The number of psychiatric in-patient beds has fallen dramatically in the UK since the 1980s and further rapid reductions with service restructuring are planned in many areas. The impact has been greatest on the long-stay wards with few long-stay beds now available within the National Health Service (NHS) outside forensic settings. The National Service Framework 1 published in 1999 and the NHS Plan 2 of 2000 mandated the setting up of crisis or home treatment teams and early intervention for psychosis teams, alongside already existing assertive outreach teams, in the hope of further reducing the need for hospital admissions.
Introduction of crisis resolution teams and home treatment teams has been associated with a reduction in hospital admissions in some trials, Reference Johnson, Nolan, Hoult, White, Bebbington and Sandor3,Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie4 and between 2001 and 2004 there was a rapid expansion of these teams in England. Reference Glover and Barnes5-Reference Glover and Barnes7 During the same time period a network of assertive community teams was also established. An observational study showed that the introduction of crisis teams was associated with a reduced rate of hospital admissions, but the reduction in occupied bed days was smaller and only statistically significant for older adults of working age. Reference Glover, Arts and Babu8 In contrast, a randomised controlled trial of assertive community teams found no advantage over routine community care in reducing hospital admissions. Reference Killaspy, Kingett, Bebbington, Blizard, Johnson and Nolan9 The PRiSM Psychosis Study also found no difference between intensive and routine community care for people with psychosis, with standard community services producing better outcomes in some domains. Reference Wykes, Leese, Taylor and Phelan10
We analysed the occupancy of NHS beds by people with psychiatric disorders over the last 11 years, using government data. 11 We compared psychiatric disorders with other medical conditions and looked at trends over the past decade. We also examined the length of stay of the major categories of medical and psychiatric disorders.
Method
We examined publicly available data on NHS bed occupancy, provided in the Hospital Episode Statistics produced by the Department of Health. 11 The statistics provide data on the total number of days in which NHS hospital beds are occupied by people with different medical conditions, including psychiatric disorders, in England. We obtained data from 11 financial years between 1998-1999 and 2008-2009. We identified the top ten medical and psychiatric conditions, in terms of the number of bed days occupied in each year of data. The conditions are coded according to broad ICD–10 categories, such as ‘schizophrenia and related disorders’ (F20-F29) and ‘cerebrovascular diseases’ (I60-I69). 12 We examined trends in the total bed days occupied by people within the different categories by constructing graphs.
We examined the mean duration of admission of people with psychiatric disorders, and identified the medical conditions with the highest length of admission for comparison. We also analysed trends in length of hospital stay, using the same methods used to study trends in bed occupancy.
Results
The top ten medical and psychiatric conditions that occupy most NHS beds included the categories of schizophrenia and mood disorders in every year that statistics were examined. Figure 1 shows the trends in bed occupancy over the past 11 years. The proportion of NHS beds occupied by people with psychiatric disorders has remained around 15% throughout the decade. The maximum occupancy was observed in 2004-2005, when those with psychiatric disorders occupied 15.8% of NHS beds. The least was in 2007-2008, when it was 13.7% of the total NHS beds, but it went up again in 2008-2009 to 15.3%. In 2008-2009, people diagnosed with schizophrenia and related disorders occupied a total of 2.85 million bed days, which was higher than any other category of medical or psychiatric disorder. People with mood disorders occupied 1.43 million hospital bed days and mood disorders was the seventh largest diagnostic category in terms of bed occupancy in 2008-2009.

Fig 1 NHS bed days occupied by top medical conditions (millions). Shading highlights the four main diagnoses compared: black – psychiatric, grey – non-psychiatric diagnoses. They are linked together to show how they have been top diagnosed conditions in terms of bed days over the period examined, with some variations in bed days over the years.
Figure 2 presents a comparative look at trends in bed occupancy over the past 11 years, for schizophrenia and mood disorders, with cerebrovascular disease and ischaemic heart disease presented for comparison. Bed days occupied by people diagnosed with schizophrenia have fluctuated, with highest bed occupancy levels over the last year of data from 2008 to 2009. There was a small reduction in bed occupancy by people with mood disorders along with those diagnosed with ischaemic heart disease over the last 4 years of data.
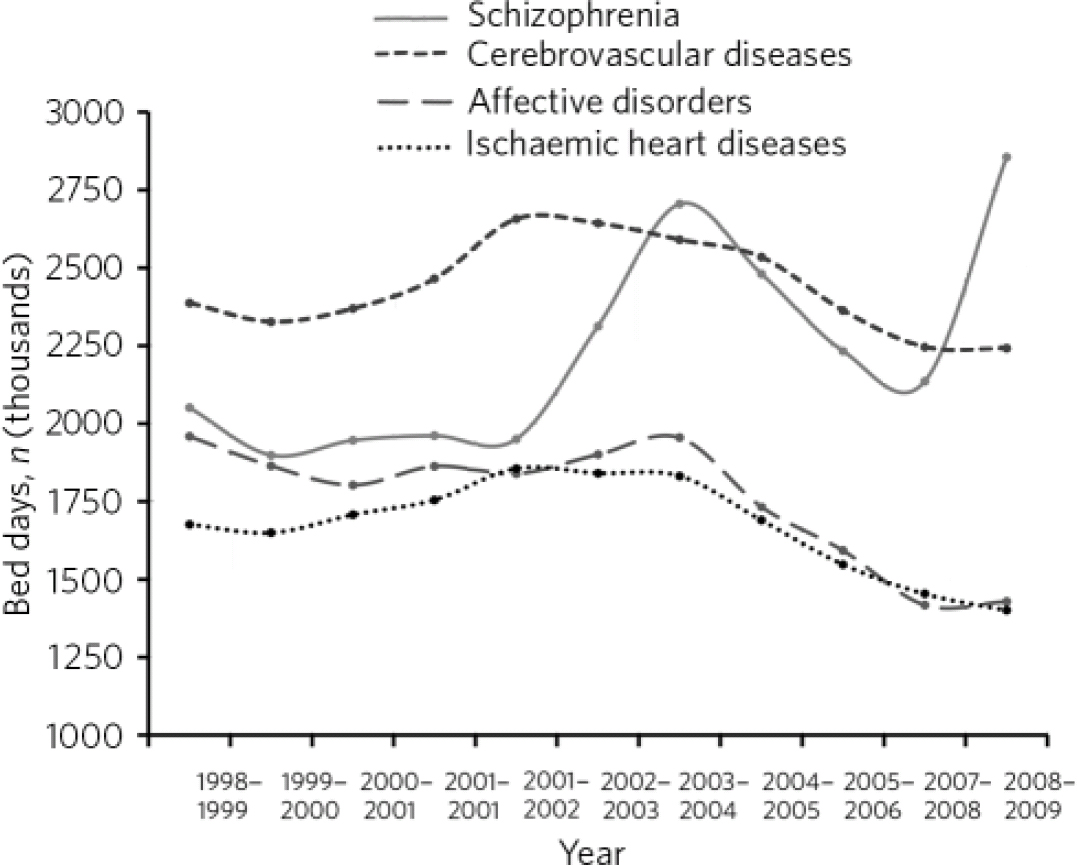
Fig 2 Bed days occupied: top ten psychiatric v. non-psychiatric disorders.
Table 1 shows the mean length of stay in days for the year 2008-2009 and comparative data for the top ten medical conditions that showed the longest duration of admission. Several psychiatric disorders had longer duration of admission than all other medical conditions (Table 1). In 2008-2009, patients with schizophrenia and related disorders had the longest mean duration of hospital stay at 108 days. Patients with mood disorders had a mean length of stay at 42 days. The longest length of stay for any specific non-psychiatric condition in 2008-2009 was for cerebrovascular diseases at 20 days. In the past 11 years, eight of the top ten diagnostic categories in terms of duration of admission were psychiatric disorders. Changes in mean duration of admission for most mental disorders and medical conditions with the longest length of stays such as cerebrovascular disorders, were small, but there was a substantial decline in length of stay for people diagnosed with ‘mental retardation’ (F70-79), from 200 days in 1998-1999 to 104 days in 2008-2009.
Table 1 Mean length of stay in days for the year 2008—2009 for the top ten psychiatric and top ten non-psychiatric disorders (ICD-10 diagnosis)

| Length of stay in days, mean | |
|---|---|
| Top ten psychiatric disorders | |
| Schizophrenia, schizotypal and delusional disorders | 107.7 |
| Mental retardation | 103.6 |
| Dementia | 56.2 |
| Other mental and behavioural disorders | 51.5 |
| Other degenerative diseases (including Alzheimer's disease) | 43.2 |
| Mood (affective) disorders | 42.4 |
| Other organic disorders including symptomatic mental disorders | 26.7 |
| Neurotic, behavioural and personality disorders | 22.9 |
| Mental and behavioural disorders due to psychoactive substances | 7.4 |
| Symptoms and signs including cognition, perception etc. | 6.4 |
| Top ten non-psychiatric disorders | |
| Unknown and unspecified causes of morbidity | 35.2 |
| Injuries to the hip and thigh | 20.5 |
| Cerebrovascular diseases | 20.4 |
| Extrapyramidal and movement disorders (including parkinsonism) | 19.2 |
| Sequelae of injuries of poisoning and other consequences | 17.9 |
| Tuberculosis | 17.1 |
| Inflammatory diseases of the central nervous system | 17.0 |
| Lung disease due to external agents | 16.8 |
| Cerebral palsy and other paralytic syndromes | 15.3 |
| Persons with potential health hazards related to the family | 13.6 |
Discussion
The limitations of our study arise from the limited nature of data available. It was not possible to calculate data by psychiatric specialty or setting, for example, and medical conditions were defined only in broad ICD–10 categories. The data do not differentiate between general acute hospitals and secure settings such as medium secure facilities and special hospitals.
The data also only look at NHS bed occupancy and exclude private hospitals, which are often utilised for long-stay patients. The report from the Care Quality Commission's Count Me In census, shows an increase in the proportion of all mental health in-patients cared for by independent providers rising from 10% in 2005 to 16% in 2009. 13 In October 2000, over a third of secure beds in England were within the independent sector. 14 It has been estimated that 85% of private sector mental health hospital beds are funded by the NHS. 15 Our figures on length of stay therefore exclude a large and growing proportion of individuals who require long-term in-patient care and are therefore likely to underestimate the total bed occupancy of people with severe psychiatric disorders. In spite of these limitations, by taking a comparative look at bed occupancy by individuals with medical and psychiatric disorders, our study demonstrates that, despite the availability of modern treatments, such individuals account for a large proportion of use of NHS beds and have a considerably longer duration of admission compared with those admitted for all other medical conditions. Psychiatric disorders rival cerebrovascular illness, obstetric complications and cardiovascular diseases for the largest in-patient occupancy. Since in-patient costs are the largest component of health service costs, the data indicate that psychiatric conditions, particularly schizophrenia and mood disorders, are some of the most costly disorders to treat in England.
In 2008-2009 the length of stay for people with cerebrovascular diseases, the specific medical condition with longest duration of admission, was less than a quarter of that of schizophrenia. A long duration of bed occupation was also seen in mood disorders, with an average length of admission of around 6 weeks. Duration of admission does not solely reflect the duration of acute symptoms, however, and many psychiatric admissions may be prolonged by the lack of the necessary housing and social support that individuals require in order to leave hospital. One factor that may contribute to the discrepancy between length of stay for medical and psychiatric conditions is the strictures of the Community Care (Delayed Discharges etc.) Act 2003, which enables acute trusts to charge local authorities for the costs of in-patient care for people who have to remain in hospital for social rather than medical reasons, known as ‘delayed discharges’. The Act does not currently cover mental health trusts, but consideration is being given to extend its provisions to the psychiatric sector. However, since the decline in the length of stay for the medical condition with the longest duration was relatively modest over the period studied, it does not appear that the introduction of the Act has had a large impact on the comparison between medical and psychiatric conditions. One recent study suggested that delayed discharge is still prevalent among older adult in-patients, with 37% being classified as having a delayed transfer of care in one area of England. Reference Jasinarachchi, Ibrahim, Keegan, Mathialagan, Mcgouty and Phillips16 National data on mental health in-patients suggest that 9% of people in mental health beds are experiencing a delayed discharge at present. 17
Our findings contrast with a previous study of Hospital Episode Statistics that found a median length of stay of only 28 days for people diagnosed with schizophrenia and psychotic disorders in the fiscal year 1999 to 2000. Reference Thompson, Shaw, Harrison, Ho, Gunnell and Verne18 The median may provide a better estimate of the length of admission of the majority of people, as it is less influenced by those at the higher end of the distribution of length of admission. The median length of stay provided in the Hospital Episode Statistics for the year 2008-2009 was 34 days for schizophrenia and related disorders, a figure in line with Thompson et al's study. Reference Thompson, Shaw, Harrison, Ho, Gunnell and Verne18 However, the contrast between the median and the mean length of stay of 108 days in the current analysis suggests that use of the median underestimates the overall burden of this psychiatric disorder. Using the mean, as we have done, reflects the longer duration of length of stay of people in rehabilitation wards and forensic settings, albeit excluding the increasing numbers of such individuals who are accommodated in the private sector.
Our findings on length of stay are more consistent with the Count Me In government census of the number of in-patients in NHS mental health trusts and independent hospitals, which showed that almost a third of patients (29%) have been in hospital for 1 year or more, and 20% for 2 years. 13 A French census found even longer length of stay in French psychiatric hospitals, with 50% of individuals remaining in hospital for 7 months, 41% for 1 year and 23% for 5 years. Reference Chapireau19 It appears therefore that a large proportion of people with psychiatric disorders cannot be discharged quickly.
The current data provide no evidence that in-patient stays have yet been reduced for people with schizophrenia since the setting up of home treatment teams and early intervention teams as mandated in the NHS Plan of 2000. The small reduction of bed days for people with mood disorders is also not large enough to be confident that it is not simply an artefact. This is despite the fact that reduced spending on NHS in-patient beds has been accompanied by increased spending on the new specialised community services. Reference Goldberg20 Indeed, since there has been a growth in private sector beds over the period of the study, it is likely that bed occupancy by people with severe psychiatric disorders has actually grown over the past decade rather than shrunk.
Despite this situation, pressure to reduce bed occupancy continues, with many mental health trusts reducing bed numbers. The higher than expected use of the supervised community treatment provision of the Mental Health Act 1983 (revised 2007) suggests that coercive treatment in the community may be being used to hasten discharge and prevent readmission. The risks associated with current attempts to reduce in-patient bed use further and their impact on individuals’ lives are yet to be seen.
The data presented here suggest that psychiatric disorders continue to present a significant burden on health service spending, requiring high levels of in-patient care, often for long periods. The aspiration of many mental health trusts to manage all but a small number of people in the community may be hard to achieve. The beneficiaries of any failure in this strategy are likely to be independent sector providers, as the NHS runs down its in-patient provision. Data on bed occupancy, as well as number of beds, in the independent sector are necessary to assess the extent to which in-patient treatment can actually be reduced and the extent to which it is simply provided elsewhere. Achieving lower NHS bed occupancy through a combination of unplanned use of the independent sector, and increasing coercion through the use of supervised community treatment may not be in patients’ or the public's best interests and requires more thorough debate.
Acknowledgement
We thank Dr Robert Blizzard for statistical advice.






eLetters
No eLetters have been published for this article.