CLINICAL SCENARIO
A 32-year-old male presents with diffuse myalgias, weakness, and dark urine for 1 day. The patient states he recently started a new exercise program. He is hemodynamically stable, and his physical examination reveals diffuse muscle tenderness. His creatine kinase (CK) returns at 8,000 international units per liter (IU/L), and his urinalysis reveals blood but only three red blood cells (RBCs) on microscopy.
KEY CLINICAL QUESTIONS
- 1.
How does rhabdomyolysis occur?
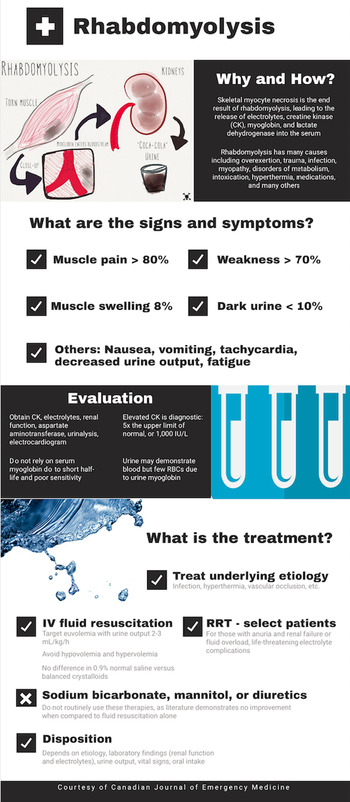
Rhabdomyolysis is the end result of skeletal myocyte necrosis. Muscle injury and decreased myocyte adenosine triphosphate (ATP) production result in cell wall destruction, leading to influx of sodium (Na+) and calcium (Ca2+), increasing intracellular water, and destroying cell attachments. High Ca2+ levels lead to muscle contraction, further decreasing ATP, and can result in cell lysis. Myocyte necrosis releases electrolytes, myoglobin, CK, and lactate dehydrogenase into the interstitial spaces and bloodstream.Reference Long, Koyfman and Gottlieb1 The renal system is at high risk of injury due to precipitation of Tamm-Horsfall protein, which interacts with myoglobin to form casts. These casts deposit in the renal system and obstruct renal tubules.Reference Long, Koyfman and Gottlieb1
Rhabdomyolysis may be classified as exertional versus non-exertional and acquired versus inherited. Most patients with a first-time episode (approximately 75%) have an acquired cause such as exercise and overexertion.Reference Long, Koyfman and Gottlieb1–Reference Scalco, Snoeck and Quinlivan3 Acquired forms other than extreme exertion include trauma, vascular ischemia, electrolyte abnormalities, toxins, hyperthermia, infections, and others.Reference Long, Koyfman and Gottlieb1–Reference Scalco, Snoeck and Quinlivan3 Up to a quarter of recurrent rhabdomyolysis cases are associated with a hereditary etiology, including myopathies and disorders of metabolism.Reference Scalco, Gardiner and Pitceathly2,Reference Scalco, Snoeck and Quinlivan3
- 2.
How can patients with rhabdomyolysis present?
Rhabdomyolysis may range from asymptomatic to severe end-organ dysfunction, renal injury and failure, disseminated intravascular coagulation (DIC), and dysrhythmias.Reference Long, Koyfman and Gottlieb1,Reference Petejova and Martinek4 The classic triad includes concurrent muscle pain, weakness, and dark urine, but this is rare. Concurrent muscle pain and weakness are not present in up to 50% of patients.Reference Long, Koyfman and Gottlieb1 Muscle pain (> 80%), weakness (> 70%), and muscle swelling (8%) are the most common symptoms. Nonspecific symptoms include nausea, tachycardia, emesis, and decreased urine output. Dark brown urine occurs in 5–10% of patients.Reference Long, Koyfman and Gottlieb1 Acute kidney injury occurs in 10–40% of cases, which may result in renal failure.Reference Long, Koyfman and Gottlieb1,Reference Petejova and Martinek4
- 3.
How is rhabdomyolysis diagnosed?
Evaluation should include electrolytes, CK, renal function, aspartate aminotransferase (AST), urinalysis, and electrocardiogram. Laboratory abnormalities that may result from rhabdomyolysis include hyperkalemia, hyponatremia, metabolic acidosis, hypocalcemia in the initial phases of disease, hypercalcemia in the recovery phase of the disease, hyperphosphatemia, and hyperuricemia.Reference Long, Koyfman and Gottlieb1,Reference Scalco, Snoeck and Quinlivan3 Hyperkalemia is a severe complication and must be treated aggressively. If concern for DIC is present, coagulation panel should also be obtained.
An elevated CK level is diagnostic at a threshold level of five times the upper-limit of normal (ULN), or approximately 1,000 IU/L.Reference Long, Koyfman and Gottlieb1,Reference Scalco, Snoeck and Quinlivan3 Baseline CK levels may be greater than five times the ULN in patients with chronic muscle diseases. For these patients, their symptoms should be correlated with their current CK level and baseline values, if available. CK levels increase 2–12 hours after the muscle injury, peak over 24–72 hours, and decline over 5–10 days.Reference Long, Koyfman and Gottlieb1 Delayed increase in CK may occur, and serial levels should be obtained if the initial level is not diagnostic but rhabdomyolysis is likely based on clinician assessment. Myoglobin should not be used for diagnosis due to poor sensitivity.Reference Long, Koyfman and Gottlieb1 This marker has a short half-life (3 hours) and normalizes within 6–8 hours after muscle injury. If used in isolation, myoglobin may miss the diagnosis if the patient presents after this time.Reference Long, Koyfman and Gottlieb1 Elevated CK and myoglobin may be associated with a greater risk of renal injury in crush injuries, but data do not demonstrate a clear association of elevated CK or myoglobin with acute kidney injury (AKI) in other etiologies of rhabdomyolysis.Reference Long, Koyfman and Gottlieb1
Urinalysis may demonstrate moderate to large blood with few RBCs on microscopy due to myoglobin release. The sensitivity of urine dipstick for blood approximates 40%. Compared to urine dipstick for blood, urine myoglobin demonstrates higher sensitivity but poor specificity (15–91%).Reference Long, Koyfman and Gottlieb1 Proteinuria may also be found on urinalysis, but there is no clear association with proteinuria and AKI.Reference Long, Koyfman and Gottlieb1
- 4.
What treatment is recommended?
Management should first focus on addressing the underlying etiology. Therapy includes intravenous fluid resuscitation targeting euvolemia. While some recommend targeting a goal urine output of 2–3 mL/kg/hr, there are no clear data supporting this recommendation.Reference Long, Koyfman and Gottlieb1,Reference Scalco, Snoeck and Quinlivan3,Reference Michelsen, Cordtz and Liboriussen5 Both hypovolemia and hypervolemia are associated with poor outcomes and should be avoided.Reference Long, Koyfman and Gottlieb1,Reference Michelsen, Cordtz and Liboriussen5 Current data do not demonstrate improved outcomes with balanced crystalloid versus 0.9% normal saline (NS), though multiple liters of 0.9% NS may result in iatrogenic hyperchloremic metabolic acidosis, which can decrease urinary clearance of myoglobin.Reference Long, Koyfman and Gottlieb1,Reference Michelsen, Cordtz and Liboriussen5 While sodium bicarbonate, diuretics, and mannitol have previously been recommended, there are no clear data suggesting additional benefit over fluid resuscitation alone.Reference Long, Koyfman and Gottlieb1,Reference Michelsen, Cordtz and Liboriussen5 Renal replacement therapy may be needed in those with anuria and fluid overload or elevated creatinine, or patients with life-threatening hyperkalemia, hypercalcemia, or acidemia.Reference Long, Koyfman and Gottlieb1,Reference Petejova and Martinek4,Reference Michelsen, Cordtz and Liboriussen5
- 5.
Do all patients with rhabdomyolysis require admission?
Patients with newly diagnosed rhabdomyolysis may require admission for rehydration and evaluation for complications. Exertional rhabdomyolysis is usually benign, with no complications.Reference Long, Koyfman and Gottlieb1,Reference Scalco, Snoeck and Quinlivan3 Patients with mild symptoms, clear etiology, normal vital signs, normal oral intake, and normal renal function and electrolytes may be appropriate for discharge home with follow-up. Patients with unclear etiology, laboratory abnormalities (including renal injury/hyperkalemia), abnormal vital signs, and recurrent episodes should be admitted.Reference Long, Koyfman and Gottlieb1,Reference Scalco, Snoeck and Quinlivan3 If discharged, the patient should drink fluids, refrain from exertion, and follow up with primary care within 72 hours, at which time a repeat electrolyte assessment and CK level should be considered.Reference Scalco, Snoeck and Quinlivan3 Patients should return to the emergency department if they experience worsening pain or weakness or decreased urine output, despite drinking fluids.Reference Scalco, Snoeck and Quinlivan3
KEY POINTS
• Rhabdomyolysis occurs with muscle breakdown.
• The classic triad of concurrent muscle pain, weakness, and dark urine is unreliable for diagnosis. Diagnosis includes CK with assessment of renal function and electrolytes.
• Data are not definitive concerning the association of CK and myoglobin with AKI.
• Initial fluid therapy requires consideration of the patient's volume status, with resuscitation to euvolemia.
• Diuretics, sodium bicarbonate, and mannitol should not be used routinely in management.
• Disposition must consider renal function, history of rhabdomyolysis, and the underlying etiology.
CASE RESOLUTION
The emergency clinician provides 1 liter of NS. While the patient's CK level is elevated, the patient's creatinine and electrolytes are normal. The patient's urine output is above 300 mL within the first hour, his vital signs are normal, and he otherwise appears well. The likely etiology is due to exertion with the new exercise program, and the patient desires discharge home. Follow-up is coordinated with the patient's primary care, return precautions are discussed, and the patient is discharged home (Figure 1).
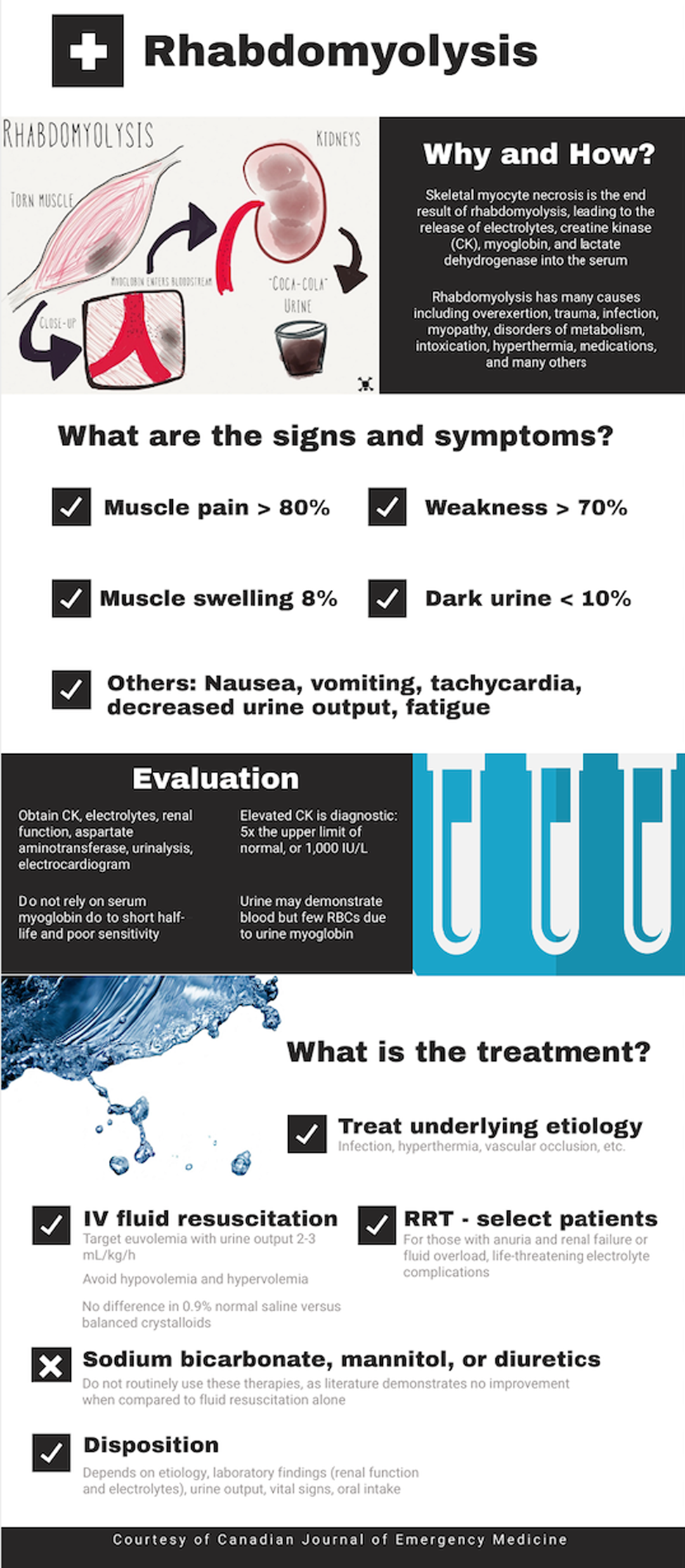
Figure 1. Rhabdomyolysis.
Competing interests
None declared.
Acknowledgements
BL, ET, and AK conceived the idea for this manuscript, obtained permission for submission from Dr. Paul Atkinson, and contributed substantially to the writing and editing of the review. This manuscript did not use any grants or funding, and it has not been presented in abstract form. This clinical review has not been published, it is not under consideration for publication elsewhere, its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder. This review does not reflect the views or opinions of the U.S. government, Department of Defense, U.S. Army, U.S. Air Force, or SAUSHEC EM Residency Program.