CLINICIAN'S CAPSULE
What is known about the topic?
Quality improvement and patient safety (QIPS) education is required in emergency medicine (EM) training, but formal structures are not well established.
What did this study ask?
This study assessed Canadian EM residents’ perspectives on QIPS education and mentorship through a national survey.
What did this study find?
Canadian EM residents perceive that they have inadequate QIPS educational and mentorship opportunities locally and are interested in obtaining more.
Why does this study matter to clinicians?
QIPS education and mentorship should be improved for Canadian EM residents to build capacity for continued growth in care delivery.
INTRODUCTION
The field of quality improvement and patient safety (QIPS) can be defined as the utilization of robust methodological and statistical techniques to bring about positive changes in the delivery of healthcare.1 Previously published landmark literature has demonstrated that QIPS is fundamental to the provision and advancement of healthcare, as preventable errors have been identified as key causes of adverse patient events.Reference Kohn, Corrigan and Donaldson2–Reference Baker, Norton and Flintoft5 The emergency department (ED), in particular, represents a high-risk work environment prone to preventable medical errors, including medication errors and poor staff communication.Reference Kohn, Corrigan and Donaldson2, Reference Calder, Forster and Nelson6–Reference Stang, Wingert, Hartling and Plint8
QIPS competencies have been added to the Canadian Medical Education Directives for Specialists (CanMEDS) frameworks for both the Royal College of Physicians and Surgeons of Canada (RC) and the College of Family Physicians of Canada, as requirements for medical resident training standards.Reference Frank, Snell and Sherbino9,Reference Shaw, Oandasan and Fowler10 This emphasis has also been recognized internationally with the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Emergency Medicine (ABEM) adopting similar recommendations.11,12 In addition, Canadian and American emergency medicine (EM) residency program directors desire formal QIPS training to be provided to their trainees, but they have emphasized logistical challenges and significant variability in how this could be operationalized.Reference Chartier, Vaillancourt and McGowan13,Reference Wolff, Macias and Garcia14 Finally, the 2018 Canadian Association of Emergency Physicians’ Academic Symposium on Leadership has recommended that healthcare providers and support staff be trained in QIPS methodologies in order to improve patient care.Reference Chartier, Mondoux and Stang15
Despite the impetus for EM residents to be trained in QIPS methodologies, the current level of knowledge and expertise of Canadian EM residents with QIPS is unknown. Understanding what support and opportunities are provided to them will help guide efforts to provide the education required for this essential skill. In this project, we assessed the Canadian EM residents’ perspective on the current state of QIPS education and support that they receive during their residency program, as well as investigated whether they have interest in further project and mentorship opportunities.
METHODS
We conducted an English language, cross-sectional electronic survey of Canadian EM residents from both the RC and the College of Family Physicians of Canada – EM (FM-EM) residency training programs.
Survey design
The survey was designed through an iterative process. Initially, the EM resident members of the research team (SVT, RJH, JNH, LN) designed questions surrounding the following themes: familiarity with QIPS, local opportunities for QIPS projects and mentorship, and desire for additional QIPS education and mentorship. These questions were subsequently revised based on feedback from EM attending physicians and QIPS content experts (ESHK, LBC) and a research coordinator (DP). The research team then pilot-tested the survey for clarity, completeness, and functionality with representative participants. Revisions were made after this initial pilot-test, and the survey was tested one final time by the project team.
The survey comprised a total of 23 questions consisting of multiple-choice, Likert, or free-text entry designs (Appendix A). Responses were anonymous, but demographic data including the year of residency, training stream, and home university were collected to assess generalizability. Participants were given the opportunity to self-identify if they were interested in participating in further QIPS activities. No question was mandatory, and therefore some questions’ response rates could be different.
Recruitment
We sent the survey to all 535 Canadian EM residents registered in one of the 17 Canadian universities’ RC or FM-EM training streams in October 2018. Residents were contacted by email, either directly by our team or through their program's administrative assistant (according to the relevant program director's preference). The survey was open for a 5-week period, and, in accordance with previously established survey design methodology, formal reminder emails were sent after the first and third weeks.Reference Dillman16 An electronic consent form was built into the survey platform prior to the survey administration.
Survey administration and data collection
The survey was administered electronically through the SurveyMonkey© 2018 platform (SurveyMonkey Canada Inc., Ottawa, ON). A link to the survey was included in the recruitment and reminder emails sent to the participants. Results were collected into an encrypted Microsoft Excel© 2017 (Microsoft Corp., Redmond, WA) spreadsheet for data analysis. Descriptive statistics are reported here. Qualitative analyses of the free-text entry questions were performed independently by two authors (SVT and RJH) for emergent themes and quotes, which were subsequently combined and refined to determine the most important themes to present.
Ethical considerations
We received ethical approval from the University Health Network's Research Ethics Board for this study.
RESULTS
One hundred eighty-nine (35.3%) residents responded to the survey, representing all EM training programs across all 17 Canadian medical schools (Table 1). The response rates were similar across training streams, with 35.2% (142/403) for the RC residents and 31.8% (42/132) for the FM-EM residents (6 respondents did not disclose their training stream). Of the responding residents from the RC stream, there was a comparable distribution across postgraduate training years (Table 2).
Table 1. Respondents by school of residency training
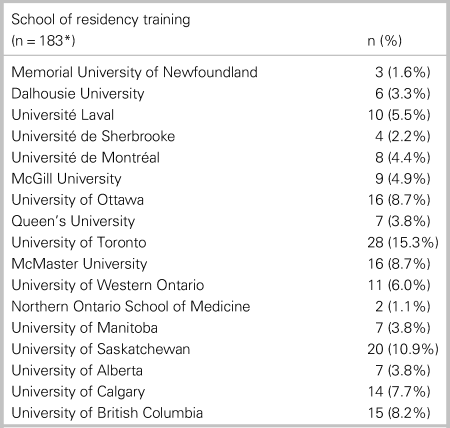
*Six respondents did not provide their school of residency training.
Table 2. Respondents by year of training
FM-EM = Family Medicine – Emergency Medicine; PGY = postgraduate training year; RC = Royal College.
QIPS education
Of responding residents, 17.5% (28/160) stated that QIPS methodologies were formally taught in their residency program, and 66.9% (107/160) reported a desire for it to be formally taught. According to responding residents, at least 10 of the 31 (32.3%) total RC and FM-EM programs across the country had formal QIPS training. More specifically, residents reported this teaching at 8/14 (57.1%) of the country's RC programs and 2/17 (11.8%) of the country's FM-EM programs. Additionally, 4.8% (2/42) of the FM-EM respondents stated that they received QIPS training during their FM residency. One hundred twelve (70.4%) of 151 respondents indicated that they were interested in becoming involved in QIPS training and initiatives to some extent: “very interested” for 18/159 (11.3%), “moderately interested” for 37/159 (23.3%), and “slightly interested” for 57/159 (35.9%). When residents were asked whether they were satisfied by their residency program's current QIPS training, 44 (55.0%) of 80 respondents reported being either “satisfied” or “very satisfied” with their current offerings. Qualitative comments revealed that residents did not feel that the importance of QIPS was adequately emphasized (e.g., “covered too quickly,” “needs to be more awareness around the importance of QIPS”) and that the education was not provided in a “practical, meaningful way”; 61.5% (99/161) of respondents stated that they were unaware of ways to seek QIPS training outside of their normal residency education.
In optional free-text entry questions, respondents stated a desire for QIPS to be more visible in residency training, with some suggesting that formal curricula should exist, and that residents should be required to complete an improvement project during residency training. Respondents also expressed a desire to be paired with local or national QIPS mentors in order to advance their training in this field. Residents desired a list of local projects and mentors, as well as a national database of mentorship opportunities. Finally, the respondents who were aware of external avenues to seek QIPS training indicated that they had done so by taking local or online courses, or graduate-level degree programs.
Experience with QIPS
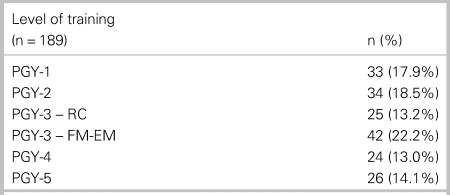
Figure 1 illustrates the level of familiarity with QIPS methodologies of responding residents, with 54.2% (88/161) reporting being “somewhat” or “very” familiar with them; 45.3% (73/161) of respondents reported that they had previously been or were currently involved with a QIPS project, either as the lead (30/73, 41.1%) or as a collaborator (43/73, 58.9%); 26.7% (43/161) of respondents responded that they had previously published or presented work related to QIPS. The most common types of events at which they had presented their QIPS work were at local events (30/43, 69.8%) or national conferences (10/43, 23.2%).
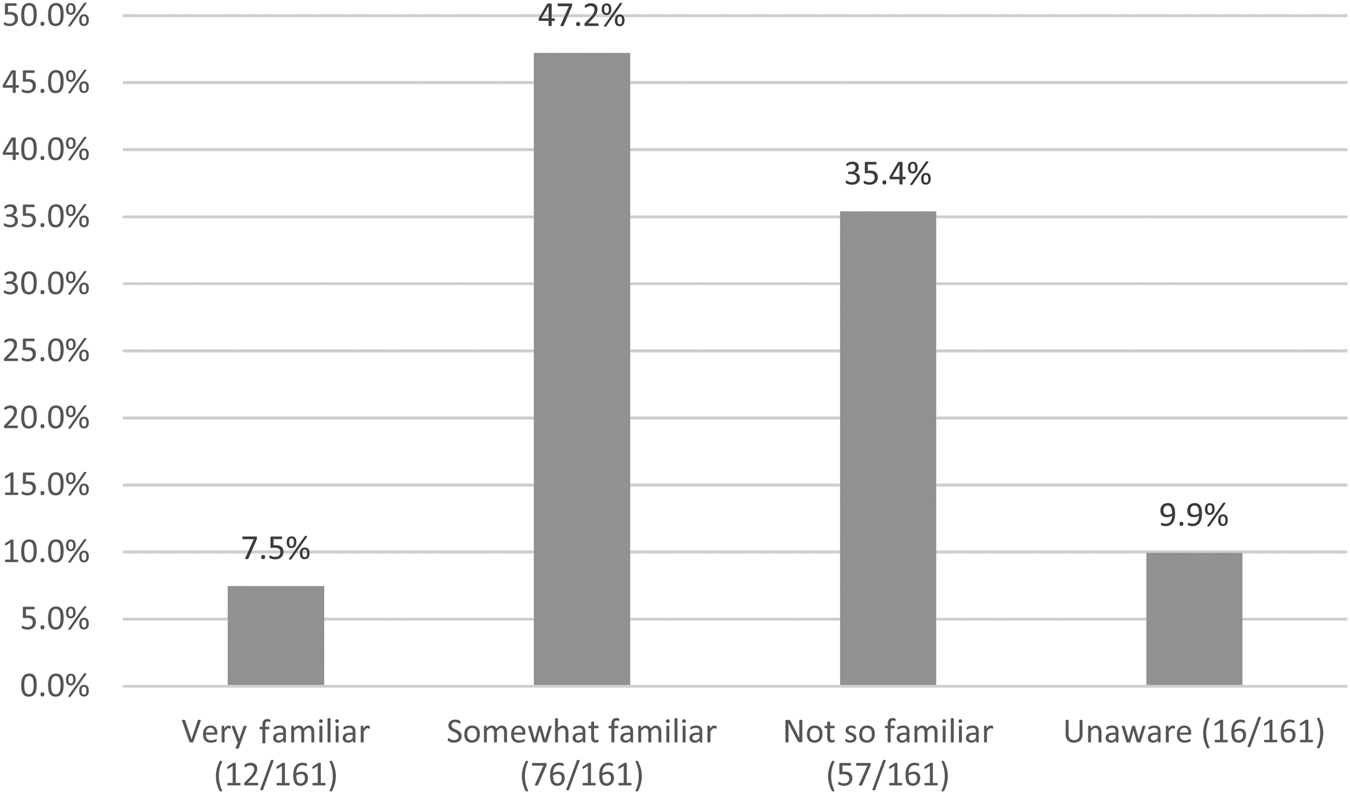
Figure 1. Familiarity with QIPS methodologies of responding residents.
Local QIPS opportunities
Figure 2 illustrates how readily available QIPS project opportunities are, with 85 (52.8%) of 161 residents indicating that opportunities to participate in their work environment are readily available. Figure 3 similarly demonstrates the availability of QIPS mentorship, with 48.4% (78/161) indicating that these were readily available at their institution; 69.6% (110/158) of respondents felt that their work environment allowed for adequate mentorship in QIPS methodologies. At least one respondent from 24 (77.4%) of all 31 EM residency programs answered “no” or “unsure” with respect to the availability of local QIPS projects and mentorship opportunities. Similarly, at least one respondent from 24/31 (77.4%) of programs did not feel that their work environment allowed for adequate mentorship in QIPS. Qualitative comments revealed that opportunities varied from mandatory projects in residency to needing to seek out projects on their own. Projects included flow improvement (e.g., time to ECG, improving triage processes), improving communication (e.g., handover tools), patient safety improvement (e.g., decision tools, checklists), and morbidity and mortality rounds.
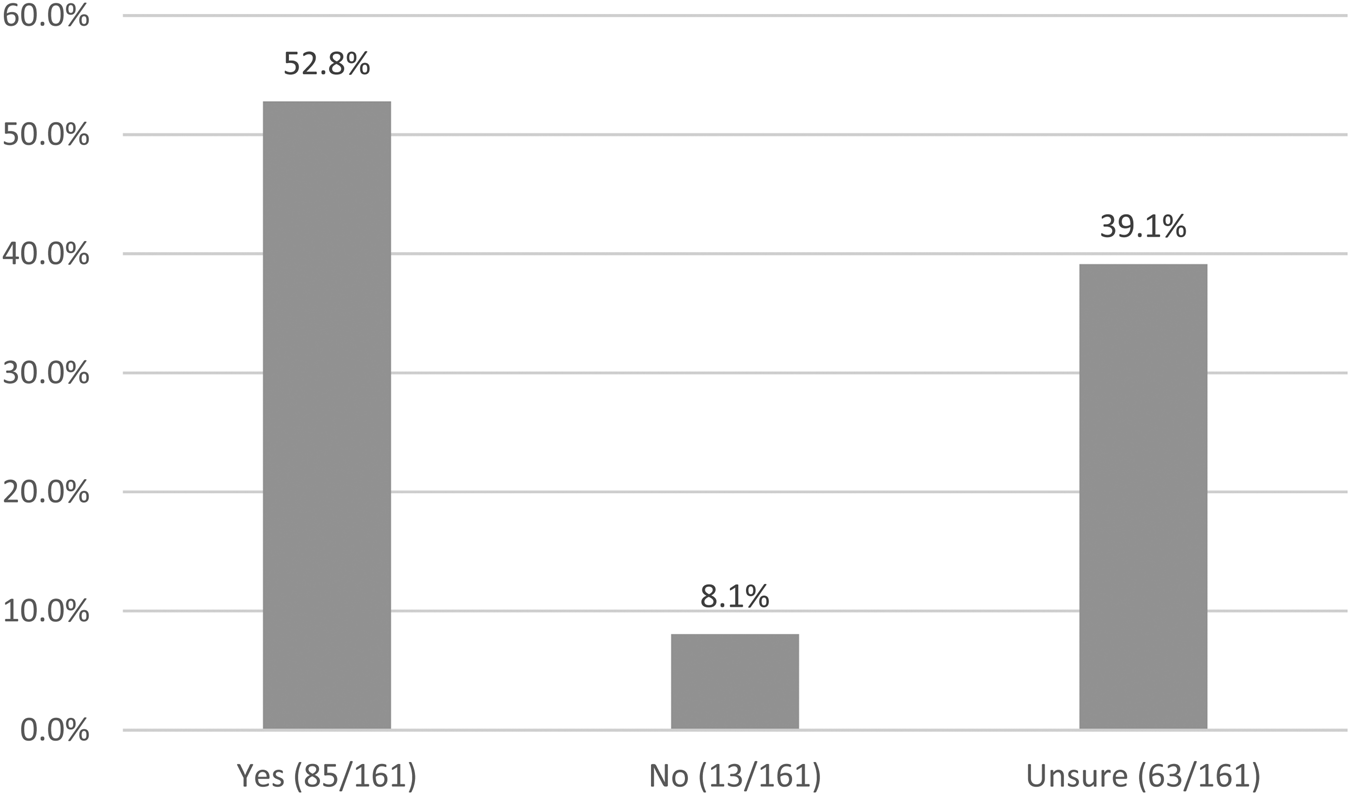
Figure 2. Availability of QIPS project opportunities.
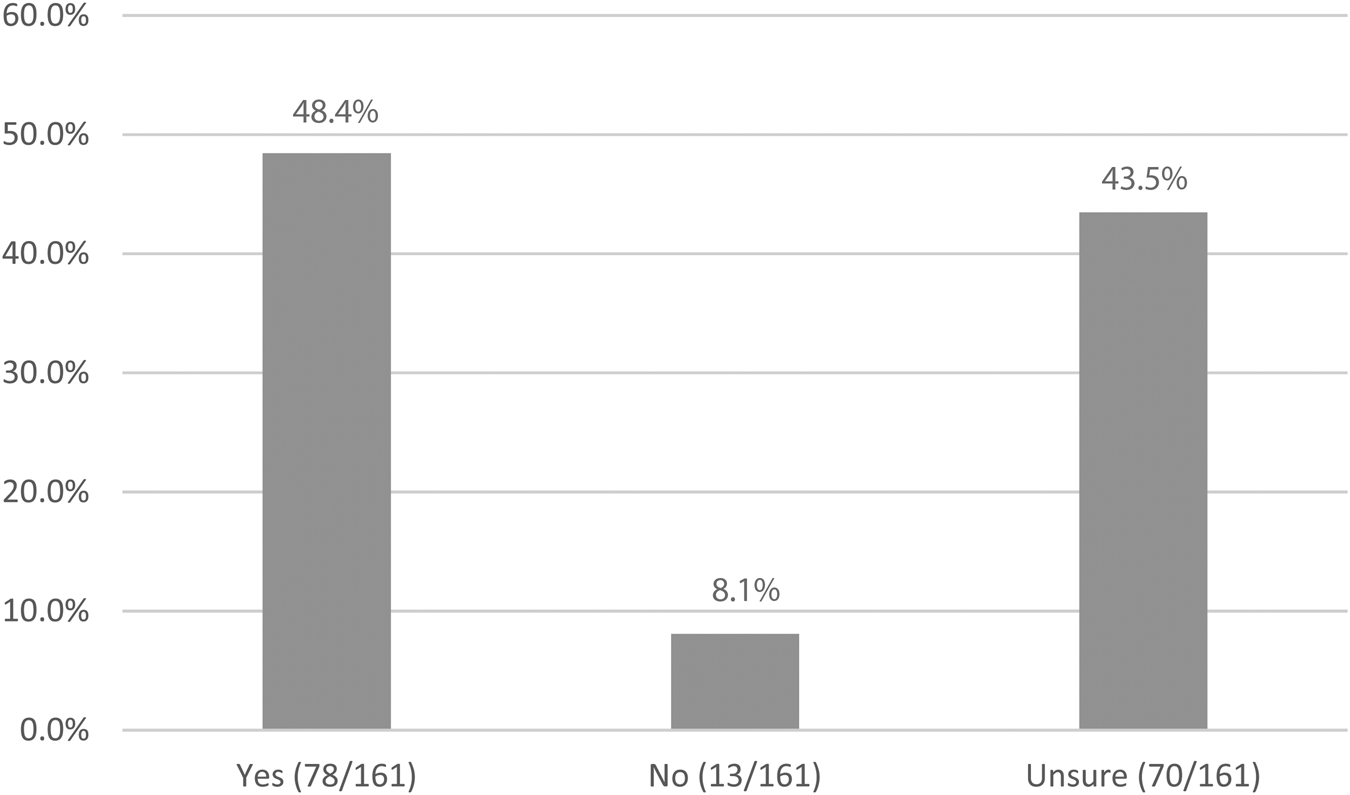
Figure 3. Availability of QIPS mentorship.
DISCUSSION
This study represents the first analysis of the residents’ perspective on QIPS education and mentorship in Canadian EM residency training programs. Our study findings demonstrate that Canadian EM residents are interested in obtaining greater QIPS education, as well as QIPS project and mentorship opportunities, but they do not currently have adequate access to these at the current time. Just over half of residents endorsed some level of familiarity with QIPS. A majority of those residents who had completed QIPS projects were able to achieve scholarly publications and/or presentations. The majority of responding residents indicated an interest for formal QIPS training and project opportunities. Our results also demonstrated a low level of satisfaction with their current residency program offering. Qualitative comments indicated that the current delivery of QIPS education is not at a level where residents are able to understand its practicality in relation to clinical practice, and that local QIPS opportunities are often targeted towards staff physicians. Additionally, only half of the responding residents indicated that they had access to project or mentorship opportunities for QIPS, even if they were in programs with existing curricula. Ultimately, as the importance of QIPS increases in the EM community, it is necessary to support residents with more robust educational infrastructures.
Our results provide a useful snapshot of the residents’ perspective on the current landscape of QIPS training in Canadian EM residency programs, demonstrating some gaps and challenges. Responding residents noted a desire for formal curricula and resources to learn QIPS methodologies, a position that has previously been endorsed by other groups in medical education, including Canadian EM residency program directors.Reference Chartier, Vaillancourt and McGowan13,Reference Wolff, Macias and Garcia14,Reference Bowe and McCormick17,Reference Morrison, Bowe and Brenner18 Despite both residents and program leadership desiring formal QIPS curricula, our results demonstrate that QIPS is taught in at least a third of the programs. A recognized potential barrier to the successful implementation of QIPS curricula in both our results and the literature is the lack of local faculty QIPS expertise and experience.Reference Chartier, Vaillancourt and McGowan13,Reference Wolff, Macias and Garcia14,Reference Mondoux, Chan and Ankel19 This could explain why some responding residents took the initiative to seek training through avenues outside of their residency education. Additionally, our results demonstrate that many residents were participating in QIPS activities, despite having not received formal training, indicating that this may be an informal pathway for the development of QIPS skills.
Only half of our respondents indicated having adequate access to QIPS mentorship and project opportunities, and this was seen across the majority of sites, regardless of whether they had local QIPS training. This perceived deficiency may be a result of poor visibility of QIPS activities, highlighting that stronger QIPS infrastructures at the hospital and academic departmental levels are needed. The promotion of QIPS as a growing field has been advocated for by Canadian ED leadership, and the provision of stronger educational infrastructures would help serve this purpose.Reference Kwok, Perry, Mondoux and Chartier20 Beyond the increase in visibility, the teaching of quality improvement (QI) methods has been demonstrated to yield beneficial clinical outcomes, including the improvement of patient care.Reference Boonyasai, Windish and Chakraborti21 If local expertise is not present, it may be necessary for programs to collaborate with external QIPS leaders to help facilitate the provision of this education. Programs may be able to build local capacity by the adoption of co-learning models, an effective approach model in which both faculty and residents are trained alongside in QI methodologies.Reference Wong, Goldman and Goguen22
Given that the CanMEDS framework now indicates that QIPS skills be taught in all residency programs, program leadership should ensure that their local curriculum meets the needs of their trainees. In order to avoid the duplication of efforts and ensure that the most academically robust curricula are developed, efforts could be made to create a standardized curriculum across the country.Reference Frank, Snell and Sherbino9–11 Canadian EM chief residents from both training streams revealed that existing curricula vary in structure, but most appear to be lecture-based, and not all require a formal QIPS project to be completed (personal communication). In our results, responding residents indicated that their existing training did not easily facilitate the translation of QIPS knowledge into practical applications. As a result, the use of an innovative educational design may be needed to ensure a comprehensive understanding of QIPS principles. Experiential or mixed-method educational methods have been advocated for in the teaching of QIPS methodologies and should be adopted.Reference Morrison, Bowe and Brenner18 In addition, published literature has demonstrated the successful teaching of QIPS concepts through other novel approaches, including debates, interdisciplinary curricula, and peer case review.Reference Strayer, Shy and Shearer23–Reference Mamtani, Scott and DeRoos25
EM residency programs are currently evolving to require residents to participate in QI initiatives. Within the context of the RC stream, residents are required to participate in at least one QI initiative as part of a special assessment.26 This requirement asks that the residents participate in several tasks relevant to QIPS work, but it does not outline specific milestones.26 There does not appear to be a similar requirement within the FM-EM residency programs. However, the College of Family Physicians of Canada has recently begun the Practice Improvement Initiative, which intends to educate FM residents on QI, and it is possible that a similar requirement will exist in the future.27 The ACGME and ABEM have established milestones for American EM residents around QIPS, and these could be adapted for the Canadian context.12 These comprehensive American milestones include both QI themes, such as the knowledge of process improvement methodologies, and patient safety themes, including the use of standardized communication tools, as well as contributing to debriefings and morbidity and mortality rounds.12 Despite the acknowledgement of these milestones, EM-specific competencies have not been identified. The identification of core QIPS competencies within the context of EM would assist in the design of a standardized QIPS curriculum. Although these competencies have been identified for other residency training programs, this represents an area of focus for further EM educational research.Reference Kruszewski28
Limitations
Our study has some limitations. The generalizability of our responses may be limited by our survey response rate of 35.3% and the disproportionate number of residents in the RC compared with the FM-EM training programs. QIPS was also not formally defined in the survey and, therefore, responding residents may have answered questions based on a variable understanding and definition of the term. Approximately one-third of our respondents were junior residents and may not have been aware of QIPS offerings within their program. Furthermore, our results may have been skewed by a disproportionate number of responses from EM residents who are already interested or involved in QIPS activities. Our survey was available in English only, possibly limiting participation from residents in French-speaking residency programs, although 11.6% of respondents were from such programs. Finally, because our study was intended to reflect the residents’ perspective as the end-users of the local educational and structural processes, we did not collect data from program directors or site-specific QIPS content experts. As such, there may be an uncaptured discrepancy between these individuals’ perspectives and the reported resident experience.
CONCLUSION
Our study is the first to assess the Canadian EM residents’ perspectives on the landscape of QIPS education in their residency training programs. Our results indicate that EM residents are interested in receiving education, mentorship, and project opportunities in QIPS, but many perceive an inadequate access to such opportunities, including those who are training in programs with existing QIPS curricula. Future efforts should be aimed at defining EM-specific QIPS competencies, developing standardized QIPS curricula for implementation within residency programs, and enhancing the local and national visibility of QIPS mentors, training, and activities.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2019.465.
Acknowledgements
The authors would like to thank Olivier Levac-Martinho for his contributions to this study.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None declared.







