The rates of multiple pregnancies in developed countries continue to rise as a consequence of the increasing use of assisted reproductive technology (ART) and advanced maternal age (Black & Bhattacharya, Reference Black and Bhattacharya2010; Collins, Reference Collins2007), and currently account for 3% of live births in England and Wales (National Institute for Health and Clinical Excellence (NICE), Reference Karkhanis, Sturgiss, Brandon, Glinianaia and Bell2011). Multiple pregnancies remain a high-risk group with a much greater risk of adverse pregnancy outcomes and childhood disability than singletons, thereby posing significant challenges to midwives, obstetricians, and pediatricians.
The Regional Maternity Survey Office (RMSO) established a prospective population-based multiple pregnancy register (MPR) in the North of England (counties of Northumberland, Tyne and Wear, Durham, Teesside, and North Cumbria) in 1998, relaunched as the Northern Survey of Twin and Multiple Pregnancy (NorSTAMP) in 2007. The principal aims of this survey were to identify all multiple pregnancies, at the point of diagnosis, among women attending maternity units in the North of England, to ascertain their outcome, to determine the changes in the epidemiology of multiple pregnancy over time, and to develop a core dataset for future studies in twin research (Glinianaia et al., Reference Glinianaia, Rankin, Wright, Sturgiss and Renwick2002). An earlier update of the development of the NorSTAMP was published in 2006, describing the introduction of obtaining explicit consent from parents for their data to be held on the register and summarizing the main findings of the first 5 years of data collection (Ward Platt et al., Reference Ward Platt, Glinianaia, Rankin, Wright and Renwick2006).
This paper describes recent developments to the NorSTAMP and presents mortality outcomes for the first 10 years of data collection (1998–2007).
Methods
The NorSTAMP captures data on all multiple pregnancies in the North of England (UK), which has a population of around 3 million and 31,000 deliveries per year. The NorSTAMP ascertains multiple pregnancies from the earliest antenatal scan at which a multiple pregnancy is determined (recommended at 10–13 weeks in the UK; National Institute for Health and Clinical Excellence (NICE), 2008), and then successively at the time of the 20-week routine ultrasound anomaly scan and at delivery. Multiple pregnancy may also be identified following miscarriage, or by the discovery of the remains of a second fetus at the time of an apparently singleton birth. Initial ascertainment is provided on a notification card that gives basic identifying information and, where possible, the ultrasound assessment of chorionicity. Full data are then obtained following birth by completion of a data registration form at the delivery hospital (Glinianaia et al., Reference Glinianaia, Rankin, Wright, Sturgiss and Renwick2002).
The records are maintained and held at the RMSO on a single database linked through the mother's details to the Perinatal Morbidity and Mortality Survey (PMMS; Hey et al., Reference Hey, Welch, Lawson, Barron, Bullough, Morris and McNay1984), the Northern Congenital Abnormality Survey (NorCAS; Richmond & Atkins, Reference Richmond and Atkins2005), the Northern Diabetes in Pregnancy Survey (NorDIP; Bell et al., Reference Bell, Glinianaia, Tennant, Bilous and Rankin2012), and the North of England Collaborative Cerebral Palsy Survey (NECCPS; Glinianaia et al., Reference Glinianaia, Rankin and Colver2011b). Beaumont Colson Ltd, database designers, developed the RMSO database using Bespoke software. The external linkage with the Office for National Statistics (ONS) birth and death tapes was also built into the database automatically to allow cross-validation. This system provides data on various maternal demographic and clinical characteristics, prevalence of multiple pregnancy as well as pregnancy outcome, such as early fetal loss, selective feticide, stillbirth (fetal loss at ≥24 weeks of gestation), infant deaths, and any major congenital anomaly (Ward Platt et al., Reference Ward Platt, Glinianaia, Rankin, Wright and Renwick2006). The final diagnosis of chorionicity for like-sex twin pregnancies is based on placental examination and histology, and when unavailable, on the appropriate first trimester ultrasound determination. Information on zygosity is not recorded. The RMSO cannot capture data on whether a pregnancy was conceived using ART owing to the restrictions imposed by the Human Fertilisation and Embryology Acts (1990, 2008).
Regional Multicentre Research Ethics Committee's approval was sought for the register at the outset. In keeping with the UK regulations and guidance at that time, particularly with regard to the Health and Social Care Act 2001 (http://www.legislation.gov.uk/ukpga/2001/15) and the Data Protection Act 1998 (http://www.legislation.gov.uk/ukpga/1998/29), a system of informed consent was introduced in 2005 for women's identifying details to be held by the register (Ward Platt et al., Reference Ward Platt, Glinianaia, Rankin, Wright and Renwick2006).
The survey was relaunched in 2007 as NorSTAMP, with a renewed focus on clinically relevant collaborative audit. All 11 maternity units within the North East and North Cumbria participated in the Steering Group and contributed data to the NorSTAMP. Regional consensus standards of care for multiple pregnancy were developed, agreed, and launched in July 2009 (available on the RMSO website at www.nepho.org.uk/rmso/surveys/multiple). Alongside these, measurable indicators of outcome and process of care were proposed. Some of these are not yet covered by the existing data collection process. Central to these standards is the concept of the development of multidisciplinary teams who will be responsible for developing protocols for the management of multiple pregnancies, and where possible, delivering care for these women within dedicated clinics and antenatal classes.
Results
The number of births in the North of England declined during 1998–2002, increasing again during 2003–2007. The twinning rate increased from 13.6 per 1,000 maternities in 1998 to 16.6 per 1,000 in 2002, declining to an average of about 15 per 1,000 maternities during 2003–2007. The numbers of triplet and higher order multiple pregnancies declined substantially (Table 1).
TABLE 1 Multiple Pregnancies, Maternities, and Twinning Rates in the North of England, 1998–2007
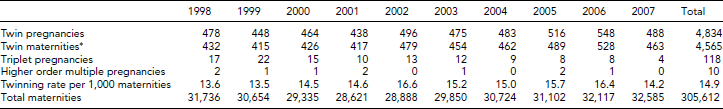
*Maternities are pregnancies with at least one live birth or stillbirth (birth of a dead fetus at 24 or more completed weeks of gestation), including maternities where there has been an early or late fetal loss (before 24 weeks of gestation); the twinning rate is defined as the number of twin maternities per 1,000 total maternities with at least one live birth or stillbirth (Glinianaia et al., Reference Glinianaia, Rankin, Wright, Sturgiss and Renwick2002).
The table shows that during 1998–2007, there were a total of 4,834 twin pregnancies (9,668 twins); 4,565 were twin maternities (pregnancies with at least one live birth or stillbirth; 9,130 twins); and the remaining 269 twin pregnancies (538 twins) were either spontaneous losses of both twins before 24 weeks gestation or terminations of pregnancy. The overall stillbirth and neonatal mortality rates in twins were 18.0 per 1,000 births and 23.0 per 1,000 live births respectively. Stillbirth and neonatal mortality rates were significantly higher in monochorionic than dichorionic twins: 44.4 versus 12.2 per 1,000 births (relative risk [RR] 3.6, 95% Confidence Intervals [CI] 2.6–5.1), and 32.4 versus 21.4 per 1,000 live births (RR 1.5, 95% CI 1.04–2.2) respectively. There was no significant improvement over time in either stillbirth or neonatal mortality rates in either group (Figure 1; see further details in Glinianaia et al., Reference Glinianaia, Obeysekera, Sturgiss and Bell2011a).

FIGURE 1 Stillbirth and neonatal mortality rates for dichorionic (DC) and monochorionic (MC) twins with 95% confidence intervals for 1998–2002 and 2003–2007.
The percentage of twin maternities with determined chorionicity fluctuated on a yearly basis: it was the lowest (86%) in 1998 and the highest (95%) in 2002. Rates were similar between quinquennia at about 90%, but have shown no improvement since 2002. Between 1998 and 2002 and between 2003 and 2007, the relative proportions of monochorionic and dichorionic twins remained the same.
Discussion
The NorSTAMP data show that in our North of England population the twinning rate has remained relatively stable for the last few years at about 15 per 1,000 maternities. Monochorionic twins have a 3.5-fold higher risk of stillbirth and a 50% higher risk of neonatal death compared with dichorionic twins, and there was no evidence of significant improvement in these outcomes between quinquennia (1998–2002 and 2003–2007).
Before the introduction of the informed consent system in 2005, we had reason to believe that our methods of ascertainment of multiple pregnancy were robust, as confirmed by annual cross-validation with the ONS data. Diagnosis of a twin pregnancy at an early ultrasound scan (about 65% twin pregnancies are diagnosed before 13 weeks of gestation) enabled us to register a twin pregnancy with an early fetal loss, which made our ascertainment more complete, as the ONS labeled such pregnancy as singleton. We acknowledge that we cannot be certain of capturing all the early twin pregnancies, some of which will later become singletons, because a first trimester ultrasound scan was not provided on a routine basis for the early years of the register and not all women book in time to undergo it. We therefore have to regard the early pregnancy twin ascertainment as a minimum estimate.
After the introduction of the explicit informed consent system, the rate of complete data reduced with considerable variation between maternity units, in particular for pregnancies with a miscarriage or single twin demise, as the survey could not retain identifying details for pregnancies that were notified without a record of maternal consent. In May 2007, the notification and consent issues were raised and discussed at a half-day regional meeting alongside the clinical issues that could be addressed using the NorSTAMP data. A suggestion by the NorSTAMP Steering Group to relaunch the register with a new clinical focus, while maintaining its epidemiological strengths to fully maximize the potential of the register, was widely supported by the local clinicians of all 11 maternity units. A number of further regional workshops took place to discuss and agree on the proposed regional standards of care for multiple pregnancy, which were finalized and launched in 2009. It was agreed to audit key clinical outcomes and benchmark against agreed standards of care. Discussion on more effective ways to improve the consent and notification rates also took place. One barrier to improving consent rates was the existing notification system, whereby multiple pregnancies were first reported to the RMSO, which prompted a consent letter to be raised and returned to the unit for completion when the woman attended for antenatal care. This was therefore simplified to a single notification and consent form, and completed at the earliest point in pregnancy. Implementation of this system resulted in substantial improvement in the proportion of pregnancies for which a record of consent was obtained.
Analysis of complete data for 1998–2005 was presented at the NorSTAMP annual workshop in 2009 to provide key benchmarks for monitoring future trends, with the ultimate goal to improve perinatal outcomes of twin pregnancies, which were demonstrated to be still much higher compared to singletons (Regional Maternity Survey Office, 2011). It was also shown that chorionicity was a major determinant of twin perinatal outcomes, with monochorionic twins being at a higher risk of both stillbirth and neonatal mortality than dichorionic twins. The importance of improving care for this high-risk group of pregnancies has been recognized by the UK National Institute for Health and Clinical Excellence (NICE) (www.nice.org.uk) resulting in the development of clinical guidance for the care of multiple pregnancies (National Institute for Health and Clinical Excellence (NICE), 2011). Experts from the North of England contributed to the development of this national guidance. It is reassuring that our regional guidance is consistent with the NICE principles. For example, in accordance with our regional standards, it has been emphasized in the NICE guidance that clinical care for women with multiple pregnancies should be provided by a nominated multidisciplinary team, consisting of a core team of named specialist obstetricians, specialist midwives, and ultrasonographers, all of whom have experience and knowledge of managing multiple pregnancies. Progress toward this goal has been monitored by regular surveys of participating units. While challenges remain, many units have made significant progress in developing multidisciplinary teams with nominated specialists.
As far as we are aware, the NorSTAMP remains the only UK register of multiple pregnancy with ascertainment from the first ultrasound scan, chorionicity information, and with a direct link to regional registers of congenital anomaly, pregnancy loss and infant mortality, and cerebral palsy, and also to the national birth data. A number of studies using this rich source of linked data have been published recently (Glinianaia et al., Reference Glinianaia, Obeysekera, Sturgiss and Bell2011a, Reference Glinianaia, Rankin and Wright2008; Karkhanis et al., 2011; Pharoah et al., Reference Pharoah, Glinianaia and Rankin2009; Ray & Ward Platt, Reference Ray and Ward Platt2009; Webster et al., Reference Webster, Glinianaia, Loughney and Bell2011). However, our current inability to identify those pregnancies conceived using ART remains a significant limitation.
The ability to capture data on multiple pregnancies from very early in pregnancy makes the NorSTAMP a unique resource for perinatal epidemiology research and provides the basis for aetiological and long-term follow-up studies. The NorSTAMP, based on a well-developed regional clinical network and supported by collaborative clinical audit, provides rich data on multiple pregnancy, which is crucial for improving the quality of care and birth outcomes in multiple pregnancy. The continuance and further development of the NorSTAMP should be seen as a public health priority and a key component of the drive to improve maternal and child health.
Acknowledgments
We are grateful to all the district conveners and coordinators in the North of England for their continued collaboration and support of the NorSTAMP, PMMS, NorCAS, and NorDIP.




