Introduction
Borderline personality disorder (BPD) is a complex mental health condition affecting 1–6% of the population, with many of those diagnosed with BPD (c.85%) being women of child-rearing age (Coid et al., Reference Coid, Yang, Tyrer, Roberts and Ullrich2006; Grant et al., Reference Grant, Chou, Goldstein, Huang, Stinson, Saha, Smith, Dawson, Pulay, Pickering and Ruan2008). The pervasive functional impairments in emotion regulation, interpersonal relationships, identity disturbance, and behavioral control associated with BPD (American Psychiatric Association, 2013) are recognized as having a substantial impact on family organization and functioning (Feldman et al., Reference Feldman, Zelkowitz, Weiss, Vogel, Heyman and Paris1995) and poor developmental outcomes for children of parents with BPD (Stepp, Reference Stepp2012). As such, there is increasing interest in the impact of maternal BPD on parenting, with studies identifying a number of parenting challenges, such as diminished sensitivity, augmented overprotectiveness, and increased hostility (e.g., Apter et al., Reference Apter, Devouche, Garez, Valente, Genet, Gratier, Dominguez and Tronick2017; Eyden et al., Reference Eyden, Winsper, Wolke, Broome and MacCallum2016; Høivik et al., Reference Høivik, Lydersen, Ranøyen and Berg-Nielsen2018; Kiel et al., Reference Kiel, Viana, Tull and Gratz2017).
Previous studies have explored potential contributory factors to parenting in mothers with BPD, such as the child’s temperament (Abela et al., Reference Abela, Skitch, Auerbach and Adams2005; Zalewski et al., Reference Zalewski, Stepp, Scott, Whalen, Beeney and Hipwell2014), maternal emotional dysregulation (Gratz et al., Reference Gratz, Kiel, Latzman, Elkin, Moore and Tull2014), and maternal mind-mindedness (Schacht et al., Reference Schacht, Hammond, Marks, Wood and Conroy2013). However, no studies to date have examined the key question of whether mothers with BPD possess the knowledge of what makes an "ideal"Footnote 1 sensitive mother. Understanding levels of sensitive parenting knowledge is important as maternal sensitivity is well documented as being essential for children’s secure attachment (e.g., Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Juffer2003), self-esteem (e.g., Shaffer & Kipp, Reference Shaffer and Kipp2010), and as a protective factor in a range of physical, cognitive, and socio-emotional difficulties (for a review see Deans, Reference Deans2020).
Although less researched than other parenting domains, parenting knowledge matters as it shapes parenting cognitions, behaviors, and developmental expectations (Bornstein et al., Reference Bornstein, Yu and Putnick2020). The extant literature shows parenting knowledge is associated with parenting practices (Bornstein et al., Reference Bornstein, Cote, Haynes, Hahn and Park2010, Reference Bornstein, Yu and Putnick2020; Okagaki & Bingham, Reference Okagaki, Bingham, Luster and Okagaki2005), parenting competence (Winter et al., Reference Winter, Morawska and Sanders2012), and successful interpretations of child behavior (Bugental & Corpuz, Reference Bugental, Corpuz and Bornstein2019; Bugental & Happaney, Reference Bugental, Happaney and Bornstein2002). Parents who are ill-informed about parenting have incongruent child expectations and experience more parental stress (Winter et al., Reference Winter, Morawska and Sanders2012). Lower parenting knowledge has potential implications on child outcomes such as internalizing behavior (Winter et al., Reference Winter, Morawska and Sanders2012), poorer mother-child interactions, and inappropriate discipline (Goodnow, Reference Goodnow and Bornstein2002; Huang, Reference Huang, Caughy, Genevro and Miller2005). Also, parenting knowledge is associated with increased age and higher education (Bornstein et al., Reference Bornstein, Cote, Haynes, Hahn and Park2010), which is notable as mothers with BPD typically are younger when becoming a parent (Zanarini et al., Reference Zanarini, Frankenburg, Reich, Wedig, Conkey and Fitzmaurice2015) and have lower education attainment (Bagge et al., Reference Bagge, Nickell, Stepp, Durrett, Jackson and Trull2004). Furthermore, parenting knowledge is associated with enhanced perceptions of parenting self-efficacy (Bornstein et al., Reference Bornstein, Hendricks, Hahn, Haynes, Painter and Tamis-LeMonda2003, Reference Bornstein, Putnick and Suwalsky2018), that is, the mother’s belief regarding her ability to parent successfully (Jones & Prinz, Reference Jones and Prinz2005), which is salient given the consistent association between parenting self-efficacy, maternal mental health, and a range of parenting perceptions, practices, and child outcomes (e.g., Bornstein et al., Reference Bornstein, Putnick and Suwalsky2018; Goodman et al., Reference Goodman, Simon, McCarthy, Ziegler and Ceballos2022; Jones & Prinz, Reference Jones and Prinz2005; Vance & Brandon, Reference Vance and Brandon2017). Therefore, exploring the knowledge that mothers with BPD possess of sensitive parenting and their perceptions of their parenting self-efficacy may be key to informing future effective interventions. As BPD and depression often co-occur (83% lifetime prevalence of major depressive disorder; Zanarini et al., Reference Zanarini, Frankenburg, Dubo, Sickel, Trikha, Leniv and Reynolds1998), the present study will also compare to mothers with depression, and healthy mothers.
Mothers with BPD report feeling less competent and less satisfied with their parenting than healthy comparison mothers (Elliot et al., Reference Elliot, Campbell, Hunter, Cooper, Melville, McCabe, Newman and Loughland2014; Newman et al., Reference Newman, Stevenson, Bergman and Boyce2007; Steele et al., Reference Steele, Townsend and Grenyer2020), and the identity disturbance and unstable sense of self often experienced by those with BPD can manifest in low self-confidence and poor self-regard (e.g., Zeigler-Hill & Abraham, Reference Zeigler-Hill and Abraham2006). Perceptions of their parenting being judged by others as poor (Lerner, Reference Lerner2021) may be further exacerbated by BPD symptomatology and impact on their parenting self-efficacy. Depression is also associated with parenting difficulties (Lovejoy et al., Reference Lovejoy, Graczyk, O'Hare and Neuman2000). Mothers with depression experience low self-esteem and poor self-concept (e.g., Fennell, Reference Fennell2004; Fox, Reference Fox2000), and studies show low parenting self-efficacy is associated with maternal depression (Kohlhoff & Barnett, Reference Kohlhoff and Barnett2013).
A history of childhood adversity is often associated with BPD (Battle et al., Reference Battle, Shea, Johnson, Yen, Zlotnick, Zanarini, Sanislow, Skodol, Gunderson, Grilo, McGlashan and Morey2004; Carlson et al., Reference Carlson, Egeland and Sroufe2009; Linehan, Reference Linehan1993), in particular abuse, neglect (Spatz Widom et al., Reference Spatz Widom, Czaja and Paris2009; Zanarini et al., Reference Zanarini, Williams, Lewis, Reich, Vera, Marino, Levin, Yong and Frankenburg1997, Reference Zanarini, Yong, Frankenburg, Hennen, Reich, Marino and Vujanovic2002), and family adversity (Winsper et al., Reference Winsper, Zanarini and Wolke2012), with childhood adversity 13 times more likely in BPD than in other clinical and non-clinical controls (Kleindienst et al., Reference Kleindienst, Vonderlin, Bohus and Lis2021; Porter et al., Reference Porter, Palmier-Claus, Branitsky, Mansell and Warwick2020). Parenting received in childhood by those later diagnosed with BPD has been found to be typically more conflicting (Winsper et al., Reference Winsper, Zanarini and Wolke2012), less caring and affectionate (Bandelow et al., Reference Bandelow, Krause, Wedekind, Broocks, Hajak and Ruther2005), and inconsistent and invalidating (Zanarini et al., Reference Zanarini, Williams, Lewis, Reich, Vera, Marino, Levin, Yong and Frankenburg1997). Furthermore, from a social learning theory perspective (Bandura, Reference Bandura1977) being less likely to have been exposed to or had opportunity to observe appropriate parenting during childhood (Pears & Capaldi, Reference Pears and Capaldi2001) may generate maladaptive parenting schemas when later becoming a parent. Childhood adversity is also associated with severe chronic depression (Negele et al., Reference Negele, Kaufhold, Kallenbach and Leuzinger-Bohleber2015). However, as depression can be of varied etiology, duration, and severity (NHS, 2020; Wang et al., Reference Wang, Wu, Lai, Long, Zhang, Li, Zhu, Chen, Zhong, Liu, Wang and Lin2017) potentially limited to a current event/life circumstance rather than associated with adverse childhood experiences, childhood adversity may be less prevalent for mothers with depression than for those with BPD. As such, any associations with childhood maltreatment (and subsequent poor parenting experiences/maladaptive parenting schemas) are potentially less prevalent, and parenting knowledge may be only mildly or not affected in those with maternal depression only, compared to mothers with BPD.
While often difficult to untangle comorbidities, it is important to delineate whether BPD, depression, or their combination is associated with parenting knowledge and self-efficacy, or whether it is the severity of maternal mental health, which has previously found to be associated with parenting difficulties, and child development outcomes (e.g., Brennan et al., Reference Brennan, Hammen, Andersen, Bor, Najman and Williams2000; Mars et al., Reference Mars, Collishaw, Smith, Thapar, Potter, Sellers, Harold, Craddock, Rice and Thapar2012). Low social support is also associated with low parenting self-efficacy (Angley et al., Reference Angley, Divney, Magriples and Kershaw2015), with larger social support networks associated with increased parenting knowledge (Cochran & Niegro, Reference Cochran, Niegro and Bornstein2002); therefore, perceived social support was also explored in this current study. Parents typically rely on familiar sources for knowledge (Cochran & Niegro, Reference Cochran, Niegro and Bornstein2002), and as mothers with BPD have fewer people for support and parenting discussions (Dunn et al., Reference Dunn, Cartwright-Hatton, Startup and Papamichail2020), often experience relationship instability (American Psychiatric Association, 2013), and have unstable social support (Clifton et al., Reference Clifton, Pilkonis and McCarty2007), maternal perceived social support may be associated with parenting knowledge and/or self-efficacy. Further, with potentially fewer positive parenting models to draw upon, and with parenting most often learned from own parents (Dunn et al., Reference Dunn, Cartwright-Hatton, Startup and Papamichail2020), it is possible that when becoming a mother themselves their idea of appropriate sensitive parenting is limited or distorted.
The current study
The current study addressed a gap in the literature by exploring knowledge of "ideal" sensitive parenting and perceived parenting self-efficacy in mothers with BPD compared to mothers with depression, and mothers with no mental health difficulties. This investigation aimed to begin to understand how knowledge and self-efficacy are impacted in maternal clinical populations (BPD and depression) with the intention that findings would inform further exploration of the impacts of knowledge and self-efficacy on maternal parenting practices, as well as improving targeting of parenting interventions. The study addressed these questions: Do mothers with BPD have knowledge of sensitive parenting and/or diminished parenting self-efficacy, and are differences in parenting knowledge or self-efficacy specific to BPD or are comparable differences also found in mothers with depression? Are childhood adversity, mental health symptom severity, or social support associated with knowledge and self-efficacy outcomes? We first hypothesized that mothers with BPD will have lesser knowledge of sensitive parenting than mothers with depression or no mental health difficulties (H1), and second that both mothers with BPD and depression will have lower parenting self-efficacy than healthy comparison mothers (H2). Finally, we hypothesized that childhood adversity, symptom severity, and perceived social support are the major factors associated with poor parenting knowledge and diminished self-efficacy (H3).
Method
Participants
This study is part of a UK National Health Service (NHS) approved study (16/WM/0076, project ID:105429) exploring the parenting of mothers with BPD. Mothers were included if they were age 18 or over, fluent in English, had a child up to age 12 who had lived with them for the majority of the child’s life, and prior to identification for recruitment had either:
-
a. received a primary clinical diagnosis of BPD (BPD group),
-
b. received a primary clinical diagnosis of depression (DPN group) or
-
c. had experienced no mental health difficulties whilst being a parent (healthy comparison, HC group).
Mental illness diagnoses had been made independently by a clinician using DSM/ICD diagnostic criteria (American Psychiatric Association, 2000; World Health Organization, 2004), and participants were not so severely impaired that they were unable to participate.
Recruitment took place from 2017 to 2018 in England, UK. Mothers with BPD were recruited from psychiatry services, dialectical behavior therapy clinics, or personality disorder services; mothers with depression were recruited from clinical services (psychiatry and psychology) or community services (mother and baby groups, school newsletters, social media); and mothers with no mental health difficulties were recruited from similar community services. In all contexts, interested mothers were given the study information and signed consent-to-contact was obtained. Consenting mothers were contacted to assess eligibility. Non-response rates could not be calculated due to the nature of recruitment; however, drop-out rates after consenting to be contacted or agreeing to participate were BPD n = 2; DPN n = 7; HC n = 5. Child age range was kept broad to maximize the recruitment potential of mothers with BPD. Due to developmental differences, children’s developmental stage was stratified between groups, as was educational level of mothers.
A total of 76 mothers participated: BPD n = 26, DPN n = 25, HC n = 25. A priori power analysis using G-Power 3.1 (Faul et al., Reference Faul, Erdfelder, Lang and Buchner2007) indicated a total of 73 participants to yield power of 0.95 for detecting medium effects with ANOVA statistics.Footnote 2 Home visits lasted approximately 2½ hr (one participant was seen at the University lab). Informed written consent was obtained. Mother’s ages ranged from 20 to 54 years (M years = 33.35, SD = 7.59), and child ages from 5 months to 11 years (M months = 51.37, SD = 38.40). Significant between-group differences showed that mothers with BPD were the youngest with a mean age of 30 and were less likely to be in employment (Table 1). There were no group differences regarding mothers’ qualification level, relationship/marital status, or ethnicity; children’s ages (in months or developmental stage), gender, number of siblings, or presence of child learning/mental health difficulties; nor for the clinical groups with diagnosis duration or therapy history.
Table 1. Mother and child demographic characteristics
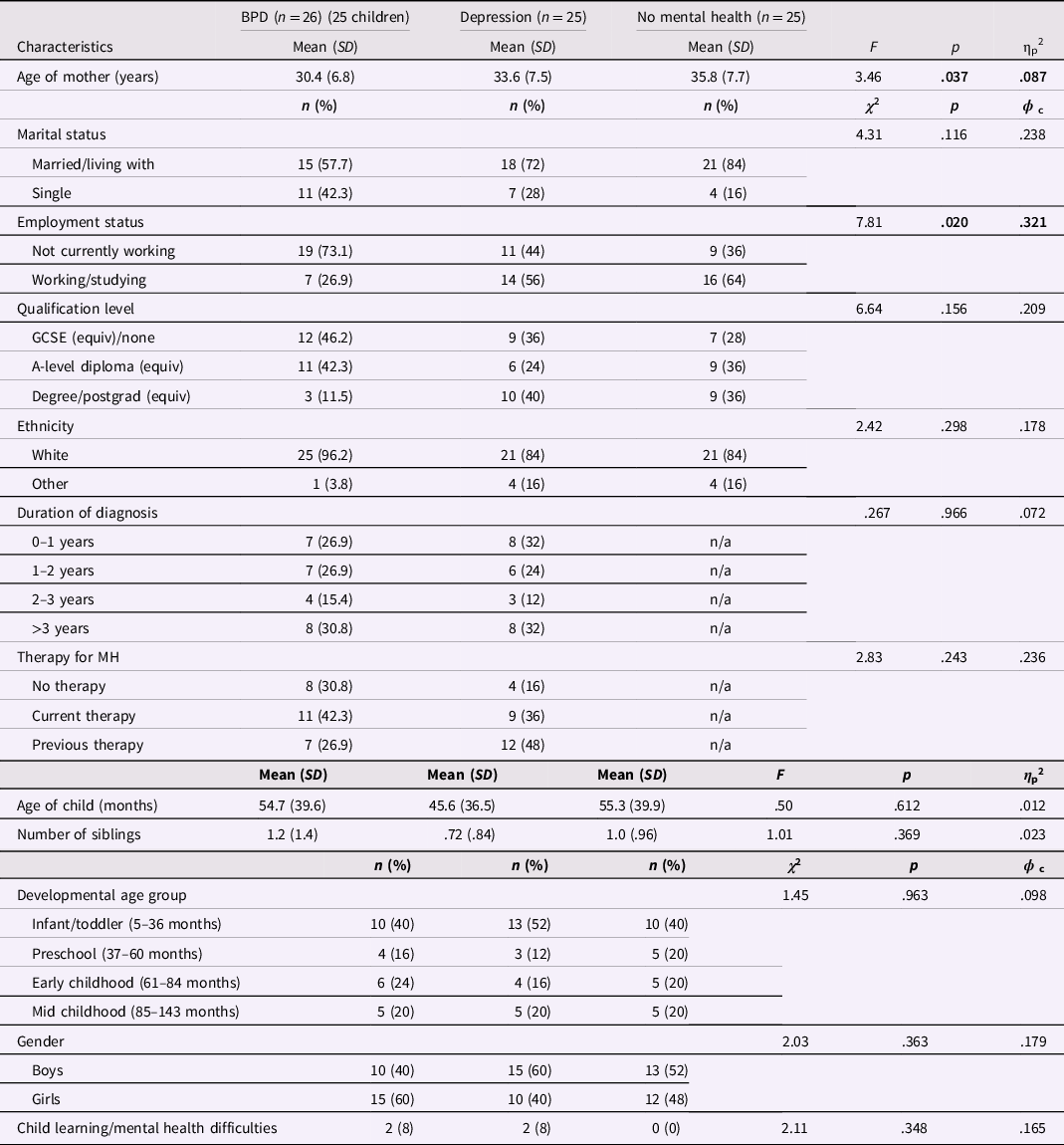
Notes. MH = mental health.
Values in the table in bold denote those reaching statistical significance.
Measures
All participating mothers completed the following questionnaires.
BPD
The Personality Assessment Inventory (PAI-BOR; Morey, Reference Morey1991) is a 24-item self-report Likert scale questionnaire used to assess the BPD subscales of affective instability, identity disturbance, negative relationships, and impulsivity/self-harming. The PAI-BOR has concurrent validity with DSM-IV (APA, 2000) and SCID-II (First et al., Reference First, Gibbon, Spitzer, Williams and Benjamin1997). Possible scores range from 0 (not true at all) to 3 (very true). Consistent with Morey’s PAI scoring, subscale totals and overall total scores were transformed to T-scores for analyses to provide comparison with normative community sample scores (Morey, Reference Morey1991). Cronbach’s alpha for the current sample was .92.
Depression
Current depression symptoms were measured using the Patient Health Questionnaire (PHQ-9; Kroenke et al., Reference Kroenke, Spitzer and Williams2001), a 9-item self-report Likert scale questionnaire. Possible scores range from 0 (not at all) to 3 (nearly every day). Validity and reliability for the PHQ-9 have been well established (e.g., Löwe, Spitzer, et al., Reference Löwe, Spitzer, Gräfe, Kroenke, Quenter, Zipfel, Buchholz, Witte and Herzog2004; Löwe, Unützer, et al., Reference Löwe, Unützer, Callahan, Perkins and Kroenke2004), and is the measure used by NHS, England. Cronbach’s alpha for the current sample was .93.
Knowledge of sensitive parenting
A Q-sort task was used to assess mothers’ knowledge of the behaviors that most indicate a sensitive mother. The maternal behavior Q-set (MBQS) was based on and correlates highly with Ainsworth’s scales of maternal sensitivity and attachment (Behrans et al., Reference Behrans, Parker and Haltigan2011, Reference Behrans, Hart and Parker2012), and has been used with a variety of populations including mothers with psychopathology (e.g., Kim & Kim, Reference Kim and Kim2009). It was originally designed by Pederson and Moran (Reference Pederson and Moran1995) for clinician use and later adapted by Mesman et al. (Reference Mesman, van IJzendoorn, Behrens, Carbonell, Carcamo, Cohen-Paraira, de la Harpe, Ekmekçi, Emmen, Heidar, Kondo-Ikemura, Mels, Mooya, Murtisari, Noblega, Ortiz, Sagi-Schwartz, Sichimba, Soares and Zreik2015) for self-report. Ninety behavior statements are ranked from the most ideal to the least ideal sensitive mother behaviors. Examples of behavior statements include “Makes sure she can hear or see her child”; “Her responses to her child are unpredictable.” Pilot testing revealed a few misinterpretations of the Mesman-adapted statements, which were amended whilst retaining Pederson and Moran’s intended meanings (supplementary item 1 shows the full list). Correlation coefficients were computed comparing the mother-ranked behavior scores with Pederson and Moran’s criterion of an ideal sensitive mother (MBQS-score). High MBQS scores indicate an understanding of maternal sensitive parenting behavior. A discrepancy score was calculated to denote the number of items which differ by 3 or more from Pederson and Moran’s criterion score representing behaviors ranked in a different category (e.g., an “ideal” statement ranked as “not ideal”).
Parenting self-efficacy
Mothers’ parenting self-efficacy was measured using the Tool to Measure Parenting Self-Efficacy (TOPSE; Kendall & Bloomfield, Reference Kendall and Bloomfield2005). The TOPSE is a 48-item self-report Likert scale questionnaire, which assesses eight parenting domains: emotion and affection; play and enjoyment; empathy and understanding; control; discipline and setting boundaries; parenting pressure; parenting self-acceptance; and parenting knowledge and learning. In each parenting domain are six items to rate; for example: “I am able to stay calm when my child is behaving badly” (Control subscale), “I find it hard to cuddle my child” (Emotion and Affection), “I am able to have fun with my child” (Play & Enjoyment). Possible scores range from 0 (completely disagree) to 10 (completely agree). A score was given for each subsection, however as the adapted TOPSE baby questionnaire (for mothers with a child under 12 months) excludes the domains of Control and Discipline, for comparability the overall TOPSE score was converted to a percentage score for each participant (TOPSE%). The TOPSE has good internal and external reliability and construct validity (e.g., Bloomfield & Kendall, Reference Bloomfield and Kendall2007). Cronbach’s alpha for the current sample was .97.
Childhood adversity
Mothers’ recall of their own childhood adversity was measured using the Adverse Childhood Experiences questionnaire (ACE-IQ; World Health Organization, 2018). The ACE-IQ has robust validity and reliability and is widely used (e.g., Kazeem, Reference Kazeem2015; Wingenfeld et al., Reference Wingenfeld, Schäfer, Terfehr, Grabski, Driessen, Grabe, Löwe and Spitzer2010). Items on neglect (emotional and physical), abuse (emotional, physical, and sexual), family household adversities (witnessing home violence; household member with substance abuse, psychopathology, or incarcerated; separation/death of a parent), and bullying are included in an 11-subcategory, 23-item self-report Likert scale questionnaire. Possible responses range from always to never for questions regarding occurrence of an event, and yes/no for binary questions. Responses were coded using the ACE-IQ score calculation guide (WHO, 2020). The ACE-binary scale denotes the presence/absence of each ACE, and ACE-frequency the prevalence of each adversity. Possible scores range from 0–11 on each scale (to represent each ACE-IQ subcategory above), the higher the ACE scores the greater the childhood adversity. Cronbach’s alphas for the current sample were .82 (ACE-binary) and .83 (ACE-frequency).
Perceived social support
The Significant Others Scale (SOS, Power et al., Reference Power, Champion and Aris1988) measured the levels of received and preferred emotional and practical support from significant others in the mother’s life. The SOS includes four self-report Likert scale questions assessing the level of support received (e.g., “Can you trust, talk to frankly and share feelings with this person?”). To capture preferred/ideal support, each question was followed by “what rating would your ideal be?” Possible scores ranged from 0 (never) to 7 (always); participants could report up to four significant persons. SOS variables were created for received/actual support, preferred/desired support, and a discrepancy score of preferred minus received support. Cronbach’s alphas for the current sample were .90 (received support) and .91 (preferred support).
Procedures
Mothers provided demographic information (Table 1) and completed clinical, adverse childhood, and parenting self-efficacy questionnaires. For the 4-sort Q-sort task, mothers were asked to consider the "ideal" behaviors of a sensitive mother parenting a 0–3-year-old.Footnote 3
Sort 1: Mothers sorted the behavior cards into piles of most ideal, least ideal, or neither most nor least ideal parenting. The cards were then ranked from 9-1 (sorts 2, 3, & 4 below) with 9 representing the most ideal maternal parenting behaviors.
Sort 2. From the ideal behaviors pile, mothers chose the top 10 behaviors (ranked as 9), the 10 next most ideal behaviors (ranked 8), and then the 10 they ranked as 7. Any remaining cards were placed in the neither/nor pile.
Sort 3. The least ideal pile was ranked in a similar manner from 1 to 3 with 10 in each (1 being the least ideal). Any remaining cards were placed in the neither/nor pile.
Sort 4. Finally, the neither/nor pile was ranked choosing the most ideal 10 out of the remaining cards ranked as 6, followed by 5 then 4. Mothers were given a £10 voucher as a thank you for participating and a debriefing letter signposting to relevant support services.
Data processing and analysis
Missing data
Missed questions on the TOPSE questionnaire (n = 2) were omitted from the overall percentage score. A question missed on the PAI-BOR (n = 1) was replaced with the mean value for that subsection, and questions where participants (n = 7) opted for “prefer not to answer” on the ACE-IQ questionnaire were not included in total ACE scores. The two ACE scales (binary, frequency) were highly correlated, r(76) = .91, p < .001; therefore ACE-binary (i.e., number of ACEs) was used in the main analyses.
Statistical methods
IBM SPSS version 25 was used. Analyses of covariance (ANCOVA) were computed to identify group differences in each of the clinical/support variables (PAI-BOR, PHQ-9, ACE-IQ, SOS) and outcome variables (TOPSE, MBQS). As mother’s age and employment status differed between groups, these demographic characteristics were entered as covariates, with Bonferroni correction applied in post hoc multiple comparisons. To address multicollinearity between borderline severity (PAI-BOR) and depression severity (PHQ-9), r(76) = .84, p < .001, principal components analysis was used to create a composite variable of mental health symptom severity (Field, Reference Field2009; Song et al., Reference Song, Lin, Ward and Fine2013). Variables included borderline severity (PAI-BOR), depression severity (PHQ-9), number of diagnosed comorbid conditions, and difficulty in daily functioning measures (as measured on the PHQ-9). No rotation method was required as only one composite had an Eigen value > 1, The Kaiser-Meyer-Olkin measure of sampling adequacy exceeded the minimum recommended value (>.5): Kaiser-Meyer-Olkin = .69, and Bartlett’s test of sphericity was significant: χ2(6) = 167.47, p < .001. The extracted composite explained 68% of the variance, with PAI-BOR, PHQ-9, comorbidity, and functioning difficulty loading as .928, .910, .839, and .561 respectively. Standardized Cronbach’s alpha = .83.
Where significant group differences were found, hierarchical regressions were performed to explore the strength of associations among the variables (childhood adversity, mental health severity, social support, maternal knowledge). For parenting self-efficacy, childhood adversity (ACE-binary) was included at step 1 due to the temporal priority of this variable; mental health severity was added at step 2; and given the importance of a supportive social network on parenting self-efficacy and the relation between knowledge and self-efficacy, discrepancy between received and preferred support (SOS), and parenting knowledge (MBQS) were added at step 3. Approximate normality, multicollinearity, homoscedasticity, linearity, outliers, and independence of errors assumptions were met with the exception of one outlier, which was a valid response and therefore retained. Significance was set at .05.
Results
Clinical profile
For all BPD scales, BPD mothers scored significantly higher than DPN and HC mothers; DPN mothers scored significantly higher than HC mothers on all scales except self-harm/impulsivity (see Table 2). For current depression symptoms, BPD mothers had higher scores than DPN mothers who had higher scores than HC mothers. Moderate or severe depression (≥10 on PHQ-9) was reported in 88% (n = 23) of BPD mothers, 56% (n = 14) of DPN mothers, and 4% (n = 1) of HC mothers, χ2(2, N = 38) = 34.43, p = .077. No difference was found between the two clinical groups for difficulty in daily functioning score; however, BPD mothers had significantly more comorbid conditions. All effect sizes were large.
Table 2. Means, standard deviation, ANCOVA statistics, and pairwise comparisons (with Bonferroni correction applied) for BPD scores (PAI-BOR), depression scores (PHQ-9), comorbidity, childhood adversity scores (ACE-IQ), and social support (SOS) by participant group
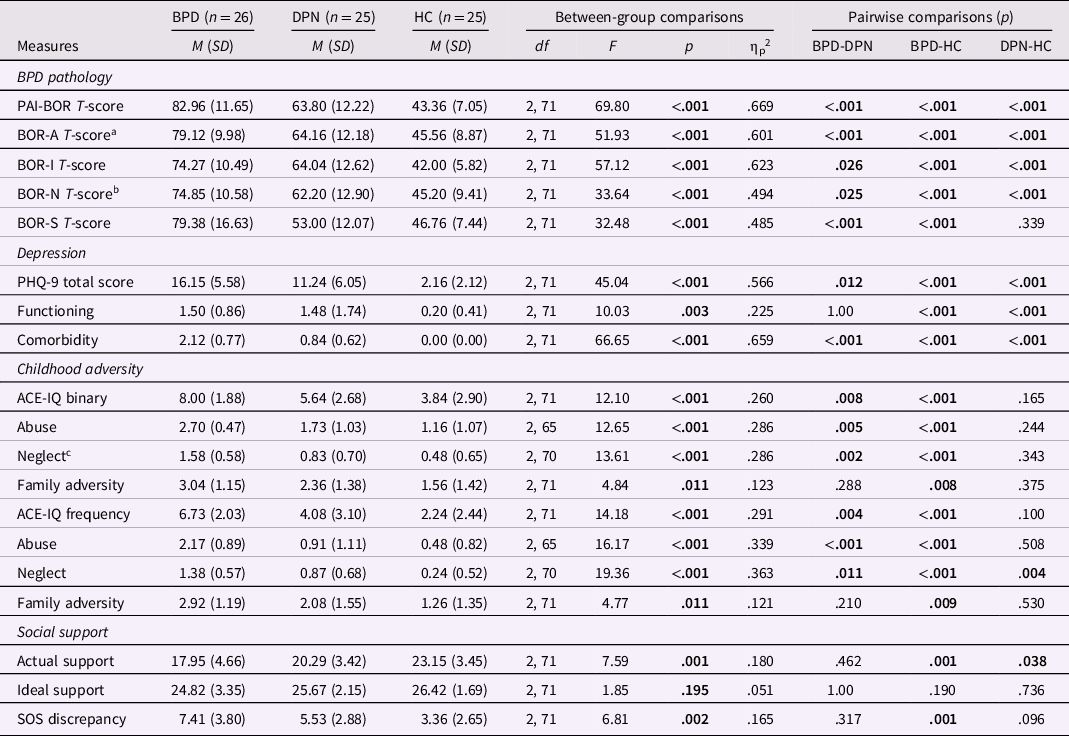
a The covariate of age of mother had a significant main effect on BOR-A T-score, F(2,71) = 5.95, p = .017, ηp 2 = .079, whereby as mother’s age increased affective instability decreased r(76) = −.40, p < .001.
b The covariate of working status had a significant main effect on BOR-N T-score, F(2,71) = 4.89, p = .030, ηp 2 = .066, whereby as working status increased (i.e., when in employment) negative relationships decreased r(76) = −.43, p < .001.
c The covariate of age of mother had a significant main effect on Neglect binary score, F(2,71) = 5.54, p = .021, ηp 2 = .075, as mothers age increased, neglect was less likely to have occurred, r(76) = −.39, p = .001.
Values in the table in bold denote those reaching statistical significance.
Childhood adversity
BPD mothers reported experiencing more abuse and neglect and experienced these adversities more frequently than DPN or HC mothers. BPD mothers self-reported more family adversity than HC mothers (see Table 2). No differences were found between DPN and HC mothers on ACE-binary scores except for neglect, where DPN mothers scored significantly higher than HC mothers. No differences were found between the BPD, DPN, and HC groups for occurrences of being bullied (42% n = 11; 28% n = 7; 16% n = 4 respectively; χ2(2, N = 76) = 4.30, p = .116). All effect sizes were large except for family adversity (moderate).
Perceived social support
ANCOVA analyses showed a difference between groups for received support with large effect sizes; both mothers with BPD and DPN received less actual support than HC mothers (Table 2). For preferred support there were no significant group differences; all mothers had similar support preferences. Significant group differences were found with SOS discrepancy (i.e., the difference between actual/received support and ideal/preferred support) again with large effects. BPD mothers had a significantly larger discrepancy than HC mothers (all other comparisons were not significant). As the discrepancy score most accurately reflects the mother’s perception of support, this variable was used in subsequent analyses.
Main results
H1: Mothers knowledge of ideal sensitive parenting
H1 was not supported as no significant differences were found between groups with the MBQS ideal sensitive mother score (see Table 3). To investigate whether there were any group differences by specific maternal behavior statements, the ten highest scoring items and the ten lowest scoring items were reported by group. Table 4 shows almost complete convergence of the most ideal and least ideal maternal behavior items chosen by the BPD, DPN, and HC mothers. All Q-sort findings indicate that BPD mothers have the same knowledge of what makes an ideal sensitive mother as DPN and HC mothers.
Table 3. Means, standard deviations, ANCOVA statistics, and pairwise comparisons (with Bonferroni correction applied) for mother’s parenting perceptions (TOPSE) and mother’s parenting knowledge (MBQS) by participant group
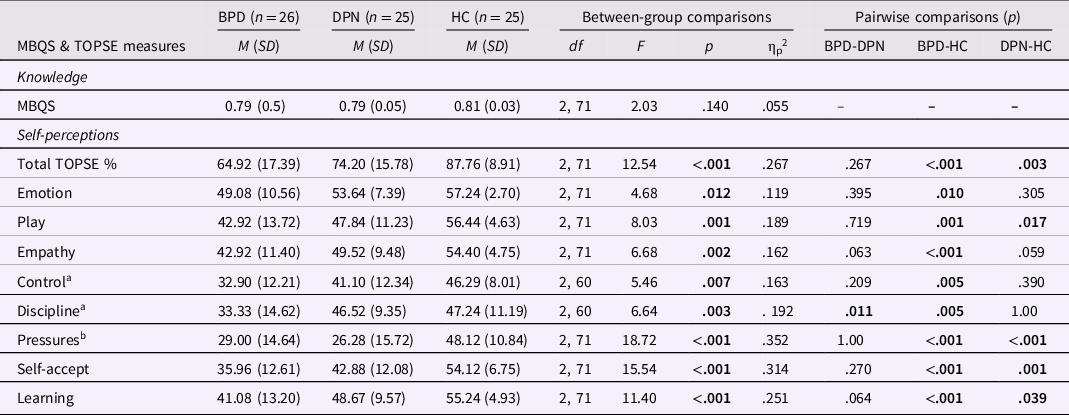
a n = 21 for BPD, DPN & HC.
b The covariate of age of mother had a significant main effect on TOPSE Pressure score, F(2,71) = 6.43, p =.013, ηp 2 = .085, whereby as mother’s age increased their ability to manage parenting pressures increased, r(76) = −.32, p = .005.
Values in the table in bold denote those reaching statistical significance.
Table 4. Highest and lowest scoring MBQS items by participant group
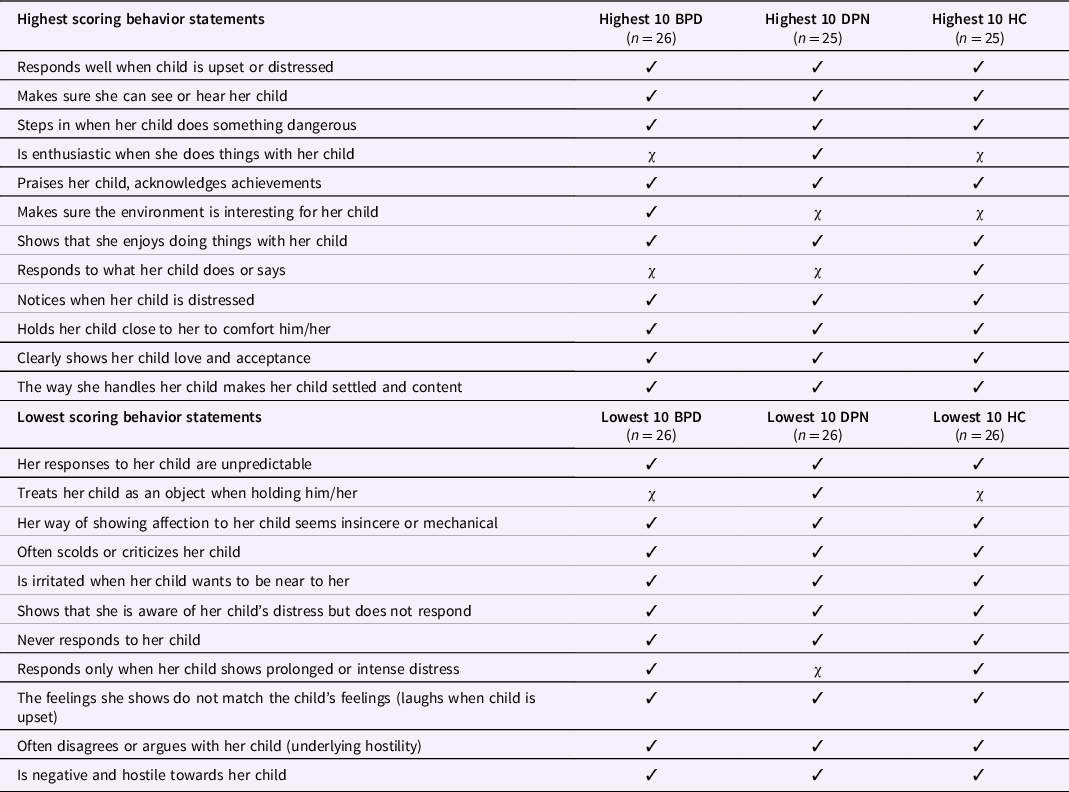
Note. Ticks represent the mother behavior statements chosen by each group.
H2: Mother’s parenting self-efficacy
H2 was supported as separate ANCOVAs revealed significant group differences for the total TOPSE% score and for each TOPSE subscale (Table 4). All yielded large effect sizes. Post hoc tests showed both mothers with BPD and DPN had overall lower parenting self-efficacy than HC mothers. Similarly, both clinical groups had lower perceived self-efficacy on the measures of Play, Parenting pressures, Self-acceptance, and Learning than HC mothers. Mothers with BPD had lower perceived self-efficacy than HC mothers for Emotion and affection, Empathy, Control, and lower self-efficacy than DPN and HC mothers for Discipline/boundary setting.
H3: Associations with maternal parenting self-efficacy
H3 was partially supported. Significant negative correlations were found between mother’s parenting self-efficacy (TOPSE%) and ACE-binary r(76) = −.29, p = .006; symptom severity r(76) = −.67, p < .001; SOS discrepancy r(76) = −.45, p < .001, and a positive correlation between parenting self-efficacy and MBQS r(76) = .24, p < .020. Step 1 of the hierarchical regression showed that childhood adversity contributed significantly to the regression model, F(1, 74) = 6.79, p = .01, f 2 = .09, accounting for 8.4% of the variance of mother’s parenting self-efficacy (Table 5). At step 2 the model was again significant, F(2, 73) = 30.14, p < .001, f 2 = .82, but with symptom severity added childhood adversity no longer significantly contributed to the model (p = .60); symptom severity accounted for 36.8% of the variance. Finally at step 3, the addition of support discrepancy resulted in a significant model, F(4, 71) = 17.74, p < .001, f 2 = 1.0, with support uniquely accounting for 3.6% of the variance. Childhood adversity and knowledge coefficients were not significant (p = .22, p = .15); symptom severity and support discrepancy were significant (p < .001, p = .04). The final model accounted for 47% of total variance, with symptom severity having the strongest effect on mother’s parenting self-efficacy (ß = −.61); three times that of perceived social support (ß = −.21).
Table 5. Hierarchical regression exploring the relative contribution of childhood adversity, symptom severity and social support in mother’s self-perceptions of parenting (TOPSE%)
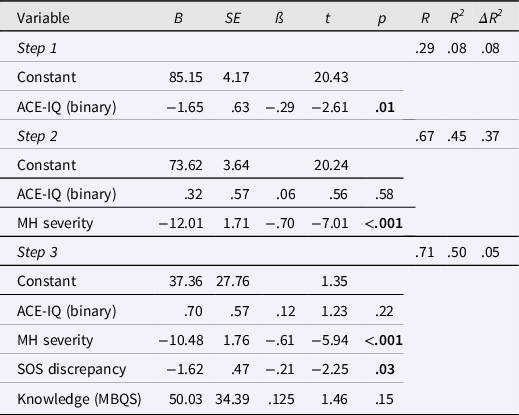
Notes. N = 76.
Values in the table in bold denote those reaching statistical significance.
Discussion
This is the first study to explore whether mothers with BPD are knowledgeable about "ideal" sensitive parenting behaviors: Do they know what sensitive parenting looks like and do they think they are parenting well? Mothers with BPD had a similar knowledge of parenting as mothers with depression and mothers with no mental health difficulties. However, both clinical groups had lower overall perceptions of their parenting efficacy than those without mental health difficulties. Mothers with BPD had experienced more childhood adversity, and the clinical groups received less support than HCs despite having similar social support preferences. The discrepancy between preferred and received support was significantly larger in mothers with BPD than healthy comparison mothers.
H1: Parenting knowledge
Contrary to our hypothesis, mothers with BPD appear to know what good parenting is, and at the same level as healthy mothers despite experiencing greater childhood adversity and presumably having had fewer opportunities to observe appropriate parenting (Pears & Capaldi, Reference Pears and Capaldi2001). Similarly, having fewer people for support and fewer with whom to discuss parenting strategies did not limit parenting knowledge in mothers with BPD, despite social parenting models suggesting that parents rely first and foremost on family and friends for support (Cochran & Niegro, Reference Cochran, Niegro and Bornstein2002). Knowledge of parenting practices are often learned from one’s own parents (Dunn et al., Reference Dunn, Cartwright-Hatton, Startup and Papamichail2020); however, such knowledge may also be gleaned from other sources such as psychiatric services and health visitors, in particular regarding infant parenting (the age of focus for the parenting knowledge Q-sort task); from other relatives, friends’ parents during childhood, and observing other mothers in the community; and from the plethora of literary, media, and online resources of parenting strategies readily accessible to help-seeking parents (e.g., Bornstein et al., Reference Bornstein, Cote, Haynes, Hahn and Park2010; Bornstein, Reference Bornstein, Bornstein, Leventhal and Lerner2015; Smith, Reference Smith2010). Further exploration of how mothers with BPD (and mothers with other psychopathology) gain parenting knowledge despite often-adverse childhood experiences and relationship difficulties (as identified in this study, and Stepp et al., Reference Stepp, Lazarus and Byrd2016), is warranted.
It could be that mothers with BPD have an abstract general understanding of parenting knowledge but perhaps are less knowledgeable about when and how to translate their knowledge into parenting practices, for example, timings of child developmental abilities (Tamis-LeMonda et al., Reference Tamis-LeMonda, Shannon and Spellmann2002), or show poor synchronicity with their child (Feldman, Reference Feldman2003). Discrepancies between cognitions and practices in parenting are well known (Bornstein, Reference Bornstein, Bornstein, Leventhal and Lerner2015). Alternatively, it could be that mothers with BPD are fully aware of how to apply this knowledge but are less able to do so due to their BPD symptomatology (e.g., emotional dysregulation, American Psychiatric Association, 2013) and/or associated difficulties (e.g., reflective functioning, Bateman & Fonagy, Reference Bateman and Fonagy2008, making it difficult to place` themselves in the child’s mind; Steele et al., Reference Steele, Townsend and Grenyer2020). How parenting knowledge is applied in actual parenting practices calls for future investigation.
H2: Parenting self-efficacy
Mothers with BPD and depression reported lower parenting self-efficacy (Elliot et al., Reference Elliot, Campbell, Hunter, Cooper, Melville, McCabe, Newman and Loughland2014; Kohlhoff & Barnett, Reference Kohlhoff and Barnett2013; Newman et al., Reference Newman, Stevenson, Bergman and Boyce2007; Steele et al., Reference Steele, Townsend and Grenyer2020) than healthy comparison mothers. Lower discipline and boundary setting (permissive parenting) was specific to BPD, consistent with previous research (Bartsch et al., Reference Bartsch, Roberts and Proeve2022; Harvey et al., Reference Harvey, Stoessel and Herbert2011). Parenting knowledge does not appear to equate to perceived parenting self-efficacy in that mothers with BPD or depression thought they were not doing well as parents, nor parenting as well as other mothers (as seen by the self-acceptance scores). Borderline personality and depression symptomatology of low sense of self and low self-esteem (APA, 2013) could color their responses. However, mothers with BPD and depression could be accurately reporting their parenting efficacy, as highlighted by maternal BPD and depression studies of observed parenting behavior (Bornstein et al., Reference Bornstein, Manian and Henry2022; Eyden et al., Reference Eyden, Winsper, Wolke, Broome and MacCallum2016; Lovejoy et al., Reference Lovejoy, Graczyk, O'Hare and Neuman2000), and may instead struggle to translate parenting knowledge into sensitive parenting behavior. For instance, poorer reflective capacity may make it difficult for mothers with BPD to understand their child’s mind and thus effectuate confident, appropriate play and/or attunement (Steele et al., Reference Steele, Townsend and Grenyer2020). As parenting self-efficacy is associated with effective parenting behavior (Vance & Brandon, Reference Vance and Brandon2017), indirectly affecting the child via parenting practices (Jones & Prinz, Reference Jones and Prinz2005; Reiner-Hess et al., Reference Reiner-Hess, Teti and Hussey-Gardner2004), these findings raise important questions of how, for example, mothers utilize parenting self-efficacy in parenting practices, which require exploration in these two clinical groups.
H3: Associations with maternal parenting self-efficacy and knowledge
Whilst a history of adverse childhood experiences can affect own parenting self-perceptions (Michl et al., Reference Michl, Handley, Rogosch, Cicchetti and Toth2015) and although childhood adversity was initially associated with lower parenting self-efficacy in the regression analyses, symptom severity was most strongly associated with mothers’ parenting self-efficacy scores over and above the contribution of childhood adversity. If childhood adversity is involved with parenting self-efficacy in any causal way, then the relation could be due to the impact of childhood adversity on mental health severity, which calls for evaluation with longitudinal data. Associations of borderline severity with depression severity, comorbidity of depression with BPD, and the inability to untangle the two make it challenging to conclude with certainty whether differences found in mothers’ parenting self-efficacy are due to borderline personality or depression symptomatology. However, it is likely that lower reported self-efficacy is linked to negative cognitive self-schemas often associated with these disorders (Baer et al., Reference Baer, Peters, Eisenlohr-Moul, Geiger and Sauer2012; Beck, Reference Beck1967). Similarly, it is not conclusive whether the results are due to depression severity or the severity of mental health more generally. However, the findings suggest that severity of mental health rather than specific diagnosis underpins the association with parenting self-efficacy given that mothers with depression also had higher borderline severity scores than healthy comparison mothers.Footnote 4 The finding regarding mental health severity is consistent with the general shift in conceptualization of mental health difficulties along dimensions of severity rather than via diagnostic categories alone (e.g., Bach & First, Reference Bach and First2018; Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014).
Regardless, implications of these findings for interventions with mothers with BPD or depression are the same: that is, to treat those with low parenting self-efficacy and implement strategies to reduce symptom severity, in particular impulsivity and emotional dysregulation. Early intervention to improve maternal parenting self-efficacy is important as mothers who consider themselves as competent parents are typically more responsive and attentive, discipline their children less, and have more realistic expectations of their children’s developmental capabilities (De Hann et al., Reference De Hann, Prinzie and Dekovic2009; Meunier et al., Reference Meunier, Roskam and Browne2011). Mother-Infant Dialectical Behavior Therapy has been associated with reported improvement in parenting confidence in mothers with BPD (Sved Williams et al., Reference Sved Williams, Osborn, Yelland and al.2021), as have recently developed parenting interventions specifically for mothers with BPD (e.g., McCarthy et al., Reference McCarthy, Jarman, Bourke and Grenyer2015; Renneberg & Rosenbach, Reference Renneberg and Rosenbach2016).
Strengths and Limitations
This study is the first to examine parenting knowledge in mothers with BPD. Comparison with healthy mothers and including a comparison clinical group of mothers with depression permitted a test of how BPD, depression, and the severity of mental health symptoms are associated with parenting self-efficacy and knowledge. Depression and symptom severity proved major predictors.
The study has some limitations as well. First, the sample is small to moderate in this acknowledged hard-to-reach population (e.g., Woodall et al., Reference Woodall, Morgan, Sloan and Howard2010), although larger than 70% of the studies that have examined parenting in mothers with borderline pathology (Eyden et al., Reference Eyden, Winsper, Wolke, Broome and MacCallum2016). However, effect sizes were typically large, indicating statistically significant and substantively meaningful findings. Furthermore, findings of p > .05 and moderate effect size showed the same patterns, whereby mothers with BPD typically had lower scores followed by mothers with depression then healthy mothers. Second, not all mothers in the depression group were currently experiencing depression symptoms due to practical and logistical difficulties between initial recruitment and assessment at time of study. Nevertheless, perceptions of parenting self-efficacy of mothers with depression were collectively lower than in healthy mothers. Third, mothers with BPD in this sample were receiving NHS care typically indicating those who have quite complex presentations relative to those who could meet diagnostic threshold in the wider population. Finally, we acknowledge that causal conclusions cannot be made from these results and the potential for bias when using self-report. However, the questionnaires used report construct validity (e.g., Bloomfield & Kendall, Reference Bloomfield and Kendall2007; Wingenfeld et al., Reference Wingenfeld, Schäfer, Terfehr, Grabski, Driessen, Grabe, Löwe and Spitzer2010), substantial effects were observed, and findings are consistent with previous studies of self-perceptions of parenting (e.g., Elliot et al., Reference Elliot, Campbell, Hunter, Cooper, Melville, McCabe, Newman and Loughland2014; Kohlhoff & Barnett, Reference Kohlhoff and Barnett2013). Furthermore, for the novel parenting knowledge finding we used a Q-sort method, which is acknowledged as an objective way to investigate more subjective issues (Robbins & Krueger, Reference Robbins and Krueger2000).
Conclusions
Mothers with BPD and depression know what good parenting is but believe they are not parenting well. The higher their mental health symptom severity, the lower their parenting self-efficacy. Parenting self-efficacy in mothers with BPD or depression may be improved by reducing mental health symptoms in individual treatment or via parenting programs that provide feedback on positive parenting and boost self-efficacy.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S095457942200147X
Acknowledgements
The authors are extremely grateful to all the families that took part in the study and the clinicians and healthcare workers who aided with introductions.
Funding statement
This study was funded by the University of Warwick, Department of Psychology and supported by the Intramural Research Program of the NIH/NICHD, USA (Z99 HD999999), and an International Research Fellowship at the Institute for Fiscal Studies, London, UK, funded by the European Research Council under the Horizon 2020 research and innovation program (grant agreement No 695300-HKADeC-ERC-2015-AdG).
Conflicts of interest
None.








