People with mental health problems often consider employment as a yardstick to their recovery. Reference Shepherd1,Reference Dunn, Wewiorski and Rogers2 However, they experience low rates of employment, especially those using secondary mental health services, of whom typically between 4 and 16% are employed. Reference Perkins and Rinaldi3-Reference Marwaha, Johnson, Bebbington, Stafford, Angermeyer and Brugha5
The low priority given to employment by mental health professionals combined with the low expectations of people with mental health problems themselves in being able to gain employment may partly account for these low employment rates. 6-Reference Rinaldi, Perkins, Glynn, Montibeller, Clenaghan and Rutheford8 These low expectations are reinforced by the attitudes of an overwhelming number of professionals, with only 8% of community mental health teams’ (CMHTs) case notes addressing vocational needs Reference Bertram and Howard9 and mental health professionals holding the belief that the majority of people on their case-loads are only capable of sheltered or voluntary work. Reference Marwaha, Johnson and Balachandra10 Yet, surveys in England show that people with mental health problems who use mental health services would like help with gaining employment: 11 supporting people to do the things they want to do is critical if we are to successfully enable recovery, independence and inclusion.
The individual placement and support (IPS) approach is an evidence-based practice and has repeatedly been shown to be more effective than other vocational rehabilitation approaches in enabling people with severe mental health problems to gain employment. Reference Crowther, Marshall, Bond and Huxley12-Reference Rinaldi and Perkins14 It has been recommended by the Department of Health 15,16 and the National Institute for Health and Clinical Excellence. 17,18 The South West London and St George’s Mental Health NHS Trust has successfully implemented the IPS approach to high fidelity within CMHTs Reference Rinaldi and Perkins14,Reference Rinaldi and Perkins19 and early intervention teams for young people with a first episode of psychosis Reference Rinaldi, McNeil, Firn, Koletsi, Perkins and Singh20,Reference Rinaldi, Perkins, Hickman, McNeil and Singh21 and evaluated the lessons learnt to implementing this evidence-based practice. Reference Rinaldi, Perkins, Glynn, Montibeller, Clenaghan and Rutheford8,Reference Rinaldi, Miller and Perkins22 This paper reports the effects of implementing the IPS approach within four CMHTs in London and the associated effect on the employment rates across these teams. In addition, service user experience is reported in relation to met and unmet need with finding work and the perception of whether service users felt they were unable to work because of their mental health problems.
Method
The IPS service
In February 2004, the IPS approach was implemented in the four CMHTs in the London borough of Merton, with three employment specialists working across these teams. By January 2005 there was a full-time employment specialist in each CMHT and an independent assessment identified that high-fidelity IPS was being delivered. 17
Cross-sectional survey
Data concerning the vocational status of people with longer-term mental health problems during the 10 years from 1990 to 1999 were collected via a cross-sectional survey of adults using secondary mental health services in Merton. Basic demographic, psychiatric, service usage, accommodation and vocational information was collected by care coordinators on 1 April each year for all service users who had experienced their first contact with psychiatric services at least 2 years previously. Vocational status was reported in five categories: open employment, sheltered work, voluntary work, mainstream education and unemployed. Open employment included ordinary, existing, full-time, part-time or casual work gained in open competition. It did not include jobs created under special employment schemes for people with mental health problems.
On 1 December 2003 the cross-sectional survey was repeated using the same survey tool, criteria and method previously used within the service during the 1990s. The survey was repeated thereafter on 1 December each year through to 2006.
General employment rates for Merton were obtained from the Office for National Statistics. 23
Service user survey
In the last quarter of 2006, a questionnaire survey was conducted in Merton to find out what service users thought about the care they received from mental health services. Using the Healthcare Commission’s community mental health service users’ survey instrument, 11 care coordinators were asked to distribute the questionnaire to all service users, encouraging them to complete and return it anonymously in a ‘free-post’ envelope supplied. A section of the survey asked service users to rate the support they have received within the community. One question in this section asked: ‘In the past 12-months, have you received any help with finding work?’ There were four response options: ‘Yes’, ‘No, but I would have liked some’, ‘I did not need any help’ and ‘I cannot work because of my mental health problems’.
Results
Employment rates
Table 1 shows that there was a mean of 569 longer-term service users in Merton in contact with local mental health services each year between 1990 and 1999, over half of whom had a diagnosis of schizophrenia. For the years 2003-2006 there was a mean of 728 longer-term service users in contact with mental health services, over half of whom had a diagnosis of schizophrenia.
Table 1 Characteristics of the population of longer-term service users from Merton, 1990–1999 and 2003–2006

| 1990– 1999 |
2003– 2006 |
|
|---|---|---|
| Mean total number | 569 | 728 |
| Mean percentage males | 43% | 46% |
| Mean age, years (s.d.) | 43.5 (11.4) | 42.8 (11.8) |
| Primary diagnosis | ||
| Schizophrenia/schizoaffective disorder | 55.8% | 51.6% |
| Bipolar disorder | 11.4% | 11.5% |
| Depression | 16.9% | 19.3% |
| Anxiety | 5.6% | 5.2% |
| Other | 10.3% | 12.5% |
Table 2 shows general employment rates in Merton from 1994 to 2006 (data from the Labour Force Survey 23 were only available from 1994) and employment rates for longer-term service users from 1990 to 1999 and 2003 to 2006 (the two periods when our cross-sectional survey was carried out). Between 1990 and 1999 the employment rate among service users with longer-term mental health problems decreased significantly (χ2 = 18.9, d.f. = 1, P>0.0001). Employment rates decreased from 25.7% in 1990 to 19.2% in 1993 and it can be assumed that this downward trend was also found in the general employment rate in Merton as the country was in recession. However, April 1993 is regarded as when the country came out of the last recession 24 and the general employment rate in Merton grew from 76.8% in 1994 to 79.3% by 1999. By contrast, the employment rates for longer-term service users continued to decrease, from 14.2% in 1994 to 13.6% by 1999. The employment rate also significantly decreased for long-term service users with a diagnosis of schizophrenia between 1990 and 1999 (χ2 = 7.17, d.f. = 1, P>0.01). The employment rate among this group fell from 16.6% in 1990 to 8.5% in 1999, despite the increase in general employment rates during the latter part of this period.
Table 2 Employment rates in Merton 1990–2006

| % | |||
|---|---|---|---|
| Employment rate among longer-term service usersFootnote b |
|||
| Year | General employment rate in MertonFootnote a |
All service users | Diagnosis of schizophrenia |
| 1990 | – | 25.7 | 16.6 |
| 1991 | – | 24.7 | 17.3 |
| 1992 | – | 20.9 | 13.8 |
| 1993 | – | 19.2 | 10.8 |
| 1994 | 76.8 | 14.2 | 9.1 |
| 1995 | 76.2 | 12.5 | 7.5 |
| 1996 | 76.3 | 16.8 | 9.3 |
| 1997 | 77.7 | 14.0 | 9.0 |
| 1998 | 78.9 | 14.8 | 7.9 |
| 1999 | 79.3 | 13.6 | 8.5 |
| 2000 | 73.7 | – | – |
| 2001 | 78.5 | – | – |
| 2002 | 79.1 | – | – |
| 2003 | 77.2 | 10.9 | 7.8 |
| 2004 | 75.8 | 13.7 | 11.2 |
| 2005 | 71.2 | 19.0 | 14.4 |
| 2006 | 74.1 | 20.5 | 15.9 |
a. Data from the Labour Force Survey were only available from 1994. Reference Kilian and Becker26
b. The cross-sectional survey was not carried out in 2000–2002.
The cross-sectional survey was not carried out between 1999 and 2003. Within this time the employment rate among service users with longer-term mental health problems decreased significantly, from 13.6% in 1999 down to 10.9% in 2003 (χ2 = 4.06, d.f. = 1, P>0.05). However, for those longer-term service users with a diagnosis of schizophrenia the employment rate only decreased marginally from 8.5% in 1999 to 7.8% in 2003 (χ2 = 0.353, d.f. = 1, P = NS).
In 2004, IPS was implemented into the four CMHTs in Merton; Fig. 1 shows the impact on the employment rates among service users with longer-term mental health problems. In 2003, the employment rate for longer-term service users was 10.9% and by 2006 this had risen significantly to 20.5% (χ2 = 8.60, d.f. = 1, P>0.0003). Figure 2 shows that the same effect was found for longer-term service users with a diagnosis of schizophrenia: in 2003 the employment rate was 7.8% and this rose to 15.9% in 2006 (χ2 = 10.2, d.f. = 1, P>0.001). However, this trend is not found in the general employment rate for Merton: in 2003 the general employment rate was 77.2% and it decreased for the next 2 years down to 71.2% in 2005, before rising again in 2006 to 74.1%.
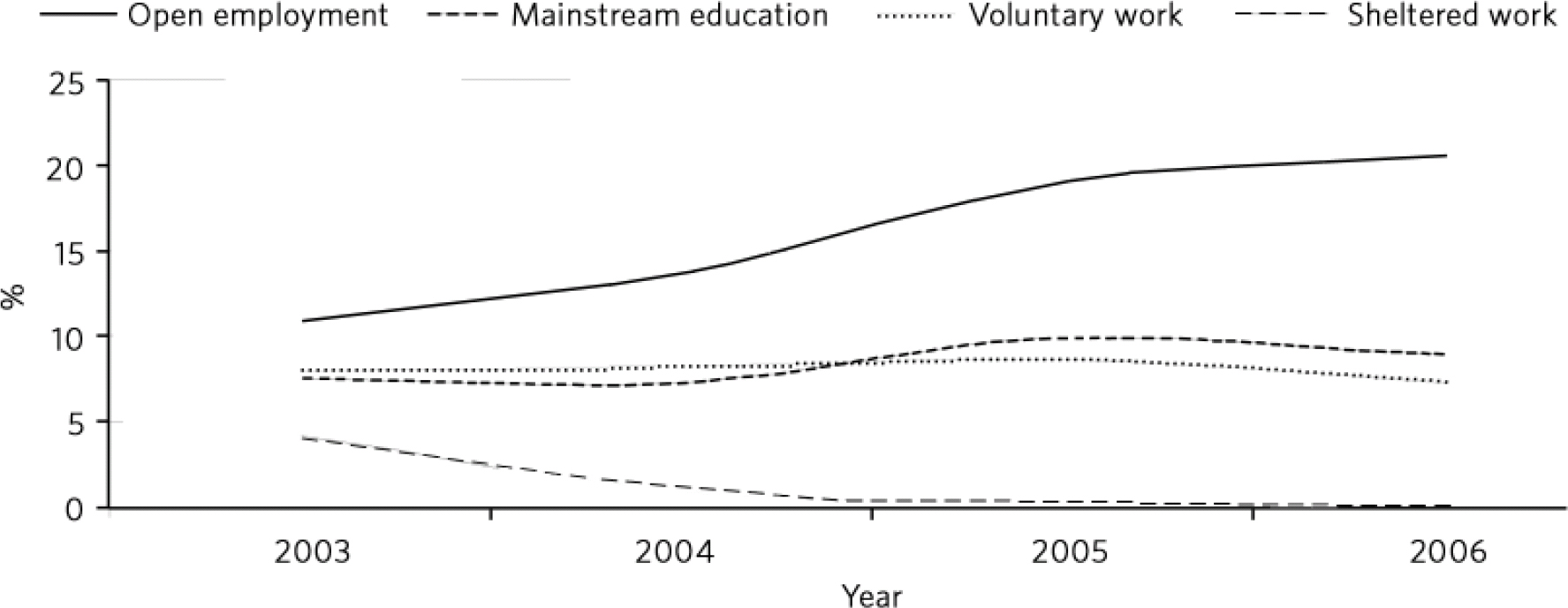
Fig 1 Long-term service users in Merton engaged in work or employment.
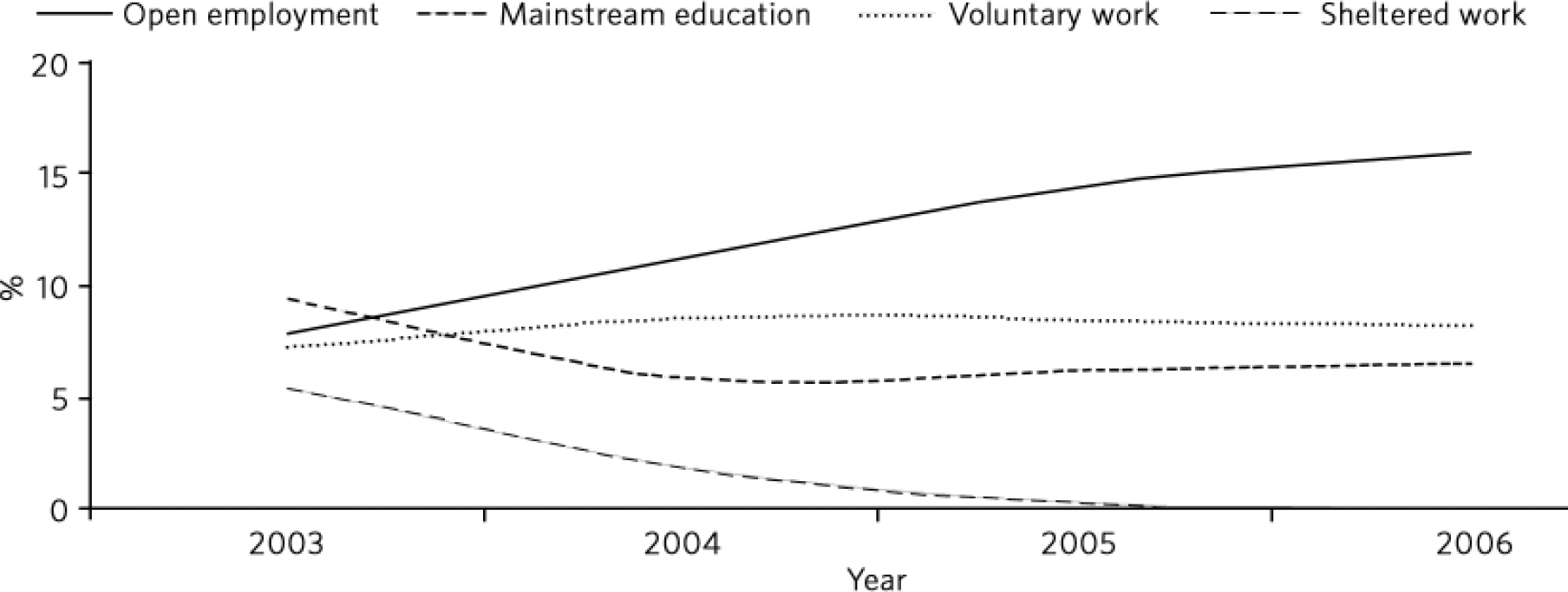
Fig 2 Merton long-term service users with a diagnosis of schizophrenia engaged in work or employment.
During the 1990s a sheltered workshop was available to people with mental health problems who lived in Merton along with a variety of pre-vocational schemes to help them gain employment. In 2000 a worker was introduced into the Volunteer Bureau to assist people with mental health problems in taking up volunteering opportunities. In 2003, a day centre closed that provided the funding for the employment specialists in the CMHTs. The sheltered workshop closed in the financial year 2004/05. It is encouraging to note, as Fig. 1 and 2 show, that although the closure of the sheltered workshop resulted in nobody undertaking further sheltered work, the employment rate for people with longer-term mental health problems rose during this period along with the rates for mainstream education and voluntary work.
Service user experience survey
Overall, 128 service users in Merton responded to the question about whether they had received help with finding work in the past 12 months (Fig. 3): 29% said they had received help to gain/retain work, which was significantly more than in the National Patient Survey, 11 where 9% said they had received help to gain work (χ2 = 62.4, d.f. = 1, P>0.001). Further, 7% of service users within the Merton CMHTs and 8% in the National Patient Survey 11 had not received help with finding work but would have liked some (χ2 = 0.345, d.f. = 1, P = NS).
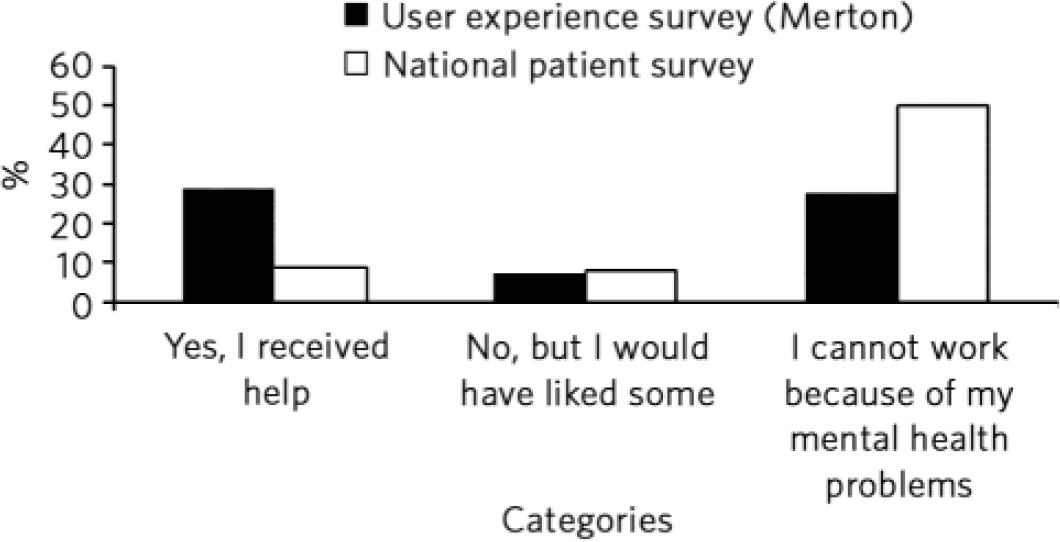
Fig 3 Whether service users had received help with finding work in the past 12-months.
However, a significantly lower proportion of service users in Merton (28%) said they were unable to work because of their mental health problems in comparison with service users in the National Patient Survey (50%) (χ2 = 23.6, d.f. = 1, P>0.001). This would suggest that within the Merton CMHTs, service users had higher expectations about their ability to be able to manage their conditions and gain and retain open employment. Additionally, mental health professionals may have seen open employment as a realistic option for service users and were therefore more actively discussing the possibility of gaining a job and the support that could be offered.
Discussion
The data presented here clearly show that during the 1990s the proportion of people with longer-term mental health problems in open employment significantly decreased in Merton. This effect is comparable with that found in the neighbouring borough of Wandsworth and the potential reasons for this are likely to be similar. Reference Perkins and Rinaldi3 However, the data for the 4-year period from 2003 to 2006 suggest that implementing high-fidelity IPS appears to have had a significant effect on the employment rates of longer-term service users of secondary mental health services in Merton. It is very encouraging that longer-term service users with a diagnosis of schizophrenia also benefited, with the employment rate significantly increasing from 7.8% in 2003 to 15.9% in 2006.
Both the decrease in the employment rates for longer-term service users during the 1990s and then the increasing employment rates from 2003 onwards did not reflect the general employment rate in Merton in the manner that might have been expected. As general employment rates rose, the employment rates for those with longer-term mental health problems decreased and then vice versa. This is consistent with findings in the UK, where local employment rates for people with a diagnosis of schizophrenia have been found to be independent of the development of the general employment rate. Reference Marwaha and Johnson25 However, at a macroeconomic level, general labour market conditions as well as economic disincentives affect the likelihood of people with a diagnosis of schizophrenia finding or maintaining a job. Reference Kilian and Becker26 The finding that the employment rate for mental health service users appears to be independent of the general employment rate especially when the latter was decreasing is intriguing. This is contrary to the general belief that vocational outcomes for people with mental health problems worsen during times of general unemployment and seems to suggest that general unemployment is not necessarily a barrier to employment for users of mental health services. The IPS approach is both a focused and targeted intervention and shows what can be achieved when an intervention is targeted irrespective of societal barriers.
Along with significant increases in employment rates, it appears that by implementing high-fidelity IPS within the CMHTs a higher proportion of service users felt able to return to open employment and a greater proportion of service user demand for help to gain/retain open employment was addressed. Service users’ expectations of being able to return to work were apparently higher (i.e. a smaller proportion believed they were unable to work because of their mental health problems), suggesting that a higher proportion viewed open employment as a realistic and achievable option. This raises important issues in relation to recovery-focused mental health services.
Implementing IPS involves the integration of an employment specialist into a clinical team. The effect of integrating a person whose expertise is helping people to return to work can challenge care coordinator’s own expectations of what service users can achieve in terms of gaining open employment. The literature on client characteristics and vocational success identifies motivation and self-efficacy (wanting a job and believing you can do it) as robust indicators of vocational success Reference Mowbray, Bybee, Harris and McCrohan27-Reference Tsang, Lam, Ng and Leung29 and not factors such as diagnosis, severity of symptoms, social skills or level of impairment. Reference Bond, Resnick, Drake, Xie, McHugo and Bebout30,Reference Catty, Lissouba, White, Becker, Drake and Fioritti31 From a shared decision-making perspective, Reference O'Connor, Wennberg, Legare, Llewellyn-Thomas, Moulton and Sepucha32 the decision to pursue work should be an active choice based on a clear understanding of what the decision means. Therefore, the challenge for care coordinators, in line with the literature, is not to decide who can and who cannot work but how to support all service users to move forward with life beyond their illness and to help them to identify strategies that they find helpful for managing their conditions as they gain and sustain employment.
Study limitations
There are some limitations with this study. First, the cross-sectional survey from 2003 was carried out for 4 years and although the employment rate trend had been positively reversed, it was still some way off of achieving the employment rates found in 1990. Second, due to a major redesign of Merton adult mental health services in 2007 the cross-sectional survey was not carried out and was replaced by the national Public Service Agreement (PSA) 16 target. Reference Treasury33 Third, there was no attempt to independently audit care coordinator returns from the cross-sectional survey for accuracy. However, there were no employment targets during the period of the study and so there was no reason for care coordinators to over-report employment status. Fourth, there was a low response rate to the service user survey without additional testing for non-response effects. Even so, this high non-response rate need not necessarily affect the validity of the data collected. Finally, there is no comparison group within this study and it is possible that the changes in employment rates are the result of many factors other than the introduction of IPS or other factors discussed here. However, these changes in employment rates are not echoed anywhere else in England. 34
In conclusion, this study suggests that at an individual level implementing IPS appears to have a positive effect on service users, with a higher proportion of them feeling able to return to open employment, a smaller proportion believing they were unable to work because of their mental health problems and overall more service users gaining employment. At a CMHT level, it suggests that through implementing IPS mental health professionals may have seen open employment as a realistic option for service users and were therefore more actively discussing the possibility of gaining a job and the support that could be offered. At a local labour market level, this study suggests that local employment rates for people with longer-term mental health problems, including those with a diagnosis of schizophrenia, are independent of the development of the general employment rate.








eLetters
No eLetters have been published for this article.