Mental disorders are the leading cause of disability worldwide, accounting for 23% of all non-fatal burden. Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine1 Approximately 38% of the EU population experience a mental disorder each year, Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jonsson2 causing significant societal costs, estimated at €453 billion in Europe in 2010; in the USA costs were $300 billion in 2002–2003. Reference Gustavsson, Svensson, Jacobi, Allgulander, Alonso and Beghi3,Reference Reeves, Strine, Pratt, Thompson, Ahluwalia and Dhingra4 Mental disorders are treatable and potentially preventable. Reference Barrera, Torres and Munoz5–Reference Waddell, Hua, Garland, Peters and McEwan7 However, help-seeking is often delayed or completely absent. Reference Wang, Angermeyer, Borges, Bruffaerts, Tat Chiu and de Girolamo8 The low treatment rate further aggravates burden and costs, Reference Campion, Bhui and Bhugra9 as untreated individuals are more likely to experience problematic interpersonal and family functioning and have lower life expectancies. Reference Bhatia and Bhatia10–Reference Rugulies13 Prevention of mental disorders through early intervention and the encouragement of help-seeking are major challenges for public health. 14,15 However, several factors influence help-seeking for mental health problems. Desire to handle the problem on one's own, low perceived need, low mental health literacy and financial factors are associated with a reduction in help-seeking. Reference Adler, Britt, Riviere, Kim and Thomas16–Reference Mojtabai, Olfson, Sampson, Jin, Druss and Wang20 Negative and stigmatising attitudes towards mental illness, and towards help-seeking and people with mental illness, further referred to as stigma, are other important barriers to help-seeking. Reference Clement, Schauman, Graham, Maggioni, Evans-Lacko and Bezborodovs21–Reference Thornicroft27
Commonly, four stigma types that influence help-seeking can be distinguished: perceived public stigma (PublicS), personal stigma (PersonS), self-stigma (SelfS) and attitudes towards help-seeking (HelpA). PublicS and PersonS are two types of public stigma (also referred to as social or enacted stigma), defined as the stigmatising perception about a person who has a mental illness endorsed collectively by members of the general population. Reference Corrigan22,Reference Rusch, Corrigan, Knifton and Quinn28–Reference Vogel, Wade and Haake31 More specifically, PublicS is understood to be the individual's perception of public stigma, Reference Corrigan22 as measured by Link's Perceived Devaluation Discrimination Scale; Reference Link32 PersonS, on the other hand, describes personal attitudes towards members of a stigmatised group, Reference Corrigan, Kerr and Knudsen29,Reference Eisenberg, Downs, Golberstein and Zivin33–Reference Schomerus, Matschinger and Angermeyer37 and can find a behavioural expression in the desire for social distance. Reference Angermeyer, Holzinger, Carta and Schomerus38 When these two types of public stigma were compared, endorsement of PublicS was substantially higher than PersonS. Reference Eisenberg, Downs, Golberstein and Zivin33 SelfS (also called internalised or anticipated stigma) occurs when an individual affected by a mental illness endorses stereotypes about mental illness, anticipates social rejection, considers stereotypes to be self-relevant and believes himself or herself to be a devalued member of society. Reference Rusch, Corrigan, Knifton and Quinn28–Reference Link, Yang, Phelan and Collins30,Reference Corrigan and Watson39–Reference Ritsher and Phelan42 HelpA includes the perception of a need for help, stigma tolerance associated with seeking such services, openness regarding one's problems and confidence that the help will be of assistance. Reference Fischer and Turner43 Overall, stigma is a multifaceted concept and has, therefore, been measured with a variety of instruments. Reference Rusch, Corrigan, Knifton and Quinn28,Reference Stevelink, Wu, Voorend and van Brakel44
Recent reviews of the influence of mental health-related stigma on help-seeking have reported that stigma, in particular SelfS and HelpA, had negative effects on help-seeking. Reference Clement, Schauman, Graham, Maggioni, Evans-Lacko and Bezborodovs21–Reference Thornicroft27 Many of these studies did not distinguish between intended or recommended and active help-seeking, thereby referring to the Theory of Planned Behaviour, Reference Ajzen45 which proposes that intentions correlate strongly with behaviour. Reference McEachan, Conner, Taylor and Lawton46 In practice, however, although most people would recommend seeking professional help for mental problems, Reference Holzinger, Matschinger and Angermeyer47 or report an intention to seek help when affected by mental problems themselves, Reference Lally, O'Conghaile, Quigley, Bainbridge and McDonald48 a considerably lower proportion actually sought it. Reference Wang, Angermeyer, Borges, Bruffaerts, Tat Chiu and de Girolamo8 Stigma might be one reason for not putting help-seeking intentions into action. However, only active help-seeking will reduce the burden of the disorder. We conducted, for the first time, a systematic review and meta-analysis to estimate the association of the four types of stigma with active help-seeking in the general population. Additionally, we estimated the role of potential moderating study characteristics such as sample source or response rate.
Method
Our systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see online supplement DS1). Reference Liberati, Altman, Tetzlaff, Mulrow, Gotzsche and Ioannidis49 Inclusion and exclusion criteria were specified and documented in advance by F.S.L. and N.S. (see online supplement DS2). We included only studies with general population rather than clinical samples to reduce potential selection bias towards active help-seeking. Quantitative, cross-sectional or longitudinal surveys examining the impact of at least one of the four stigma types on actual help-seeking were eligible. We searched three electronic databases (PubMed, PsycINFO and EMBASE) with no language restriction. The last search was carried out on 10 July 2015. Potentially relevant studies published in peer-reviewed journals since 1990 were identified using keywords (adapted to the respective database) related to mental disorder AND stigma AND help-seeking (see online supplement DS3 for full search strategies and details of keywords). We also scrutinised the reference lists of relevant papers, Reference Clement, Schauman, Graham, Maggioni, Evans-Lacko and Bezborodovs21–Reference Thornicroft27 and contacted expert researchers for potential additional studies.
Study selection and data extraction
We screened the titles and abstracts of all studies that met the search criteria and then consulted the full text to determine eligibility. We revised the data extraction sheet during the extraction process until it was applicable to all studies. Authors N.S. and N.G. extracted data independently, with potential disagreements resolved by discussion with F.S.L.. Authors of eligible studies were contacted for additional information or missing data, if necessary. We extracted the following information:
-
(a) publication details: author, year of publication, location and time of survey, setting and design;
-
(b) source of study population: general population sample (GPS) or subgroups of GPS such as students or military personnel (further referred to as selective GPS samples), total number of survey participants, number of participants used in analyses, random selection and representativeness;
-
(c) stigma measure: scale/items, reliability of scale and classification into one of the five stigma types – four specific stigmas, and ‘general stigma’ (GenS) for studies that did not survey a distinct stigma but combined more than one type into a single variable;
-
(e) help-seeking time-frame: help-seeking within the past 12 months v. lifetime help-seeking;
-
(e) statistical method;
-
(f) results: effect size of association with corresponding confidence interval or coefficient of association with corresponding standard error and covariates.
If a study reported more than one stigma type, we extracted all of them. We used estimates from the fully adjusted models. We recorded the direction of the stigma measure (e.g. higher scores indicate more stigma) and its range, as well as the direction of the association. Finally, we rated the quality of reporting according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement, Reference Von Elm, Altman, Egger, Pocock, Gotzsche and Vandenbroucke50 with a higher number of reported items representing a higher quality score.
Statistical analysis
The odds ratio (OR) for stigma effect on help-seeking was the main outcome. We calculated ORs and 95% confidence intervals if only regression coefficients and standard errors (s.e.) were provided. We combined ORs in random effect meta-analyses. We conducted separate meta-analyses for each stigma measure to detect their independent effect on help-seeking. ORs of studies reporting lower levels of stigma increasing (rather than higher levels of stigma decreasing) the odds of help-seeking were inversed. Reference Osborne and Osborne51 Heterogeneity was assessed using the I 2 statistic; this provides information about the percentage of total variation across individual studies that cannot be explained by chance. Reference Higgins, Thompson, Deeks and Altman52 Values range from 0% to 100%, with higher values showing an increase in heterogeneity: 25%, 50% and 75% have been commonly used to represent low, moderate and high heterogeneity, respectively. Reference Higgins, Thompson, Deeks and Altman52 We additionally examined the heterogeneity using τ2 statistics. Unlike I 2, τ2 is not affected by the number of participants included in the meta-analysis. Reference Rucker, Schwarzer, Carpenter and Schumacher53 Its values range from 0 to infinity, with higher values indicating higher heterogeneity. Values of 0.04, 0.16 and 0.36 have been commonly used to represent low, moderate and high heterogeneity, respectively. Reference Da Costa and Juni54 We assessed bias of small study effects with funnel plots and Egger's test. Reference Sterne and Egger55 Subgroup analyses were pre-specified to investigate whether effects of stigma on help-seeking depended on specific study characteristics. We stratified analyses according to study population (GPS v. selective GPS sample), time of help-seeking (within the past 12 months v. lifetime), survey period (before 2006 v. 2006 and after), response rate (<70% v. ⩾70%), quality of reporting (higher v. lower quality based on the median STROBE checklist score, with studies scoring 25 or above deemed higher quality) and setting (questionnaire v. interview). We defined two stratifications post hoc according to healthcare systems – private (USA) v. state-involved (other countries) – and study design (cross-sectional v. prospective). Stratification was only conducted if more than one study per group was found. All statistical analyses were done in Stata version 14 (Stata Corporation, College Station, Texas, USA).
Results
We identified 7968 papers in the initial search of databases and the reference lists of previous reviews (Fig. 1). Reference Clement, Schauman, Graham, Maggioni, Evans-Lacko and Bezborodovs21–Reference Thornicroft27 After removing 1163 duplicates we screened the titles and abstracts of 6805 potentially eligible studies. We assessed the full text of 201 articles. We contacted authors of nine studies for additional data, five of whom responded and their findings were thus included. One of the studies with missing data provided data for only one stigma type, Reference Blais, Tsai, Southwick and Pietrzak56 and was therefore only partially included. Two were excluded owing to missing data. One study used robust standard errors (RSE), did not report CIs, and the authors were not able to provide parametric standard errors or confidence intervals. This study was excluded because the calculation of confidence intervals from RSEs leads to different results from those when standard errors are used. One study reported a lower CI limit equal to the estimate; Reference Green, Hunt and Stain64 we assumed it to be a rounding problem and with lack of an author response used data ‘as is’. A final total of 27 studies were included in the meta-analyses. Reference Adler, Britt, Riviere, Kim and Thomas16,Reference Eisenberg, Downs, Golberstein and Zivin33,Reference Blais, Tsai, Southwick and Pietrzak56–Reference Vogt, Fox and Di Leone80
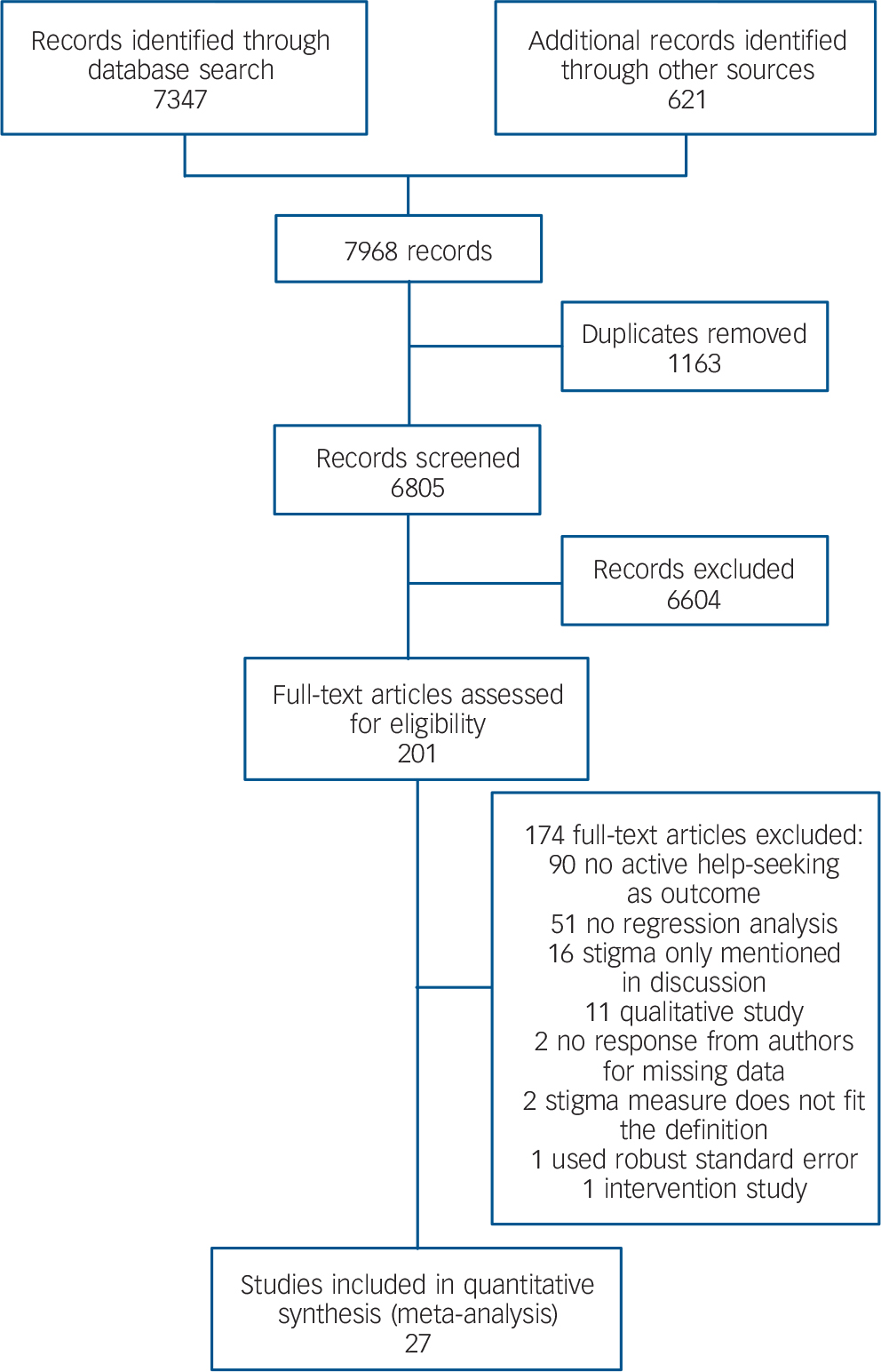
Fig. 1 PRISMA flowchart of selection of eligible studies, with reasons for full-text exclusion.
General study characteristics
Altogether, the 27 studies included 31 677 participants aged 15 years or older. They included GPS (13 studies) or subsamples of non-clinical GPS (14 studies). Four studies used a prospective design. All studies but one, from Singapore, Reference Nyunt, Chiam, Kua and Ng75 were conducted in Western societies (Europe, Australia or USA). Included studies investigated at least one of the four types of stigma, but varied greatly in their assessment (online supplement DS4). Thirteen assessed PublicS, with six of them using the Perceived Devaluation Discrimination (D-D) Scale, Reference Link32 or its adaptation. Reference Spiegelhalter, Abrams and Myles81 Of the six studies that investigated PersonS, two used a social distance scale and two employed an adaptation of the D-D scale (‘most people’ replaced with ‘I’). Three of the five studies investigating SelfS used a single-item assessment. Four of the 13 studies investigating HelpA used Fischer's Attitudes Towards Seeking Professional Psychological Help scale, Reference Fischer and Turner43 and two used a single item scale. Seven studies used a non-specific general stigma measure (see online Table DS1). All studies reported help-seeking from a formal, professional source such as a psychiatrist, psychotherapist or general practitioner. Only one study also investigated informal, lay sources of help, such as family or a priest. To improve the homogeneity of our outcome measure we only extracted data for formal, professional sources. Twenty studies reported recent help-seeking (within the past 12 months), seven reported lifetime help-seeking and one study reported both. Reference Green, Hunt and Stain64 From the latter we extracted only data for lifetime help-seeking.
Influence of stigma type on help-seeking
Figure 2 shows the results of the five random effect meta-analyses for each of the stigma types, as well as general stigma. Negative HelpA (OR = 0.80, 95% CI 0.73–0.88) and higher PersonS (OR = 0.82, 95% CI 0.69–0.98) were associated with less active help-seeking for mental health problems. Higher SelfS (OR = 0.88, 95% CI 0.76–1.03) showed an indication of less active help-seeking, but the results were not statistically significant. PublicS (OR = 0.97, 95% CI 0.93–1.02) and the unspecific GenS (OR = 0.98, 95% CI 0.84–1.15) were not associated with active help-seeking. There was substantial between-study heterogeneity in each of the meta-analyses, with I 2 ranging from 58% for PublicS to 91% for PersonS. Between-study variance τ2, by contrast, was low to moderate, Reference Spiegelhalter, Abrams and Myles81,Reference Sarikaya, da Costa, Baumgartner, Duclos, Touze and de Bray82 ranging from 0.003 for PublicS to 0.044 for PersonS. Only HelpA showed evidence of small-study bias (Egger's test, P<0.01; all other stigma measures P>0.294; see online figure DS1 for funnel plots and P values).
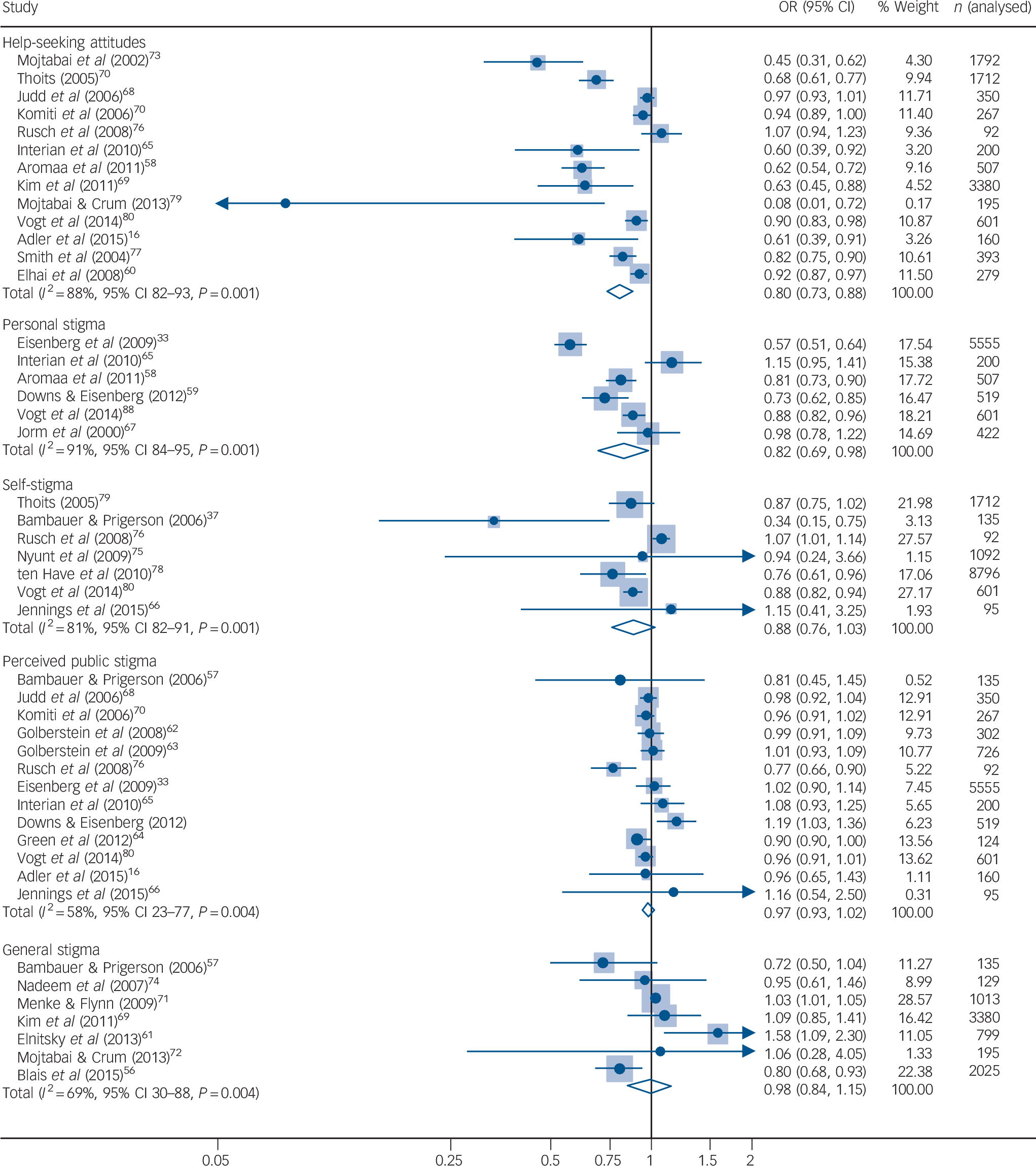
Fig. 2 Forest plot of the results of meta-analyses of five stigma types on active help-seeking.
Odds ratios (OR) and 95% confidence intervals (CI) of individuals studies and pooled estimates of separate random effects meta-analyses. OR<1 indicates negative associations between stigma or attitudes and help-seeking, i.e. higher levels of stigma are associated iwth less help-seeking. Estimates of between-study variance: τ2 = 0.018 for HelpA, τ2 = 0.044 for PersonS and τ2 = 0.023 for GenS. The study by ten Have et al (2010) estimated relative risk ratio; OR estimate was not reported and not available from study authors.
Subgroup analyses
The stratified meta-analyses for the most part did not demonstrate any major influence of study characteristics (Fig. 3; online supplement DS5). Associations between HelpA and help-seeking were weakly influenced by type of study population, time of help-seeking, setting, response rate, design and quality of reporting. We found stronger negative associations in surveys with random v. selective general population samples, recent v. lifetime help-seeking, personal assessments v. questionnaires, higher v. lower response rates, prospective v. cross-sectional design and lower v. higher reporting quality. Associations between SelfS and help-seeking were weakly influenced by study setting, survey period and response rate. We found stronger negative associations in surveys with personal assessments v. questionnaires, those conducted before v. after 2006, and with higher v. lower response rates. There was a small effect of year of study publication on the association between GenS and help-seeking, with older studies reporting slightly stronger effects. Associations between PersonS and help-seeking were weakly influenced by study design, with cross-sectional studies reporting negative associations whereas prospective studies did not report significant associations. Stratification by the country's type of healthcare insurance did not show any effect. Results of stratified analyses of PublicS and PersonS were robust across all the investigated strata. A decline in between-study heterogeneity was observed in some stratification analyses. None of the stratification analyses could fully explain the observed heterogeneity in all of the associations between stigma types and help-seeking.
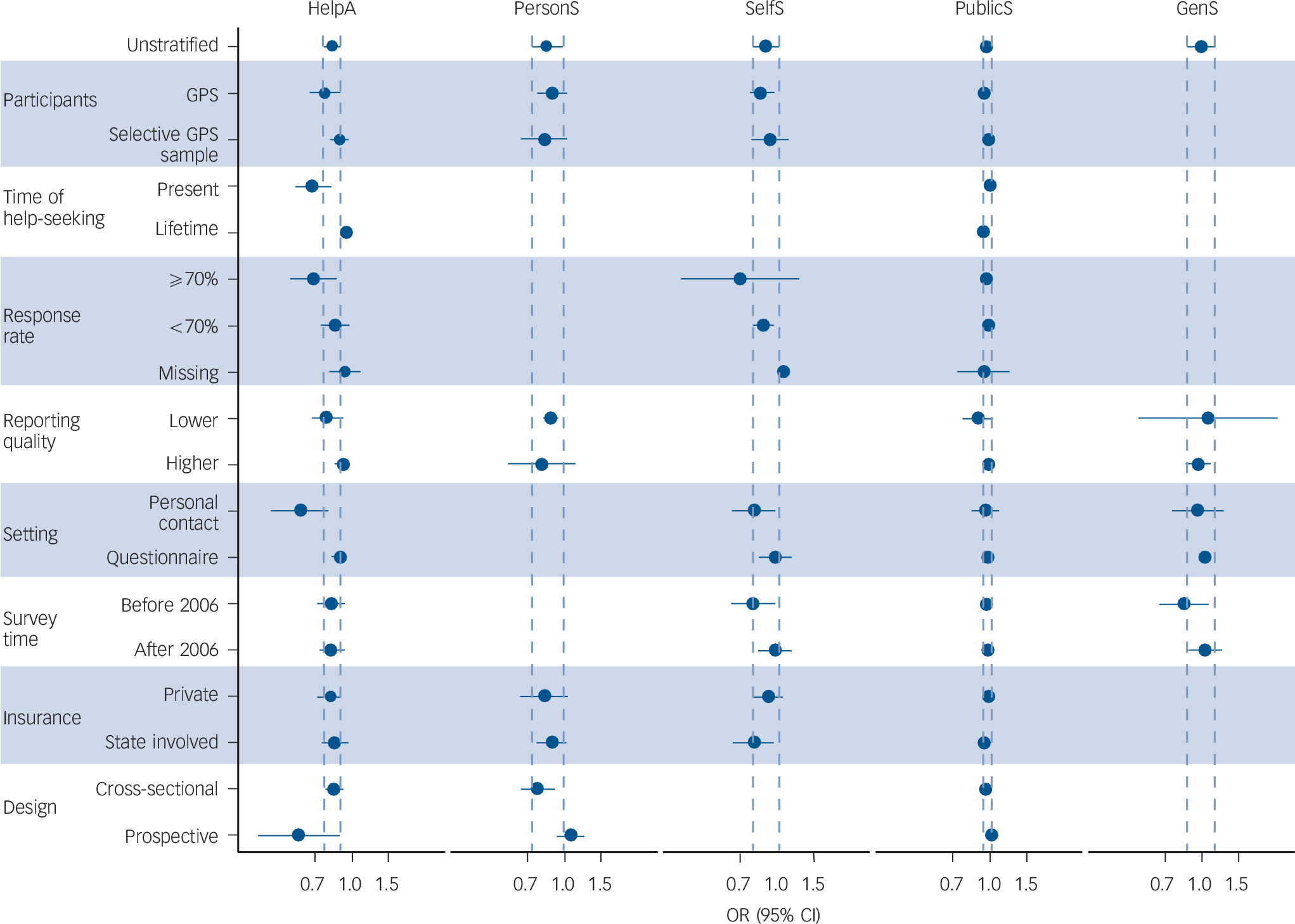
Fig. 3 Forest plot of the results of stratified meta-analyses of five stigma types on active help-seeking.
Pooled estimates (odds ratio; OR) and 95% confidence interval (CI) of each strata are reported. Dashed lines represent 95% CI of non-stratified analyses (top row). GenS, general stigma; HelpA, help-seeking attitude; PersonS, personal stigma; PublicS, perceived public stigma; SelfS, self-stigma. OR<1 indicates negative associations between stigma or attitudes and help-seeking, i.e. higher levels of stigma are associated with less help-seeking.
Discussion
Our results confirm the notion that stigma related to mental illness or mental health services is directly associated with less active help-seeking for mental problems in the general population. The strength of association depends on the type of stigma, rather than being the case for stigma in general. We found associations between less active help-seeking and participants' levels of HelpA and PersonS. SelfS showed insignificant associations. PublicS and unspecific GenS showed no association. These findings are in line with social psychological studies demonstrating that attitudes towards a behaviour are associated with engaging in the behaviour itself in other situations. Reference Ajzen and Fishbein84 Persons with pronounced PersonS might try to avoid contact with the stigmatised group, Reference Allport85–Reference Voci87 and therefore refrain from help-seeking. PublicS and SelfS failed to show significant associations, but both pointed to the expected direction of more stigma predicting less active help-seeking. The majority of studies surveying SelfS used a single item asking about a person's embarrassment when thinking about help-seeking for his or her mental health problems. Even though embarrassment/shame seems to be a barrier to help-seeking intentions, Reference Rusch, Muller, Ajdadic-Gross, Rodgers, Corrigan and Rossler88 it is unclear whether this facet of SelfS can fully capture this stigma type. Reference Omori, Mori and White89 Although a recent systematic review found a small association between SelfS and help-seeking (intentions/recommendations and active), Reference Clement, Schauman, Graham, Maggioni, Evans-Lacko and Bezborodovs21 the influence of SelfS on active help-seeking in the general population needs further exploration. To assess stigma related to mental illness and its impact on help-seeking, future studies using GenS might also consider assessing one of the more specific stigma types.
Although the four stigma types revealed independent effects on help-seeking, they are interrelated. Reference Jennings, Cheung, Britt, Goguen, Jeffirs and Peasley66,Reference Corrigan90–Reference Coppens, Van Audenhove, Scheerder, Arensman, Coffey and Costa94 Self-stigma seems to arise from an individual's own attitudes towards people with mental illness, as well as from (perceived) public stigma. Reference Jennings, Cheung, Britt, Goguen, Jeffirs and Peasley66,Reference Omori, Mori and White89–Reference Link and Phelan91 Perceived public stigma, personal stigma and self-stigma seem to predict attitudes towards help-seeking. Reference Jennings, Cheung, Britt, Goguen, Jeffirs and Peasley66,Reference Corrigan, Bink, Schmidt, Jones and Rusch92–Reference Vogel, Wade and Haake95 Furthermore, studies have suggested that stigma is associated with a low perceived need for help, Reference Jennings, Cheung, Britt, Goguen, Jeffirs and Peasley66,Reference Preville, Mechakra, Vasiliadis, Quesnel, Gontijo-Guerra and Lamoureux-Lamarche96,Reference Kanehara, Umeda and Kawakami97 and a strong desire to handle the problem on one's own. Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi and Borges98 These two factors were proposed as important barriers in considering delayed or no help-seeking. Reference Kanehara, Umeda and Kawakami97,Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi and Borges98 Future studies might consider them as additional moderators of active help-seeking and in interaction with stigmatising attitudes. Reference Jennings, Cheung, Britt, Goguen, Jeffirs and Peasley66 It is crucial to understand the complexity of various types of stigma, their role in help-seeking for mental health problems, and their direct impact on mental problems such as suicidality, Reference Oexle, Rusch, Viering, Wyss, Seifritz and Xu99 in order to develop efficient public campaigns promoting help-seeking.
Several anti-stigma and information campaigns aiming to improve people's knowledge about mental illness (mental health literacy) and to reduce stigma associated with mental illness have been conducted in recent years. Reference Mehta, Clement, Marcus, Stona, Bezborodovs and Evans-Lacko100 Whereas knowledge about the causes and treatment of mental illness seemed to improve over time and after campaigns, Reference Thornicroft, Wyllie, Thornicroft and Mehta101–Reference Yap, Reavley, Mackinnon and Jorm104 reducing negative attitudes has proved to be more difficult. Reference Angermeyer, Matschinger and Schomerus102 Only 7% of the world population reported a belief that mental illness can be overcome, Reference Seeman, Tang, Brown and Ing105 and those most reluctant to seek help perceived the lowest benefits in engaging in this behaviour. Reference O'Connor, Martin, Weeks and Ong106 To promote help-seeking, findings from these meta-analyses suggest that campaigns should address negative personal attitudes by strengthening beliefs in the treatability of mental illness. Advanced, biologically oriented mental health literacy, Reference Schomerus, Schwahn, Holzinger, Corrigan, Grabe and Carta107 and activation of fear due to media reports, Reference Niederkrotenthaler, Reidenberg, Till and Gould108 can increase the desire for social distance towards people with mental illness. Therefore, the content of campaigns should be chosen thoughtfully to avoid unintended effects. Reference Corrigan109
Future studies
Subgroup analyses suggested that associations between stigma and help-seeking can depend on certain study characteristics, in particular response rate and assessment setting. Higher response rates were generally associated with stronger negative effects of stigma. As higher response rates can reduce a potential non-responder bias, Reference Asch, Jedrziewski and Christakis110 they lead to more reliable results. Reference Baruch and Holtom111 Consequently, reporting of response rates is crucial for assessing the validity and reliability of research findings, Reference Baruch and Holtom111 which should be considered in future surveys. With regard to differences in setting, face-to-face assessments were associated with stronger negative effects than were self-reports by questionnaire. Since the expression of stigmatising attitudes towards people with mental illness or towards mental health services might be affected by social desirability bias, Reference Krumpal112 this is a surprising finding. Social desirability should have a greater role in personal contact. Surveys investigating social taboos (such as stigmatising attitudes) showed increased levels of response accuracy when data were assessed using self-administration (such as questionnaires), compared with interviewer administration. Reference Krumpal112 Questionnaires might therefore be more suitable when researching stigma. In our analyses three out of four studies with personal assessment reported high response rates; Reference Mojtabai and Crum72,Reference Mojtabai, Olfson and Mechanic73,Reference Thoits79 the fourth did not report a response rate. Reference Interian, Ang, Gara, Link, Rodriguez and Vega65 Four studies using questionnaires reported low rates, Reference Aromaa, Tolvanen, Tuulari and Wahlbeck58,Reference Jorm, Medway, Christensen, Korten, Jacomb and Rodgers67,Reference Smith, McGovern and Peck77,Reference Vogt, Fox and Di Leone80 two reported none, Reference Elhai, Schweinle and Anderson60,Reference Rusch, Kanter, Manos and Weeks76 and only three reported high response rates. Reference Adler, Britt, Riviere, Kim and Thomas16,Reference Kim, Britt, Klocko, Riviere and Adler69,Reference Komiti, Judd and Jackson70 Inspection of single study effects indicates that across these questionnaire studies, those with high response rates reported a stronger negative association. Sampling bias associated with lower response rates might therefore have a more crucial role in detecting associations between stigma and active help-seeking than the mode of assessment.
The association between HelpA and help-seeking was stronger when recent rather than lifetime help-seeking was considered. Furthermore, the association between HelpA and help-seeking was stronger in prospective studies, whereas the association between PersonS and help-seeking disappeared in prospective studies. These results indicate the importance of a timely association between current attitudes and active help-seeking. Past help-seeking might shape a person's attitude towards help-seeking. For future help-seeking, only attitudes towards help-seeking but not personal attitudes towards people with a mental illness seem to be obstructive. More prospective studies of stigma and help-seeking are needed to disentangle this interplay and to overcome the problem of reciprocal or reversed causation in cross-sectional studies.
Strengths and limitations
This is the first meta-analysis to extricate the influence of types of stigma on active help-seeking, focusing on the general population (the main target group of efforts to increase help-seeking) and considering study characteristics as potential moderators. However, our study has some limitations. We could have missed relevant studies owing to publication bias, although only HelpA showed some evidence of possible small-study bias. Several characteristics of the studies could have contributed to observed heterogeneity between them: studies used a large variety of stigma measures, differing in reliability and number of response categories. There was little information on exact operationalisation of stigma measures in the analyses; even if the number of categories was reported, it was often not specified whether stigma measures were used as dichotomous, categorical or continuous predictors, whether a cut-off for continuous measures was applied or whether the number of categories was collapsed. Future studies should report not only which stigma measure was used but also how it was handled during the analyses, all of which can affect the association with outcomes. Most studies adjusted for age and gender but differed greatly in their remaining adjustments. Future studies should adjust for variables such as mental health literacy, Reference Gulliver, Griffiths and Christensen19 perceived need, Reference Vogel, Wade and Haake95 or desire to handle the problem on one's own, Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi and Borges98 which seem to influence mental health help-seeking. We would encourage additional reporting of unadjusted associations in future studies to allow better comparison and research synthesis. All studies were conducted in high-income, mostly Western countries. The results of these meta-analyses may not generalise to non-Western or low-income countries. Despite these limitations, our results reinforce efforts to challenge mental health-related stigma as a major goal for global mental health. Reference Collins, Patel, Joestl, March, Insel and Daar113 Its reduction might facilitate help-seeking by those affected by mental illness.
Future research
The results confirmed the negative association between stigma and active help-seeking, underscoring the important differential role of stigma types, with a minor role of perceived public attitudes compared with the individual's own attitudes. Furthermore, sensitivity analyses highlighted the importance of a sufficiently high response rate, as well as the control of potential reciprocal causation, and point towards a smaller social desirability bias in interview studies than is commonly assumed. Future studies on the effect of stigma on help-seeking for mental problems in the general population should use questionnaires that differentially assess stigma types, employ a prospective design, take care to monitor and increase response rates, and assess potential confounders, such as an independent low perceived need for help or a strong desire to handle problems on one's own. Reference Jennings, Cheung, Britt, Goguen, Jeffirs and Peasley66,Reference Vogel, Wade and Haake95–Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi and Borges98 Well-designed general population studies are needed to develop and optimise campaigns promoting mental health by facilitating early help-seeking and fighting mental illness stigma.
Acknowledgements
The authors gratefully acknowledge the help of the following researchers in providing additional data and studies, as well as for support in statistical questions: (in alphabetical order) S. M. Alang, M. C. Angermeyer, P. Bebbington, T. Becker, R. K. Blais, H. L. Cheng, T. C. Cheng, R. Dempster, J. D. Elhai, F. A. Gary, P. Held, K. S. Jennings, A. F. Jorm, A. Komiti, M. Koschorke, K. D. Locke, C. Michel, R. Mojtabai, A. Moser, M. O'Connor, D. Rabiner, S. G. Riedel-Heller, W. Rössler, N. Rüsch, N. Sartorius, S. J. Schmidt, G. Schomerus, M. ten Have, P. A. Thoits, G. Thornicroft, D. S. Vogt and M. Zwahlen.






eLetters
No eLetters have been published for this article.