Introduction
There is considerable variation in prevalence rates of mental health problems among people with learning disabilities (LD) due to the diagnostic criteria applied in each study, the assessments and sampling methods used (Cooper et al., Reference Cooper, Smiley, Morrison, Williamson and Allan2007; Emerson and Hatton, Reference Emerson and Hatton2007; Dagnan and Lindsay, Reference Dagnan, Lindsay, Emerson, Hatton, Dickson, Gone, Caine and Bromley2012) and the inclusion or exclusion of individuals with co-morbid conditions such as autism spectrum disorder (ASD), dementia and challenging behaviour (Deb et al., Reference Deb, Thomas and Bright2001; Cooper et al., Reference Cooper, Smiley, Morrison, Williamson and Allan2007). Collectively, studies report that people with LD suffer from mental health problems at least at the same and most probably at a higher rate than the general population (Borthwick-Duffy, Reference Borthwick-Duffy1994; Cooper et al., Reference Cooper, Smiley, Morrison, Williamson and Allan2007; Tsiouris et al., Reference Tsiouris, Kim, Brown and Cohen2011), with depression and anxiety as the most common disorders (Richards et al., Reference Richards, Maughan, Hardy, Hall, Strydom and Wadsworth2001; Smiley, Reference Smiley2005; Reid et al., Reference Reid, Smiley and Cooper2011).
Reported increased rates of mental illness have been attributed to a number of factors related to individuals’ biological vulnerability, socioeconomic position and adverse life experiences (Clarke, Reference Clarke2003; Emerson and Hatton, Reference Emerson and Hatton2007; Hulbert-Williams and Hastings, Reference Hulbert-Williams and Hastings2008). People with LD are more likely to have experienced stigma and discrimination (Reiss and Benson, Reference Reiss and Benson1984; Jahoda et al., Reference Jahoda, Dagnan, Jarvie and Kerr2006; Dagnan and Lindsay, Reference Dagnan, Lindsay, Emerson, Hatton, Dickson, Gone, Caine and Bromley2012), poverty and unemployment (Emerson, Reference Emerson2003; Emerson, Reference Emerson2007; Emerson and Gone, Reference Emerson, Gone, Emerson, Hatton, Dickson, Gone, Caine and Bromley2012) and sexual and physical abuse (Sequeira and Hollins, Reference Sequeira and Hollins2003; Lindsay et al., Reference Lindsay, Steele, Smith, Quinn and Allan2006). Jahoda and colleagues (Reference Jahoda, Dagnan, Jarvie and Kerr2006) have stressed the important role that adverse social experiences play in shaping people's cognitions and self-perception, thus suggesting that cognitions are more likely to mediate depression in people with LD than in the general population due to these individuals’ increased risk of experiencing such adverse events.
NICE guidelines recommend the use of cognitive behavioural therapy (CBT) for the treatment of anxiety and depression among the general population (NICE, 2009, 2011). Despite the increased mental health needs of individuals with LD, the development of psychosocial interventions such as CBT has been slow (Hatton, Reference Hatton2002) as people were perceived to lack the cognitive skills considered necessary to engage in CBT. Hence, pharmacological and behavioural interventions have been the treatment of choice (Stenfert Kroese, Reference Stenfert Kroese, Stenfert Kroese, Dagnan and Loumidis1997). A number of psychological therapies have been adapted across the years for people with LD, including CBT. To participate in CBT, individuals are said to need to possess the following abilities: (i) understand cognitive mediation, namely the mediating role of thoughts in emotional responses, (ii) link activating events to emotions, and (iii) differentiate between feelings, thoughts and behaviours (Hatton, Reference Hatton2002). Studies have consistently shown a significant relationship between individuals’ verbal ability and CBT skills (Dagnan et al., Reference Dagnan, Chadwick and Proudlove2000; Joyce et al., Reference Joyce, Globe and Moody2006; Sams et al., Reference Sams, Collins and Reynolds2006; Willner, Reference Willner2006).
Despite the previous dearth of research evidence about the effectiveness of CBT with people with LD, there is currently a proliferation of studies examining how effective this approach is among people with LD and anger, depression or anxiety symptoms. However, existing evidence remains modest and more rigorous and robust research is needed (Willner, Reference Willner2005; Hamelin et al., Reference Hamelin, Travis and Sturmey2013; Vereenooghe and Langdon, Reference Vereenooghe and Langdon2013; Nicoll et al., Reference Nicoll, Beail and Saxon2013; Willner et al., Reference Willner, Rose, Jahoda, Stenfert Kroese, Felce and MacMahon2013; Unwin et al., Reference Unwin, Tsimopoulou, Kroese and Azmi2016).
McGillivray and Kershaw (Reference McGillivray and Kershaw2015) compared the effectiveness of CBT, cognitive and behavioural strategies in attenuating the depressive symptoms and negative automatic thoughts of individuals with mild LD. The results indicate the long-term superiority of CBT, while behavioural strategies appear to produce only short-lived effects. Existing programmes for people with mild LD and mental health problems (Douglass et al., Reference Douglass, Palmer and O'Connor2007; Ghafoori et al., Reference Ghafoori, Ratanasiripong and Holladay2010; Marwood and Hewitt, Reference Marwood and Hewitt2012) that have been shown to be effective tend to focus on teaching participants behavioural coping strategies and it is likely that their effectiveness may be improved by greater emphasis on cognitive strategies. However, it has been shown that people with LD may have difficulties understanding the cognitive components of CBT (Dagnan and Chadwick, Reference Dagnan, Chadwick, Stenfert-Kroese, Dagnan and Loumidis1997; Dagnan et al., Reference Dagnan, Chadwick and Proudlove2000; Joyce et al., Reference Joyce, Globe and Moody2006; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006; Sams et al., Reference Sams, Collins and Reynolds2006; Dagnan et al., Reference Dagnan, Mellor and Jefferson2009) even if the model has been adapted to meet their learning needs (i.e. use of simple language and visual aids, involvement of carers, etc.) (Whitehouse et al., Reference Whitehouse, Tudway, Look and Stenfert Kroese2006; Willner and Goodey, Reference Willner and Goodey2006).
The majority of adults with mild LD appear to be able to link specific events and emotional consequences (Reed and Clements, Reference Reed and Clements1989), but many have difficulties discriminating between thoughts, feelings and behaviours (Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006; Sams et al., Reference Sams, Collins and Reynolds2006) and in understanding cognitive mediation (Dagnan and Chadwick, 1997; Dagnan et al., Reference Dagnan, Chadwick and Proudlove2000; Joyce et al., Reference Joyce, Globe and Moody2006; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006; Sams et al., Reference Sams, Collins and Reynolds2006; Dagnan et al., Reference Dagnan, Mellor and Jefferson2009).
It has been suggested that individuals who seemingly lack the prerequisite skills for CBT could possibly benefit from a pre-therapy structured intervention aiming to teach them CBT core concepts, such as cognitive mediation (Dagnan et al., Reference Dagnan, Chadwick and Proudlove2000; Sams et al., Reference Sams, Collins and Reynolds2006). This type of training is predicted to increase a client's suitability to participate in CBT. Such a hypothesis is in accordance with the concept of the zone of proximal development introduced by Vygotsky (Reference Vygotsky1978), which suggests that it is more significant to know what clients can learn and achieve when assisted by a tutor than what they can do alone (Dagnan et al., Reference Dagnan, Chadwick and Proudlove2000). Three studies have so far examined whether preparatory training can enhance the CBT skills of individuals with mild to moderate LD (Bruce et al., Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010; Vereenooghe et al., Reference Vereenooghe, Reynolds, Gega and Langdon2015, Reference Vereenooghe, Gega, Reynolds and Langdon2016).
Bruce and colleagues (Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010) found that individuals who received one-hour structured training in CBT skills were more capable of creating links between thoughts and feelings compared with a control group, as assessed by The Thought to Feeling Task (Doherr et al., Reference Doherr, Reynolds, Wetherly and Evans2005). Individuals had a verbal IQ score of 59 or below [WASI (Wechsler Abbreviated Scale of Intelligence); Wechsler, Reference Wechsler1999]. However, training had no effect on participants’ ability to discriminate feelings, thought and behaviours, as measured by their performance on The Thought–Feeling–Behaviour Task (Quakley et al., Reference Quakley, Reynolds and Coker2004). Vereenooghe and colleagues (Reference Vereenooghe, Reynolds, Gega and Langdon2015) investigated the impact of computerized training on cognitive mediation skills, measured by tasks developed by Dagnan and Chadwick (1997) and Dagnan and colleagues (Reference Dagnan, Chadwick and Proudlove2000). Participants had an average IQ score of 53 (WASI-II; Wechsler and Hsiao-pin, Reference Wechsler and Hsiao-pin2011). The results indicate that the intervention was effective in increasing participants’ ability to choose the appropriate feeling when they were provided with congruent pairings of events and thoughts, but had no effect on their ability to identify the correct mediating cognition when provided with either congruent or incongruent pairings of events and emotions. Vereenooghe and colleagues (Reference Vereenooghe, Gega, Reynolds and Langdon2016) used ‘The Behaviour, Thought, Feeling Questionnaire’ (Greenberger and Padesky, Reference Greenberger and Padesky1985; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006) and the questionnaire by Dagnan and colleagues (Reference Dagnan, Chadwick and Proudlove2000) to examine the impact of computerized training on people's CBT skills. Study outcomes showed that participants’ ability to distinguish between behaviours, thoughts and feelings significantly improved post-intervention, whereas training had no significant effect on their cognitive mediation skills.
These three studies suggest that it is feasible to teach people with LD some of the prerequisite skills for CBT. However, The Thought to Feeling Task (Doherr et al., Reference Doherr, Reynolds, Wetherly and Evans2005) used by Bruce et al. (Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010) may not be a reliable indicator of cognitive mediation and overestimate individuals’ skills, as they are solely asked to identify how a fictional character would feel in specific situation–thought pairs. Their ability to correctly identify a mediating belief based on a situation–feeling pair is not assessed. Added to this, the task has only congruent situation–thought pairings and therefore does not examine the effect of incongruity on individuals’ ability to identify appropriate feelings. Vereenooghe and colleagues (Reference Vereenooghe, Reynolds, Gega and Langdon2015) taught participants with LD how to make associations between situations and feelings using the Reed and Clements (Reference Reed and Clements1989) task. They did not receive training in cognitive mediation skills and the intervention effect on participants’ ability to distinguish between thoughts, feelings and behaviours was not assessed.
The current study adopts an idiographic approach to gain a better insight into the capacity of people with LD to understand the basic elements of CBT. The main aim is to examine whether three of the cognitive skills considered critical to the successful implementation of CBT can be taught to people with LD using short, cartoon-animated videos. These skills are: (i) the ability to identify mediating cognitions, (ii) the ability to link events to emotions, and (iii) the ability to discriminate between feelings, thoughts and behaviours. A secondary objective is to investigate the acceptability of the intervention and the visual aids that were developed.
Method
Design
This study employed a within-subjects case series research design to examine if people with LD can be taught some of the requisite skills for CBT. This type of design permits exploration of individuals’ abilities in depth and emphasizes individual uniqueness and complexity. Quantitative and qualitative methods were used and CBT skills were assessed at three time points: (i) before the intervention, (ii) following the intervention and (iii) one week after the intervention. The intervention was the presentation of a video, developed by the researchers, consisting of a number of digital stories explaining the basic principles of CBT. The order of the administration of outcome measures was counterbalanced across participants in order to control for fatigue effects on their performance.
Participants
Sample
The recruitment target was achieved and six individuals with LD were recruited from a day centre in Birmingham. The sample consisted of four women and two men aged between 31 and 60 years (mean age 44.3 years).
Inclusion and exclusion criteria
Participants met the following inclusion criteria: (i) had mild to moderate LD, (ii) were over 18 years old, (iii) had English as their first language, and (iv) had normal or corrected to normal vision and hearing. The level of LD was not formally assessed; suitable participants were identified by staff members and were administratively defined as having a LD as they were accessing a LD service. Those individuals who had been diagnosed with a severe mental health problem (such as psychosis) or were currently receiving CBT were excluded from the study.
Training intervention
A video was created by the first author to teach people with LD about the cognitive skills considered necessary to engage in CBT (the video is available upon request). It consisted of several simple digital stories, lasted approximately nine minutes and was created using Pixton Comics (2014), an online comic making tool. The idea of using this online software derived from Vereenooghe and colleagues (Reference Vereenooghe, Reynolds, Gega and Langdon2015) who originally used it in their study and shared their ideas and provided valuable suggestions.
The video has four main parts. In the first part, the three basic concepts of CBT (i.e. feelings, thoughts and behaviours) are defined and several examples of each category are provided. The second part focuses on teaching individuals how to discriminate between feelings, thoughts and behaviours. Participants are also taught how to use hand gestures that signify, respectively, feelings, thoughts and behaviours. In the third part, participants are trained in linking activating events to emotions and in the final section in making associations between mediating cognitions and subsequent emotional responses. The video presents participants with scenarios and they are asked questions similar to those in the questionnaires. Correct answers are provided in the video and if needed the researcher gives participants further explanations. The video is paused after each part and the researcher responds to queries of the participants, repeating and/or rephrasing the core concepts, depending on each individual's needs.
Measures
British Picture Vocabulary Scale II (BPVS II; Dunn et al., Reference Dunn, Dunn, Whetton and Burley1997). This measure assesses language comprehension. Although it was originally developed for use with children, it has been extensively used among adults with LD for clinical and research purposes. Participants are presented with a series of pages with four pictures on each and are asked to select the picture that best illustrates the word presented to them. According to Glenn and Cunningham (Reference Glenn and Cunningham2005), the reliability of the measure is good (Cronbach's alpha: 0.93, median split-half: 0.86), with proven validity. BPVS is also highly correlated with other measures of cognitive ability such as the British Ability Scales (Sams et al., Reference Sams, Collins and Reynolds2006).
Cognitive Mediation Task (Dagnan et al., Reference Dagnan, Mellor and Jefferson2009). This questionnaire measures the ability of people with LD to understand cognitive mediation. Participants are presented with six simple scenarios, such as ‘You want to go on a special trip but there is only one place and your friend is chosen to go instead’ and each scenario is linked to a positive or a negative emotion: ‘You feel happy’ or ‘You feel sad’. Then individuals are asked ‘What would you be thinking or saying to yourself in this situation?’. Each scenario is presented twice, paired with a feeling and subsequently with its opposite, and participants can achieve a maximum score of 12. Pixton Comics (2014) with a voice-over was used and presentation cards were created for female and male participants (Appendices 1a and 1b). An example of one congruent and one incongruent scenario is shown below in Fig. 1.

Figure 1. Visual representation of a congruent and an incongruent scenario from the Cognitive Mediation Task (Dagnan et al., Reference Dagnan, Mellor and Jefferson2009)
This task generates and assesses the inferential (situation-specific) beliefs of the participants. This study followed the recommendation of Dagnan and colleagues (Reference Dagnan, Mellor and Jefferson2009) to present each scenario twice and examine whether incongruity between situation and emotion affects the ability of individuals to identify mediating beliefs. The reliability and the validity of this questionnaire and of its earlier versions has not been assessed, although they have been used extensively with people with LD.
Linking Activating Events to Emotions Task (Reed and Clements, Reference Reed and Clements1989). This measures the ability of individuals with LD to make associations between activating events and subsequent emotions. The task consists of four parts. Its validity and reliability are not known.
-
(i) Emotion recognition from facial images (happy and sad).
-
(ii) Emotion recognition from faces modelled by the researcher (happy and sad).
-
(iii) Situation-specific emotion recognition. Participants are shown six different scenarios and are asked whether the protagonist of each scenario feels happy or sad, and why. They can respond either verbally or point to the face that best represents the emotion of the protagonist. Six is the maximum score participants can obtain. Scenarios were created using Pixton Comics (2014) as well as presentation cards for female and for male participants (Appendices 2a and 2b). An example of a scenario given to female participants and the respective response options is presented in Fig. 2.
-
(iv) Personally relevant situation-specific emotion recognition. Participants are asked how they would feel if someone verbally offended them (happy or sad).

Figure 2. Visual representation of a scenario from the Linking Activating Events to Emotions Task and the respective response options (Reed and Clements, Reference Reed and Clements1989)
The Behaviour, Thought, Feeling Questionnaire (Greenberger and Padesky, Reference Greenberger and Padesky1985; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006). This questionnaire assesses the ability of individuals with LD to discriminate among feelings, thoughts and behaviours. Participants are presented with a list of words and are asked to identify if each word ‘is something you do, something you think or something you feel’. As Fig. 3 shows, emotion icons (emojis) were used to develop visual aids that assist individuals with differentiating between behaviours, thoughts and feelings.
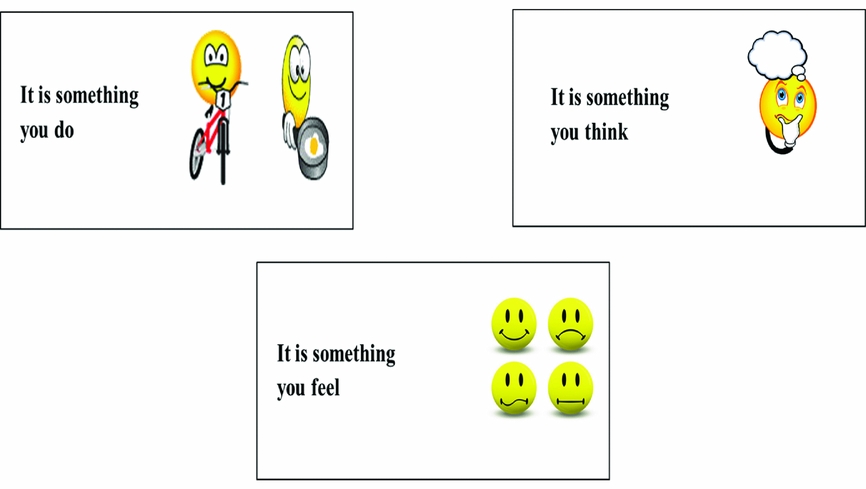
Figure 3. Visual aids for The Behaviour, Thought, Feeling Questionnaire (Greenberger and Padesky, Reference Greenberger and Padesky1985; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006)
This task was originally developed in 1985 by Greenberger and Padesky and was adapted for people with LD in 2006 by Oathamshaw and Haddock. In that study, four people with LD were consulted and asked to propose a number of feelings, thoughts and behaviours. The task instructions were written by a speech and language therapist with experience with this population. The measure was piloted with 20 ‘expert by experience’ participants and after one week it was re-administered to four of the participants. The test–retest reliability was found to be 0.83; its validity has not yet been established. The maximum score for this questionnaire is 23.
Questions on video
Following the intervention, participants were asked to provide qualitative feedback about the video. Three semi-structured questions were developed asking participants to express their opinion about the content of the video and the knowledge they acquired. They are: (1) Did you like the video you watched?; (2) Do you think that the video you watched was interesting?; and (3) Did you learn anything from the video? These were followed up by secondary questions asking participants about the aspects of the video intervention that they did not like.
Ethical approval
Full ethical approval was obtained by the Science, Technology, Engineering and Mathematics Ethical Review Committee of the University of Birmingham (reference number ERN_14-0632).
Procedure
All the participants were recruited from a day service for people with LD. The day centre officers and staff were provided with a project information sheet, giving a study outline and describing the inclusion and exclusion criteria. A list with potentially suitable participants was created and the researcher met with those interested in taking part and explained the study to them using the Participant Information Sheet. Participants were encouraged to ask any questions they might have about the project.
An assessment procedure developed by Arscott et al. (Reference Arscott, Dagnan and Stenfert Kroese1998) was used to assess whether the individuals who wished to participate in the research had the capacity to consent. All the included participants were capable of giving consent and were asked to read and sign a participant consent form with the assistance of the researcher.
All the meetings took place in a quiet room in the day centre. Although participants were offered the option of having someone to accompany them if this would make them feel more relaxed, no one asked for a support worker. In the initial pre-intervention meeting, the three outcome measures were administered to the participants and their verbal ability was assessed using BPVS-II. In the second meeting, which took place after 1–6 days, the intervention was implemented by the researcher and the three questionnaires were re-administered to assess the impact of the intervention. In addition, the participants were asked to provide qualitative feedback on the video. The follow-up assessment took place approximately one week after the intervention and the same measures were administered. In every session, the researcher wrote down the answers provided by the participants using bespoke evaluation forms.
Analysis
The results were analysed separately for each participant. The Reliable Change Index (Jacobson and Truax, Reference Jacobson and Truax1991) could not be used in this study, because the reliability of the measuring instruments has not been assessed. There is only limited evidence of test–retest reliability for The Behaviour, Thought, Feeling Questionnaire (Greenberger and Padesky, Reference Greenberger and Padesky1985; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006), derived from four participants who did not have LD.
To analyse the quantitative data, graphs were plotted and the differences in the pre-, post- and follow-up scores of the participants at the three outcome measures were examined. In addition to the differences in their total scores, differences in the sub-scales of the questionnaires were also investigated (e.g. cognitive mediation in congruent vs incongruent scenarios). Post-intervention and follow-up effects sizes were calculated using the standard mean difference (Busk and Serlin, Reference Busk, Serlin, Kratochwill and Levin1992; Olive and Smith, Reference Olive and Smith2005). The method described by Busk and Serlin (Reference Busk, Serlin, Kratochwill and Levin1992) and Olive and Smith (Reference Olive and Smith2005) estimates variability by calculating the (within subject) standard deviation of baseline scores. This approach was adapted in the current analysis such that the difference between each participant's pre-intervention and post-intervention and follow up scores was calculated and was then divided by the baseline (between-subjects) standard deviation. A summary of participants’ qualitative feedback about the training intervention and supporting materials is also presented.
Results
The results are presented separately for each participant. They include (i) a report of individuals’ performance on the quantitative assessments, (ii) descriptions and observations of their responses during the video and the sessions, including any difficulties they might have faced and (iii) participants’ feedback about the video and the visual aids the researcher developed. Tables 1, 2 and 3 provide information about individuals’ scores on each of the three outcome measures, together with the post-intervention and follow-up effect sizes. Figures 4, 5 and 6 depict the graphical representations of all six participants’ scores.
Table 1. Scores and effect sizes on the Cognitive Mediation Task
C.S., congruent scenarios; I.S., incongruent scenarios.
Table 2. Scores and effect sizes on the Linking Activating Events to Emotions Task
Table 3. Scores and effect sizes on The Behaviour, Thought, Feeling Questionnaire

B, behaviours; T, thoughts; F, feelings.

Figure 4. Performance on the Cognitive Mediation Task for each participant
Figure 5. Performance on the Linking Activating Events to Emotions Task for each participant
Figure 6. Performance on The Behaviour, Thought, Feeling Questionnaire
Participant 1
This 50-year-old man achieved the highest BPVS raw score (87) among all participants. He achieved a perfect score for the Reed and Clements (Reference Reed and Clements1989) test and his ability to associate mediating cognitions with emotional responses improved following the intervention. His ability to distinguish between feelings, thoughts and behaviours did not improve at post-intervention or at the one-week follow-up.
The ability of this participant to correctly identify mediating cognitions (Dagnan et al., Reference Dagnan, Mellor and Jefferson2009) increased following intervention (score going up from 5 to 7) and this improvement was maintained at the one-week follow up. In particular, he became more capable of identifying mediating beliefs when presented with incongruent scenarios. This is demonstrated by the responses he provided in item five at follow up: ‘You have been asked to go and see your manager.’ When the scenario was paired with a sad feeling (congruent pairing), he was able to suggest an appropriate thought: ‘I am in trouble with my manager; I will be dismissed.’. When it was paired with a happy feeling (incongruent), he suggested his thought could be: ‘He will talk about the supervision; I did an excellent job.’
His ability to differentiate between feelings, thoughts and behaviours decreased following the intervention. In the baseline session, he correctly recognized eight feelings, four behaviours and one thought. After the intervention, there was a substantial fall in his ability to distinguish feelings. His score dropped from 8 pre-intervention, to 4 at the post-intervention and 5 at the follow-up assessment. The answers he provided to the post-intervention assessments and the video questions showed that he specifically confounded feelings with behaviours.
This participant provided positive feedback about the video and the visual aids and he enjoyed his participation in the study. He believed that the video was interesting and he particularly liked some of the digital stories (about the dentist and the chocolate bar). The only thing he did not like and suggested could be improved was that ‘There is no story attached to it; it's not like a film.’
Participant 2
This 32-year-old female had a relatively low verbal ability (BPVS raw score: 37). Although her performance on the Linking Activating Events to Emotions Task was excellent, the intervention had no effect on her cognitive mediation skills and her ability to discriminate between feelings, thoughts and behaviours decreased following the intervention.
The training intervention had no impact on the ability of this participant to identify mediating beliefs and her performance (score: 5) remained steady across all the assessments. Her responses to the video questions demonstrated that she had a particular difficulty in understanding cognitive mediation when the scenario was incongruent. Although the intervention was adapted to her needs by repeating the core concepts, using hand gestures more frequently and by frequently checking for comprehension, her ability to identify mediating beliefs did not improve. Another observation was that when she had personal experience of the situation described in a scenario, she was able to identify the correct mediating cognitions more quickly and easily. For example, when she was presented with this congruent situation–emotion pairing, ‘You walk into a room where there is a group of your friends. As you walk in they start to laugh. You feel sad.’, she effortlessly responded that her thought would be ‘they make fun of me’. Then she added, ‘they always do that to me. Why?’. Conversely, she had greater difficulty and more hesitations with scenarios she did not appear to be familiar with, such as the following: ‘You are in bed one night and you hear a loud noise downstairs.’
The capacity of this second participant to discriminate between feelings, thoughts and behaviours decreased after the intervention; although her baseline performance was already low (score: 6), it fell by three points in the post-intervention and the follow-up assessment. During the assessment, she appeared to be confused and tended to respond impulsively to the questions.
In her feedback, she said that she liked the video and the pictures a lot. In response to the question about the most interesting thing in the video, she referred to two specific digital stories, one about the links between events and emotions and one about cognitive mediation. She was able to recall a cognitive mediation scenario, with details about the mediating belief of the protagonist: ‘He thought they made fun of him and laughing at him. It was difficult.’
Participant 3
The third participant, a 49-year-old woman, had a BPVS raw score of 54. Her ability to relate mediating cognitions with emotional responses increased post-intervention, while her ability to distinguish among feelings, thoughts and behaviours remained stable. In the Reed and Clements (Reference Reed and Clements1989) task, she obtained the highest possible score throughout.
This participant could identify the same number of mediating cognitions (score: 4) both before and immediately after the intervention and her cognitive mediation skills were superior in the follow-up assessment (score: 6). She had greater difficulty in identifying mediating beliefs when she was presented with incongruent pairings of events and emotions. The answer she gave to the following incongruent scenario indicates her difficulty: ‘You see a group of your friends, but they do not say hello. You feel happy.’ Her spontaneous respond was ‘no, I don't feel like that’ and she was not able to identify a suitable mediating belief.
Her performance on The Behaviour, Thought, Feeling Questionnaire remained steady between baseline and follow-up. Like Participants 1 and 2, she was more able to differentiate feelings compared with behaviours and thoughts in all the assessments. Her responses further demonstrated her confusion and her particular inability to recognize thoughts. Finally, she had greater difficulty when she was asked questions that were beyond her experience, such as the following: ‘Is playing darts something you do, something you think, or something you feel?’ Her response was: ‘I don't know. I don't do that, I don't like darts’.
When asked what she learned from the video, she answered that she learnt ‘about feelings’ and could recall both scenarios that were used to teach the links between events and emotions. It is notable that her performance in the tasks that examined the concepts presented in these scenarios was high. In particular, she was able to identify feelings in the discrimination task and she achieved a perfect score in the ‘linking events to emotions’ questionnaire.
Participant 4
This 44-year-old male obtained the second highest BPVS score (66) among all the participants. His performance on both the cognitive mediation and the discrimination task improved after the intervention, while his ability to understand the links between events and emotions was excellent pre- and post-intervention.
The number of mediating beliefs he was able to correctly identify increased from four at baseline to five post-intervention and seven at the follow-up assessment. His particular ability to recognize cognitive mediation in incongruent scenarios was enhanced only in the follow-up, as revealed by his answers to the next story: ‘You walk into a room where there is a group of your friends. As you walk in they start to laugh’. Post-intervention, he could identify a proper mediating belief only when the scenario was paired with the feeling of sadness (congruent pairing): ‘Making fun of me’. In the follow-up assessment, he was also able to identify the mediating cognition when the scenario was paired with the feeling of happiness (incongruent pairing): ‘I thought nice smiles. That they have nice smiles. They have fun’.
His performance on The Behaviour, Thought, Feeling Questionnaire increased from 10 at baseline to 12 in the post-intervention assessment, whereas it fell by four points at the one-week follow-up (score: 8). There was a substantial improvement in his ability to distinguish thoughts after intervention (three thoughts pre-intervention vs six thoughts post-intervention and four at follow-up). During the assessment, the participant used the hand gestures for feelings, thoughts and behaviours that he was taught in the intervention.
His feedback about the video was that ‘it was a good one. I think it's useful, other people will like it’ and he particularly liked the pictures in the scenarios. Nevertheless, he ‘didn't like the words, hard to read’ and suggested to include only pictures or limit the number of words and increase their font size. Finally, he thought that the voice-over was clear and easy to understand.
Participant 5
The fifth participant was a 60-year-old woman. Her receptive vocabulary ability was the lowest of all six participants (BPVS raw score: 31) and she also appeared to have expressive language difficulties. Her ability to understand the links between events and emotions and between mediating cognitions and emotional responses improved post-intervention, whereas her performance on the discrimination task decreased.
Before the intervention, this participant had difficulty in understanding cognitive mediation when she was presented with both congruent and incongruent scenarios (0 score). Although the intervention had no effect on her ability to correctly identify mediating beliefs for incongruent scenarios, her capacity to identify mediating cognitions for congruent scenarios increased post-intervention from zero to two. This participant had language and communication difficulties, a short attention span and she often gave incomplete and one word answers. During the video, she was unable to concentrate and was easily distracted.
The ability of the participant to differentiate between feelings, thoughts and behaviours decreased from seven pre-intervention, to six post-intervention and four at follow-up. During the assessment, it became evident that the answers she provided were entirely dependent on the position of the words ‘feel’, ‘think’ and ‘do’ in the interrogative sentence: ‘Is working something you do, you think or you feel?’. She used to select the verb at the end of the sentence (recency effect).
The performance of this participant on the ‘Linking Events to Emotions’ task was low pre-intervention (score: 2). In the initial assessment stage she was not able to identify the sad or the happy facial expression modelled by the researcher. Nevertheless, her performance was enhanced in the post-intervention (score: 4) and the follow-up assessment (score: 5).
Finally, she thought that the video ‘is all right. It was good’ and in answer to the question about what she liked most, she answered ‘the pictures. I like it.’
Participant 6
The last participant was a 31-year-old female with a relatively low language comprehension ability (BPVS raw score: 34). Post-intervention, she was more able to understand cognitive mediation and the associations between activating events and emotions. The intervention had no effect on her ability to distinguish among feelings, thoughts and behaviours.
The ability of the participant to correctly identify mediating beliefs increased from two pre-intervention, to five post-intervention and six in the follow-up assessment. Her responses to the following scenario reveal this improvement: ‘It is your first day at a new job that you have not done before’. In the baseline assessment, she was unable to identify a correct mediating cognition. Post-intervention, she gave a correct response only when the situation was paired with a feeling of happiness (congruent scenario): ‘I am happy cause I work; when people working, have job, are happy’. In the follow-up evaluation though, she also identified a suitable mediating belief for the incongruent scenario where the situation was paired with a feeling of sadness: ‘I do a hard work, job. It gives me a headache’.
The intervention had no impact on her ability to discriminate between feelings, thoughts and behaviours. She was not able to engage in the task, had poor concentration and talked about things irrelevant to the task. Nevertheless, her performance on the ‘Linking Events to Emotions’ questionnaire increased from three before the intervention to five in both the post-intervention and the follow-up assessment. This improvement is demonstrated by the answers she provided to the next scenario: ‘You get out of bed. You go downstairs. It is your birthday’. Before the intervention, although the participant correctly responded that she would feel happy, the explanation she gave was insufficient: ‘cause I am sleeping in bed’. The explanation she provided following the intervention was well-founded and demonstrated good understanding of the links between the event and the emotion: ‘it's my birthday, have a party’.
The participant provided positive feedback on the video, she mentioned that ‘it looks nice, I enjoyed it’. Finally, she particularly liked the visual aids that were used.
Discussion
This study aimed to examine whether a newly developed brief CBT preparatory intervention can enhance the cognitive skills of six individuals with mild to moderate LD. In addition, it explored the acceptability of the intervention among the participants. With respect to the effect of intervention on cognitive mediation skills, the results show that the capacity of most participants to correctly identify mediating beliefs (Dagnan et al., Reference Dagnan, Mellor and Jefferson2009) increased after the intervention, as opposed to the study of Vereenooghe and colleagues (Reference Vereenooghe, Reynolds, Gega and Langdon2015), which found no significant intervention effect on cognitive mediation. These conflicting results can possibly be explained by the differences between the two interventions. Whilst participants in this study were trained in cognitive mediation, the intervention provided by Vereenooghe and colleagues (Reference Vereenooghe, Reynolds, Gega and Langdon2015) had no cognitive mediation element.
It is interesting to note that the cognitive mediation skills of three participants further improved at the one-week follow-up and two of them (Participants 4 and 6) had an enhanced ability to identify mediating cognitions in incongruent scenarios. This is consistent with the results of Bruce and colleagues (Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010) who found that the cognitive skills of people with LD increased one week after the delivery of the intervention, as measured by The Thought to Feeling Task (Doherr et al., Reference Doherr, Reynolds, Wetherly and Evans2005). It is possible that the improvement that was observed here does not reflect an intervention effect, but practice effects as participants became more familiar with the task demands and/or developed a better rapport with the researcher. In any case, the clinical implications of this post-intervention improvement remains and the current findings suggest that people with LD (even those with very limited verbal comprehension) can learn to make connections between mediating cognitions and subsequent emotional responses when they receive one-to-one training.
The intervention had a negative effect on the ability of people with LD to distinguish among feelings, thoughts and behaviours (Greenberger and Padesky, Reference Greenberger and Padesky1985; Oathamshaw and Haddock, Reference Oathamshaw and Haddock2006), a finding consistent with the study by Bruce and colleagues (Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010). Although Vereenooghe and colleagues (Reference Vereenooghe, Gega, Reynolds and Langdon2016) did find a positive effect, in the current study the ability to discriminate got worse for most participants. Finally, the fact that the two participants (Participants 5 and 6) with the lowest verbal ability were unable to engage in the task indicates that this task might be too complicated for some people with LD and that the present training intervention increased, rather than reduced, their confusion. Moreover, this questionnaire requires participants to make a forced choice between three options and only a small number of questions is included in each subscale. Therefore, it is not possible to determine whether any improvement or deterioration in this questionnaire is an effect of random responding or not.
The difficulty experienced by some individuals might be related to the nature of the discrimination task, which asks them to identify whether a number of words and phrases are ‘something’ you ‘do’, ‘think’ or ‘feel’. Participants were particularly confused when they lacked personal experience with some task items, such as ‘gardening’ or ‘I've achieved something’ and this demonstrates the need for individually tailored and personally meaningful assessment instruments. Another problem concerns the way that some task items, such as ‘I don't know what to do for the best’ are worded. In this example, the use of the word ‘do’ may have misled some people, ‘forcing’ them to respond that this is a behaviour and not a thought. In addition, the wording of instructions and the use of language in this questionnaire is confusing in other ways. For example, Participant 1 answered that ‘upset’ is something he does, ‘Do, I do get very upset’. Finally, some participants used the word ‘feel’ as a synonym for ‘think’. This is reflected in the response of Participant 3 when she was presented with the phrase ‘I don't know what to do for the best’ and she answered ‘Feel, I feel I don't know what to do for the best’.
The majority of individuals were better at identifying feelings than thoughts and behaviours and only one participant could identify thoughts in the discrimination task. This was also found in a study conducted by Hebblethwaite and colleagues (Reference Hebblethwaite, Jahoda and Dagnan2011) where people with LD and people with normal cognitive function were equally able to identify and describe their feelings about an emotional real-life experience they had had. However, individuals with LD were less able to talk about their inferential beliefs, as measured by the Cognitive-Emotive Interview (Jahoda et al., Reference Jahoda, Pert, Squire and Trower1998; Trower et al., Reference Trower, Casey and Dryden1988). Furthermore, observations showed that the visual cues were not particularly helpful for the participants. On the contrary, they appeared distracting at times. Sams and colleagues (Reference Sams, Collins and Reynolds2006) also found that visual cues did not affect the ability of individuals with LD to discriminate between thoughts, feelings and behaviours, although the use of visual prompts increased the discrimination ability of children in a study by Quakley and colleagues (Reference Quakley, Reynolds and Coker2004).
Half of the participants achieved the maximum score possible in the Linking Activating Events to Emotions Task (Reed and Clements, Reference Reed and Clements1989) throughout all three conditions. The intervention had a positive impact on the ability of the other three participants to link activating events to subsequent emotional responses which was maintained at follow-up.
Although the qualitative feedback of the participants was generally positive for both the video and the visual aids, individuals talked about some aspects of the video they did not like and these comments have helped us generate some ideas about how the intervention could be improved. Participants mentioned that they did not like the fact that the video had ‘no story attached to it’, hence it did not look like a ‘film’. In the future, it might be worthwhile exploring whether it is possible to create resources with an underlying comprehensive narrative and whether the same characters can be used across stories. This might help people with LD identify with some of these characters and learn some skills through the process of observational learning. Furthermore, one participant commented on the fact that words included in the video were ‘hard to read’ and he did not like them. It is likely that the use of words causes some confusion rather than supporting people's understanding. As a result, future studies should consider working collaboratively with a speech and language therapist to establish the most effective way to present such complex information to people with LD.
It has been argued that the evaluation of individuals’ capacity to participate in CBT should not depend solely on their performance during assessments of CBT skills (Jahoda et al., Reference Jahoda, Dagnan, Jarvie and Kerr2006; Willner and Goodey, Reference Willner and Goodey2006; Beail and Jahoda, Reference Beail, Jahoda, Emerson, Hatton, Dickson, Gone, Caine and Bromley2012). There are a number of other critical factors that influence the successful implementation of CBT for people with LD. The research evidence points out the importance of the therapeutic relationship, motivation to participate in therapy, psychological thinking and self-efficacy (Willner, Reference Willner2006; Jones, Reference Jones2013; MacMahon et al., Reference MacMahon, Stenfert Kroese, Jahoda, Stimpson, Rose and Rose2015) and indicates that the engagement of carers in treatment might be beneficial for people with LD (Rose et al., Reference Rose, West and Clifford2000, Reference Rose, Loftus, Flint and Carey2005; Willner et al., Reference Willner, Jones, Tams and Green2002; Whitehouse et al., Reference Whitehouse, Tudway, Look and Stenfert Kroese2006). Finally, Willner and Goodey (Reference Willner and Goodey2006) have highlighted the importance of episodic memory, the ability of temporal sequencing and several other cognitive skills.
Limitations and recommendations for future research
The use of a case series research design permitted in-depth examination of pre-requisite skills for CBT of people with LD. However, the internal validity of the present study is low and the outcomes preliminary, hence more robust research is required to substantiate and extend them. In addition, all participants were recruited from a non-clinical population and were said to have mild to moderate LD. Therefore, the outcomes cannot be generalized to individuals with more severe LD or clinical populations. Although the qualitative feedback acquired from participants provides useful information about the acceptability of the intervention, it was not ‘rich’ enough to permit formal qualitative analysis such as content or thematic analysis. Moreover, with hindsight we think that the phrasing of the questions may have led to response bias and participants talking more about the positive aspects of the video intervention.
An important caveat to the study results presented here is the unknown reliability, validity and sensitivity to change of the outcome measures that were used. This is a new area of research and although the questionnaires appear to have face validity, there has been no assessment of their predictive validity. Future research should investigate whether a relationship exists between assessments of prerequisite skills for CBT and positive therapeutic outcomes (Dagnan et al., Reference Dagnan, Mellor and Jefferson2009; Bruce et al., Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010). Moreover, the cognitive mediation task requires a judgement of appropriateness of the mediating cognition and this was made by the first author based on the scoring instructions provided by Dagnan and colleagues (Reference Dagnan, Mellor and Jefferson2009). However, the assessor was not blind to phase and this might have caused some observer bias.
Future research should also examine the possibility that CBT training is not useful for specific groups of people with LD. In this study, the participants with low verbal comprehension and poor concentration skills did not appear to benefit from the intervention training. There is also a body of evidence which demonstrates strong associations between verbal ability and ability to understand CBT concepts (Reed and Clements, Reference Reed and Clements1989; Dagnan and Chadwick, 1997; Dagnan et al., Reference Dagnan, Chadwick and Proudlove2000; Joyce et al., Reference Joyce, Globe and Moody2006; Sams et al., Reference Sams, Collins and Reynolds2006).
The existing evidence and materials from this and other studies could be used to develop a preparatory training programme for CBT, using the video and visual aids prepared for this study, the computerized training tasks developed by Vereenooghe and colleagues (Reference Vereenooghe, Reynolds, Gega and Langdon2015) and the manualized intervention by Bruce and colleagues (Reference Bruce, Collins, Langdon, Powlitch and Reynolds2010). Our findings and those of others clearly indicate that more thought should be given to how to teach individuals to discriminate between feelings, thoughts and behaviours and identify cognitive mediation when presented with incongruent scenarios. Our findings suggest that participants require more than one training session and sessions using training items that are personally meaningful to them.
The ultimate aim is to improve the opportunities of this previously excluded group to access psychological therapies (Department of Health, 2009) and this study sheds more light on the role that technology could play in this direction. Although people with LD might not be able to learn all the prerequisite skills for CBT, such assessments and training interventions can help therapists gain a better understanding of each individual's special needs and of difficulties they might face during therapy. In this way, therapists will be able to make informed decisions on how to adapt sessions and make therapy more accessible to people with LD through providing individuals with appropriate scaffolding and support.
Main points
-
(1) It is feasible to teach people with mild/moderate LD some CBT concepts.
-
(2) The preparatory CBT intervention introduced in this study was highly acceptable among the participants.
-
(3) There was an improvement in participants’ cognitive mediation skills following the intervention.
-
(4) The intervention had a negative impact on the individuals’ ability to distinguish between feelings, thoughts and behaviours.
-
(5) The case series design permitted the in-depth exploration of participants’ skills and difficulties they faced, but the study's internal validity is low and further research is needed to substantiate the outcomes.
Acknowledgements
The study was part of Ioanna Tsimopoulou's thesis for the degree of Master of Research (MRes) in Clinical Psychology at the University of Birmingham in the academic year 2013–2014; Ioanna was a Scholar of Alexander S. Onassis Public Benefit Foundation at the time this study took place.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethics
Full ethical approval was obtained from the Science, Technology, Engineering and Mathematics Ethical Review Committee of the University of Birmingham (reference number ERN_14-0632).
Conflict of interest
Ioanna Tsimopoulou, Biza Stenfert Kroese, Gemma Unwin, Sabiha Azmi and Christopher Jones have no conflicts of interest with respect to this publication.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1754470X1700023X
Learning objectives
-
(1) Can people with LD learn some of the pre-requisite skills for CBT?
-
(2) Can technology help clinicians make CBT more accessible for people with LD?
-
(3) Is a newly developed brief CBT preparatory intervention acceptable among individuals with LD?












Comments
No Comments have been published for this article.