interventions (≤5 sessions), (c) shorter sessions (<50 min standard length of sessions), (d) use of single-session format (i.e. each session is stand-alone, although therapy may include more than one session) and (e) continuing therapy post-discharge.
The most common adaptation was an increased frequency of sessions. An increased frequency of sessions sometimes reflected an attempt to deliver a larger number of sessions within a shorter period of time to fit the typical length of an in-patient admission. Other studies aimed to deliver a smaller number of sessions, but still had an increased frequency of sessions to fit in with short lengths of admissions.Reference Bach and Hayes23, Reference Gaudiano and Herbert31 Only a quarter of studies reported briefer interventions (15/65), with five or fewer planned sessions. This is perhaps surprising given concerns that acute admissions are short, and so there is limited time to provide psychological therapies. However, the number of planned sessions, or the average number of sessions delivered per patient, was often not stated and we were unable to extract this information for many studies. We found that the use of the standard therapy ‘hour’ (i.e. around 50 min) was in fact the most commonly reported length of session (41/65).
Over a third of studies reported using a single-session format (24/65). This may be particularly helpful in settings when length of admission is unpredictable, and discharges may occur unexpectedly in the middle of treatment. Single-session formats may be particularly useful in groups, in meeting the needs of people who may attend only one session, but also in allowing people to flexibly ‘drop in’ over the course of an admission. In relation to group interventions, the use of single-session formats is of course closely linked to whether the group is open (people can join and leave at any session) or closed (people can join only at the beginning and are encouraged to stay for the full course). We found that open groups were the most common format reported (n = 17), with only two studies explicitly reporting a closed group format.Reference Cooper32, Reference Owen, Sellwood, Kan, Murray and Sarsam33 It was not always clear whether group formats were open or closed. There was some reference to continuing therapy post-discharge in 13 studies. This was sometimes to allow people to complete a set number of sessions, for a groupReference Bechdolf, Knost, Kuntermann, Schiller, Klosterkötter and Hambrecht34 or individual intervention.Reference Bach and Hayes23 Some studies offered booster sessions post-discharge, but take-up of these was generally low.Reference Lewis, Tarrier, Haddock, Bentall, Kinderman and Kingdon25, Reference Haddock, Tarrier, Morrison, Hopkins, Drake and Lewis35
Discussion
We conducted a systematic scoping review of psychological therapies for psychosis within acute in-patient settings. We found that there were a broad range of therapies in the published literature, delivered in many different ways, by different groups of professionals, and evaluated using a wide range of approaches. This makes a coherent synthesis of current evidence challenging. Quality was varied across different study types and over time, but we found significant methodological weaknesses in many studies, including in RCTs. Such a high degree of heterogeneity surely provides a challenge to any quantitative synthesis of findings by means of a meta-analysis. Reporting of diagnosis or symptom profile is also inconsistent in the literature – and indeed, in practice often there is no clear diagnosis for in-patients. For this reason the present review took the pragmatic step of selecting studies on the basis of setting (acute in-patient) and type of psychological therapy (such as CBT for psychosis). We would recommend that all future in-patient research on psychological therapy for psychosis reports diagnostic information on participants where available, in addition to symptom profiles using established assessment tools.
Evaluating therapies within in-patient settings is undoubtedly challenging. It is not possible, or indeed ethical, to control or keep constant all other elements of treatment each person is receiving, such as medication, nursing care or occupational therapy. Attributing change, whether it be improvement or deterioration, to any single component of treatment is therefore not normally possible. There is also the problem of accounting for ‘natural’ recovery after a mental health crisis. The added value of any psychological intervention should therefore always be carefully assessed.
Outcome assessment
The present study focused on patient outcomes – as opposed for example to change in ward milieu or in staff well-being. Direct patient outcomes can relate to well-being during admission (for example psychotic symptoms, length of admission), or after (such as subsequent relapse or readmission rates), or both. The studies reviewed included a wide range of primary and secondary outcomes and assessment tools, making it difficult to draw conclusions. The field may therefore benefit from the development of an agreed standardised set of outcomes, known as ‘core outcome sets’ (COSs). A COS can be used as the minimum to be reported for any study or trial and makes it easier to combine and compare the results of studies, over time and from different countries. The urgent need for a COS in psychosis can be no better demonstrated than by the findings of a recent review of schizophrenia intervention trials (both drug and psychological therapy trials) that found 2194 different scales were used to measure outcomes, with every fifth study introducing a new rating instrument.Reference Miyar and Adams36 We would encourage development of COSs for in-patient research that address core outcomes both during and post-admission.
Therapy delivery
Only 3 of 27 evaluations of group therapies used an RCT design, which may reflect methodological challenges in evaluating in-patient groups – in-patient group therapies are normally open to everyone on a ward, for ethical and practical reasons, and there is also increased risk of treatment ‘contamination’ between conditions on in-patient wards where patients are in close proximity. One potential solution is to use a cluster randomised design, where individual wards are randomised to a particular intervention, rather than individual patients, although there are often important differences between wards (for example catchment area, therapeutic milieu) and larger sample sizes are needed, which is often a barrier to conducting this kind of study in routine clinical practice.Reference Torgerson37
Adapting therapy protocols for in-patient settings
The majority of studies reported having adapted psychological therapy for delivery within in-patient settings. Commonly this meant offering traditional numbers of sessions but more frequently, or offering fewer sessions or developing a single-session format. We would recommend that future research describe more clearly the process of adapting therapies and protocols: for example, giving a clear rationale for the need to adapt a therapy; a clear rationale for the chosen adaptations; a clear statement about if and how the adaptations were piloted (such as a small case series); being clear about the degree of patient consultation and participation throughout the process. Furthermore, future research might examine, perhaps through mixed methods, the impact of the specific adaptations made.
Strengths and limitations
As this review was planned as a scoping review, we designed the strategy accordingly, and published our search strategy and review questions in advance on the PROSPERO database. A particular strength of this review is that we searched for literature from a wide variety of sources, including those not readily available (such as non-digitised book chapters, unpublished PhD theses). However, work not published in academic journals has not been subject to the same degree of peer review or scrutiny, and therefore should be interpreted with caution. We also attempted to search for studies underway as well as completed, by searching trial registries for planned or ongoing research, and by contacting experts in the field. However, despite increasing calls for all trials to be pre-registered on a public registry, compliance is still variable. Therefore, we cannot exclude the possibility that there is work underway that we would not have found from registry searches. There were some challenges in defining acute care for the purposes of this review, as care settings vary from country to country, and over time within the same country. We therefore adopted a liberal definition of acute care, and erred on the side of being over-, rather than underinclusive. In circumstances where the care setting was unclear or did not easily fit into standard categories of in-patient care, we focused on assessing the eligibility of the intervention itself, and included interventions that seemed feasible to deliver within an average 30-day admission. However, difficulties in defining key terms in the search strategy may have led to relevant studies being excluded, or less relevant studies being included in the final review.
Implications for practice
As this was a scoping review rather than a formal attempt to synthesise efficacy data, we cannot draw any firm conclusions in terms of what psychological interventions are most efficacious within acute in-patient settings. However, from the efficacy studies summarised in Table 1 there appears to be some promising evidence for the role of CBT-based approaches in reducing psychotic symptoms and reducing risk of relapse over the short-term. A systematic approach is now clearly needed to develop the evidence base for in-patient psychological interventions, and to progress from promising pilot studies to larger, well-designed RCTs in line with guidelines for developing complex interventions.38 The nature of in-patient care has undoubtedly changed over the more than 60 years covered by this review; for example, in UK settings, there has been a move towards shorter acute admissions and an increasing proportion of involuntary admissions.1 This not only poses new challenges for in-patient therapies in terms of developing briefer interventions, which can be effectively integrated within a larger care pathway, including community and crisis services, but also highlights opportunities for acute care to be a time to engage patients in psychological therapies that may outlast the admission. Qualitative research (including pre-trial assessment) also has a role to play, for example in optimising use of interventions within RCTs and in informing future choice of interventions.Reference O'Cathain, Thomas, Drabble, Rudolph and Hewison39 COSs are required to establish common, minimum outcomes both during and post-admission, and the process of adapting therapies for in-patient settings needs greater methodological rigour and clarity.
Funding
This paper presents independent research funded by the National Institute for Health Research (NIHR). P.J. is supported by a NIHR Doctoral Research Fellowship (DRF-2014-07-003). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2018.106.







eLetters
No eLetters have been published for this article.