Fatigue is a common complaint in the general and working population, with a reported prevalence varying from 7% to 45% (Reference Lewis and WesselyLewis & Wessely, 1992; Reference Pawlikowska, Chalder and HirschPawlikowska et al, 1994; Reference Bültmann, Kant and KaslBültmann et al, 2002). In primary care, 5-10% of patients present with fatigue as their main complaint (Reference Sharpe and WilksSharpe & Wilks, 2002). In most of these patients, fatigue lacks a clear somatic cause (Reference Sharpe and WilksSharpe & Wilks, 2002) and appears to be a functional symptom (Reference Wessely, Nimnuan and SharpeWessely et al, 1999; Reference Mayou and FarmerMayou & Farmer, 2002). Fatigue can best be understood as a continuum, ranging from mild complaints frequently seen in the community to severe, disabling fatigue such as chronic fatigue syndrome (Reference Lewis and WesselyLewis & Wessely, 1992). When fatigue becomes severe and persistent, it may lead to long-term sick leave (Reference Janssen, Kant and SwaenJanssen et al, 2003) and work disability (Reference Amelsvoort, Kant and BeurskensAmelsvoort et al, 2002).
Although persistently fatigued patients tend to rely heavily on the care of their general practitioner, evidence-based treatment options in primary care are few, and referral to secondary care is rarely an option. Studies in secondary care have shown that cognitive-behavioural therapy (CBT) delivered by skilled therapists is effective in the treatment of chronic fatigue syndrome (Reference Prins, Bleijenberg and BazelmansPrins et al, 2001; Reference Whiting, Bagnall and SowdenWhiting et al, 2001). It has been suggested that some general practitioners might also provide CBT in the treatment of (chronic) fatigue (Reference Sharpe and WilksSharpe & Wilks, 2002); however, it is unknown whether CBT is effective in less advanced fatigue cases, and whether general practitioners would be able to deliver it.
In this study, we aimed to assess the efficacy of CBT in primary care for unexplained, persistent fatigue. Our hypothesis was that delivering CBT to employees on sick leave for fatigue would reduce the complaints of fatigue and stimulate the resumption of work.
METHOD
Design and procedures
The study was a randomised controlled trial, using an adapted pre-randomisation or randomised consent design (Reference ZelenZelen, 1990) to prevent contamination and selective withdrawal (Reference Knottnerus, Ten Have, Blijham and EngbertsKnottnerus, 1997). The trial was designed to assess the efficacy of the intervention (Reference Scott and SenskyScott & Sensky, 2003), i.e. to assess the potential benefit of the intervention under ideal circumstances. Randomisation took place before detailed information about the study was provided, and patients allocated to one group were kept masked to the randomisation procedure and thus to the existence of the other group. After randomisation, patients were informed only about the procedures in the condition they were allocated to, and informed consent was obtained. Patients were randomised to receive CBT from a general practitioner (GP), or to be followed up in a control group. Allocation to group was carried out by the principal investigator (M.J.H.H.) using cards in sealed, opaque envelopes. A person independent of the study prepared the envelopes by coding them according to a computer-generated list of random numbers. Randomisation was performed in blocks of four and pre-stratified according to ‘duration of absenteeism’. Data were collected on four occasions at baseline measurement, at the end of the treatment period (4 months) and at two follow-up points (8 months and 12 months). The medical ethics committee of Maastricht University approved the study protocol.
Participants
Participants were recruited in collaboration with a local occupational health service, which monitors a working population of 80 000 employees. Employees who were on sick leave (irrespective of the reason) were sent limited study information, including a screening questionnaire, on a monthly basis by the occupational health service, followed by a reminder 2 weeks later. Based on the screening questionnaires that were sent back to the research team, we invited potential candidates who were willing to participate to visit the university research centre. Eligibility was assessed by the principal investigator (M.J.H.H.) in a clinical interview. Inclusion criteria were severe fatigue (a score of 35 or more on the fatigue sub-scale of the Dutch Checklist Individual Strength (CIS; Reference Vercoulen, Alberts and BleijenbergVercoulen et al, 1999; Reference Beurskens, Bültmann and KantBeurskens et al, 2000) for 4 months or more as one of the main health problems, and complete absenteeism from work for 6-26 weeks. Patients were excluded from participation if they had medical conditions that explained fatigue (e.g. cancer); were receiving another intervention for fatigue (e.g. treatment for burnout); had a previously classified psychiatric disorder; or were receiving current psychological treatment (e.g. CBT for major depression). People whose absenteeism was caused primarily by problems unrelated to health, such as work conflict, were also excluded.
Interventions
Participants in both groups were asked to agree to being followed up over a 12-month period. Patients allocated to the experimental treatment group were offered five to seven 30 min sessions of CBT over the course of 4 months. Nine GPs delivered all interventions at their regular practice but outside usual office hours. These ‘research GPs’ were recruited from primary care doctors in the south-east of the Netherlands, on the basis of their geographical location. Patients who agreed to receive CBT were assigned to a research GP near their home address. The intervention was partly based on the CBT programme for chronic fatigue syndrome developed by members of our group (Reference Prins, Bleijenberg and BazelmansPrins et al, 2001). The goals of the intervention were to diminish fatigue and other complaints, establish work resumption and other personal goals, and to establish self-perceived recovery. The intervention itself consisted of two stages:
-
(a) assessment of perpetuating factors such as
-
(i) cognitions (e.g. non-acceptance of fatigue, sense of loss of control over symptoms)
-
(ii) overt behaviour (e.g. disturbed sleeping pattern, unbalanced physical activities)
-
(iii) social factors (e.g. lack of social support, dysfunctional work environment);
-
-
(b) modification of identified perpetuating factors by:
-
(i) explaining the perpetuating circle
-
(ii) settling goals for activities and other problem areas
-
(iii) providing helpful cognitions
-
(iv) planning systematic and gradual work resumption
-
(v) planning achievement of other personal goals
-
(vii) involving the social environment.
-
The intervention procedure was set out in a treatment manual. The research GPs - none of whom had previous experience with CBT - were trained in delivering the intervention in two 5 h workshops, and were supervised in monthly 2 h sessions throughout the trial by two experienced behavioural therapists (G.B., E.B.). No research intervention was offered to patients in the control group. Patients in either group were free to visit their regular GP for usual care.
Outcome assessment
Researchers and research GPs were not masked to the group allocation. All self-reported outcomes were assessed using computerised questionnaires at the research centre (baseline and post-treatment measurement) and postal questionnaires (8-month and 12-month follow-up). Primary outcomes were fatigue severity, absenteeism and ‘clinical recovery’. Fatigue was measured with the fatigue sub-scale of the CIS (Reference Vercoulen, Alberts and BleijenbergVercoulen et al, 1999; Reference Beurskens, Bültmann and KantBeurskens et al, 2000), high scores indicating greater severity. Absenteeism was assessed in two ways, self-reported work resumption or absenteeism (yes/no) at each measurement, and absenteeism registered by the occupational health service (number of partial or complete sick days in 365 days). Clinical recovery was defined as having a CIS fatigue score of 34 or lower in combination with self-reported work resumption.
Secondary outcomes were global perceived effect, physical functioning and psychological distress. Global perceived effect was rated on a seven-point scale (Reference FeinsteinFeinstein, 1987) and then dichotomised into ‘recovered’ and ‘not recovered’. Physical functioning was measured with the physical functioning sub-scale of the 36-item Short Form Health Survey (SF-36; Reference Ware and SherbourneWare & Sherbourne, 1992), high scores indicating high levels of functioning. Psychological distress was measured with the Symptom Check-List 90 (SCL-90; Reference Derogatis, Lipman and CoviDerogatis et al, 1973), high scores indicating high distress.
To assess whether therapy was delivered in accordance with the treatment manual, standardised registration forms were used on which the doctors registered the actions taken in each therapy session and commented on the proceedings. On the basis of these forms and the information gathered in supervision, the CBT supervisors performed a quality check. For each patient in the experimental group, it was assessed whether the CBT received was according to ‘protocol’ - defined as being exposed to all essential steps of the intervention, something that might have been achieved in less than five sessions. In addition, treatment process indicators from our previous fatigue studies (Reference Vercoulen, Swanink and FennisVercoulen et al, 1996; Reference Prins, Bleijenberg and BazelmansPrins et al, 2001; Reference Huibers, Beurskens and PrinsHuibers et al, 2003a ) were used to assess the cognitive impact of the intervention: self-efficacy (sense of control in relation to complaints), psychological attributions (beliefs regarding the psychological cause of complaints) and somatic attributions (beliefs regarding the somatic cause of complaints), high scores indicating high self-efficacy or strong attributions.
Additional measures included psychosocial co-interventions, usual care by the person's regular GP and physical activity. Psychosocial co-interventions (defined as treatment by a psychiatrist, a psychologist and/or psychoactive drug treatment) were measured by self-report and expressed in numbers of patients who received such interventions during the first 4 months after the baseline assessment. Usual GP care was expressed as number of visits to the regular GP during the first 4 months after baseline. Physical activity was measured with the actometer, a motion-sensing device attached to the ankle and worn for 12 days continuously (Reference Van der Werf, Prins and VercoulenVan der Werf et al, 2000); scores reflect the average number of accelerations per 5 min period. High scores indicate high activity, with a mean of 91 (s.d.=25) for healthy individuals.
Sample size and data analysis
In calculating the sample size we chose the fatigue sub-scale of the CIS as our main outcome measure. From the baseline data of the affiliated Maastricht Cohort Study (Reference Kant, Bültmann and SchroerKant et al, 2003), we estimated the standard deviation to be 12. To detect a clinically significant difference of 6 or more on the CIS at a two-sided significance level of 5% and a power of 80% we would need 63 patients per group. We extended the sample size to 75 patients per group to take into account potential withdrawal from the trial. In the main analysis, data were analysed according to the intention-to-treat principle using all available data. The t-test for independent samples (continuous data) and the chi-squared test (dichotomous data) were used to compare the two conditions. Difference scores on continuous outcomes (baseline score minus follow-up score) were used in the analysis. The influence of baseline differences was assessed using linear and logistic regression. An analysis of variance was used to assess the effect of research GP on treatment outcomes. In addition to intention-to-treat analyses, explanatory subgroup analyses were performed. All analyses were performed using the Statistical Package for the Social Sciences, version 11.0.
RESULTS
Recruitment started in January 2000 and was completed in July 2001. Since all employees on sick leave, most of whom were not fatigued, were contacted by the occupational health service, only a small fraction of the responders were eligible for study participation (Fig. 1). Thus, 151 patients were enrolled in the study; after 12 months of follow-up (July 2002), data were available for the 138 patients who completed the study (withdrawal rate 8.6%).
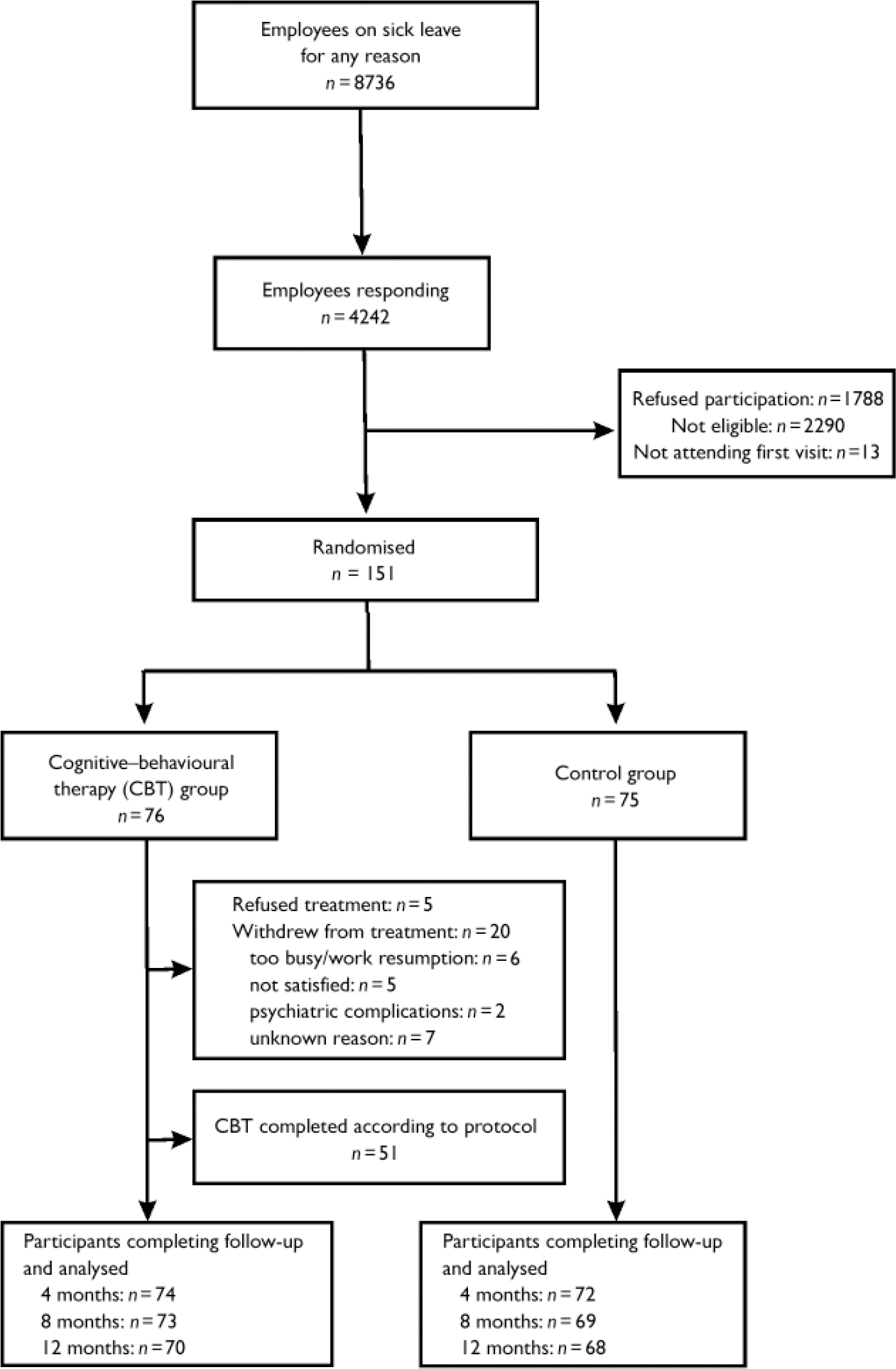
Fig. 1 Flowchart of patient recruitment, allocation and outcome assessments.
Baseline demographic and clinical characteristics were fairly similar in both groups, except for physical functioning and psychological distress (Table 1). Adjustment for these two factors did not change the findings. Patients were identified as potentially having chronic fatigue syndrome (CFS-like cases) if they met all of the following research criteria (Reference Fukuda, Straus and HickieFukuda et al, 1994): a CIS score of 40 or higher; a duration of fatigue complaints of 6 months or more; and an SF-36 score on the physical functioning sub-scale of 60 or lower. At baseline, 66 patients (44%) met research criteria for chronic fatigue syndrome, none of whom reported a previous diagnosis of the syndrome. One patient indicated that she believed she suffered from chronic fatigue syndrome.
Table 1 Baseline characteristics of study participants
| Characteristics | CBT group (n=76) | Control group (n=75) |
|---|---|---|
| Gender (male/female): n (%) | 37/39 (49/51) | 31/44 (41/59) |
| Age (years): mean (s.d.) | 43.6 (8.9) | 43.3 (7.7) |
| Education (1, low; 7, high): mean (s.d.) | 3.8 (1.7) | 3.8 (1.5) |
| Fatigue severity (CIS, possible score 35-56): mean (s.d.) | 48.8 (5.3) | 48.5 (7.1) |
| Duration of fatigue complaints (months): mean (s.d.) | 27.9 (31.4) | 26.9 (27.6) |
| Duration of absenteeism (weeks): mean (s.d.) | 12.6 (5.9) | 12 (3.7) |
| Other health complaints: n (%) | ||
| Painful joints/limbs | 30 (40) | 34 (45) |
| Stress | 22 (29) | 20 (27) |
| Headache | 17 (22) | 16 (21) |
| Back pain | 12 (16) | 17 (23) |
| Poor concentration or memory | 14 (18) | 13 (17) |
| Depressed mood | 10 (13) | 16 (21) |
| Sleep disturbance | 12 (16) | 11 (15) |
| Dizziness | 12 (16) | 10 (13) |
| Lack of energy | 8 (11) | 11 (15) |
| Bowel, abdominal or stomach complaints | 8 (11) | 7 (9) |
| Other | 17 (22) | 17 (23) |
| Physical functioning (SF-36, possible score 0-100): mean (s.d.) | 56.7 (25) | 67.1 (22) |
| Psychological distress (SCL-90, possible score 90-450): mean (s.d.) | 175 (42) | 190 (57) |
| General physical activity (actometer): mean (s.d.)1 | 67 (22) | 69.5 (22) |
| ‘CFS-like cases’: n (%)2 | 36 (47) | 30 (40) |
Outcomes
Table 2 presents the clinical outcomes at baseline, 4 months and 12 months. There was no significant difference between the CBT group and the control group on any clinical outcome at any point (including the 8-month assessment).
Table 2 Clinical outcomes
| Clinical outcome | CBT group (n=76) | Control group (n=75) | Difference (95% Cl)1 |
|---|---|---|---|
| Fatigue severity (CIS score): mean (s.d.) | |||
| t 0 | 48.8 (5.3) | 48.5 (7) | |
| t 1 | 38.2 (12.7) | 39.8 (13.7) | 2.2 (-1.7 to 6.1) |
| t 3 | 35.5 (12.9) | 33.9 (13.8) | -0.5 (-5 to 3.9) |
| Work resumers: % (n) | |||
| t 1 | 50 (37) | 61 (44) | -11% (-23 to 1) |
| t 3 | 59 (41) | 65 (44) | -6% (-23 to 10) |
| Registered absenteeism (days): mean (s.d.) | |||
| t 3 | 234 (116) | 230 (116) | 4 (-35.9 to 44) |
| Clinical recovery: % (n)2 | |||
| t 1 | 24 (18) | 28 (20) | -4% (-18 to 11) |
| t 3 | 33 (23) | 43 (29) | -10% (-26 to 6) |
| Perceived recovery: % (n)3 | |||
| t 1 | 38 (28) | 39 (28) | -1% (-17 to 15) |
| t 3 | 49 (34) | 53 (36) | -4% (-21 to 12) |
| Physical functioning (SF-36) score: mean (s.d.) | |||
| t 0 | 56.8 (25) | 67.1 (22) | |
| t 1 | 65.2 (25.8) | 72.5 (19.1) | -4.4 (-10.9 to 2.1) |
| t 3 | 70.1 (24.7) | 77.4 (20.9) | -3.6 (-10.4 to 3.1) |
| Psychological distress (SCL-90 score): mean (s.d.) | |||
| t 0 | 175 (42) | 190 (57) | |
| t 1 | 156 (42) | 163 (55) | -10.4 (-23.5 to 2.7) |
| t 3 | 152 (51) | 153 (62) | -11.4 (-27.1 to 4.3) |
Treatment received
Five patients allocated to the CBT group immediately refused the treatment offered to them (Fig. 1). Of the remaining 71 patients who agreed to receive treatment, 51 patients (72%) completed the intervention according to protocol. The mean number of CBT sessions attended was 5.3 (s.d.=1.9), with a mean duration of 33.7 min (s.d.=9.4). In addition, 13 patients (18% of 74) in the CBT group underwent psychosocial co-interventions during the first 4 months (intervention period) compared with 22 patients (31% of 72) in the control group (95% CI for the difference, -1% to 27%). The mean numbers of visits to the regular GP in the intervention period were 4.2 (s.d.=4.5) in the CBT group and 3.5 (s.d.=4.3) in the control group (95% CI for the difference, -0.8 to 2.1). No adverse event attributable to CBT was reported. Table 3 presents scores on the treatment process indicators assessed at baseline and follow-up. There was no difference between the CBT and the control group. Moreover, post-treatment scores remained stable in both groups compared with baseline.
Table 3 Treatment process indicators
| Indicator | CBT group (n=76) mean (s.d.) | Control group (n=75) mean (s.d.) | Difference1 (95% Cl) |
|---|---|---|---|
| Self-efficacy (possible score 5-24) | |||
| t 0 | 15.4 (3.5) | 14.9 (3.5) | |
| t 1 | 16.6 (3.9) | 16.4 (3.6) | 0.2 (-0.9 to 1.3) |
| Psychological attributions (possible score 7-28) | |||
| t 0 | 18.3 (4.5) | 19.4 (4.1) | |
| t 1 | 18.4 (4.8) | 19.2 (3.8) | -0.3 (-1.3 to 0.8) |
| Somatic attributions (possible score 4-16) | |||
| t 0 | 9.3 (2.5) | 9.3 (2.6) | |
| t 1 | 9.5 (2.6) | 9.4 (2.6) | -0.1 (-0.8 to 0.6) |
Outcomes in CBT completers
We compared the baseline characteristics of those who completed CBT according to protocol (n=51) with those who refused or withdrew from CBT (non-completers, n=25) and found that CBT completers were similar to non-completers at baseline. Clinical outcomes and scores on treatment process indicators for the completers group were then compared with scores in the control group (n=75). There was no significant or noticeable difference between these groups.
Subgroup analyses
Although some differences appeared between individual research GPs in treatment effect, no overall GP effect on clinical outcomes was found. Patients were stratified according to fatigue severity (CIS score 35-49, n=74; CIS score 50-56, n=77), duration of absenteeism (6-12 weeks, n=90; ≥13 weeks, n=61), duration of fatigue complaints (4-12 months, n=79; ≥13 months, n=72), CFS-like caseness (yes, n=66; no, n=85), gender (men, n=68; women, n=83), age (≤44 years, n=81; ≥45 years, n=77) and education (low, n=109; high, n=42) at baseline. There was no significant or noticeable effect of CBT compared with the control group in any of these categories.
DISCUSSION
Cognitive-behavioural therapy delivered by general practitioners to employees absent from work had no substantial effect on clinical outcomes or cognitive processes during 12 months of follow-up. This finding could not be explained by a difference in effect among research GPs or by withdrawal from treatment in the CBT group. Exploratory analyses in relevant subgroups revealed no significant or noticeable effects of CBT.
Methodological considerations
This is the second study of CBT by GPs for fatigue. In the first, preliminary study, it was concluded that primary care doctors were unable to treat chronic fatigue syndrome effectively (Reference Whitehead and CampionWhitehead & Campion, 2002), but the strength of this study should be questioned because of poor recruitment and high withdrawal rates. We designed our trial to assess whether the intervention works under ideal circumstances. Consequently, we chose to train and deploy a small number of research GPs, instead of a large sample of GPs who would have had to treat their own patients. Masking is virtually impossible in this type of research, and therefore we used a prerandomisation design to control for contamination between groups and to prevent selective withdrawal from the study (Reference Knottnerus, Ten Have, Blijham and EngbertsKnottnerus, 1997). In our view, the low withdrawal rate (8.6% of 151 patients) outweighs the occasional refusal of treatment as a result of the design.
As could be expected, patients in the control group received more co-interventions, which might have led to an underestimation of the effect of CBT. A limitation of this study is the nature of our quality check: we used registration forms instead of audiovisual recordings to assess the quality of the CBT that was delivered and, as a result, we cannot be certain that the research GPs actually did what they claimed to have done.
Previous studies
This is the first study on CBT for fatigue in primary care that adequately controlled for usual care. Treatment of chronic fatigue by skilled cognitive-behavioural therapists was no more effective than counselling in a study by Ridsdale et al (Reference Ridsdale, Godfrey and Chalder2001), but these interventions were not compared with either no treatment or usual care. It is interesting to find that the proportion of patients who failed to complete CBT in our study (33%) is comparable with rates of withdrawal from therapy in primary care (Reference Ridsdale, Godfrey and ChalderRidsdale et al, 2001) and secondary care (Reference Prins, Bleijenberg and BazelmansPrins et al, 2001) studies investigating CBT for chronic fatigue.
Few earlier studies have addressed the effectiveness of CBT provided by GPs. In a recent study by King et al (Reference King, Davidson and Taylor2002), teaching CBT skills to GPs proved ineffective. However, the extent to which GPs actually applied their skills was not assessed in that study. In a review for the Cochrane Collaboration (Reference Huibers, Beurskens and BleijenbergHuibers et al, 2003b ), we found little evidence for the effectiveness of psychosocial interventions by GPs, except for a favourable effect of problem-solving treatment by a small number of experienced GPs on major depression (Mynors-Wallis et al, Reference Mynors-Wallis, Gath and Lloyd Thomas1995, Reference Mynors-Wallis, Gath and Day2000). In general, positive effects of psychosocial interventions seemed to be associated with a small number of GPs (10 or fewer) treating many patients (Reference Huibers, Beurskens and BleijenbergHuibers et al, 2003b ).
Can the lack of efficacy be explained?
The lack of efficacy in this study cannot be attributed to clear methodological flaws: interventions were delivered under ‘ideal circumstances’ as opposed to routine care evaluations, study conditions were highly contrasted, and the majority of patients and GPs appeared compliant with the protocol. Rather, the lack of efficacy is likely to result from a disturbance in the interaction between the patient, the doctor and the intervention. Our study was not designed to reveal the source of the disturbance in this triad. However, a plausible explanation for our findings would be that research GPs did not treat enough patients to gain the necessary experience in delivering the complex intervention. Also, since many patients were characterised at baseline by an advanced degree of impairment in terms of fatigue, psychological distress and physical functioning, they might have had better chances for improvement in secondary mental health care (Reference Prins, Bleijenberg and BazelmansPrins et al, 2001). This might be particularly true for those who met the research criteria for chronic fatigue syndrome. On the other hand, one might claim that the substantial (natural) recovery in both groups is partly accountable for the lack of difference in effect between the conditions, leading to the possibility that the brief intervention was not adequate, specific or intensive enough for those who did not recover in the course of time. An additional difficulty might have been that the intervention was targeted not only at fatigue but also at the resumption of work, a complex process that is determined by a wide variety of factors.
How do our findings reflect on the evidence for the effectiveness of CBT in patients with chronic fatigue syndrome? We should keep in mind that our study differs from those of Prins et al (Reference Prins, Bleijenberg and Bazelmans2001) and Whiting et al (Reference Whiting, Bagnall and Sowden2001) in important ways. We did not deploy experienced CBT therapists but relatively inexperienced GPs; our study population consisted of individuals with a different profile (e.g. impairment, attitudes, illness beliefs, prognosis) from that of patients with ‘classic’ chronic fatigue syndrome in secondary care; and our CBT intervention consisted of only half the number of sessions administered in other studies. Apparently, these factors have to be matched appropriately for CBT to be successful in patients with chronic fatigue syndrome.
Implications for treatment
A recent review concluded that it cannot be assumed that psychosocial treatments in secondary care will produce the same magnitude of effect in primary care (Reference Raine, Haines and SenskyRaine et al, 2002), owing to differences in prognostic spectrum, treatment regimen and treatment provision. Effective CBT for chronic fatigue syndrome in secondary care consisted of approximately 16 sessions given by skilled and supervised specialists (Reference Prins, Bleijenberg and BazelmansPrins et al, 2001). In primary care, however, more treatment sessions or more training (Reference King, Davidson and TaylorKing et al, 2002) seem not to be a feasible option. Even under ideal circumstances, our research GPs were unable to deliver CBT effectively. In our opinion, it is unlikely that GPs in routine practice would be any more successful in delivering a complex psychosocial treatment such as CBT.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ ▪ Cognitive-behavioural therapy (CBT) by general practitioners did not prove to be an effective intervention for unexplained, persistent fatigue. It should be doubted whether this treatment approach provides a valuable contribution to clinical practice.
-
▪ ▪ In line with findings from a recent Cochrane review, this study adds to the notion that complex psychosocial interventions are not likely to be effective when delivered by primary care doctors.
-
▪ ▪ Many patients in this study met criteria for chronic fatigue syndrome. These patients are likely to be better off receiving specialist treatment for this condition in secondary care.
LIMITATIONS
-
▪ ▪ Co-interventions in the control group might have led to an underestimation of the effect of CBT.
-
▪ ▪ More than a quarter of the patients in the experimental group withdrew from therapy.
-
▪ ▪ Our trial was not designed to identify the factors that contributed to the lack of efficacy in this study.
Acknowledgements
This research project was funded by the Health Research and Development. Council (ZorgOnderzoek Nederland), The Netherlands (grant 2830180). The. recruitment of patients was made possible by the donation of services by. Occupational Health Service Limburg (Arbo Unie Limburg). The authors wish to. thank Dr Ludovic van Amelsvoort for statistical advice.







eLetters
No eLetters have been published for this article.