The Wernicke-Korsakoff syndrome is due to thiamine (vitamin B1) deficiency and can be precipitated by alcohol withdrawal. Wernicke's encephalopathy is classically defined by a triad of symptoms (confusion, ophthalmoplegia and ataxia), but it is increasingly recognised that few cases will present in this way, many presenting with non-specific acute confusional states. Korsakoff's psychosis is an amnestic syndrome which may be preceded by a clear-cut episode of Wernicke's encephalopathy or may result from a series of subclinical encephalopathies in which the classical features are absent (Reference Cook and ThomsonCook & Thomson, 1997). Recent work has categorised Korsakoff's psychosis and alcoholic dementia as part of the same disorder, with thiamine deficiency having a role (Reference ChickChick, 1997). It is therefore important to have a low threshold for treatment in people at risk, such as patients undergoing alcohol detoxification.
Alcohol misuse is being increasingly recognised as having significant comorbidity in psychiatric populations and many people with a primary alcohol problem will accrue psychiatric diagnoses (Reference Weaver, Madden and CharlesWeaver et al, 2003).
The incidence of Korsakoff's psychosis is rising in Scotland (Reference Ramayya and JauharRamayya & Jauhar, 1997). In 1992 Parentrovite preparations were discontinued. In 1989 the Committee on Safety of Medicines published a report warning of adverse reactions to Parentrovite (Committee on Safety of Medicines, 1989). There was a 9-month gap during which no parenteral preparation was available. It has been suggested that psychiatric practice then changed to favour oral preparations, even in malnourished patients with alcoholism (Reference O'BrienO’Brien, 1995).
The incidence of anaphylactic reactions to injectable thiamine preparations has been quoted as 4 per million pairs of intravenous ampoules sold in the UK and 1 per 5 million intramuscular ampoules sold in the UK. These are reports to the Committee on Safety of Medicines on Parentrovite (Reference Cook and ThomsonCook & Thomson, 1997) and are far lower than the incidences reported for streptokinase or penicillin. It is now suggested that psychiatric practice requires refocusing on the use of parenteral thiamine preparations.
The Royal Edinburgh Hospital has a specialised 12-bedded alcohol detoxification ward (the Alcohol Problems Clinic) and six 25-bedded adult general psychiatric wards, which cover different geographical areas of Edinburgh. The Alcohol Problems Clinic admits patients with a primary diagnosis of alcohol dependence for detoxification on a voluntary basis, and does not accept detained patients or those who require a high level of nursing observation. Patients in these latter categories undergo detoxification on the general adult wards, which also detoxify patients referred by local community healthcare teams.
The Royal Edinburgh Hospital devised a guideline for the treatment of Wernicke-Korsakoff syndrome in 1999. This identified patients in whom the presence of the syndrome should be considered (those with symptoms of ataxia, confusion, ophthalmoplegia/nystagmus, memory disturbance, hypothermia and hypotension or coma/unconsciousness) and patients ‘at risk’ (those with diarrhoea, vomiting, poor diet, weight loss or physical illness). Dosing schedules of parenteral vitamins were provided.
Method
Information from the hospital guideline on Wernicke-Korsakoff syndrome was integrated into the hospital alcohol detoxification sheet, a fixed chlordiazepoxide reducing regimen (Fig. 1). This was printed on bright yellow card and distributed to all wards in January 2002. Guidance on the identification and treatment of Wernicke-Korsakoff syndrome was printed on the reverse of the chart.

Fig. 1. Detoxification schedule.
The pre-intervention phase of the study involved all patients undergoing detoxification on general wards between 10 September 2001 and 31 January 2002. The post-intervention period included patients undergoing detoxification between 1 May 2002 and 31 October 2002. Patients were identified by clinical pharmacists working on the wards. Between September 2001 and 31 January 2002 there were 128 admissions to the alcohol detoxification unit, and between 1 May 2002 and 31 October 2002 there were 140 admissions. These numbers were outside the resources of the study, so consecutive admissions were numbered and cases selected randomly by computer (SAS, version 8.2).
Case notes were audited using a standard proforma, based on symptoms described in the hospital guideline which accorded with a recent national guideline (Scottish Intercollegiate Guidelines Network, 2003). Basic demographic data were collected. Symptoms of Wernicke-Korsakoff syndrome were recorded, as well as the timing and number of vials of parenteral thiamine administered.
The main area of interest was whether patients received better treatment pre or post intervention. A good outcome was defined as those who were treated according to the guideline. The analysis also took into account the ward to which patients were admitted (general ward v. alcohol problems clinic).
Results
A total of 70 pre-intervention and 93 post-intervention patients were included. The two groups were similar in terms of gender (50/70 v. 67/93 male), age (median age group 41-50 years in both groups) and length of admission (median stay 8 days and 11 days respectively).
From the 163 case notes studied, parenteral thiamine was indicated for 17 (24%) of the pre-intervention cases and 26 (28%) of the post-intervention cases. Among the pre-intervention cases, 11 patients had symptoms of Wernicke-Korsakoff syndrome and 6 had symptoms placing them at risk. In the post-intervention group, 15 patients had symptoms indicative of Wernicke-Korsakoff syndrome and 10 had symptoms that placed them at risk.
In a quarter of the pre-intervention cases patients were treated as per guideline; in the post-intervention group this rose to over 60%. Pre intervention 13 patients received thiamine, post intervention this rose to 21. Logistic regression was used to investigate change in adherence to the guideline, which was modelled as a binary dependent variable. The independent variables included whether patients were part of the pre-intervention or post-intervention group and whether or not they had been admitted to the Alcohol Problems Clinic. There is a significant effect for the intervention taking into account ward of admission: odds ratio 5.9; 95% Cl 1.3-27.8 (Table 1).
Table 1. Logistic regression analysis showing predictors of adherence to guideline
| Adjusted odds ratio | ||||
|---|---|---|---|---|
| β (s.e.) | P | OR | (95% Cl) | |
| Intervention | 1.78 (0.79) | 0.024 | 5.94 | 1.27-27.80 |
| Alcohol Problems Clinic | 1.94 (0.78) | 0.013 | 7.00 | 1.52-32.25 |
Using logistic regression to look at admissions to the Alcohol Problems Clinic gave an odds ratio of 7.0 (95% Cl 1.52-32.25), showing that admission to a specialist alcohol treatment unit had a stronger effect than the intervention on adherence to the protocol. Following the intervention, the average number of doses of parenteral thiamine rose from 3.08 to 4.62 (Fig. 2).
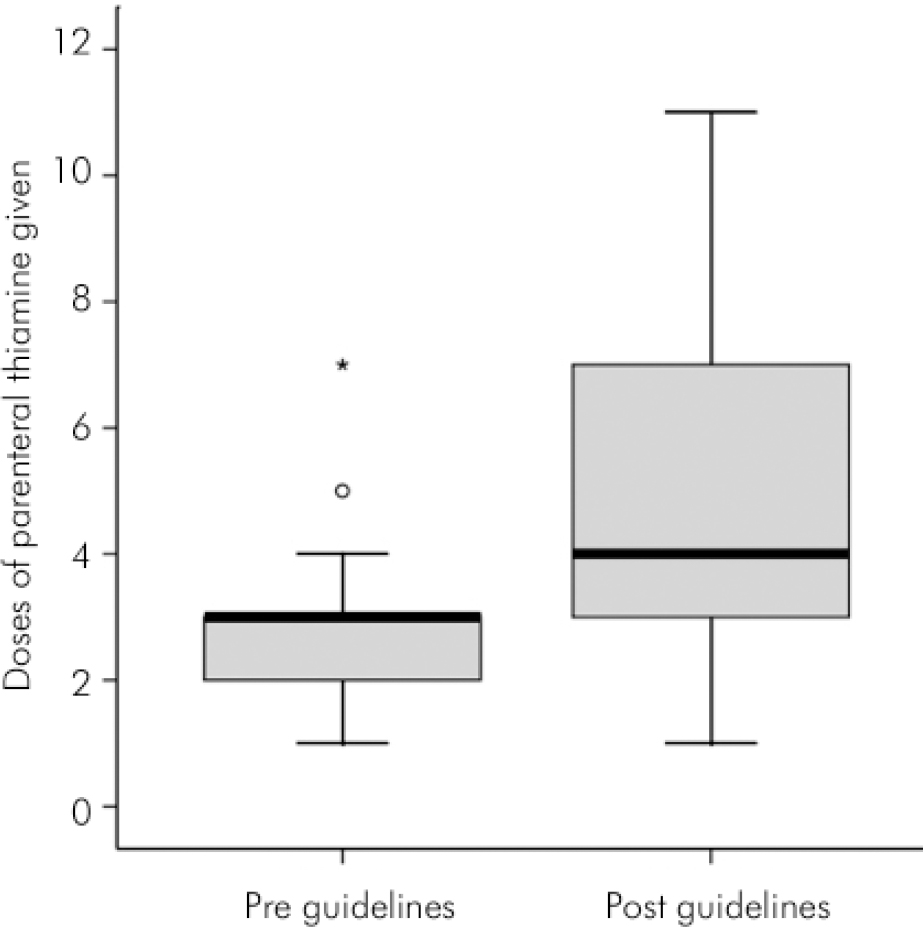
Fig. 2. Number of doses of parenteral thiamine before and after the intervention.
Discussion
In this study a quarter of patients undergoing detoxification required parenteral treatment with thiamine. The intervention of printing information from a guideline on the standard detoxification prescription sheet, and therefore having the guidance available at the time of prescribing, appeared to improve adherence to the guideline. Adherence was more common in a specialised alcohol treatment unit.
This study was a retrospective case-note analysis and as such its results should be interpreted cautiously. A standard proforma was used to minimise bias. Signs and symptoms were documented where recorded in case notes; because of this method of ascertainment it is likely that the incidence of patients requiring treatment was underestimated. The patient populations from the general ward and the specialist alcohol treatment unit may differ; however they are both likely to neglect their diet and to be at risk of alcohol-related memory impairment.
Parenteral vitamin replacement can prevent and treat the Wernicke-Korsakoff syndrome. There are increasing numbers of patients requiring alcohol detoxification in a psychiatric setting; it is therefore important that psychiatric teams have access to appropriate information and guidance to ensure the patients’ outcomes are optimised by appropriate use of parenteral vitamins. The risk of anaphylaxis is extremely low and they are on essential life and memory saving treatment.






eLetters
No eLetters have been published for this article.