Introduction
Despite the national decline in cigarette smoking, the prevalence of current smoking among adults in Cleveland, OH approximates 35% (Prevention Research Center for Healthy Neighborhoods, 2017). Thus, increasing the rates of tobacco treatment engagement and cessation is a priority. Behavioral counseling, including face-to-face and telephone-based, is effective for tobacco cessation (Fiore et al., Reference Fiore, Jaen, Baker, Bailey, Bennett, Benowitz and Treati2008), and group-based interventions demonstrate larger effect sizes compared to other counseling formats (Fiore et al., Reference Fiore, Jaen, Baker, Bailey, Bennett, Benowitz and Treati2008; Kotsen et al., Reference Kotsen, Santorelli, Bloom, Goldstein, Ripley-Moffitt, Steinberg and Foulds2019). The underutilization of group interventions is a major barrier to population impact (Kotsen et al., Reference Kotsen, Santorelli, Bloom, Goldstein, Ripley-Moffitt, Steinberg and Foulds2019). Moreover, the successes and challenges of recruiting diverse samples of tobacco smokers into intervention research have been well-documented (Belisario, Bruggeling, Gunn, Brusamento, & Car, Reference Belisario, Bruggeling, Gunn, Brusamento and Car2012; Estreet et al., Reference Estreet, Apata, Kamangar, Schutzman, Buccheri, O'Keefe and Sheikhattari2017; King, Cao, Southard, & Matthews, Reference King, Cao, Southard and Matthews2011; Otado et al., Reference Otado, Kwagyan, Edwards, Ukaegbu, Rockcliffe and Osafo2015; Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002). The goal of this study was to examine factors associated with failure to attend treatment (i.e., ‘no-shows’) among smokers scheduled to begin a group cognitive-behavioral therapy (CBT) intervention.
Previous studies have examined factors associated with initial engagement in behavioral tobacco cessation intervention trials. Evidence suggests that younger smokers (Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002), racial/ethnic minorities (Audrain-McGovern, Halbert, Rodriguez, Epstein, & Tercyak, Reference Audrain-McGovern, Halbert, Rodriguez, Epstein and Tercyak2007), and lower socioeconomic status individuals (Benson, Stronks, Willemsen, Bogaerts, & Nierkens, Reference Benson, Stronks, Willemsen, Bogaerts and Nierkens2014; Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002) are less likely to show for tobacco treatment. Additional barriers to attendance include lack of transportation, work-schedule conflicts, and low motivation to quit (Kale, Gilbert, & Sutton, Reference Kale, Gilbert and Sutton2019; Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002). In short, the scientific literature on participant no-shows for the initial session of behavioral tobacco treatment is limited, but suggests that social determinants of health are related to engagement. Moreover, studies focused on understanding initial engagement in group interventions are even more scarce.
The current analysis stemmed from an observation that show-rates for a group-based CBT tobacco cessation intervention were lower than anticipated. In addition to sociodemographic data collected at the initial contact (i.e., study screening), we considered other possible predictors of participants being no-shows for the initial visit (and thus did not enroll in the study), such as their recruitment method and the distance from the study site. We sought to contribute to the knowledge in this domain, which has implications for recruitment strategies and study design within the field of tobacco control, and group-based psychotherapeutic interventions more broadly.
Methods
Study design
Data for this study were drawn from a quasi-experimental study comparing the effectiveness of face-to-face versus telephone-delivered CBT for tobacco cessation based on participant preferences (NCT03290430). We also sought to test individual-difference predictors of outcomes, such as readiness to quit, social support, distress, and environmental factors.
Participants and data collection
This study was approved by the Case Western Reserve University Institutional Review Board. We recruited smokers from the Cleveland Metropolitan Area via flyers distributed at health fairs, community organizations, and health clinics. Online recruitment included advertisements posted on Facebook, Craigslist, Reddit, and online community boards. Participants were also recruited through clinicaltrials.gov. Respondents provided verbal consent for study screening. Inclusion criteria were 18 years of age or older, motivated to quit smoking, smoked five or more cigarettes per day or breath carbon monoxide of at least five parts per million, English-speaking, permanent contact information. Respondents were excluded if they reported current tobacco cessation or substance dependence or treatment, serious mental illness, contraindications for nicotine replacement therapy (NRT), were pregnant, or breastfeeding. We screened 179 respondents; 20 (11.2%) were ineligible and 44 (25%) had not been scheduled for visit 1 (i.e., the initial study enrollment/orientation visit) at the time of analysis. Thus, the sample for the present study included 115 respondents who were both eligible and scheduled to begin the intervention.
Measures
Demographics and smoking history
Participants self-reported their age, sex, and race/ethnicity, cigarettes smoked per day (CPD), and contact information (telephone number(s), home address).
Distance
The distance from the participants' home addresses to the research clinic was computed in miles.
Recruitment source
As described above (see Participants and data collection section), participants indicated how they learned of the study, which was coded as online or via flyers.
Study disposition
Participants were coded as attended or not (i.e., no-shows) for visit 1.
Intervention
At visit 1, participants completed enrollment and received the study/intervention orientation. The intervention included eight sessions over 4 weeks of group-based CBT, plus eight weeks of NRT (dosing according to manufacturer recommendations). Sessions covered cognitive-behavioral cessation and relapse prevention strategies, barriers to cessation, risky situations, problem-solving, and affect management. Participants completed exercises designed to assist with cessation attempts (e.g., mental and behavioral coping skills, cognitive reframing, behavioral activation, and no-smoking behavioral contracts).
Statistical analyses
We conducted descriptive statistics (means, standard deviations, frequencies). Simple logistic regression (odds-ratios with 95% confidence intervals) tested predictors of participant ‘no-shows’ (attended versus not) for visit 1, based on data obtained at the screening. Hierarchical logistic regression tested independent predictors of participant no-shows, controlling for demographics (age, sex, and race/ethnicity) in block 1, CPD (block 2), recruitment method (block 3), and distance from the clinic (block 4). The α was set at 0.05 and data were analyzed using SPSS 26.
Results
Approximately 56% (n = 64) of eligible respondents did not attend visit 1 (i.e., they were ‘no-shows’). Fifty-six percent of respondents were recruited via flyers; 44% were recruited online. As shown in Table 1, participants were mostly female (58%), African American (61%), middle-aged (M age = 49 years; SD = 13.6), and lived 8 (SD = 7.9) miles from the study site. On average, participants smoked 16 (SD = 8.2) CPD.
Table 1. Sample characteristics (N = 115)
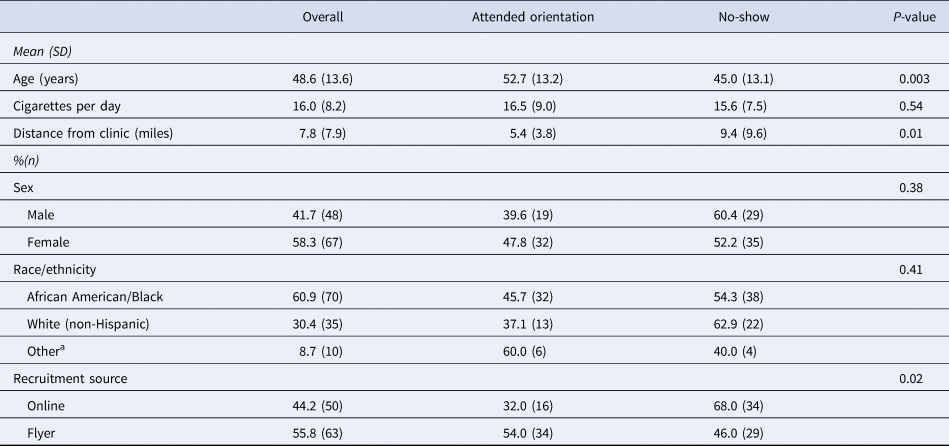
a The category ‘other’ included participants (9% of eligible sample) who identified as Hispanic/Latinx (2%; n = 2), American Indian/Native Alaskan (2%; n = 2), or identified with more than one racial group (2%; n = 2), or responded ‘other' (3%; n = 4).
Regression analyses identified characteristics related to no-shows (Table 2). Bivariate analyses indicated that age (P = 0.003), recruitment source (P = 0.02), and distance from the research clinic (P = 0.01) predicted failure to attend visit 1. Specifically, younger age respondents (M age = 45 years versus 53 years), those recruited online, and those who lived further away (M distance = 9.4 miles versus 5.9 miles) were more likely to be no-shows. In adjusted analyses, age remained a significant predictor of participant no-shows (P = 0.008).
Table 2. Logistic regression models of predictors of participant no-shows at the initial/enrollment visit (N = 115)
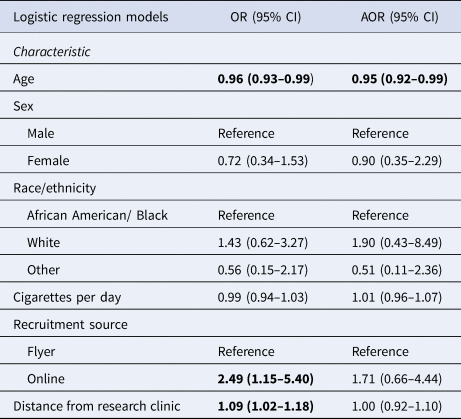
OR, odds ratio; AOR, adjusted odds ratio; CI, confidence interval.
Note: Models examined odds of participant no-shows at orientation; OR of <1.0 indicates decreased odds of no-show, OR >1.0 indicates increased odds of participant no-shows.
Bold values are statistically significant.
Discussion
Increasing our understanding of factors related to tobacco treatment engagement is important for the dissemination and uptake of evidence-based interventions. This study adds to a limited literature on initial engagement in group-based interventions, and found that demographic factors, recruitment strategy, and social determinants of health predicted the likelihood of treatment no-shows. Over 50% of scheduled respondents failed to attend the initial visit, despite proactively contacting the project and reporting high readiness to quit. Younger age, online recruitment, and distance from the research clinic predicted lower odds of visit 1 attendance. After adjustment for covariates, age independently predicted participant no-shows.
Findings are consistent with previous research. Younger age has been inversely related to attendance in both tobacco intervention studies (Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002), and in psychotherapy more generally (Fenger, Mortensen, Poulsen, & Lau, Reference Fenger, Mortensen, Poulsen and Lau2011). It is possible that younger individuals may be less motivated to quit due to the distal effects of smoking (Audrain-McGovern et al., Reference Audrain-McGovern, Halbert, Rodriguez, Epstein and Tercyak2007) or preoccupation with other obligations (Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002). Younger adults might seek alternate methods of tobacco cessation than older adults. One study found that younger adults in the UK preferred the national smoking Quitline rather than in-person treatment (Gilbert, Sutton, & Sutherland, Reference Gilbert, Sutton and Sutherland2005). A reasonable speculation is that younger individuals may also be more attracted to online services, relative to older smokers.
Recruitment source was a significant predictor of participant no-shows in the bivariate analysis, but not in the multivariable test. This finding suggests that the method of attracting potential research participants bears some relationship with engagement, and specifically, online recruitment may be a risk factor for participant no-shows. This potentially creates a challenge for researchers conducting in-person behavioral interventions, as online recruitment has high reach potential at low-cost. Pre-intervention engagement strategies may increase the likelihood of initial attendance, perhaps delivered remotely (i.e., online or via telephone), which is a direction for future research.
Bivariate analysis indicated that the distance from the study site was inversely predictive of participant no-shows for visit 1. The significance of this association was attenuated in the multivariable test, yet this represents an important signal regarding treatment engagement. The consideration of distance (miles) from the study location is novel in this context; however, other studies identified transportation as a barrier to participation in a smoking cessation trial (Woods et al., Reference Woods, Harris, Mayo, Catley, Scheibmeir and Ahluwalia2002) and that retention in tobacco treatment was greater in community versus clinic settings (Estreet et al., Reference Estreet, Apata, Kamangar, Schutzman, Buccheri, O'Keefe and Sheikhattari2017). This finding highlights the importance of meeting participants where they are, and conducting interventions in convenient, community-based locations.
In conclusion, younger smokers may be at risk for failure to attend scheduled tobacco treatment, even when they sought assistance proactively and reported readiness to quit. Online recruitment and living more than nine miles away may also contribute to participant no-shows. Future research is needed to understand the predictors of tobacco treatment engagement. This work should address the limitations of this study, by including a larger sample and an expanded screening assessment, including additional psychosocial factors and social determinants of health.
Acknowledgements
We gratefully acknowledge the Tobacco, Obesity, and Oncology Laboratory research staff for their contributions to the study.
Financial support
This work was supported by the Case Comprehensive Cancer Center.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.




