Yoga, with its origins in India centuries ago, has over the past few decades transcended geographical boundaries to become popular worldwide. In this editorial we dispassionately explore whether yoga is merely a fad or whether it has sufficient evidence base to back it as a useful intervention for psychiatric disorders.
In its ‘purest’ sense, in Indian philosophy, yoga is one of the six Darshanas or streams and was codified by the sage Patanjali around 400 b.c.e. into eight divisions (Ashtanga) in his Yoga Sutras. Although the original objective of yoga (derived from the Sanskrit word yuj, which means to yoke or unite) was to aid the mental and spiritual progress of an individual, it has been extensively used as a lifestyle practice by healthy people as well as those with physical and mental disorders. The word ‘yoga’ has various definitions and for the purpose of this editorial we define it as a set of practices derived from the Indian tradition comprising combinations of physical postures, breathing practices and meditative practices. There are multiple schools of yoga, which emphasise different aspects of these practices. For example, Sudarshan Kriya yoga places emphasis on rapid breathing, a variant of pranayama. Iyengar yoga emphasises achievement of perfection in physical posture (asana). Yoga practices have also been adapted to fit the needs of particular groups of people, such as prenatal yoga for pregnant women.
Yoga as therapy for psychiatric disorders
Earliest accounts of the salutary effects of yoga practices in people with depressive and anxiety symptoms date back to the 1970s, but these were mostly single case studies or small trials with considerable methodological limitations. Subjective improvements in well-being, mood and quality of life have been reported by people with various clinical and subclinical psychiatric disorders. The new millennium has seen a veritable explosion of research into yoga as a therapy for psychiatric disorders, as evidenced by recent systematic reviews and meta-analyses.Reference Balasubramaniam, Telles and Doraiswamy1
Methodologically sound randomised controlled trials (RCTs) have evaluated yoga as a therapeutic intervention for major depression and schizophrenia. Yoga-based interventions have been found to be efficacious in treating major psychiatric illnesses such as depression and a meta-analysis reported an impressive pooled effect size of −3.25.Reference Cabral, Meyer and Ames2 A recent review of yoga and mindfulness in severe mental illness found reasonable evidence for symptom reduction in psychosis and depression, although evidence is sparse for bipolar disorder.Reference Sathyanarayanan, Vengadavaradan and Bharadwaj3 Two recent studies reported successful treatment of major depression using yoga as the only treatment (details of these and the other trials mentioned in this editorial are available from the author on request). An 8-week RCT of a hatha yoga intervention as monotherapy for mild-to-moderate major depression compared with attention-control education sessions found that the yoga participants (n = 20) had significantly greater decline in depression scores than the control group (n = 18) and more of them achieved remission. The effect size for yoga in reducing depression scores was large (Cohen's d = −0.96). However, the small sample size limits the generalisability of the study findings. Another RCT evaluated the safety of an Iyengar yoga plus coherent breathing intervention as well as potential effects on suicidal ideation in patients with major depression. At the end of 12 weeks, eight of the nine patients who had had suicidal ideation without intent at baseline reported that it had resolved. However, the findings of this study need to be considered preliminary in view of the lack of a control group and small sample size.
Up until the early 2000s, yoga was considered unsuitable for people with psychosis for fear of possible precipitation of psychotic symptoms by meditative practices and uncertainty over whether these patients would be able to follow the practices of yoga. However, several RCTs have now shown that yoga-based interventions offer significant benefits to people with negative symptoms and to their quality of life. Yoga has also been shown to improve social cognition, a dimension that has recently gained interest. All the above led to the inclusion of yoga in the 2014 National Institute for Health and Care Excellence (NICE) guidelines for schizophrenia as one of the recommended complementary treatments. Most of the yoga-based interventions for people with psychosis include postures (Asanas) and breathing techniques (Pranayama) and not a lot of meditative practices. Evidence has also emerged to show that yoga helps reduce burden and improve quality of life for family caregivers of people schizophrenia.
Apart from their beneficial role in major psychiatric disorders, there is also preliminary evidence for the usefulness of yoga-based interventions in several other psychiatric disorders, including attention-deficit hyperactivity disorder, autism, somatoform pain disorder, alcohol and opioid misuse, obsessive–compulsive disorder, and mild cognitive impairment in the elderly. Anxiety as a symptom of stress has consistently been found to respond to yoga. Again, these encouraging findings need to be replicated in methodologically robust studies.
Yoga-induced biomarker changes in people with psychiatric disorders: evidence base
To address the criticism that yoga's positive effects have no biological underpinnings, recent research has focused on assessing changes in possible biomarkers along with clinical changes in people with psychiatric disorders who practise yoga. These include changes in blood parameters such as brain-derived neurotrophic factor (BDNF) and oxytocin, and structural and functional changes in the brain measured using magnetic resonance imaging as well as newer modalities such as functional near-infrared spectroscopy (fNIRS) and transcranial magnetic stimulation (TMS), which provide measures of regional blood flow and cortical inhibition respectively. Cortical inhibition, which is a gamma-aminobutyric acid (GABA)-mediated activity, has been shown to be dysfunctional in people with major depression and obsessive–compulsive disorder. Compared with a control intervention (walking), 12 weeks of yoga practice was shown to enhance GABA concentrations (measured by magnetic resonance spectroscopy) in the left thalamus of healthy individuals, which corresponded to subjective reports of improvements on mood and anxiety scales. Another recent study using TMS showed that healthy individuals had significant enhancement of the cortical silent period (CSP) (a TMS-derived measure of cortical inhibition mediated by GABAB subreceptors), with a possible dose–response relationship with the number of yoga sessions. Some of these biomarker changes, such as the TMS findings, have been demonstrated in healthy individuals only, but are likely to be relevant as potential mechanisms in people with psychiatric disorders.
Figure 1 provides a summary of the neurobiological effects of yoga and their postulated mechanisms of action: (a) modulation of the hypothalamic–pituitary–adrenal (HPA) axis; (b) enhancement of GABAergic neurotransmission; (c) autonomic modulation; and (d) neuroendocrinological effects.
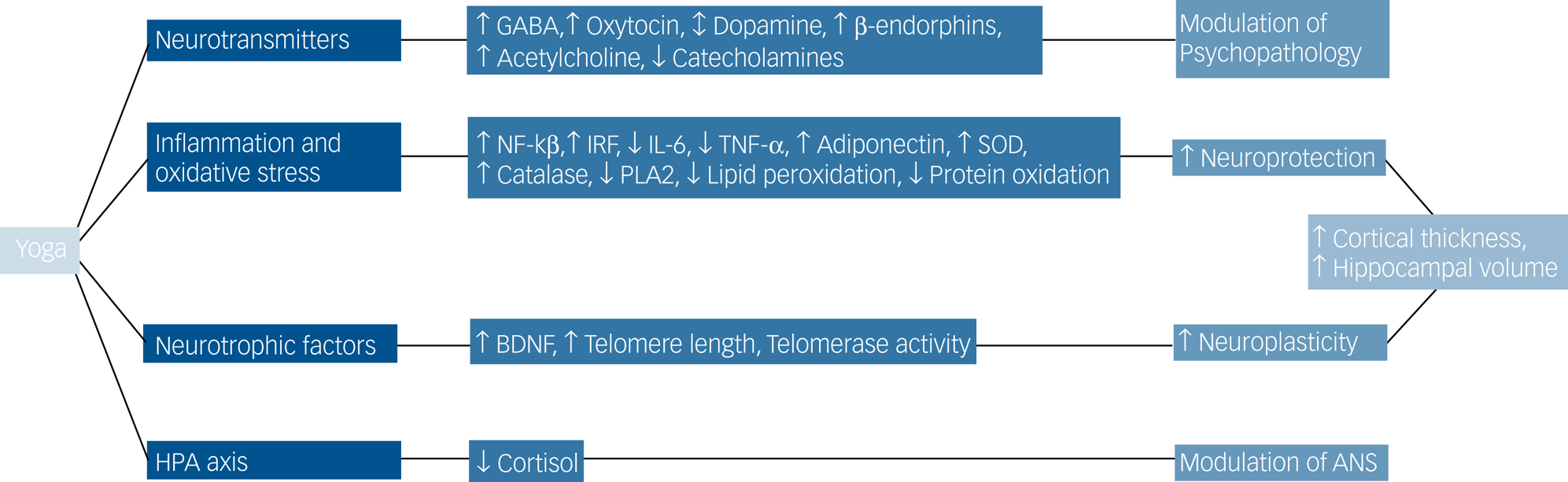
Fig. 1 The neurobiological effects and proposed mechanisms of action of yoga.
A selection of studies that have examined the biomarker effects of yoga therapy is presented below with a view to illustrating the emerging evidence base in this field and suggesting possible future direction of travel.
An 8-week course of prenatal yoga was associated with decreased salivary cortisol and anxiety measures immediately after the first yoga class and after the final class when compared with the control arm who received treatment as usual. A study involving people with schizophrenia found that 4 weeks of practising yoga postures, breathing techniques and meditation increased plasma oxytocin levels, socio-occupational functioning and facial emotion recognition in the yoga group compared with the waiting-list control group. Six months of add-on yoga nidra in women with menstrual disturbances resulted in significant decreases in serum prolactin levels at baseline and post-trial and was associated with significant improvement in mean scores on tests of anxiety, depression, and physical and psychological well-being.
Other biomarkers that have been studied include neurotransmitters and inflammatory markers. Yogic practices have been shown to increase serotonin levels in the brain, thus alleviating symptoms of depression and anxiety. In a study of university students, it was found that 12 weeks of yoga before examinations was associated with less exam-related increases in serum cortisol and decreases in the cytokine interferon gamma. Significant improvement in depression scores and serum BDNF levels have been shown using yoga as an intervention in drug-naive individuals with depression after 12 weeks of yoga therapy. Twelve weeks of Iyengar yoga practice was found to alter functional blood flow in the brain. A small study involving seven healthy elderly adults also found a measurable increase of hippocampal volume after 6 months of yoga practice. We have reviewed many of these studies in a chapter covering yoga-based interventions for mental disorders.Reference Varambally, Gangadhar, Lam and Riba4
Methodological challenges in yoga research in psychiatry
Yoga research in psychiatry is fraught with methodological and other practical challenges. Double-blinding is nearly impossible in yoga research, and the most appropriate ‘placebo’ or control intervention for comparison with yoga remains elusive. Several unanswered questions remain: the interaction of yoga with pharmacotherapy, the ‘dosing’ of yoga modules, which may be critical for the effects, the influence of the ‘guru’ and the particular schools of yoga, and the need to measure parameters of change other than psychopathology or quality of life. Some of these limitations may be overcome with pragmatic study protocols and use of ‘generic’ yoga modules, but measuring the quality and verifying the actual yoga practice are challenging.
Conclusions
Yoga as a therapeutic and evidence-based intervention in psychiatric disorders is promising and merits further attention and research. However, for it be embraced by the medical and scientific communities, it needs to be backed by methodologically robust evidence for its efficacy and neurobiological underpinnings.
Acknowledgements
We thank Dr Hemant Bhargav for his assistance with Fig. 1.




eLetters
No eLetters have been published for this article.