Dietary iodine is essential for the production of thyroid hormones which are crucial for normal growth and neurodevelopment in utero (Reference Garnweidner-Holme, Aakre and Lilleengen1–Reference Trofimiuk-Mudlner and Hubalewska-Dydejczyk3). The fetus obtains maternal iodine and thyroid hormone through the placenta and the amniotic fluid(Reference Yang, Liu and Liu4). After the 16th week of pregnancy, the fetal thyroid gland becomes functional and uses iodine for its own thyroid hormone synthesis. Iodine deficiency, estimated to affect 1·9 billion people worldwide, has been announced by the WHO as the most common preventable cause of brain damage(Reference Trofimiuk-Mudlner and Hubalewska-Dydejczyk3–5).
Severe iodine deficiency causes major adverse health effects, especially in pregnant women, who have a higher iodine requirement when compared with non-pregnant women, and their offspring(Reference Pearce, Lazarus and Moreno-Reyes2,Reference Yang, Liu and Liu4) . There are a few mechanisms responsible for increased iodine demand during pregnancy: (1) increment in thyroid hormones production due to thyroid-stimulating hormone-like action of human chorionic gonadotropin and oestrogen-stimulated increase in thyroxine-binding globulin levels; (2) 1·3–1·5-fold increase in glomerular filtration resulting in increased renal iodine clearance and (3) transplacental iodine transfer from maternal to fetal blood(Reference Trofimiuk-Mudlner and Hubalewska-Dydejczyk3,Reference Glinoer6–Reference Leung, Pearce and Braverman9) .
While severe iodine deficiency in pregnant women is associated with endemic cretinism, spontaneous abortion, preterm delivery, low birth weight, fetal growth restriction and neurological damage(Reference Yang, Liu and Liu4), mild-to-moderate iodine deficiency in pregnancy is also known to affect neurodevelopmental outcomes in the offspring(Reference Bath10).
The recommended daily intake of iodine varies according to the life cycle stage with the WHO (2007) recommending 150 µg/d for adults and 250 µg/d for pregnant and lactating women(Reference Stevenson, Drake and Givens11). Iodine is found in a range of foods, with the richest source being fish, followed by dairy products(Reference McMullan, Hunter and McCance12,Reference Delgado, Coelho and Castanheira13) . Among the European countries that have assessed iodine nutrition during pregnancy, two-thirds have reported inadequate iodine intakes(Reference Zimmermann, Gizak and Abbott14). Thus, several actions should be implemented in order to improve iodine intakes in pregnant women in Europe. The WHO emphasised that an effective iodised salt programme with high household coverage is the best strategy to provide adequate iodine to pregnant women, partly because it ensures that thyroidal iodine storage is full in women of reproductive age(5,Reference Zimmermann, Gizak and Abbott14) . Since 2013, the Portuguese Directorate General of Health recommends daily supplementation with 150–200 µg potassium iodide to women during pre-conception, pregnancy and lactation(15). This recommendation resulted from a nationwide study by Limbert et al. (2010), which evidenced that only 17 % of pregnant women in Portugal (between 2005 and 2007) had urinary iodine concentration (UIC) status above the recommended levels (≥150 µg/l)(Reference Limbert, Prazeres and Sao Pedro16). Although the Portuguese Directorate General of Health advocates the need to monitor the implementation of the recommendation and its impact on the target population, this has not been done in Portugal until today. Three main factors reinforce the importance of this monitoring effort: first, iodine supplements have a variable iodine content (in our cohort, iodine content in supplements ranged from 75 to 200 µg iodine); second, they may be available either by medical prescription (in the case of iodine-only supplements) or over the counter (in the case of multimineral/multivitamin supplements) and third, it is generally perceived that compliance to iodine supplementation is not widespread in the Portuguese population (both among health-care providers and pregnant women) given the concerns of potential health hazards, mainly in cases of subclinical thyroid dysfunction.
As a result, characterisation of compliance of health care providers to the recommendation and quantification of the prevalence of iodine supplementation and iodised salt usage by pregnant women are urgently required in Portugal.
Importantly, knowledge about iodine importance has been suggested as a predictor of iodine supplement use(Reference Martin, Savige and Mitchell17), and lack of knowledge about iodine may be a risk factor for iodine deficiency in pregnant and lactating women(Reference Garnweidner-Holme, Aakre and Lilleengen1). Until the present date, no studies have been performed to characterise knowledge about iodine importance and nutrition among Portuguese pregnant women. So, the aim of this study was to investigate iodine knowledge among Portuguese pregnant women as well as its association with iodine status.
Methods
Ethical approval
This study (trial registration number NCT04010708) was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Ethics Committee of S. João Hospital University Center/Faculty of Medicine of University of Porto. Written informed consent was obtained from all subjects.
Study design and participants
This is a prospective observational study that included 485 pregnant women from the IoMum cohort, recruited between April 2018 and April 2019 at Centro Hospitalar e Universitário S. João, Porto (Fig. 1). Participants were invited to participate at their routine first trimester ultrasound scan. At this time, a random spot urine sample was collected as well as demographic, lifestyle and iodine knowledge information through a structured questionnaire.

Fig. 1. Recruitment diagram evidencing inclusion of participants and sample size (n) for each group.
Inclusion criteria were: signed informed consent, gestational age at recruitment between 10 and 13 weeks and fetal vitality confirmed in the ultrasound. All pregnant women taking levothyroxine were excluded from the study.
Assessment of iodine knowledge
A structured questionnaire was applied to all participants. The questionnaire was divided into four main sections: (1) general information (focused on sociodemographic characteristics, anthropometric measures, previous obstetric history and smoking habits), (2) medication information (including thyroid disease and levothyroxine administration, iodine and folic acid supplement use), (3) dietary habits (including a semi-quantitative assessment of intake of specific iodine-rich food sources) and (4) knowledge on iodine (focused on knowledge of the importance of iodine in pregnancy and knowledge of iodine food sources).
Iodine knowledge questions were chosen based on validated iodine knowledge questionnaires previously used by Garnweidner-Holme et al. (Reference Garnweidner-Holme, Aakre and Lilleengen1) and Henjum et al. (Reference Henjum, Brantsaeter and Kurniasari18). The questions used in the present study specifically assessed knowledge on: (a) importance of iodine during pregnancy; (b) richest iodine foods; (c) which foods are the biggest contributors to iodine intake and (d) which types of commercially available salt correspond to iodised salt. In the questions (a) and (d), participants could choose more than one answer and thus each answer was analysed independently. In the questions (b) and (c), participants had to choose only one answer. Questions (a), (b) and (c) had only one correct answer; question (d) had two correct answers. The questionnaire was adopted after pilot test among eighteen pregnant women and content validation by three subject experts.
In order to assess to what extent the type of professional occupation of the participants was associated with knowledge on iodine, professional occupations were categorised into two ways: (a) cognitive v. manual occupations, based on the catalogue of Portuguese classification of professions(19) and in (b) health-related (including health-care and health-promoting occupations) v. other occupations not related to health care or health promotion.
Construction of a knowledge score
All four iodine knowledge questions were used to develop a total iodine knowledge score, afterwards categorised into three categories of knowledge. Each correct answer scored 2 points, and each incorrect answer scored 0 points. Based on the score of each individual knowledge question, a partial score of each question’s theme was created.
Question (a) generated a partial knowledge score of iodine importance, and participants could score either 0 points if selected an incorrect answer or 2 points if the correct answer was chosen. The set of questions (b) and (c) originated a partial knowledge score of iodine food sources where participants could score 0 points if selected an incorrect answer, 2 points if one correct answer was selected or 4 points if both correct answers were selected. Question (d) generated a partial score of knowledge about iodised salt, and participants could score 0 points if selected an incorrect answer, 2 points if one correct answer was selected or 4 points if both correct answers were selected. Thus, partial knowledge score of iodine importance has two categories: no (0 point) and yes (2 points). Partial score of iodine food sources and partial score about iodised salt were categorised into three categories: low knowledge (0 point), medium knowledge (2 points) and high knowledge (4 points).
A total knowledge score ranging from 0 to 10 points was calculated by the sum of all partial scores. Thus, a scale of knowledge was created as follows: low knowledge (0 points), medium knowledge (2–4 points) and high knowledge (6–8 points, as the maximum of 10 points were not achieved by none of the participants).
Assessment of urinary iodine excretion (urinary iodine concentration)
Random spot urine was collected directly into a urine collection container. Urine samples were stored at 4°C until the end of each day when they were aliquoted and stored frozen at −80°C until analyses.
UIC was assessed by inductively coupled plasma MS according to the methodology developed by the Centre for Disease Control and Prevention, as previously described by us(Reference Costa Leite, Keating and Pestana20).
Statistical analysis
Categorical variables were described as absolute frequencies (n) and relative frequencies (%). Variables’ distribution was assessed, and continuous variables were described as medians and interquartile ranges (25th, 75th percentiles; P25, P75) or as means and standard deviations, depending on the normality of their distribution. Statistical differences were tested using the χ 2 test for categorical variables and the Mann–Whitney test or Kruskal–Wallis test to test for differences between continuous variables from two or more than two groups, respectively, and according to the normality of distribution.
Univariate- and multivariate-weighted logistic regression models were used to assess factors associated with iodine deficiency defined as UIC below 100 µg/l. In this analysis, we considered UIC of 100 μg/l as cut-off rather than the WHO-recommended values as this population was particularly skewed to low UIC values with a small proportion achieving UIC ≥ 150 μg/l. In addition, adverse pregnancy outcomes have been reported by several studies to occur for UIC < 100 µg/l(Reference Nazarpour, Ramezani Tehrani and Amiri21–Reference Murcia, Espada and Julvez23).
The dependent variable in all models was UIC < 100 µg/l. The following independent variables were evaluated as potential confounders: maternal age, pre-pregnant BMI, parity, gestational age at the time of recruitment, education and occupation. Of these, the final model only included maternal education and professional occupation. The model goodness-of-fit was assessed by the Hosmer–Lemeshow statistic and test. The discriminative/predictive power of the model was evaluated by receiver operating characteristic curve analysis. The influence of outlier data values on model fit was estimated using leverage statistics, and collinearity was assessed by evaluation of the coefficient correlation matrix. The results are presented as adjusted OR and their respective 95 % CI.
Data were analysed using the statistical package IBM® SPSS® Statistics 2017, version 25, and differences were considered statistically significant whenever P < 0·05.
Results
Demographic characteristics
From the eligible study sample, 485 pregnant women answered the questionnaire. Table 1 presents the characterisation of the study population according to the UIC stratified by the WHO-recommended cut-off for adequacy in pregnant women (150 µg/l). The median UIC was 103·8 (P25, P75 61·4, 190·6) µg/l. The participants’ mean age was 32 (sd 5) years, and median gestational age at recruitment was 12 (P25, P75 12, 13) weeks, with 58 % of women being multiparous. Educational level ≥ 13 years was reported by 50 % of women. The great majority (89 %) of participants had a cognitive (non-manual) professional occupation, and a minority (19 %) had a professional occupation related to health care or health promotion. Also, 97 % of women were Portuguese, 57 % were taking iodine supplements and 71 % were non-smokers. Iodine supplementation was the only variable associated with UIC categories distribution below and above the WHO threshold for adequacy. Among women who were taking iodine supplements, 48 % had UIC of at least 150 µg/l.
Table 1. Demographic and clinical characteristics of the study sample by urinary iodine concentration (UIC) categories
(Numbers and percentages; mean values and standard deviations; medians and 25th and 75th percentiles (P25, P75))

* t test.
† Pearson χ 2.
‡ Mann–Whitney. Individuals with missing data vary between 1 and 22 % of the total sample.
Iodine knowledge and iodine status
Table 2 shows frequencies of answers to iodine awareness questions of the survey. Of the participants, 34 % acknowledged not knowing the importance of iodine in pregnancy, while 30 % chose incorrect answers. Importantly, only 2 % of the women revealed they did not consider iodine particularly important during pregnancy. Regarding knowledge about iodine food sources, although the higher (66 %) proportion of participants could identify fish as the richest iodine food item, only twenty-two women (5 %) correctly identified milk as the food item that contributes the most to iodine intake. In fact, milk intake has been shown to associate positively with iodine status in pregnant women(Reference Alvarez-Pedrerol, Ribas-Fitó and García-Esteban24–Reference Dineva, Rayman and Levie27) and, in Portugal, it has been shown to associate positively with iodine status in pregnant women(Reference Ferreira, Pinheiro and Matta Coelho28) and in school-age children(Reference Costa Leite, Keating and Pestana20), while other iodine-rich food sources such as milk products, fish or eggs have not.
Table 2. Response frequencies to iodine awareness questions
(Numbers and percentages)

* Correct answers.
Furthermore, a high proportion of these women had never heard about iodised salt (46 %), and, from the ones that had heard about iodised salt before, only 24 % could correctly identify iodised salt products from the list given (data not shown).
Table 3 shows the distribution of the study population by scores of iodine knowledge and the association with iodine status. Regarding iodine knowledge scores, 54 % had adequate knowledge about the importance of iodine in pregnancy, 65 % had medium knowledge about iodine food sources and 32 % were completely unable to correctly identify any iodine food source (scoring 0 points, low knowledge). The majority of the study sample (71 %) presented lack of knowledge regarding iodised salt. For the total score of iodine knowledge (scored from 0 to 8 points), the majority (61 %) of the study sample presented medium knowledge (2–4 points). No participant was able to answer correctly to all iodine knowledge questions, reaching the maximum of 10 points in the total score (data not shown).
Table 3. Urinary iodine excretion (UIC) by partial and total score of iodine knowledge in the total sample and in iodine-containing supplement non-users and users
(Numbers and percentages; medians and 25th and 75th percentiles (P25, P75))
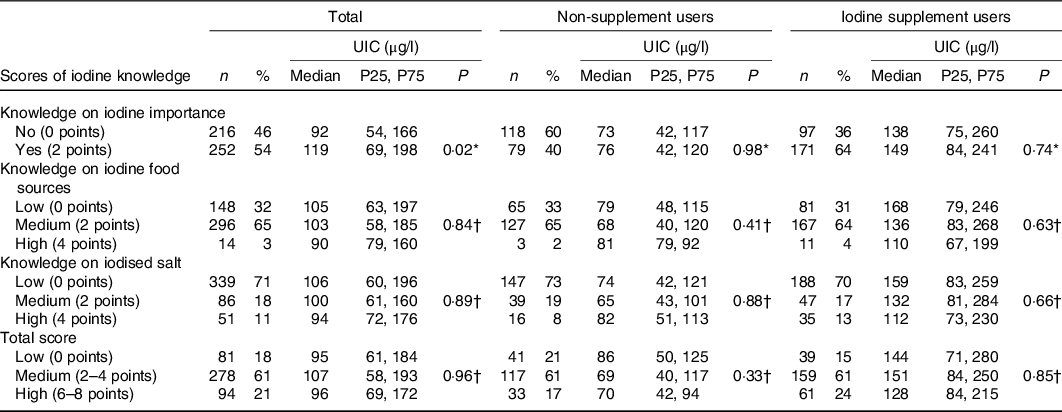
* Mann–Whitney.
† Kruskal–Wallis.
Regarding association between scores of iodine knowledge and urinary iodine excretion (UIC), participants recognising iodine importance (partial score) presented a median UIC 30 % higher than participants with no knowledge on iodine importance (P = 0·02). The partial score of knowledge on iodine food sources, the partial score of knowledge on iodised salt and the total score of iodine knowledge were not associated with iodine status.
When the sample was split by iodine supplement use, the association between knowledge score of iodine importance and UIC was no longer observed (Table 3).
As mentioned, knowing the importance of iodine showed a positive association with median UIC values (P = 0·02; Table 3). This association may be explained by a higher compliance to iodine supplementation by the participants who know the importance of iodine when compared with participants who do not recognise this micronutrient’s importance (68 v. 45 %, P < 0·001; Table 4). In addition, despite knowledge on iodine food sources lacked association with UIC, the proportion of women consuming fish (but not eggs, milk or other dairy products) at least 4 times a week was higher for higher knowledge score on iodine food sources (P = 0·002, online Supplementary Table S1).
Table 4. Association between knowledge on iodine importance and iodine supplement use
(Numbers and percentages)

* Pearson χ 2.
Iodine knowledge and sociodemographic characteristics
Furthermore, an analysis was conducted to examine if the sociodemographic characteristics educational level and professional occupation were associated with the scores obtained on the total knowledge scale. The results show that having high education level (≥13 years) was positively associated with the total iodine knowledge score (P < 0·001). Also, having a health-related professional occupation was positively associated with the total iodine knowledge score (P < 0·001) and having a cognitive professional occupation tended to be associated with higher total iodine knowledge scores, when compared with a manual occupation (P = 0·05) (Table 5).
Table 5. Associations between total score of iodine knowledge and maternal education and professional occupation
(Numbers and percentages)

* Pearson χ 2.
Being multiparous was not associated with any iodine knowledge scores and neither with iodine supplement use (data not shown). In fact, multiparous women had lower UIC (median 92 (P25, P75 56, 173) µg/l) than primiparous women (median 122 (P25, P75 71, 215) µg/l) (P = 0·004).
Finally, logistic regression analysis of the likelihood of having low UIC (i.e. below < 100 µg/l) showed no association with low iodine knowledge independently of professional occupation and educational attainment (Table 6).
Table 6. Logistic regression models for the association between urinary iodine concentration (UIC) < 100 µg/l (n 240) and measures of knowledge on iodine importance, food sources or iodised salt*
(Adjusted odds ratios and 95 % confidence intervals)

* Adjusted for the co-variates: educational level and type of professional occupation (cognitive v. manual and health-related v. health unrelated).
Discussion
Globally, both iodine knowledge and awareness are low among women of childbearing age, including non-pregnant, pregnant and lactating women(Reference Bouga, Lean and Combet29).
The main finding of this study was that Portuguese pregnant women had inadequate iodine knowledge and that iodine knowledge was significantly associated with iodine supplement use and consequently with iodine status. This is the first study reporting iodine knowledge and its association with iodine intake in Portugal. In a context where almost half of the population were uncompliant with the iodine supplementation recommendation, knowledge about iodine importance seems to be an important determinant of this compliance.
In our study, partial scores were obtained for knowledge about the importance of iodine in pregnancy, iodine food sources and iodised salt. Of our participants, 54 % correctly recognised iodine as important to neurocognitive development of the child, 65 % had medium score in knowledge about iodine food sources, while 32 % were unable to identify any iodine-rich food and 71 % did not know which types of salt (sea salt; special sea salt; Fleur de sel; iodised sea salt; iodised refined salt) really correspond to iodised salt. As a result, in our study, 61 % of pregnant women had a medium total score of iodine knowledge and, importantly, 18 % were unable to correctly answer to any question about iodine.
Charlton et al. observed that between 2007 and 2012 in Australia, the knowledge about iodine was generally poor across all areas assessed. In that study, between 27 and 31 % of pregnant and lactating women correctly identified mental retardation as a potential outcome. Therefore, comparatively with our study, the Australian women seem to have a lower level of knowledge regarding the detrimental outcomes of iodine deficiency during pregnancy(Reference Charlton, Yeatman and Lucas30).
In another study conducted in Norway in 2016, Garnweidner-Holme et al. also assessed knowledge about iodine in pregnant and lactating women(Reference Garnweidner-Holme, Aakre and Lilleengen1). That study found a lack of knowledge about the importance of iodine in this population, as well as about the most important dietary sources of iodine. Namely, 52 % of pregnant women reported knowing what iodine is but only 24, 16 and 27 % of pregnant women correctly identified iodine as important for normal child growth and development, for normal fetal development and for maintaining normal metabolism, respectively. Again, those numbers reveal a poorer knowledge on iodine importance in pregnancy comparing with our cohort. One possible explanation for the better scores in our study could be the fact that women were asked to sign an informed consent which briefly referred the importance of iodine and thyroid hormones for brain development. Regardless of this putative bias, knowledge on iodine importance in pregnancy was shown to be associated with a better iodine status as assessed by iodine quantification in urine samples collected at the same time as informed consent and questionnaire application. So, this knowledge should not be exclusively viewed as instantly acquired.
Regarding knowledge on iodine food sources, only 5 % of pregnant women of our cohort correctly answered about milk being the major contributor to iodine intake and the majority wrongfully believed that it was fish (60 %). Milk is considered to be the main iodine source in countries without mandatory salt iodisation(Reference Henjum, Brantsaeter and Kurniasari18), which is the case of Portugal. Importantly, milk, but not yogurt, cheese, fish or eggs, was found to contribute to iodine intake in pregnant women of the IoMum cohort(Reference Ferreira, Pinheiro and Matta Coelho28) and also in Portuguese school-age children(Reference Costa Leite, Keating and Pestana20). Nevertheless, knowledge on the role of milk consumption on iodine intake is usually low among pregnant women. Similarly to our study, Combet et al. observed in the UK between the years 2011 and 2012 that only 9 % of pregnant women could recognise milk as a source of iodine(Reference Combet, Bouga and Pan31). Curiously and in the same line, a study performed in Northern Ireland in 2015 revealed that exactly the same proportion of pregnant women (9 %) was aware of dairy products as a good source of iodine(Reference McMullan, Hunter and McCance12).
UIC is regarded as a good population biomarker of recent iodine intake because more than 90 % of ingested iodine is excreted in the urine(Reference Zimmermann8). Importantly, in our study population, knowledge about iodine importance in pregnancy is positively associated with UIC and this may be attributable to iodine supplement use, which was also positively associated with knowledge on iodine importance in pregnancy. Nevertheless, a high knowledge on iodine importance in pregnancy may not be enough to ensure adequate iodine status since the median UIC in pregnant women who correctly recognised iodine as important for fetal neurodevelopment was lower than the WHO cut-off for iodine adequacy in pregnancy (150 µg/l).
So, our study suggests that awareness about iodine importance during pregnancy may contribute to the use of iodine supplements and, thus, to an adequate iodine status.
In addition, knowledge on iodine food sources was positively associated with fish intake frequency (but not with UIC). This again suggests that knowledge may influence food choices. The lack of association between knowledge on iodine food sources and UIC, despite its positive association with the frequency of fish intake, may be explained by the fact that fish is usually consumed in amounts insufficient to ensure a sufficient daily iodine intake. This was further analysed by Ferreira et al. in the IoMum cohort(Reference Ferreira, Pinheiro and Matta Coelho28).
Inversely to what could be expected, being multiparous did not associate with iodine knowledge and it was associated with a lower median UIC when compared with being primiparous. This evidences that multiparous women did not acquire iodine knowledge from their previous pregnancy(ies), suggesting that knowledge on iodine is an emergent issue among Portuguese pregnant women.
In line with our results, Martin et al. observed that pregnant women may be prone to take an iodine supplement if they have greater knowledge of the increased iodine needs during pregnancy(Reference Martin, Savige and Mitchell17). Additionally, Wang et al. evaluated knowledge, practices and nutrition related to iodine in pregnant women in China(Reference Wang, Lou and Mo32). In that study, participants with a high level of knowledge were iodine sufficient (median UIC = 150 µg/l), while those with a low level of knowledge were iodine deficient (median UIC below 150 µg/l). Previous studies in Norway and Australia also showed that pregnant women’s iodine knowledge was positively associated with their UIC(Reference Garnweidner-Holme, Aakre and Lilleengen1,Reference Watutantrige-Fernando, Barollo and Bertazza33) .
Nevertheless, other studies in women of childbearing age found that participants’ knowledge scores were not associated with women’s iodine status(Reference Garnweidner-Holme, Aakre and Lilleengen1,Reference Henjum, Brantsaeter and Kurniasari18) , where suboptimal iodine intake was attributed to inappropriate practices, but not to knowledge(Reference Mirmiran, Nazeri and Amiri34).
The positive association between level of education and iodine knowledge scores found in our study corroborates results by Garnweindner-Holme et al. who showed that being highly educated was a predictor for higher iodine knowledge scores in pregnant women in Norway(Reference Garnweidner-Holme, Aakre and Lilleengen1).
The limitations and the strengths of this study should be considered to frame the interpretation of its results. One of the limitations is the education level found in our study group which was higher than that expected for Portuguese women. In fact, national statistics show that in the year 2018, more than 50 % of the Portuguese female population with at least 15 years old had a maximum of 9 years of education(35). This bias may be justified by the fact that more educated women are usually more prone to agree to participate in any scientific study. As such, in a more representative sample of Portuguese pregnant women, a lower degree of iodine knowledge than the one reported in this study could be expected.
The use of random spot urine could be seen as another limitation. In fact, random spot UIC is not a good measure for the assessment of individual iodine status and as it may be influenced by recent iodine intake, it may account for an extra intra-individual variability. Nevertheless, considering also the high complexity and unfeasibility of collecting 24 h urine samples in big populations such as ours, this has been considered the method of choice for evaluating iodine status at a population level(36). In addition, adjustment to creatinine excretion could be considered, but as this also depends on nutritional status and muscle mass, an extra variable could be accounting for the results(36–Reference Mayersohn, Conrad and Achari38).
Despite these limitations, important strengths of this study include its relatively large sample size and the fact that the population includes both iodine supplement users and non-users. Another strength is that all women were recruited in the first trimester of pregnancy, as the invitation was made upon their check-in for the first ultrasound scan at the same hospital. Finally, the collected urine sample was exclusively used for the scope of this study, completely abolishing the risk of contaminations from health-care professional handling, such as the use of a dipstick for clinical assessments.
Studies on knowledge and practices related to iodine are helpful to determine the existing nutrition problem, identify the barriers to dietary practices and feed into future design of intervention and education(Reference Wang, Lou and Mo32,Reference Watutantrige-Fernando, Barollo and Bertazza33) . Our study evaluated and explored iodine knowledge, supplementation use and iodine status in pregnant women in Porto region in Portugal. The present study has shown that the majority of pregnant women had medium knowledge about iodine. Although the consequences of iodine deficiency are well known, the potential consequences of mild-to-moderate iodine deficiency are likely to be more subtle. Scientific evidence points to the importance of initiating iodine supplement use and use of iodised salt prior to pregnancy in order to ensure sufficient thyroidal store to handle the increased needs during pregnancy(Reference Bath10,Reference Moleti, Lo Presti and Campolo39–Reference Abel, Caspersen and Meltzer41) .
In conclusion, this study reveals for the first time that dietary iodine knowledge and knowledge on iodine importance among Portuguese pregnant women is medium and that iodine knowledge associates with compliance to iodine supplementation and thus with iodine status. Nevertheless, this study also acknowledges that recognising iodine importance in pregnancy may not be sufficient to ensure iodine adequacy. Knowledge and awareness are a means of empowerment in any case of choice. In view of this, several actions should be implemented to improve iodine knowledge and intake in Portuguese women of childbearing age to ensure that they enter pregnancy with adequate thyroid hormone storage. More and better educational approaches to the community by the public health authorities and clinical registered nutritionists are needed to improve iodine knowledge in the population.
Acknowledgements
The authors thank all the pregnant women who kindly enrolled in this study and also all medical doctors, nurses and the administrative staff from the Department of Obstetrics of Centro Hospitalar Universitário S. João, Porto, Portugal, who provided important support to recruitment activities. The authors also acknowledge the valuable collaboration of Dr L. G. Braga for the classification and categorisation of professional occupations of study participants.
This work was supported by National Funds through FCT – Fundação para a Ciência e a Tecnologia/MCTES within CINTESIS, R&D Unit (reference UID/IC/4255/2019) and REQUIMTE (reference UIDB/50006/2020) and through FCT postdoctoral fellowship (V. C. F., grant number SFRH/BPD/109153/2015).
C. P. and N. X. M. participated in population recruitment, sample management and storage and also in writing the article. P. F., C. M. C., A. C., C. P., C. A. R., C. M., I. M., G. P., I. B., J. G., N. X. M. and E. P. carried the study in tasks such as population recruitment, sample management and storage and sample analyses. V. C. F. coordinated sample analyses and participated in the interpretation of the findings. A. A., C. D.-M., D. P. and N. M. participated in interpretation of the findings. C. R., C. C. and L. F. A. were in charge of study design and participated in writing the article. A. M.-R. and C. C. D. were in charge of analysing the data. A. L. B. had responsibilities in designing the study and writing the article. E. K. and J. C. L. coordinated the work and were mainly responsible for formulating the research question, designing the study and writing the article.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521000155










