The organisational structure of the National Health Service (NHS) in England is undergoing major transformation. Reforms initiated by the last Labour government have been endorsed and extended by the Coalition government and will change how healthcare services are commissioned and regulated.
In the past, the NHS was funded via primary care trusts through the block contract payment mechanism. As part of the modernisation of the NHS, the Department of Health (England) introduced a payment by results system in the acute sector from 2003 to fund healthcare based on activity, with reimbursement according to national tariffs. Reference Jacques1 Acute medical specialties are reimbursed via the payment by results system 2 according to the numbers of patients in each Healthcare Resource Group reported to commissioners. This can disadvantage mental health services when the acute sector ‘over perform’ against expected activity and claim more funding than was budgeted from finite primary care trust resources. The payment by results process is being extended to mental health services, with 2012 as the introductory year for many adult and older adult services. Providers will be reimbursed according to their activity levels (and eventually outcomes), with the possibility of nationally set tariffs from 2014.
To support the extension of payment by results to secondary mental health services, the Department of Health commissioned the development of a tool to assign patients within a classification system based on need and likely service utilisation, not primarily on their diagnosis. The tool used to deliver payment by results in mental health is the Mental Health Clustering Tool (MHCT), 3 which was developed jointly by the Royal College of Psychiatrists and the Care Pathways and Packages Project (CPPP, www.cppconsortium.nhs.uk). The MHCT combines the Health of the Nation Outcome Scales (HoNOS) Reference Wing, Curtis and Beevor4 with six of the CPPP Summary of Assessments of Risk and Need (SARN) Reference Self, Rigby, Leggett and Paxton5 scales. Problem severity is assessed by clinicians on a0-4 scale. This modification of an established outcome measure, to record clinical need at assessment, enables clinicians to assign people accessing secondary mental health services to a set of 21 care clusters developed by the CPPP. Following a full clinical assessment, the scores recorded by clinicians on the MHCT are matched against those required for assignment to each of the 21 care clusters as described in the Mental Health Clustering Booklet. 3 There are concerns regarding the advantages and disadvantages of the payment by results system. Reference Fairbairn6 Despite these concerns the Department of Health has a clear time frame for the implementation of mental health payment by results. Reference Alexander7
The scope of payment by results in mental health does not yet include learning disability services, forensic secure or child and adolescent mental health services. The MHCT is based on the HoNOS which, unlike the HoNOS for People with Learning Disability (HoNOS-LD) tool, does not contain the additional scales that are required to capture the specific needs of people with intellectual disability. An integrated mental health and learning disability clustering tool is in development, based on the HoNOS-LD scales, which may become available to clinicians during 2012.
Our organisation, South London and Maudsley NHS Foundation Trust, was an early implementer of payment by results in mental health in the adult and older adult trust services. Although the MHCT was not designed to capture the needs of adults with intellectual disability or pervasive developmental disorder, adults with these conditions who require acute mental healthcare often access community or in-patient adult mental health services when the MHCT is used to identify their needs.
This paper reports a local evaluation of the MHCT when used for people with intellectual disability accessing specialist mental health services. It is an important area that needs to be researched and evaluated. Promoting inclusion and facilitating access for people with intellectual disability to general adult mental health services, as emphasised in government policies, 8 means identifying additional needs associated with intellectual disability and ensuring these are reflected in the tariff for a particular care cluster. We were interested to establish what proportion of adults with intellectual disability on our case-load with or without pervasive developmental disorder could be assigned to the current clusters and also to identify any common characteristics in those who could not be assigned to any cluster other than the variance cluster, Cluster 0.
Method
We assessed our active case-load using the MHCT to evaluate the utility of the tool for adults accessing specialist mental health in learning disability services and specifically to establish whether these patients could be assigned to the present care clusters (Table 1). Three clinicians having direct clinical contact with each service user carried out this pilot evaluation of the tool after attending a training day. At least one clinician from the team who had been in direct contact with the service user was involved in administering the tool. Clinicians who were not trained in using the tool either administered the MHCT in the presence of a trained clinician or had their work reviewed following administration.
TABLE 1 The 21 care clusters for payment by results in mental health
| Cluster | Description |
|---|---|
| 1 | Common mental health problems (low severity) |
| 2 | Common mental health problems (low severity with greater need) |
| 3 | Non-psychotic (moderate severity) |
| 4 | Non-psychotic (severe) |
| 5 | Non-psychotic disorders (very severe) |
| 6 | Non-psychotic disorder of over-valued ideas |
| 7 | Enduring non-psychotic disorders (high disability) |
| 8 | Non-psychotic chaotic and challenging disorders |
| 9 | Blank cluster |
| 10 | First-episode psychosis |
| 11 | Ongoing or recurrent psychosis (low symptoms) |
| 12 | Ongoing or recurrent psychosis (high disability) |
| 13 | Ongoing or recurrent psychosis (high symptoms and disability) |
| 14 | Psychotic crisis |
| 15 | Severe psychotic depression |
| 16 | Dual diagnosis |
| 17 | Psychosis and affective disorder - difficult to engage |
| 18 | Cognitive impairment (low need) |
| 19 | Cognitive impairment or dementia complicated (moderate need) |
| 20 | Cognitive impairment or dementia complicated (high need) |
| 21 | Cognitive impairment or dementia complicated (high physical or engagement) |
It was proposed to administer the MCHT instead of the routine outcome measure HONOS-LD Reference Roy, Matthews, Clifford, Fowler and Martin9 to all 127 patients who were active on the Lambeth community mental health learning disability team case-load between April 2010 and October 2010. However, 10 of the patients could not be included for the following reasons: lack of comprehensive historical clinical records (n = 7), new referrals yet to be seen (n = 2) and patients in transition (n = 1).
The community team covers the adult population in the London Borough of Lambeth, which is a multi-ethnic inner-city borough. Adults with intellectual disability access mainstream mental health services when needed, and are only referred to our specialist mental health team based on the complexity of their needs or disability. Acute mainstream adult mental health beds are used for crisis admissions. At the time of this evaluation there was no information available regarding the development of a revised version of the MHCT that might meet the needs of our patients.
The patients’ MHCT scores and cluster assignments were recorded on the Trust's electronic clinical records system and cluster assignment was checked using an online clustering algorithm (an Excel macro) which estimated best fit to cluster based on reported scale scores. This clustering algorithm was manually overridden where necessary, with clinicians exercising their clinical judgement when assigning to clusters, in line with the national guidance for using the MHCT. Patients were not contacted for this evaluation and data were anonymised before analysis. The data were collected on a standard proforma and included demographics, level of intellectual disability, presence or absence of pervasive developmental disorder, care programme approach status, MHCT scores and cluster assignment.
Data were analysed using SPSS v15 for Windows. The dependent variable in the analyses was whether or not patients were allocated to Cluster 0. Preliminary univariate analyses for categorical variables were tested with χ2-tests and for continuous variables with t-tests. The MHCT scale scores were categorised 0-2 v. 3-4 (absent to mild v. moderate to very severe). Variables significantly associated with the dependent variable (P<0.05) were included in a binary logistic regression.
Results
The average age of women in the sample was slightly greater than that for men (mean 44.8 years v. 42.2 years) and 62% of the sample was male.
The MHCT ratings were recorded for 117 patients on our team case-load. As anticipated, clinicians were unable to match problem severity on MHCT scales to that required for assignment to the 21 care clusters in a large proportion of the sample, and 48% (56/117) were assigned to the ‘variance’ cluster, Cluster 0. This is an appropriate decision when the person's presenting needs are not adequately captured by the profiles of need required for assignment to the current 21 clusters but a mental health service is, or will be, provided. Cluster 0 patients were compared with the patients allocated to one of the 21 care clusters to identify differences in needs between the two groups.
Level of intellectual disability was determined by the patients’ ICD-10 diagnosis (i.e. F70 (mild), F71 (moderate), F72 (severe)). 10 These diagnoses are not among those which are expected for the 21 clusters that have been adopted for adults of working age/older adults in non-specialist services. Of the whole sample, 59.8% (70/117) individuals had mild intellectual disability, and 65.7% of people with mild intellectual disability were assigned to Clusters 1-21 compared with 31.9% of people with moderate or severe intellectual disability assigned to Clusters 1-21.
Preliminary univariate analysis showed that there was a significant association between intellectual disability severity (mild) and clinicians’ ability to assign patients to Clusters 1-21 (χ2 = 12.87, d.f. = 1, P<0.001).
Pervasive developmental disorder was recorded for 34% (40/117) of the sample, but 51.8% (29/56) of those assigned to Cluster 0 had pervasive developmental disorder, whereas only 18% (11/61) of those assigned to Clusters 1-21 had pervasive developmental disorder. The association between pervasive developmental disorder and assignment to Cluster 0 was significant (χ2 = 14.73, d.f. = 1, P<0.001).
There was also a significant association between pervasive developmental disorder and level of intellectual disability (χ2 = 22.50, d.f. = 1, P<0.001).
There was no association between assignments to Clusters 1-21 as opposed to Cluster 0 based on age, gender or care programme approach status. Neither was mean total HoNOS score associated with assignment to either cluster group (t = 1.01, d.f. = 115, P = 0.316).
Average (mean) scores on each of the MHCT scales were compared for both cluster groups (Cluster 0 v. Clusters 1-21), shown in Fig. 1. These suggested possible differences between cluster groups on the scales measuring: overactive, aggressive, disruptive or agitated behaviour; cognitive problems; hallucinations and delusions; activities of daily living; historic problems with agitated, aggressive behaviour/expansive mood; safeguarding children and vulnerable adults; problems with engagement; and vulnerability.
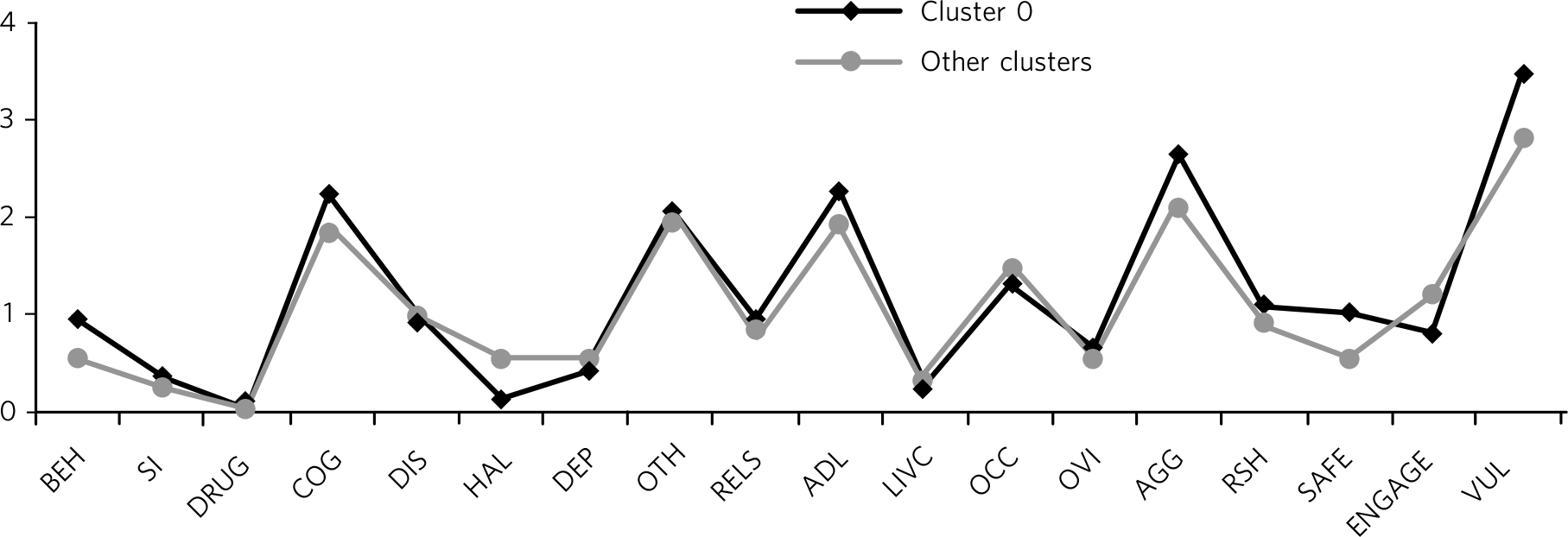
FIG. 1 Comparison of mean scores on Mental Health Clustering Tool scales for Cluster 0 and other clusters (n = 117).
BEH, overactive, aggressive, disruptive or agitated behaviour (current); SI, non-accidental self-injury (current); DRUG, problem-drinking or drug-taking (current); COG, cognitive problems (current); DIS, physical illness or disability problems (current); HAL, problems associated with hallucinations and delusions (current); DEP, problems with depressed mood (current); OTH, other mental and behavioural problems (current); RELS, problems with relationships (current); ADL, problems with activities of daily living (current); LIVC, problems with living conditions (current); OCC, problems with occupation and activities (current); OVI, strong unreasonable beliefs occurring in non-psychotic disorders only (current); AGG, agitated behaviour/expansive mood (historical); RSH, repeat self-harm (historical); SAFE, safeguarding other children and vulnerable adults (historical); ENGAGE, engagement problems (historical); VUL, vulnerability (historical).
The question of whether MHCT scales and their anchor points should be treated as continuous or categorical variables is debated and the MHCT scales data were recoded into two categories, with the higher severity scores of 3 and 4 (corresponding to moderate to very severe problems) in one group and lower severity scores of 0-2 (absent to mild problem severity) in another group.
Preliminary analyses using the categorical variables described above considered the relationship between MHCT scale severity and cluster group assignment. The results are summarised in Table 2. The MHCT scale 13 (‘Strong unreasonable beliefs occurring in non-psychotic disorders only’) was excluded from the analysis because data were missing in 49% of cases.
TABLE 2 Percentage of patients in Cluster 0 with moderate to very severe scores on Mental Health Clustering Tool scales compared with those assigned to Clusters 1-21
| Scale | Cluster 0, % | Clusters 1-21, % | P |
|---|---|---|---|
| 1: Overactive, aggressive, disruptive or agitated behaviour in the current rating period | 10.7 | 8.2 | 0.641 |
| 2: Non-accidental self-injury | 1.8 | 1.6 | 0.951 |
| 3: Drug/alcohol problems | 0.0 | 0.0 | |
| 4: Cognitive problems | 33.9 | 21.3 | 0.126 |
| 5: Physical illness/disability | 12.5 | 13.1 | 0.921 |
| 6: Hallucinations/delusions | 2.0 | 6.7 | 0.251 |
| 7: Depressed mood | 0.0 | 1.7 | 0.341 |
| 8: Other mental and behavioural problems | 27.8 | 19.1 | 0.31 |
| 9: Relationship problems | 14.5 | 11.7 | 0.647 |
| 10: Activities of daily living | 39.3 | 21.7 | 0.039 |
| 11: Problem with living conditions | 1.8 | 3.3 | 0.61 |
| 12: Problems with occupation and activity | 19.6 | 18.3 | 0.857 |
| 13: Strong unreasonable beliefsFootnote a | - | - | - |
| A: Historic problems with agitated behaviour/expansive mood | 62.5 | 38.3 | 0.009 |
| B: Historic repeat self-harm | 7.3 | 13.3 | 0.288 |
| C: Historic safeguarding issues | 21.4 | 10.9 | 0.133 |
| D: Historic engagement problems | 10.7 | 20.0 | 0.168 |
| E: Historic vulnerability | 85.7 | 61.7 | 0.003 |
a. Not analysed (see text).
These results indicated significant differences between cluster groups in MHCT scale severity on the three scales measuring problems with activities of daily living, historic problems with agitated, aggressive behaviour/expansive mood, and vulnerability.
These three variables (each categorised either 0-2or 3-4) plus the variables coding level of intellectual disability (mild v. moderate/severe) and the presence of pervasive developmental disorder were then entered into a binary logistic regression analysis with cluster group (Cluster 0 v. Clusters 1-21) as the dependent variable. The ratio of cases (n = 117) to this number of variables is acceptable with binary logistic regression and the results are shown in Table 3.
TABLE 3 Result of binary logistic regression analysis
| WaldFootnote a | P | Exp (B)Footnote b | |
|---|---|---|---|
| Presence of pervasive developmental disorder | 7.42 | 0.01 | 3.86 |
| Level of intellectual disability | 1.93 | 0.16 | 1.94 |
| Scale A (historic aggression) | 5.09 | 0.02 | 2.68 |
| Scale E (vulnerability) | 3.38 | 0.07 | 2.64 |
| Scale 10 (activities of daily living) | 0.16 | 0.69 | 1.22 |
| Constant | 14.22 | 0.00 | 0.12 |
a. Equivalent to Z statistic.
b. Equivalent to odds ratio.
This multivariate analysis indicated that only the presence of pervasive developmental disorder and Scale A score severity were independently associated with assignment to Cluster 0.
Discussion
Assignment to cluster group
The clustering algorithm was estimated to be accurate on less than 65% of occasions by those who tested it for the Trust. In this study, there may be issues with the coding of patients in Clusters 2-5 (non-psychotic) where the scores on key scales were out of the expected range for 11 patients who had been assigned to these non-psychotic clusters. Some were undercoded and others overcoded based on their reported scores. Furthermore, six patients assigned to psychosis clusters had scores on a key scale out of the expected range for the attributed cluster. This was the result of clinicians deciding on the most appropriate cluster based on their clinical knowledge of the service user and their history rather than on their presentation in the 2-week rating period for the HoNOS. Thus the clustering algorithm was manually overridden where necessary, with clinicians exercising their clinical judgement when assigning to clusters, in line with the national guidance for using the MHCT. 3
Clinicians’ ability to assign patients to the current Clusters 1-21 was primarily related to the absence of pervasive developmental disorder in those assessed. Severity of intellectual disability did not appear to be associated with Cluster 0 assignment independent of pervasive developmental disorder. Historical agitation, aggression/expansive mood was more evident in the Cluster 0 group.
It appears that the characteristics and needs of people with pervasive developmental disorder are different from patients with intellectual disability, and probably from adult mental health patients of working age and older adults.
The MHCT is designed for use at the time of presentation and at key points of review when cluster transitions reflect changes in the individual's care needs. This study applied the tool cross-sectionally to an existing case-load and so may not be a true reflection of its use in practice for payment by results. However, the existing 21 clusters capture the mental health needs of people with intellectual disability in only 52% of patients in our study.
Clinical implications
There is a need to develop other clusters which capture the needs of those with pervasive developmental disorder and severe behavioural difficulties associated with intellectual disability in whom it is difficult to establish an underlying mental illness. If the care clusters are to be the commissioning currency of the future, then it is important that the additional needs of people with intellectual disability who access mental health services are adequately assessed and reflected in the tool. This would also minimise the need to clinically override any clustering algorithm that is nationally mandated for cluster data quality assurance.
We are aware that a national pilot project is currently in development to evaluate a modified clustering tool (Integrated Mental Health and Learning Disability Clustering Tool) to identify the needs of this population. Until the tool is available to clinicians, the use of the MHCT to identify the needs of people with intellectual disability, especially those with moderate to severe intellectual disability, will result in an incomplete assessment of their needs.
Implications
-
(a) The MHCT in its current form does not reliably capture the needs of patients with intellectual disability when used in clinical settings.
-
(b) Most people with mild intellectual disability (65.7% in our study) accessing specialist mental health of learning disability services could be allocated to existing clusters, making the current clusters, more relevant for people with mild intellectual disability.
-
(c) The planned revision of the tool should incorporate options to capture the more specialist needs of people with intellectual disability and mental health needs. For instance, the description of scale ratings in existing clusters could be revised to enable higher level of needs (e.g. vulnerability, activities of daily living) to be scored.
-
(d) People with pervasive developmental disorder have additional needs which can onlybereliablycaptured by additional clusters that specifically identify their needs.
-
(c) Use of the MHCT tool in its current form to allocate people with intellectual disability to care clusters for payment purposes could result in services not being paid for all interventions offered during treatment episodes.
Acknowledgements
We would like to thank the trainee doctors (Dr Katrina Davis and Dr Nkechi Ofor) and community psychiatric nurses (Marina Russ and Susan Greaves) for their contribution to the project through administering the tool alongside the main authors.







eLetters
No eLetters have been published for this article.