Psychiatric intensive care units (PICUs) are designed to treat in-patients who display seriously disturbed behaviour and who cannot be safely treated in an open acute psychiatric ward. 1 The units generally admit detained patients whose behaviour is judged to present a significant risk to others, Reference Pereira, Dawson and Sarsam2,Reference Brown, Chhina and Dye3 and sometimes use potentially risky interventions such as rapid intramuscular (IM) tranquillisation and high-dose medication in order to maintain a safe environment. Reference Abdelmawla and Mitchell4 A number of protocols guide the management of seriously violent behaviour. The most widely used UK guidelines are probably those produced by the National Institute for Health and Clinical Excellence (NICE) and the Maudsley Hospital. 5,Reference Taylor, Paton and Kerwin6
The high-risk nature of some PICU activity means that it is important that individual units have effective procedures for clinical governance and monitoring treatment. However, there is little published data on clinical activity in PICUs and minimal reference data against which units can measure their own activity. Surveys of PICU policies and practice leave doubts about whether answers to hypothetical questions reflect actual practice. Reference Pereira, Dawson and Sarsam2,Reference Pereira, Paton, Walkert, Shaw, Gray and Wildgust7 Prescribing patterns on individual PICUs Reference Goldney, Bowes, Spence, Czechowicz and Hurley8-Reference Brown and Bass11 may not generalise to other units. The limited evidence suggests that the prescribing practices of different PICUs are converging Reference Macpherson, Dix and Morgan12 but it is difficult to judge the appropriateness of individual practices without reference data from representative units. This paper aims to provide such reference data by describing the drug treatments given to 332 patients consecutively admitted to seven English PICUs.
Method
Anonymised data were collected prospectively on 332 patients admitted consecutively to seven English PICUs between February 2006 and August 2007. Details of the units, patients and data collection procedure are described by Brown et al. Reference Brown, Chhina and Dye3 Data on class of medication administered, route of administration and total dose were collected by staff working on the units and recorded on a semi-structured collection sheet, developed by a steering group of representatives from each participating unit and piloted on one of the units. All numbers refer to drugs recorded on the patient's drug chart as having been administered. Mental state was measured at admission and at 2 weeks, using the extended version of the Brief Psychiatric Rating Scale (BPRS). Reference Lukoff, Nuechterlein and Ventura13
The research and development coordinator at the lead site advised that the project represented service evaluation rather than research and hence did not require research ethical committee approval. The study protocol was approved by appropriate local audit committees.
Statistics
Statistical analysis was undertaken using SPSS version 14.0 for Windows. Groups were compared using t-tests for normally distributed continuous data andz non-parametric tests for categorical and skewed continuous data. Preselected variables (age, gender, ethnicity, recent behaviour, behaviour in the PICU, BPRS scores) were tested for association with the use of particular interventions, in univariate logistic regression analysis. Variables which were significant at 5% level were then entered into a multiple logistic regression model by forward stepwise procedure.
Results
Data were collected on 332 consecutive admissions to seven different PICUs (referred to here as units A-G) between 1 February 2006 and 30 September 2007. There were 258 (78%) males and 72 (22%) females in the sample: 241 (73%) White and 83 (27%) from Black and minority ethnic groups. The major diagnostic groups were schizophrenia/schizoaffective disorder (n = 179, 54%), mania (n = 64, 19%) and substance misuse (n = 26, 8%). The mean length of PICU stay was 35 days (median = 18, range 1-315). Further details of patient characteristics and behaviour are given by Brown et al. Reference Brown, Chhina and Dye3
Three data-sets were missed in patients with brief PICU stays and one unit (D) failed to record BPRS scores on 29 patients. A few other items were missed from individual patient records. Most of the data analysis was of 329 data-sets; percentages are of the total number of results for each variable.
Medication
The proportion of patients who received particular types of psychotropic drugs is shown in Table 1. During their PICU stay, 97% of patients received at least one psychotropic drug. Most received more than one drug (mean 3.5, median 3, range 0-11, ANOVA between units: d.f. = 321, F = 11.2, P<0.001), a mean of 2.4 regular and 1.4 as needed (PRN) prescriptions. The number of drugs administered correlated with length of stay (correlation coefficient = 0.511, d.f. = 322, P<0.001). The most common combination was regular administration of an atypical antipsychotic drug and PRN administration of a typical antipsychotic drug and a benzodiazepine (usually haloperidol and lorazepam).
Table 1 Drug treatments prescribed to 332 patients consecutively admitted to seven English psychiatric intensive care units
| Variation between different unitsa | ||||
|---|---|---|---|---|
| Treatment | Number of patients, n (%) | Range, % | χ2 | P |
| IM rapid tranquilisation | 71 (22) | 6–48 | 30.4 | <0.001 |
| IM zuclopenthixol acetate (acuphase) | 56 (17) | 2–46 | 66.3 | <0.001 |
| No rapid IM medication | 225 (68) | 50–84 | 29.7 | <0.001 |
| IM depot antipsychotic | 102 (31) | 10–60 | 43.8 | <0.001 |
| No IM medication | 165 (50) | 28–80 | 38.6 | <0.001 |
| Regular antipsychotic medication | 282 (86) | 72–94 | 12.5 | 0.05 |
| PRN antipsychotic medication only | 16 (5) | 0–8 | 4.5 | 0.6 |
| No antipsychotic medication | 31 (10) | 2–22 | 15.2 | 0.02 |
| No psychotropic drugs | 10 (3) | 0–8 | 7.7 | 0.26 |
| Oral typical antipsychotic | 146 (44) | 24–54 | 34.0 | <0.001 |
| Oral atypical antipsychotic | 235 (71) | 46–84 | 12.9 | 0.04 |
| Oral benzodiazepine | 261 (79) | 60–97 | 28.7 | <0.001 |
| Antidepressant | 47 (14) | 2–28 | 16.9 | 0.009 |
| Mood stabiliser | 94 (29) | 6–44 | 22.4 | <0.001 |
| Aggregate concurrent antipsychotic dose, > BNF limits | 20 (6) | 2–18 | 18.7 | 0.005 |
Rather surprisingly, 10 patients (3%) did not receive any psychotropic medication while on the PICU. These patients had significantly lower mean BPRS scores on admission (42.2 v. 58.6, t = 2.3, d.f. = 295, P<0.02) and shorter mean PICU stays (7 v. 36 days, ANOVA F = 3.7, d.f. = 320, P = 0.05). Only one had a diagnosis of a major psychotic illness. A further 21 patients (6%) received only psychotropic medication other than antipsychotic drugs.
The majority of patients (n = 298, 91%) were recorded as receiving at least one antipsychotic drug during their stay on the PICU; 134 (45%) took only oral medication, whereas 164 (55%) received at least one IM injection. Most of the patients who took antipsychotic drugs had a psychotic illness (or drug-induced psychosis), but 43 (14%) did not. Of those patients who did not have a psychotic illness, 27 (63%) received regular and 16 (37%) PRN antipsychotic drugs. Most patients received more than one antipsychotic drug (mean 1.8, median 2, range 0-6, ANOVA between units: d.f. = 321, F = 9.1, P<0.001), a mean of 1.2 antipsychotic drugs regularly and 0.6 on PRN prescription. The number of different antipsychotic drugs received correlated with length of stay (correlation coefficient = 0.52, d.f. = 322, P<0.001).
Antipsychotic drugs in combination
Seventy-two (23%) patients received more than one regular antipsychotic drug simultaneously (range 6-60%, χ2 between units = 56.6, d.f. = 6, P<0.001). The most common reasons given for this were ‘for symptomatic/behavioural control’ (n = 37, 51%), ‘cross-tapering oral medication’ (n = 14, 19%) and ‘switching from oral to depot medication’ (n = 13, 18%).
Twenty patients (6%) were recorded as receiving one or more antipsychotic drugs at an aggregate dose which exceeded current British National Formulary (BNF) limits either singly or in combination. 14 The use of doses in excess of BNF limits was predicted by damage to property in the PICU (OR = 5.89, 95% CI 1.91-18.21, d.f. = 1, P = 0.002) and by violence in the PICU (OR = 3.32, 95% CI 1.13-9.81, d.f. = 1, P = 0.03). No other variables were significant in univariate analysis.
Rapid IM tranquillisation
The study recorded 146 episodes of rapid tranquillisation by IM injection, involving 71 different patients. Such patients had significantly higher mean BPRS scores on admission (70.5 v. 54.7, t = 6.0, d.f. = 295, P<0.001) than those who were not given rapid IM tranquillisation. They received a mean of 2.1 injections (median 2.0, range 1-12). No patients were given psychotropic medication by intravenous injection during the study period.
The use of rapid IM tranquillisation was predicted by damage in PICU (OR = 3.78, 95% CI 1.79-7.96, d.f. = 1, P<0.001), male gender (OR = 3.39, 95% CI 1.24-9.29, d.f. = 1, P = 0.01) and higher admission BPRS score (OR = 1.04, 95% CI 1.02-1.05, d.f. = 1, P<0.001, a 4% increase in odds of receiving rapid tranquillisation for each point increase in BPRS score). Its use varied eightfold between the different units (Fig. 1), but this was not a significant predictor variable in the regression model. No other variables were significant in univariate analysis. Patients who were physically restrained (48/90 v. 23/232, d.f. = 1, χ2 = 71.1, P<0.001) or secluded (19/32 v. 52/238, d.f. = 1, χ2 = 28.8, P<0.001) during their PICU admission were significantly more likely to receive rapid IM tranquillisation than those who were not. The study did not examine whether guidelines on post-rapid tranquillisation patient monitoring were observed.
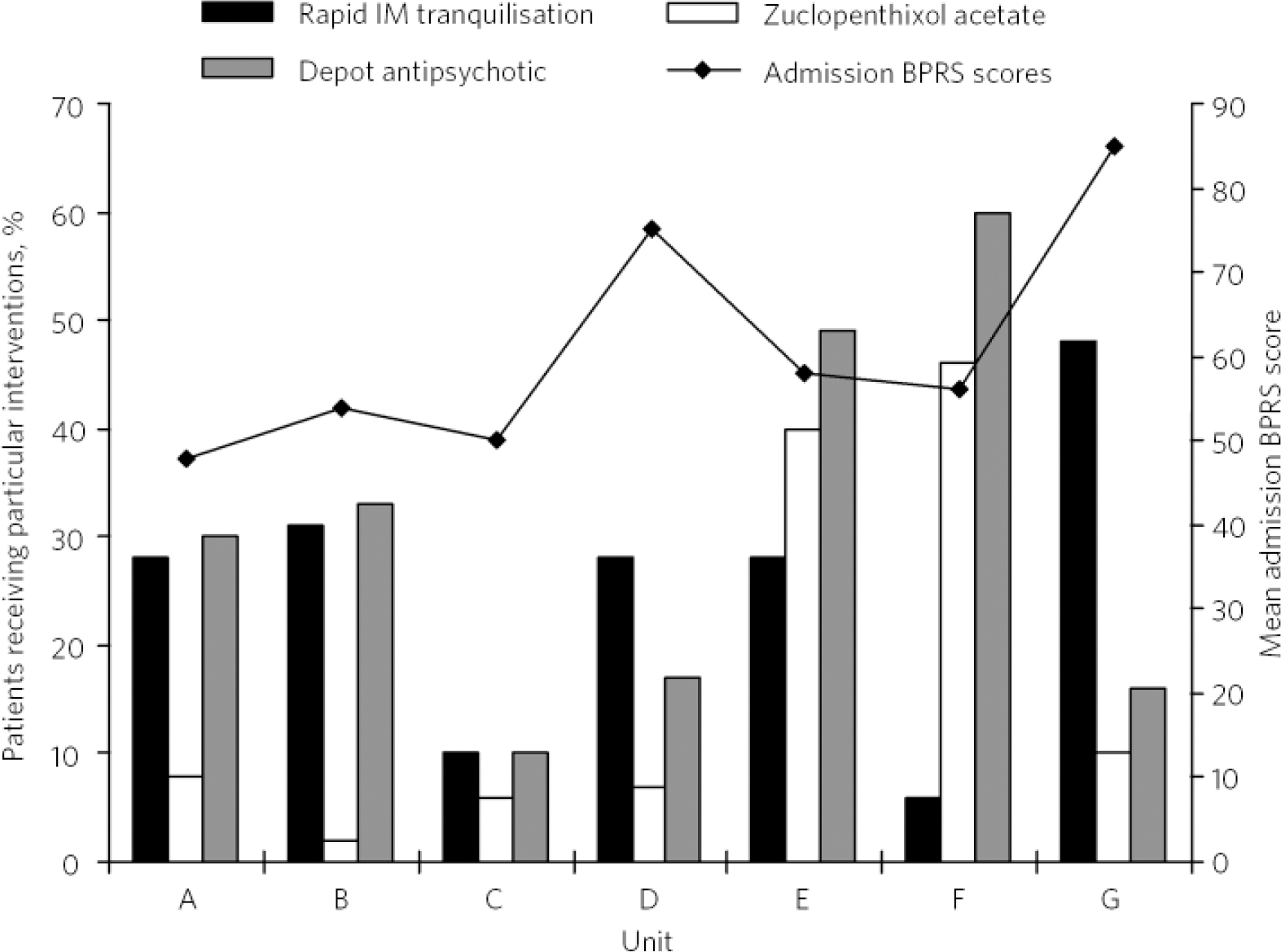
Fig 1 Proportion of patients in each unit receiving antipsychotic medication by intramuscular injection.a IM, intramuscular; BPRS, Brief Psychiatric Rating Scale. a. Unit D only recorded BPRS scores on 21 patients.
Zuclopenthixol acetate
The medium-acting antipsychotic injection zuclopenthixol acetate was given to 56 patients (17%); 23 patients (7%) received both rapid tranquillisation and zuclopenthixol acetate during the course of their admission. Of 67 patients experiencing a first episode, 9 (13%) received zuclopenthixol acetate; whether they were psychotropic-drug naive was not recorded.
There was a 23-fold variation in the use of zuclopenthixol acetate between the highest and lowest using unit (Fig. 1). Patients who received zuclopenthixol acetate had significantly higher BPRS scores on admission (63.0 v.57.0, t = 2.0, d.f. = 295, P = 0.04). The use of zuclopenthixol acetate was predicted by violence in the PICU (OR = 7.42, 95% CI 2.57-21.41, d.f. = 1, P<0.001), damage in PICU (OR = 7.57, 95% CI 2.87-19.93), male gender (OR = 4.17, 95% CI 1.15-15.14, d.f. = 1, P = 0.03) and by treatment either at unit E (OR = 15.94, 95% CI 2.70-93.89, d.f. = 1, P = 0.02) or F (OR = 29.33, 95% CI 4.8-178.42, d.f. = 1, P<0.001). No other variables were significant in univariate analysis.
Intramuscular depot injection
About a third of patients (n = 102) received antipsychotic medication by depot injection at some point during their PICU stay. Over half of these (n = 58) also received IM rapid tranquillisation (n = 27), zuclopenthixol acetate (n = 34) or both of these treatments (n = 13).
Oral medication
The variation between units in the use of oral psychotropic drugs was less marked than in respect of IM drugs (Fig. 2). There was little difference in the relative use of typical and atypical antipsychotic drugs. Benzodiazepines were given to 261 (79%) patients, all the units giving benzodiazepines to more than half of their patients. The greatest variation between units was in the use of mood stabilisers (principally lithium and sodium valproate) and antidepressant drugs. These were prescribed relatively infrequently, in a pattern which reflected the patients' primary diagnoses.
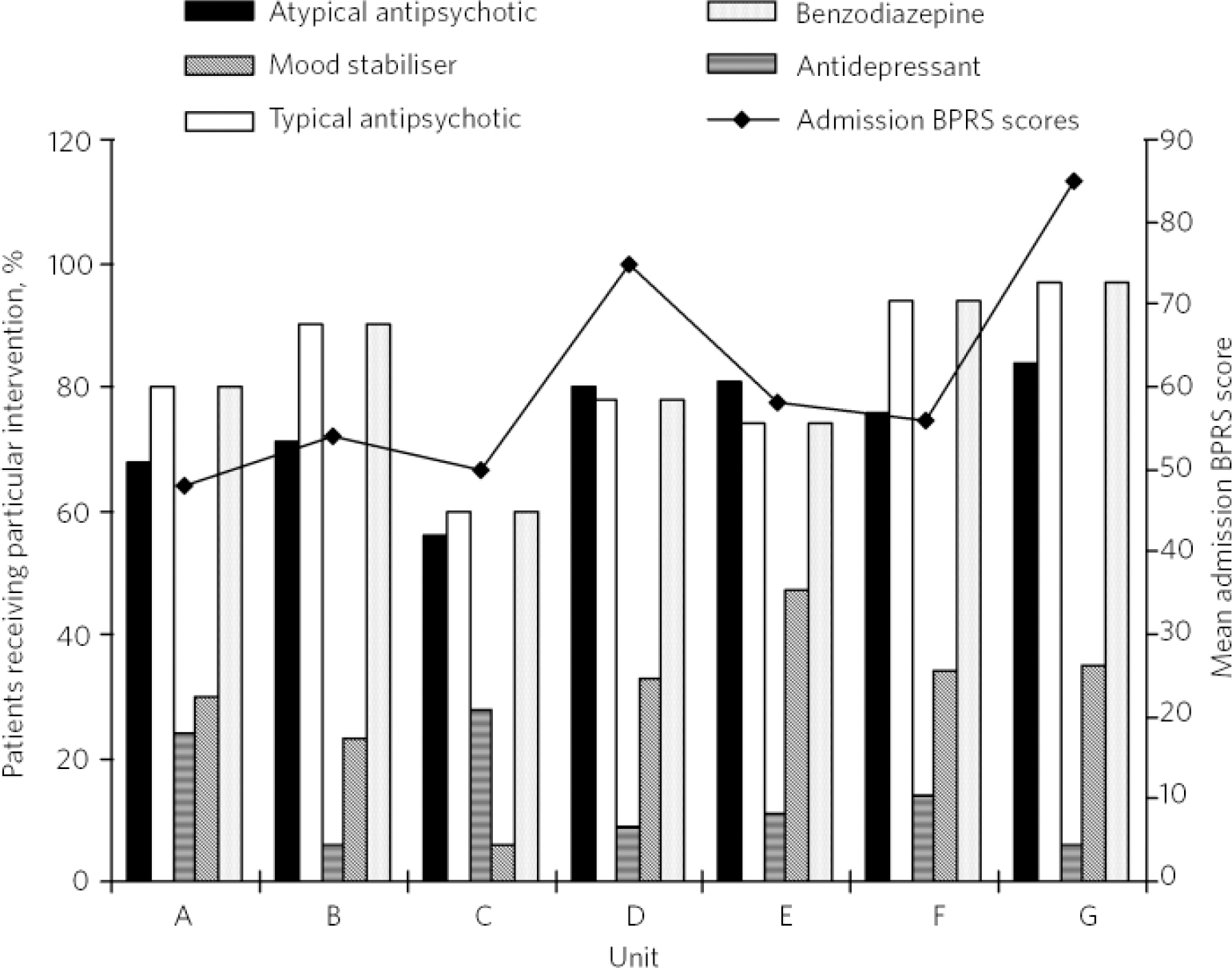
Fig 2 Proportion of patients in each unit receiving particular classes of oral psychotropic medication.a BPRS, Brief Psychiatric Rating Scale. a. Unit D only recorded BPRS scores on 21 patients.
Discussion
These results suggest that the standard treatment for patients admitted to a PICU is a combination of antipsychotic drug and benzodiazepine, with most patients receiving more than one antipsychotic drug during their stay. Nearly all the patients showed significant improvements in mental state during their PICU stay. Reference Brown, Chhina and Dye3 The study design cannot explicitly link the improvement to particular treatments, nor does it provide information on the relative efficacy of different drugs or allow more than the most general speculation about the appropriateness of these drug treatment interventions.
Bias
The units involved in the study were probably not representative of English PICUs. All were self-selected; all were actively involved in the National Association of Psychiatric Intensive Care units, either in research or through the clinical governance network. Thus the results may reflect better than average practice.
The patients were probably representative of those treated on these particular PICUs: the study described 332 consecutive admissions and lost only three from follow-up. The protocol aimed to collect data on 50 consecutive admissions at each site (350 admissions), but one unit (G) ceased data collection after 32 admissions after a change of role. This unit admitted more disturbed patients and recorded high rates of drug prescription so the loss of 18 data-sets probably reduced the mean overall drug use. This may have been partly balanced by the loss of data on three patients with brief PICU admissions who probably received little medication.
The main weakness of the study was its reliance on individual units to collect data about their own performance. This method was used because of the limited resources available but it must leave open the possibility of selective reporting. The results from each unit were internally consistent but there was no independent verification.
A second weakness was the focus on medication. A large part of the treatment undertaken in a psychiatric unit is psychosocial. Effective use of non-pharmacological interventions such as de-escalation probably reduces drug prescription but these are difficult and expensive to measure reliably in a multisite study.
The data about IM drug use should be robust as these came from drug charts, important legal documents which are closely locally monitored. The data about oral drug use are less robust. It is likely that some prescribed oral medication was not actually taken: non-adherence to prescribed medication is common Reference Okocha, Beer, Pereira and Paton15 and it is unlikely that PICUs are exempt from this problem. The failure to record specific drugs and dosages represents a missed opportunity but it was decided during the study design that this would make data collection more onerous and possibly decrease adherence to the study protocol.
The reported use of high-dose medication was inconsistent with the rest of the data and with a recent audit of prescribing on acute UK in-patient wards where 34% of patients were prescribed total antipsychotic doses in excess of BNF limits. Reference Paton, Barnes, Cavanagh, Taylor and Lelliot16 The reported results are probably an underestimate and probably arose because data collectors failed to understand (despite written guidance) that they should calculate the aggregate antipsychotic dose rather than simply check whether each individual drug exceeded BNF limits. This misunderstanding is probably widespread and has important safety implications.
Medication use
The overall pattern of drug use found in this study was similar to those found in previous studies of single PICUs. Reference Goldney, Bowes, Spence, Czechowicz and Hurley8,Reference Brown and Bass11 The overall use of rapid tranquillisation and zuclopenthixol acetate appeared similar to that in the south Manchester study, Reference Hyde, Harrower-Wilson and Morris10 but direct comparison was limited by lack of detail about the route of administration. Practice had clearly changed since Pilowsky et al's 1992 study when intravenous medication was used in more than half of rapid tranquillisation episodes. Reference Pilowsky, Ring, Shine, Battersby and Lader9
The present study suggests that rapid tranquillisation and zuclopenthixol acetate are used relatively infrequently - a mean of about 20 episodes/unit of rapid tranquillisation and 8 episodes/unit of zuclopenthixol acetate over an 18-month period. Extrapolating these figures to the 170 units identified as PICUs in a national survey Reference Pereira, Dawson and Sarsam2 suggests a very approximate national annual figure of 2350 episodes of rapid tranquillisation involving 1150 patients. A similar calculation suggests that about 1000 PICU patients receive zuclopenthixol acetate each year. These figures are slight underestimates as some of the units collected 50 patients in fewer than 18 months; they ignore the rest of the mental health system and thus underestimate the total use of these treatments. The figures represent a significant number of traumatic and potentially risky events but also suggest that individual clinicians use acute IM medication infrequently. This reinforces the need for effective staff training and supervision.
Compliance with guidelines
Clinicians on PICUs sometimes have to balance the use of potentially risky drug treatments against the risks of failing to control violent behaviour. Patients on those units fit the profile for being at high risk of neuroleptic malignant syndrome. Reference Keck, Pope, Cohen, McElroy and Nierenberg17 Antipsychotic drugs are associated with a small but significantly increased risk of sudden death; Reference Abdelmawla and Mitchell4 benzodiazepines cause respiratory depression. Reference Gibson, Fenton, Coutinho and Campbell19 The NICE and Maudsley guidelines accept that interventions such as forced IM injection and high-dose therapy are sometimes necessary. 5,Reference Taylor, Paton and Kerwin6 Both set stringent standards about the minimum equipment, facilities, monitoring and staff training needed to deal with potential emergencies and suggest that forced IM tranquillisation should not be used unless it can be safely administered and monitored. The responsibility to supply the necessary equipment and training lies with managers; the responsibility for individual drug prescription, administration and monitoring lies firmly with the responsible clinicians.
In its guidelines, NICE suggests that IM medication should be reserved for situations when other interventions ‘have failed, been refused, judged not a proportionate response or are not indicated by previous clinical experience’. 5 The guidelines do not define a threshold for the use of IM medication or suggest what proportion of patients should receive it. The Maudsley guidelines describe rapid tranquillisation as ‘essentially a treatment of last resort’ to be used when other approaches have ‘failed to de-escalate acutely disturbed behaviour’. Reference Taylor, Paton and Kerwin6 Thus these guidelines are sufficiently vague that most of the prescribing in this study fell within them.
The units varied greatly in their use of rapid IM tranquillisation (eightfold difference between lowest and highest user) and zuclopenthixol acetate (23-fold variation between lowest and highest user). A small amount of variation was introduced by unit E's involvement in a trial of sublingual midazolam for PRN treatment of agitation but most appears to represent differences in individual clinical practice. The variation in use of IM medication was far greater than would be explained by variations in aggressive behaviour between different units and did not correspond to the differences in mean admission BPRS scores. It is difficult to avoid the suspicion that some patients who received forced IM medication might have been managed successfully without it.
The use of zuclopenthixol acetate is particularly contentious. A Cochrane review identified a dearth of evidence supporting the use of zuclopenthixol acetate. Reference Holmes, Simmons, Beer, Pereira and Paton18 It is not recommended for rapid tranquillisation by NICE, but its guidelines say it may be ‘considered as an option’ in certain circumstances. 5 The Maudsley guidelines advise that zuclopenthixol acetate should only be used after a patient has required repeated injections of short-acting antipsychotic drugs. Reference Taylor, Paton and Kerwin6 Its use is, however, advocated by some clinicians who believe that the greater duration of action may reduce the need for repeated traumatic injections of shorter acting drugs.
This study suggests that zuclopenthixol acetate is not currently used in line with the available guidelines. Whether this represents poor clinical practice or inadequate guidelines is open to debate. There is a tension between the demand for evidence-based treatment protocols and individual clinical experience. This is particularly problematic in the treatment of severely disturbed individuals who lack capacity to consent to involvement in the kind of trials needed to provide a quality evidence base for treatment.
Conclusions
This study presents a snapshot of current drug prescribing in English PICUs. The units themselves may not be entirely representative but the results are robust enough to serve as reference data for clinical governance purposes. There was considerable variation in prescribing patterns between the units; nevertheless, any PICU whose prescribing diverged significantly from that described here should examine its practice carefully. Randomised controlled trials of emergency treatment to disturbed patients who lack capacity are probably impossible but further research is needed into the details of the specific drugs and dosages currently used to treat seriously disturbed behaviour. This should focus on actual clinical practice and should, if possible, be undertaken by independent researchers.
Funding
This study was partly financed by a travel grant of £500 to N.C. from the National Association of Psychiatric Intensive Care Units.
Acknowledgements
We thank everyone who contributed towards this study and especially the project leaders at each site: Agron Ramadani, Felix Kadzombe, Veronica Daus, Jo Pittam, Lisa Archibald and Catherine Seabourne. We thank Caroline Parker for her comments on the manuscript.






eLetters
No eLetters have been published for this article.