Perinatal mental health is a major public health concern, with 10% of postpartum mothers developing a depressive illness in the first year following delivery. Reference Cox, Holden and Sagovsky1 Four per 1000 will be admitted to a psychiatric unit, 2 per 1000 with puerperal psychosis. Reference Kendell, Chalmers and Platz2 Postnatal depression is the most common peripartum mental health problem, with an incidence of 13-20%. Reference Cox, Murray and Chapman3 When untreated, it can result in partner depression, higher divorce rates, higher rates of behavioural problems in children and lower emotional and cognitive developmental scores in children. Reference Lyons-Ruth, Zoll, Connell, Grunebaum, Tronick and Field4
The Confidential Enquiries into Maternal Deaths (CEMD) highlight the high human cost of perinatal mental illness, with suicide the leading cause of maternal death in the 2000-2002 report. Reference Lewis5 The last CEMD (2003-2005) 6 showed a decline in numbers of deaths by suicide, possibly owing to the implementation of improvements suggested in the 2000-2002 report, but psychiatric illness is still responsible for 0.85 deaths per 100 000 pregnancies, equivalent to the number of deaths owing to pre-eclampsia and eclampsia. Psychiatric disease is responsible for 6% of maternal mortality in the UK 6 and it has been a consistent finding over the past decade that the risk of recurrence of psychiatric disorder is poorly identified and managed. Sixty per cent of women who took their own life within the first year postpartum had a history of serious mental illness but only 40% of these were identified antenatally and only 20% had a detailed management plan in place.
In Ireland there are three dedicated mental health liaison clinics (all in Dublin), where perinatal mental healthcare is provided on a sessional basis by consultant psychiatrists with a special interest in perinatal mental health. In the remainder of the country, care is provided by general adult psychiatrists on an on-call basis. One of the main differences in the provision of antenatal care in Ireland when compared with the UK is that traditionally the majority of Irish women are seen regularly by an obstetrician during their pregnancy. However, in recent years there has been an increase in midwifery-led antenatal care and shared care between the primary care physician and the midwife.
The aim of this study was to determine the level of psychological service provision in the Coombe Women and Infants University Hospital, through review of the case notes of women who indicated in their booking questionnaire that they were experiencing, or had experienced in the past, mental health problems. Where mental health problems were identified by the midwife, we aimed to assess whether the obstetrician examined the patient's mental state, whether their mental health history was documented in the medical notes and if so, whether they were referred to the hospital social worker, to the mental health liaison clinic or to their sector mental health team.
Method
The study took place in the Coombe Women and Infants University Hospital, which has 8000-9000 deliveries per year. Women are assessed initially at the midwife booking clinic, where they complete a booking questionnaire which includes questions on obstetric and surgical history, medical and psychiatric history, as well as drug and social history. All women are thereafter assessed by an obstetrician at the obstetrician first visit clinic. There were 8088 deliveries in our hospital in 2006, with 7937 booking questionnaires completed. A sample of women who both booked and delivered in 2006 was chosen (n = 4188). Individual case-note review was performed on 27.4% of women (1147/4188) where past or present mental health problems were indicated. Patients with a standalone diagnosis of eating disorder, counselling or panic (n = 648) were excluded as the aim of the investigation was to focus on severe and enduring mental illness. These patients were included if they had a comorbid illness. Of the 499 women with a significant mental health history, 95% of the charts were available for review.
Results
When the case notes were reviewed, 12% (n = 499/4188) of women had a significant mental health history. Figure 1 details the information obtained at this initial midwifery booking visit.

Fig 1 Mental health information on booking questionnaire (n = 499).
Figure 2 summarises the documentation of mental health issues in the obstetrician's notes during the pregnancy. In 66% of women with a history of mental health problems (n = 328) there was no documented comment in the obstetric notes. There were 69 referrals to the mental health liaison clinic during the period under study. Of the 47 women who reported feeling depressed at the time of filling out the booking questionnaire, 26% had no comment made by the obstetrician in their case notes and only 40% were referred to the mental health liaison clinic. Of the 135 women who reported a history of postnatal depression, in 63% of cases this was not addressed by the obstetrician and only 16% were referred to the mental health liaison clinic. One patient reported a history of bipolar affective disorder, one a history of puerperal psychosis and one a history of schizophrenia. There was no comment documented in the obstetric case notes of those patients, with no referral to psychiatric services or no evidence of a detailed multidisciplinary management plan.
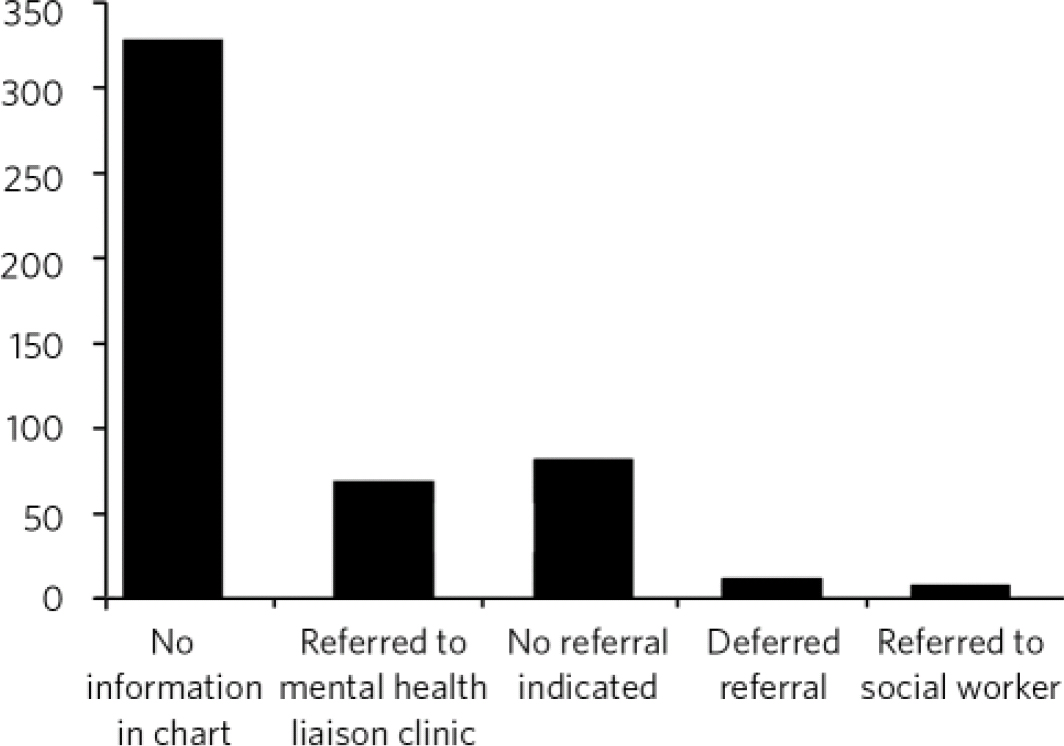
Fig 2 Documentation of psychiatric history in obstetric medical notes.
Discussion
Forty-seven women reported being depressed when completing the booking questionnaire. Out of a total of 4188 women, this is a low rate (1%). In the 2001 European Outcome of Depression International Network (ODIN) study, Ayuso-Mateos et al Reference Ayuso-Mateos, Vázquez-Barquero, Dowrick, Lethinen, Dalgard and Casey7 reported the prevalence of female depressive episodes in urban Ireland at 20% (95% CI 5.3-53.9).
The rate of bipolar affective disorder and schizophrenia in our study was 1 reported patient out of 4188. These low rates could possibly be explained by a number of reasons - women being reluctant to report illness themselves because of stigma, the fear of Social Services becoming involved or inflexible phraseology in the booking questionnaire, which may make it difficult for the woman to report her diagnosis. It is possible that lack of insight into their illness may also account for the low rates of reported mental illness in our study. It is also possible that the retrospective design of the study may lead to falsely low rates, whereas a prospective, specifically designed questionnaire may provide a more accurate picture. We agree with the view that the blanket term ‘postnatal depression’ is unhelpful and may do a disservice to women experiencing severe postnatal episodes of illness. Reference Oates8
Strengths and limitations
Ninety-five per cent of the charts were available for review. The hospital's electronic database was used to identify cases; however, we acknowledge that data entry into the database may have been subject to entry error. This investigation used only the written case notes as evidence that the obstetrician addressed the mental health history. In some cases there may have been conversations in relation to the mental health history which were not documented. Likewise, there may have been verbal referrals to the social worker or sector mental health teams that were not documented. These findings are based on an Irish setting, therefore it is difficult to estimate how generalisable they are to other settings.
Further actions
The results of this study were presented at the grand rounds in the Coombe Women and Infants University Hospital, and the response from the consultants and midwives was very positive. We have been invited to take part in the midwife educational training programme and have recommended that the non-consultant hospital doctor induction programme should incorporate a module on perinatal mental health. This should include practical interview skills so as to make it easier for obstetric staff to enquire about mental health concerns. Also recommended is the appointment of a dedicated mental health liaison nurse on site to provide immediate advice and support. We are happy to report that a dedicated mental health liaison nurse commenced practice in June 2010. As a result of the findings from our study, a mental health liaison clinic referral form was designed to make it easier for hospital staff to refer patients to our service. Future initiatives include a poster campaign in the hospital to increase awareness of psychological problems and reduce stigma and the compilation of an information booklet on perinatal mental health which will be given to all patients at their booking clinic visit.
Acknowledgements
We thank the Master of the Coombe Women and Infants University Hospital, the Medical Ethics Committee and the IT and Medical Records Department.





eLetters
No eLetters have been published for this article.