Introduction
End-of-life care is often required for people suffering with end-stage nonmalignant chronic diseases (NMCDs), such as chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), heart failure, motor neurone disease, and Parkinson's disease (Low et al., Reference Low, Pang and Chan2003; Seamark et al., Reference Seamark, Clare and Halpin2007; Jaarsma et al., Reference Jaarsma, Beattie and Ryder2009; Russon and Mooney, Reference Russon and Mooney2010). These patients tend to present challenges to end-of-life care, which was originally designed for advanced cancer patients (Luddington et al., Reference Luddington, Cox and Higginson2001). Symptom clusters of some major end-stage NMCDs are similar to those of advanced cancers (Stiel et al., Reference Stiel, Matthies and Seuß2014), with common debilitating symptoms including pain, dyspnea, fatigue, anxiety, and spiritual distress (Moens et al., Reference Moens, Higginson and Harding2014; Stiel et al., Reference Stiel, Matthies and Seuß2014; Chochinov et al., Reference Chochinov, Johnston and McClement2016). However, patients with NMCDs tend to be older, less functional, and more likely to be hospitalized toward their end-of-life period, owing to prolonged disease trajectories (Lau et al., Reference Lau, Tse and Chen2010; Ho et al., Reference Ho, Chan and Leung2013a; Bostwick et al., Reference Bostwick, Wolf and Samsa2017). Predicting end-stage for patients with NMCDs is often an inexact science complicated by the highly variable disease trajectories, comorbidities, and poor general health of the patients (Coventry et al., Reference Coventry, Grande and Richards2005; Amblàs-Novellas et al., Reference Amblàs-Novellas, Murray and Espaulella2016). Moreover, “prognostic paralysis” (Murray et al., Reference Murray, Boyd and Sheikh2005, p. 612) often leaves families unprepared for patients’ deterioration. This can also hinder communication of care needs and expectations and can inadvertently delay and compromise the quality of end-of-life care that all patients deserve (O'Leary and Tiernan, Reference O'Leary and Tiernan2008; Barclay and Maher, Reference Barclay and Maher2010).
Palliative care is a human right (Breitbart, Reference Breitbart2008). Community-based end-of-life care begins with the notion that the patient resides in a community where his/her family lives, works, and plays (Kamal et al., Reference Kamal, Currow and Ritchie2013). By “bringing care to the patient” (Berkeley Forum, 2014, p. 6), community-based end-of-life care extends supports from hospital inpatient settings into the community and the home by respecting patients’ preferences and choices regarding the place of care. Health-promoting palliative care calls for a social model that engages community resources for the prevention of distress. It fosters holistic care and dignity through coordinated community support, education, and collective action (Kellehear and O'Connor, Reference Kellehear and O'Connor2008). Brown and Walter (Reference Brown and Walter2014) commented that a social model of care mobilizes preventive and anticipatory support from families and their informal networks, and therefore neutralizes society's taboos on death and dying. Such anticipatory care and neutralization of death taboo are two important elements for honest communication of the condition of the patient, swift coordination of the needed care by capitalizing on the assets of one's social circle, and eventually preventing prognostic paralysis and its adverse consequences. Family caregivers are in the key role for detecting patients’ changes and dispensing the round-the-clock care. A well-coordinated social care program can provide “care in place” that supports the families in their natural habitat and facilitates them to utilize their community capital, and this is essential for avoiding delays in the care for the dying patient, especially those with a variable disease trajectory.
Quality of life is a key outcome for evaluating the effectiveness of end-of-life care programs (Mularski et al., Reference Mularski, Dy and Shugarman2007). The multidimensional construct is often indicated by the well-being of the physical, psychological, social, spiritual, and practical dimensions in the patients and their family caregivers (Sherman, Reference Sherman1998; Kaasa and Loge, Reference Kaasa and Loge2003). Patients and families could be supported early in their familiar community to empower them in facing an exhausting and demanding illness trajectory by disease education, self-help strategies for symptom management, family discussion on advance care planning, deployment of caregiving resources (e.g., manpower and finances), and a “hope for the best and prepare for the worst” attitude (Boland et al., Reference Boland, Martin and Wells2013; Halpin, Reference Halpin2018). Effective community support that could meet the caregiving families’ practical, emotional, and information needs can augment patient and caregiver quality of life.
In Hong Kong as of March 2019, there were 379 palliative care beds and 16 specialized palliative care teams serving a total population of about 7.4 million (Hospital Authority, 2019). Between 2001 and 2018 in Hong Kong, approximately 50% deaths were from NMCDs, while only one-third were from cancers (Centre for Health Protection, 2019). NMCD patients in Hong Kong have been found to spend up to 4.5 months of their last 6 months of life in the community (Lau et al., Reference Lau, Tse and Chen2010). The Life Rainbow Programme (LRP) offers community-based supportive care in these last months to enhance the quality of life of patients with end-stage NMCDs and their families. This program adapted the integrative body–mind–spirit (IBMS) approach (Lee et al., Reference Lee, Chan and Chan2018), which is a holistic nonpharmaceutical intervention based on the amalgamation of therapeutic wisdom and practices of Western psychotherapies and traditional Chinese philosophies (Chinese medicine, Buddhism, Daoism, and Confucianism). IBMS emphasizes (i) the interconnection between somatic, emotional, and spiritual well-being; (ii) the achievement of tranquility through normalization, acceptance, and reframing sufferings; (iii) the empowerment of oneself to transcend difficulties into opportunities for personal growth by exploring the meaning and blessing behind sufferings; and (iv) the promotion of mutual support, compassion, and gratitude. These four emphases could be particularly helpful for families facing end-stage NMCDs as they are often fighting uncertain, exhausting, and socially isolated battles on a daily basis. These emphases will build personal strengths for meeting daily practical, emotional, and information demands, and therefore augment the quality of life of the patients and their families. The approach has underpinned the development of interventions aimed at empowering families with life-limiting diseases and demonstrated to foster the quality of life among families facing lung cancer (Lau et al., Reference Lau, Chow and Ng2020; Xiu et al., Reference Xiu, Fung and Lau2020), breast cancer (Ho et al., Reference Ho, Fong and Lo2016; Liu et al., Reference Liu, Hsiung and Chang2008), colorectal cancer (Ho et al., Reference Ho, Wan and Chan2017), other cancers (Leung and Chan, Reference Leung, Chan, Christ, Messner and Behar2015), dementia (Lee et al., Reference Lee, Chan and Chan2018), and palliative care (Ho et al., Reference Ho, Leung and Tse2013b).
This paper reports on the effectiveness of the LRP, by illustrating within-group change in the quality of life over the first 3 months of joining the program, for patients and caregivers.
Methods
Design
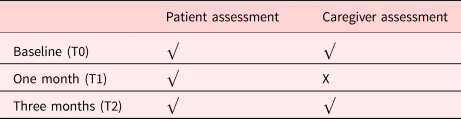
This study applied a single-group pre–post comparison, rather than a parallel comparative trial. The use of a control group is ethically controversial in end-of-life care (Evans et al., Reference Evans, Stone and Manthorpe2013). A randomized fast-track trial has been proposed to minimize the delay in treatment by offering the intervention group treatment immediately after referral, although the control group still has to wait until the intervention finishes, before receiving it (Higginson et al., Reference Higginson, Costantini and Silber2011). Such an approach incurs unnecessarily-constrained access to treatment for people who need it, simply because of methodological considerations. We reckoned this is less than ethical nor feasible for patients with unpredictable disease trajectories, such as end-stage NMCDs. Patients were assessed at the baseline (T0), 1 month- (T1), and 3 months (T2) after intake; while the caregivers were assessed at baseline (T0) and 3 months (T2) after intake (Table 1). The study received ethical approval from the Human Research Ethics Committee of the University of Hong Kong (EA1512009).
Table 1. Patient and caregiver assessments
Setting
The LRP primarily serves the Eastern District of the Hong Kong Island with a population of about 550,000.
Recruitment
Hong Kong residents aged 18 years or older with a diagnosis of end-stage NMCDs were recruited. Medical profiles of the referred patients living in their own home in the community were screened by the medical team in the participating hospital before admission to the LRP.
Patients were also screened for eligibility using a Surprise Question (“Would I be surprised if this patient died in the next six months”), which has been used as an estimate of the eligibility of end-stage patients into palliative care based on the Gold Standards Framework (2011). In addition to a negative response for the surprise question, the following criteria were used specifically for COPD and ESRD patients:
i) COPD: Stage IV (very severe) and forced expired volume in one second (FEV1) or forced vital capacity (FVC) <70%; FEV1 < 30% or FEV1 < 50% predicted plus chronic respiratory failure.
ii) ESRD: Stage V (kidney failure), glomerular filtration rate <15 ml/min/1.73 m2, accepting peritoneal analysis
The LRP also accepted cases with end-stage cardiovascular disease (e.g., heart failure and stroke) and neurodegenerative diseases (e.g., Parkinson's disease and motor-neurone disease).
Intervention
The LRP was delivered by a team of two social workers, a nurse, a program assistant, three professional volunteers (retired nurses), and 43 trained community volunteers. To recruit as many participating families as possible, the program relied on collaboration with the medical units at the participating district hospital. Thus, the hospital medical units were responsible for recruitment, screening, referral, and providing domiciliary medical support, while the LRP team provided community support to patients and families.
Importantly for its success, the LRP involved two types of collaborations:
• a multidisciplinary approach between the LRP team and the hospital medical team; and
• a transdisciplinary approach within the LRP team itself.
Choi and Pak (Reference Choi and Pak2006) distinguished multidisciplinarity from transdisciplinarity, with the former referring to a collaboration among different disciplines with knowledge staying within the disciplinary boundary, while the latter integrates knowledge of different disciplines in a manner that transcend disciplinary boundaries. The social workers, nurses, and professional volunteers on the LRP overlapped their professional boundaries by delivering an eclectic mix of symptom assessment, education, and management based on the IBMS model. The social workers served as case managers to conduct assessments, deliver non-pharmaceutical interventions, and coordinate the community resources. The community volunteers, who had received at least 20 h of training prior to engaging in the program, provided practical and emotional support to the families under close supervision by the case managers.
The active intervention was based on four dimensions (Figure 1). First, patients and caregivers were empowered to manage their symptoms and optimize functioning through holistic means. In addition to disease education, patients and caregivers were taught to record vital signs and use simple, non-pharmaceutical symptom management skills (e.g., pursed-lip breathing, postural drainage, massage, relaxation breathing, proper transfer and lifting skills, use of cold/heat pack for pain relief, simple Qigong-inspired exercises, and acupressure) to relieve their symptoms. They were also instructed to formulate and adhere to gradual but achievable personal action plans for health behaviors (e.g., “Practice three-minutes of pursed-lip breathing twice a day in the coming week” for a COPD patient). Second, along the line of psycho-social–spiritual support, patients and caregivers were taught stress management skills to relieve their emotional distress. Creative therapeutic techniques (e.g., drawing, music, photography, and pottery making) were used for life reviews and facilitate discussion of relationship reconciliation, fulfilment of unfinished businesses, and expression of gratitude and forgiveness. Third, family-oriented discussions about advance care planning fostered patients’ and caregivers’ understanding of life-sustaining treatments, clarified treatment goals and ceilings, formulated contingency plans about caregiving resources (e.g., manpower, finances, and accommodation), and prepared them for the imminent death. Lastly, the program identified practical needs of the caregiving families (e.g., home modification, financial support, respite, and assistive devices) and link them with existing informal networks and community resources.
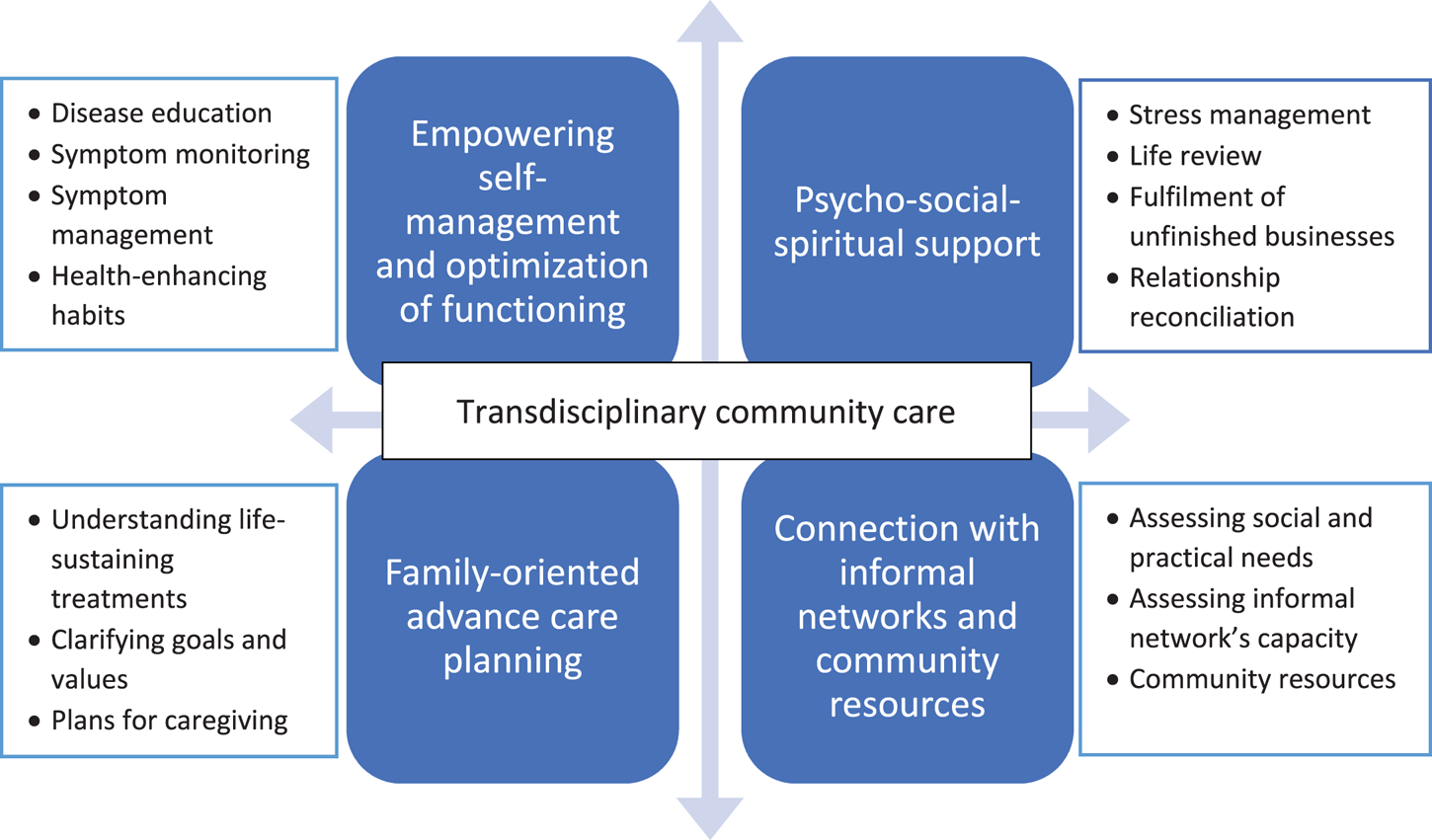
Fig. 1. Active intervention of the LRP.
Figure 2 illustrates the service pathway. After case referral and establishment of eligibility by the medical units, a comprehensive assessment was conducted by the case manager on the patients’ well-being, socio-economic circumstances, preparedness for death, and other related issues. Personalized intervention goals and service plans were established jointly with the patients and the caregiving families. These were then implemented by an average of six to eight home visits and multiple phone calls during the active intervention phase that lasted for 3–4 months. As the most intensive interventions were generally delivered during this phase, the structured evaluations were also conducted over this time period. After the intensive first 3 months, trained volunteers continued to check in with the families to provide emotional, practical, and social support through monthly phone calls. Active intervention was re-activated, if required, due to changing circumstances of patients and their families. Engagement with the families continued into the dying and bereavement phases. Case closure was decided jointly between the case manager and the surviving family members. Throughout the service journey, engagements were conducted through a combination of home visits and telephone meetings with family members who were not available during home visits or have (urgent) inquiries. If the patient was showing symptoms that could not be adequately managed in the community, the workers assisted the family to contact the corresponding hospital and facilitated the admission. All workers kept detailed records of the case notes and intervention plans. Monthly case meetings were held for discussing the progress of the cases, supervision, and mutual support.
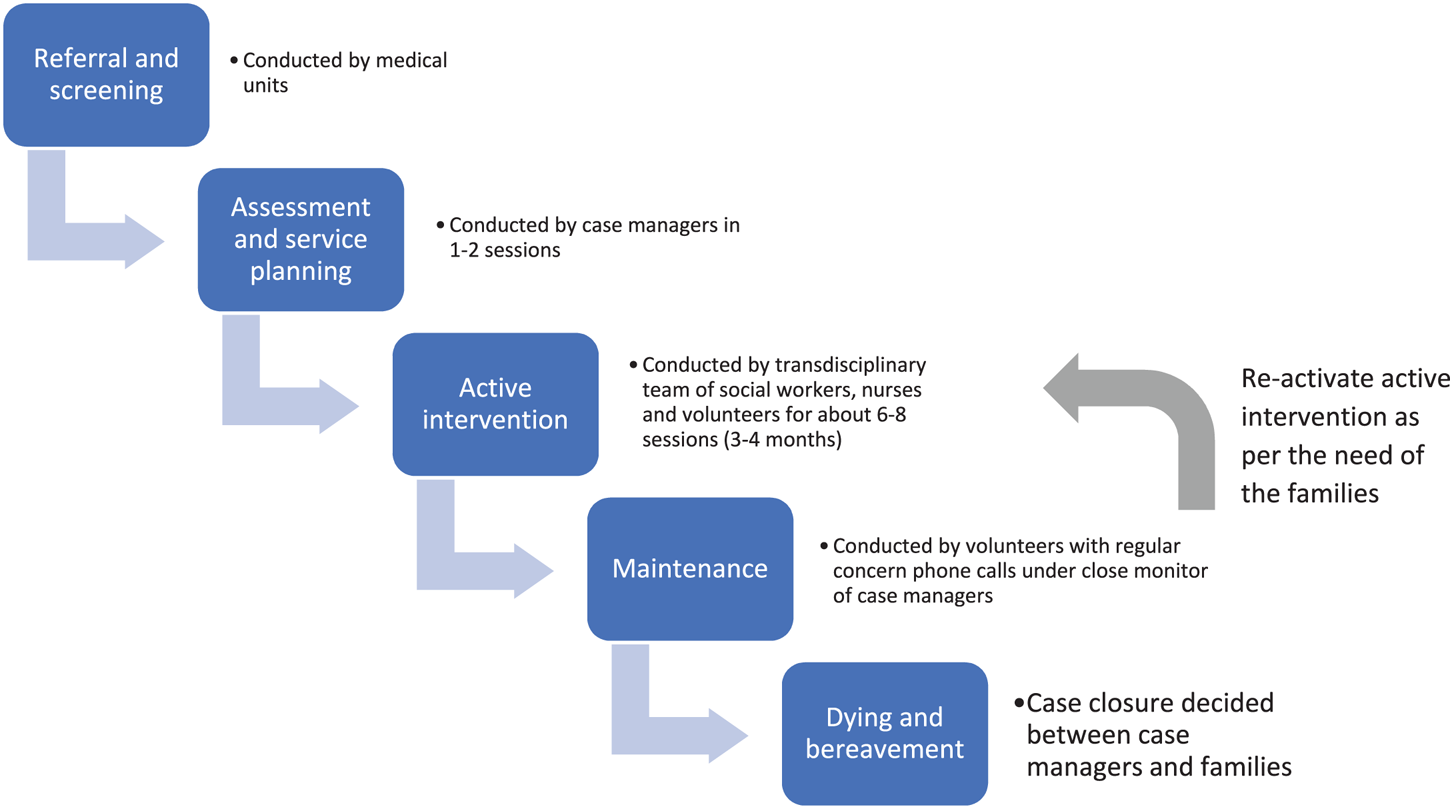
Fig. 2. Service pathway.
Outcome measures
Patient
The traditional Chinese version of the Integrated Palliative Outcome Scale (IPOS; Chan and Yu, Reference Chan, Yu, Chan, Fong, Wong, Lou and Chan2019) — staff version with a 3-day recall period was used to evaluate patient quality of life. The IPOS contains a 10-item symptom subscale (pain, shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, sore or dry mouth, drowsiness, and poor mobility) and a 7-item psychological and communication subscale (patient anxiety, family anxiety, patient depression, whether the patient has felt at peace, whether the patient could share his/her feeling with family, information, and practical needs fulfillment). Patients responded on a 5-point scale (0–4) for each item. Within this sample, the symptom subscale ranged from 0 to 40 and demonstrated adequate internal consistency (α = 0.62), while the psychological and communication subscale ranged from 0 to 28 and showed good internal consistency (α = 0.83). Higher scores refer to greater distress. Considering the previous month (at each measurement time point), patients’ presentations at accident and emergency (A&E; yes/ no), intensive care unit (ICU) admission (yes/ no), and hospital wards (number of hospital bed-days) were reported by either the caregiver or the patient.
Caregiver
The Chinese version of the Modified Caregiver Strain Index (C-M-CSI; Chan et al., Reference Chan, Chan and Suen2013) was used to evaluate caregiving strain. The Index contains 13 items (e.g., “Caregiving is inconvenience,” “My sleep is disturbed,” and “There have been family adjustments”), with each item scored on a 3-point scale [0 (No), 1 (Yes, sometimes), and 2 (Yes, on a regular basis)]. The scale scores from 0 to 26 and showed excellent internal consistency (α = 0.90) within this sample of caregivers. In addition, caregivers responded to four self-constructed single items on overall well-being [i.e., “My health is good,” “My mood is good,” “My life is good,” “My spiritual life is rich (e.g., living peacefully and meaningfully)”] using scales ranging from 1 (strongly disagree) and 10 (strongly agree).
Data analyses
All analyses were computed by SPSS 19.0. Medico-demographic characteristics, number of hospital bed-days, and over-time changes in IPOS scores were evaluated using paired-samples t-tests, comparing baseline and 1 month, and baseline and 3 months. Further investigations were made using post hoc analysis with least square difference adjustment, where there was a significant overall time effect. Over-time usage of A&E and ICU was compared using McNemar's tests. Due to the small sample size of caregivers, Wilcoxon-signed rank tests were used to compare the changes of scores on C-M-CSI and the four self-constructed items on overall well-being. Effect sizes were calculated with Cohen's d or ![]() $r = Z/\sqrt {( {{\rm number}\;{\rm of}\;{\rm observations}} ) }$ as appropriate to the data distribution.
$r = Z/\sqrt {( {{\rm number}\;{\rm of}\;{\rm observations}} ) }$ as appropriate to the data distribution.
Results
Sample
One hundred and seventy-nine eligible patients were referred to the service. Among them, 124 (69.3%) provided their consent to participate in the research and completed the T0 assessment, 95 (76.6%) completed T1, while 74 (59.7%) patients completed T2. Data from these 74 patients were included in the current analysis. Among them, 36 (48.6%) caregivers completed both baseline and follow-up assessment. Figure 3 provides the flow of cases.
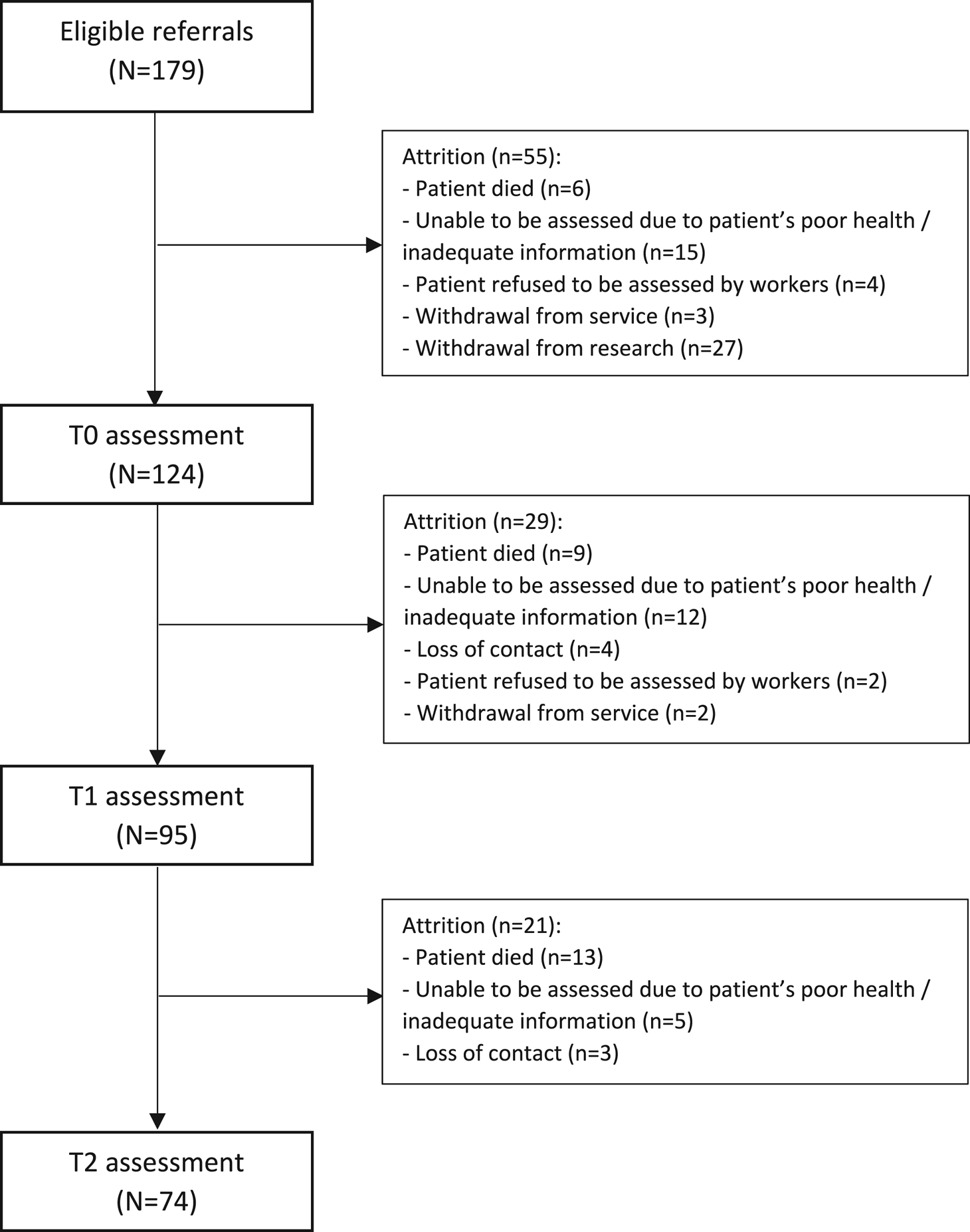
Fig. 3. Flow of cases.
Sample characteristics
Table 2 provides the medico-demographic characteristics of the sample, where 55.4%, 14.9%, 13.5%, 10.8%, and 5.5% suffered from chronic lower respiratory diseases (including COPD), Parkinson's disease, chronic renal failure, cardiovascular diseases (e.g., chronic heart failure and stroke), and neurological diseases (e.g., motor neurone disease and Huntington's disease), respectively. 66.2% patients were male and the mean age was 74.5 (±10.6). Most patients were either nonreligious (47.3%) or believing in traditional Chinese folk religions (36.5%). The majority of patients (75.7%) lived with their family members. At the baseline assessment, no patient was using palliative care services, including hospice, in-patient, and daycare, while one patient was receiving home care. As of December 31, 2018, 25 (33.8%) of the 74 patients in the program had deceased.
Table 2. Sample characteristics
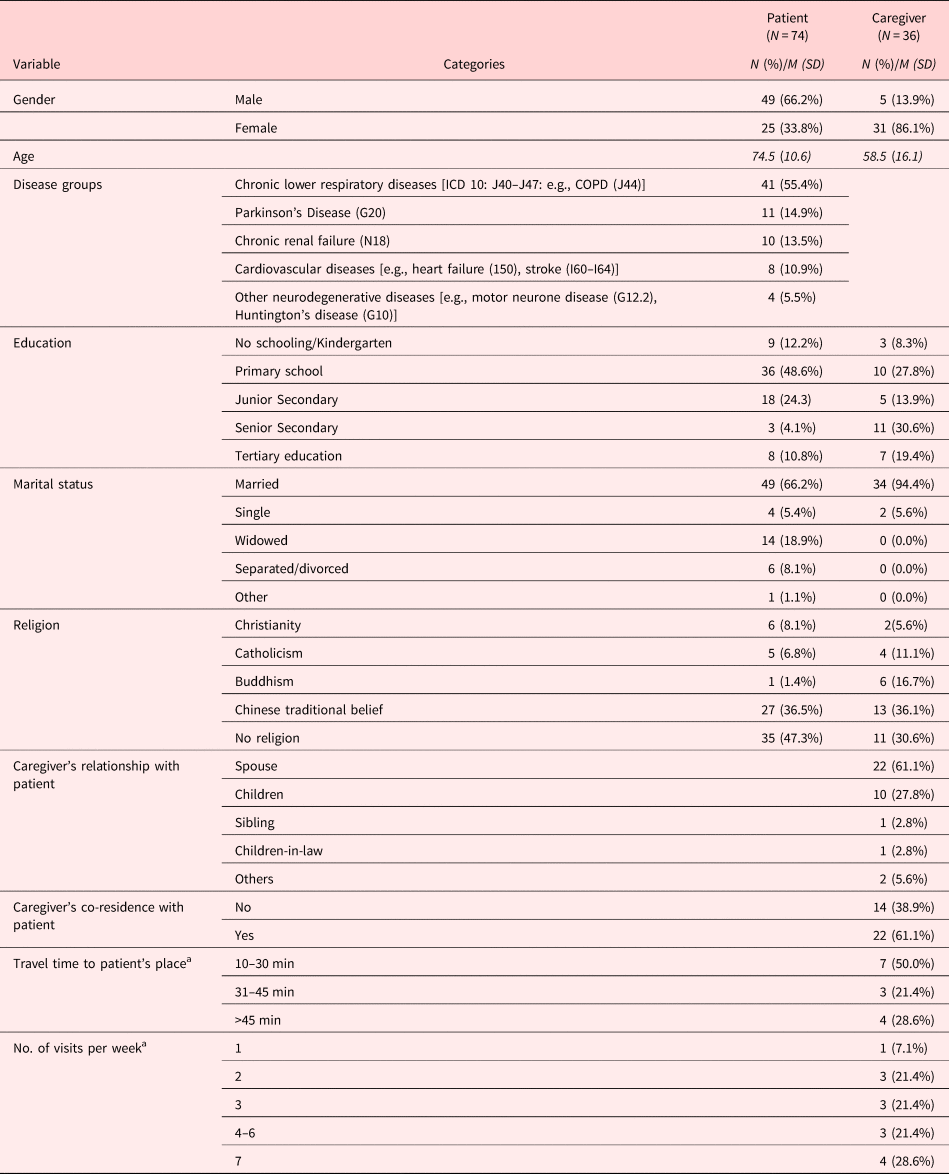
a Answered by only caregivers who were not residing with their patients.
Most of the caregivers were female (86.1%), with mean age of 58.5 (±16.1). The caregivers were either spouses (61.1%) or adult children (27.8%) of the patient. Most of them were either home-makers or retirees (63.9%), while only about one-fifth (22.2%) were still in full-time employment. Like the patients, most of the caregivers were either nonreligious (30.6%) or believed in traditional Chinese folk religion (36.1%). Most of the caregivers (61.1%) were co-residing with the patients. Among the 14 caregivers who were not co-residing with their patients, seven were living within 10–30 min from the patients, and 10 were visiting the patients three times or more per week. The majority of the caregivers (69.4%) had one or more chronic conditions, with hypertension (52.8%), diabetes (19.4%), and arthritis (19.4%) being the three most common.
Patient and caregiver outcomes
Table 3 reports the descriptive statistics and effect sizes of the patient outcomes. Omnibus time effects were significant for the symptom subscale and individual symptoms including pain, shortness of breath, weakness or lack of energy, poor appetite, drowsiness and poor mobility. Compared to baseline, a significant reduction in shortness of breath, weakness or lack of energy, poor appetite, drowsiness and poor mobility was found at one month. Pain, weakness or lack of energy, nausea at three months were also significantly lower than baseline measures. The overall symptom scores were also reduced at both paired comparisons (baseline and one month, baseline and three months). All of the significant effects were regarded as moderate to strong (Cohen, Reference Cohen1992).
Table 3. Patient outcomes (N = 74)
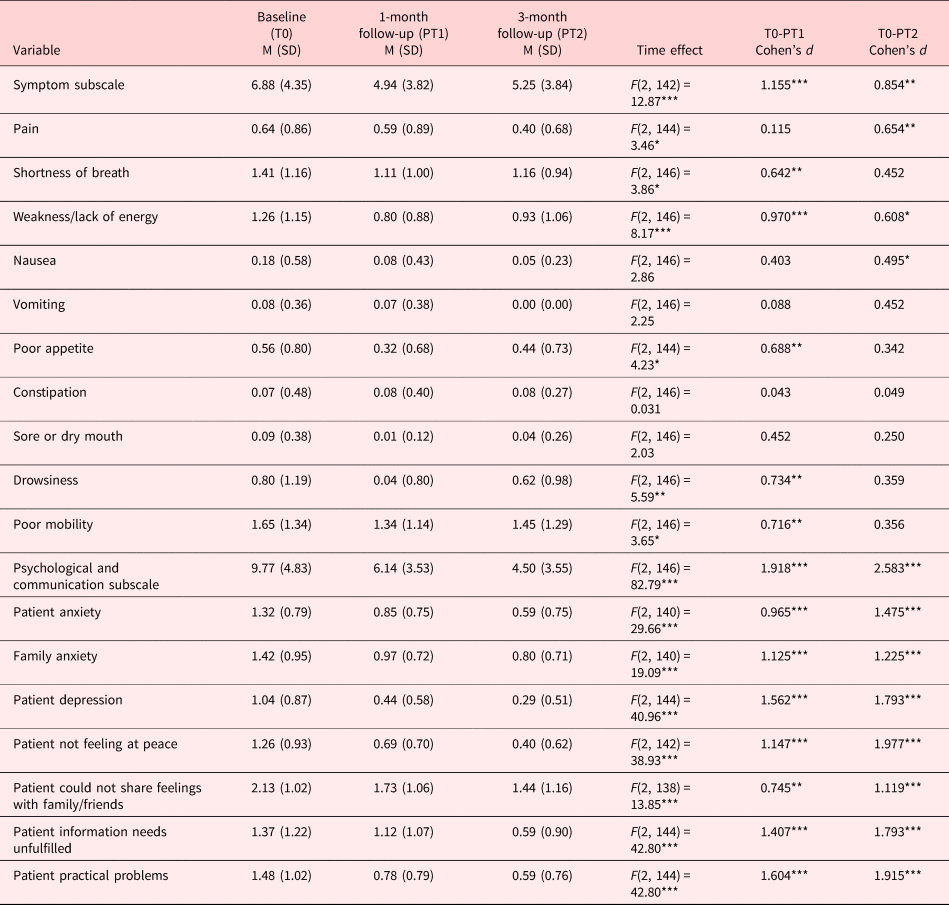
* p <0 .05.
** p <0 .01.
*** p <0 .001.
Omnibus time effects, as well as paired comparisons, were significant for the psychological and communication subscale, and all the individual items. The effects were regarded as strong by Cohen's standard (Reference Cohen1992), except the improvement reported by patients on sharing feelings with family/friends from baseline and 1 month.
At baseline (T0), five (6.8%) patients had been admitted to A&E in the previous month, while only four (5.4%) and three (4.1%) reported using A&E at 1 (T1) and 3 (T2) months, respectively. The T0–T1 and T0–T2 comparisons were nonsignificant. No patient had been admitted to the ICU in the month prior to baseline (T0), while one had been admitted during the second month (prior to T2). At T0, the average total hospital bed-days were 3.50 (SD = 6.70; median = 0; range = 0–30). At 1 and 3 months, the average total hospital bed-days fell to 1.68 (SD = 4.27; median = 0; range = 0–25) and 1.96 (SD = 4.89; median = 0; range = 0–27), respectively. The omnibus time effect and the T0–T1 comparisons were significant [time: F(2, 146) = 3.50, p = 0.033; T0–T1: F(1, 73) = 5.897, p = 0.018].
For caregivers, significant reductions were found for the C-M-CSI score and the item “My spiritual life is rich” (see Table 4). The two effects were moderate (Cohen, Reference Cohen1992).
Table 4. Caregiver outcomes (N = 36)
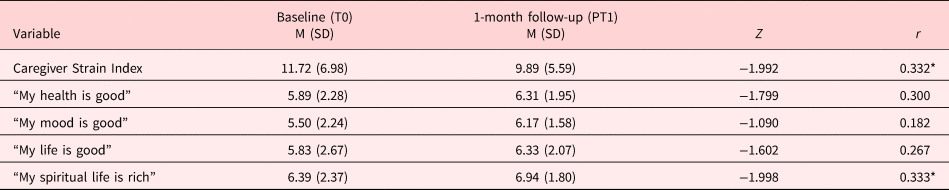
* p <0 .05.
** p < 0.01.
*** p <0 .001.
The arithmetic changes of the scores on the patient and caregiver scales across T0 and T2 were calculated, and the correlations between patients’ and caregivers’ improvement were explored. The improvement in the psychological and communication subscale of the patients was significantly related to the improvement in caregivers’ mood (r = −0.42, p = −0.012), life satisfaction (r = −0.46, p = 0.005), and spiritual well-being (r = −0.43, p = 0.009). The correlations with the changes in patients’ symptoms scales were nonsignificant.
Discussion
The LRP offers a personalized, and unique blend of holistic, nonpharmaceutical, community-based family-support interventions, underpinned by a fusion of East-West philosophies. This preliminary investigation found a significant reduction in hospital bed-days within the first month of commencing the active intervention, and a significant and ongoing improvement in well-being and quality of life for patients, over the first 3 months of the intervention. Moreover, in the same time period, caregivers reported a significant decrease in caregiving strain and improvement in spiritual well-being. The significant correlations between the changes in the patients’ and the caregivers’ outcomes highlight the interdependence of the quality of life, especially the psychological, social, and spiritual dimensions, between the two parties (Sherman, Reference Sherman1998).
The LRP was designed to operate within the complex framework of a district-level care system in Hong Kong that involves the hospitals, social care units, neighborhoods, and homes. It was aligned with the philosophy proposed by Mistry et al (Reference Mistry, Bainbridge and Bryant2015), that in addition to addressing the physical needs of the patients, the most important elements of community-based end-of-life care include addressing psychological and spiritual needs; ensuring continuous and coordinated support; honoring patients’ wishes of how, when, and where treatments should be provided; preparing for and accepting death; communication and relationship development; and supporting families. The significant decrease in hospital bed-days found in the LRP concurs with findings by other researchers. Spilsbury and Rosenwax (Reference Spilsbury and Rosenwax2017) reported that community-based end-of-life care reduced up to 9% of per-day hospital costs for noncancer patients in Western Australia, while Maetens et al. (Reference Maetens, Beernaert and De Schreye2019) reported that those who received palliative home care support had a lower risk of hospital, ICU and A&E admissions, and a higher chance of home death.
Ideally, community-based end-of-life care should be “Consistent across transitions, Prognosis-independent, and Collaborative and Coordinated” (Kamal et al., Reference Kamal, Currow and Ritchie2013, p. 259). In a study comparing the usage of home-based palliative care between cancer and noncancer patients, Kralik and Anderson (Reference Kralik and Anderson2008) found that noncancer patients tended to receive more home-based services and for a longer period of time. Moreover, reducing caregiver burdens enhances the effectiveness of home-based palliative support (Pereira-Morales et al., Reference Pereira-Morales, Valancia and Rojas2019). To provide the most benefit, this strategy should be extended beyond hospital walls into the community, where the patients spend most of their last months of life (Kamal et al., Reference Kamal, Currow and Ritchie2013). The LRP did this by establishing a two-level approach to its operations. The multidisciplinary collaboration between the hospital medical care units and the LRP ensured that the different disciplines understood and respected each other's professional expertise, and collaborated effectively to transit the patient from the hospital to the community. However, the second level of the program was its unique strength. With its transdisciplinary approach to providing humanistic care, the LRP team members (social workers, nurses, and trained volunteers) were not only trained together, but also blended their skills to deliver care that transcends traditional disciplinary boundaries. Shared activities included use of expressive arts, games, and physical exercises to improve the quality of life of the patients and the families (Wang et al., Reference Wang, Chow and Chan2017b; Nan et al., Reference Nan, Lau and Szeto2018). The transdisciplinary approach was founded on the notion that if the LRP is to empower families to care for their loved ones, then the community care team members from different disciplines should be empowered to learn these skills too.
The other important characteristic of the program was the use of social workers as case managers. Social workers can take an advantageous role in advance care planning. Wang et al. (Reference Wang, Chan and Chow2017a) found that social workers tend to readily empower families to personalize their preparation for the imminent death of their loved ones through fulfilling unfinished businesses, reconciling interpersonal conflicts, counseling, while attending to the practical needs. During the intervention, practical needs, not limited to manpower, finances or care equipment, were assessed and discussed among family members, and these were resolved through soliciting help from families’ informal networks and community resources. When these needs were articulated, debated, and then met, families were empowered with adequate knowledge and support, and they became more willing to care for their loved ones in their homes (Woodman et al. Reference Woodman, Baillie and Sivell2016). The expertise of social workers in case management and community resources also enabled them to be a plausible “one-stop shop” by connecting multidisciplinary services to the families. The IBMS (Lee et al., Reference Lee, Chan and Chan2018) approach augmented their case management efforts by providing an evidence-based, holistic, empowerment-focused conceptual framework from which to mount their intervention.
Limitations
First, the single-group pre–post design did not allow for parallel comparison with other interventions and thus precluded inference of causation. A large percentage of patients and caregivers dropped out of the study assessments soon after recruitment, although they continued to receive palliative care services from the team. Most of these patients and their families preferred receiving services relative to their particular need, instead of participating in a highly structured research project that requires them to respond to questionnaires several times. Although Bloomer et al. (Reference Bloomer, Hutchinson and Brooks2018) in a systematic review of the literature found that palliative care patients generally possessed a positive attitude toward research, their review did not address the concerns of the older, less well-educated patients with NMCDs, and their caregivers, who tend to be unfamiliar with research assessments (especially quantitative ones). We therefore suspect that our findings may have overestimated the effects of the program, as the most distressed participants may have been more likely to drop out of the study, although our post-hoc analyses showed no significant difference in all baseline outcomes and age between those who stayed (N = 79) and dropped out (N = 50) after T0, except for caregivers’ subjective evaluation of their lives (“my life is good”). An earlier referral process may have recruited participants who were less likely to be overwhelmed by their distress and who were more willing to participate in repeated structured assessments. Adapting the assessment into different modes, such as, a questionnaire that can be filled in by caregivers using their smartphones or tablets, or adroitly merging the assessment into a naturalistic conversation about the everyday lives of the participants, may help boost the completion rates. Besides, the research was undertaken in only one region of Hong Kong and recruited patients from only one hospital. This limits the generalizability of the findings. Moreover, sampling was nonrandom, resulting in an imbalanced representation of men and women, and diagnoses. This precluded robust investigation of gender and diagnostic effects. Lastly, our outcome indicators had yet to fully capture the therapeutic effects of LRP, including meaning reconstruction, reducing regrets, acceptance of death, and uptake of advance care planning and advance directives. Future studies may utilize a wider range of outcomes to comprehensively capture the efficacies of community-based programs.
Conclusions
The LRP showcased a feasible multidisciplinary collaboration between medical units and a community-based transdisciplinary team to support patients and their families facing end-stage NMCDs. Our investigation indicates support for the effectiveness of the holistic community program for patients and their family caregivers through significant improvements in the quality of life, and lower hospital stay for patients.
Acknowledgments
We are grateful to Professor Amy Chow, Director, and Miss Iris Chan, Senior Training Officer of the JCECC Project for leading the research and impact assessment team of JCECC which LRP is part of. We are grateful to the dedicated medical units of the hospital and community partners (details withdrawn for blind review). We are also indebted to the community volunteers and families who participated in the program.
Funding
The project was funded by the Jockey Club End-of-life Community Care (JCECC) Programme of the Jockey Club Charities Trust. This outcome assessment is part of the JCECC program evaluation study (HKU HREC: EA1512009).










