Introduction
Hoarding disorder (HD) is a chronic, progressive condition (Grisham et al., Reference Grisham, Frost, Steketee, Kim and Hood2006), defined by excessive acquisition of objects and difficulties with discarding possessions, resulting in an accumulation of clutter (American Psychiatric Association, 2013). Clutter can impair functionality of the home, with many activities of daily living threatened, including cooking, cleaning and personal hygiene (Grisham et al., Reference Grisham, Frost, Steketee, Kim and Hood2006; Kim et al., Reference Kim, Steketee and Frost2001). Clutter also increases health and safety hazards such as falls or fires (Mataix-Cols et al., Reference Mataix-Cols, Frost, Pertusa, Clark, Saxena, Leckman, Stein, Matsunaga and Wilhelm2010; Williams and Viscusi, Reference Williams and Viscusi2016).
Thought to affect between 2 and 5% of the population (Iervolino et al., Reference Iervolino, Perroud, Fullana, Guipponi, Cherkas, Collier and Mataix-Cols2009; Mueller et al., Reference Mueller, Mitchell, Crosby, Glaesmer and de Zwaan2009; Samuels et al., Reference Samuels, Bienvenu, Grados, Cullen, Riddle and Liang2008), HD is reportedly three times more prevalent in older adults compared with younger adults (Hombali et al., Reference Hombali, Sagayadevan, Tan, Chong, Yip, Vaingankar, Chong and Subramaniam2019; Nordsletten et al., Reference Nordsletten, Reichenberg, Hatch, Fernández De La Cruz, Pertusa, Hotopf and Mataix-Cols2013), with age appearing to exacerbate severity of behaviours (Ayers et al., Reference Ayers, Bratiotis, Saxena and Wetherell2012). It must be noted, however, that some research has failed to identify any distinct age or gender differences (Bulli et al., Reference Bulli, Melli, Carraresi, Stopani, Pertusa and Frost2014; Fullana et al., Reference Fullana, Vilagut, Rojas-Farreras, Mataix-Cols, de Graaf, Demyttenaere, Haro, de Girolamo, Lépine, Matschinger and Alonso2010; Nordsletten et al., Reference Nordsletten, Reichenberg, Hatch, Fernández De La Cruz, Pertusa, Hotopf and Mataix-Cols2013; Timpano et al., Reference Timpano, Exner, Glaesmer, Rief, Keshaviah, Brähler and Wilhelm2011). It is possible that the increased rates of hoarding reported in older adults may be due to the disorder being more easily detected in this age group compared with younger counterparts due to the significance of difficulties created by hoarding, with up to 81% of older adults found to be at a physical health risk due to their hoarding behaviours (Kim et al., Reference Kim, Steketee and Frost2001).
Indeed, while the onset of hoarding behaviours typically begin to emerge at a subclinical level during adolescence, these are often not identified as problematic until later in life (Grisham et al., Reference Grisham, Frost, Steketee, Kim and Hood2006; Tolin et al., Reference Tolin, Meunier, Frost and Steketee2010). As such, delayed treatment-seeking is common in this population (Vilaverde et al., Reference Vilaverde, Gonçalves and Morgado2017). The exacerbation of significant hoarding behaviours in middle-aged adults has also been found to coincide with a stressful or traumatic life event (Grisham et al., Reference Grisham, Frost, Steketee, Kim and Hood2006). Indeed, a dose–response relationship between cumulative trauma and severity of hoarding behaviours has been suggested (Landau et al., Reference Landau, Iervolino, Pertusa, Santo, Singh and Mataix-Cols2011; Przeworski et al., Reference Przeworski, Cain and Dunbeck2014), although the literature is not conclusive about the nature of this link (Shaw et al., Reference Shaw, Witcraft and Timpano2016; Tolin et al., Reference Tolin, Meunier, Frost and Steketee2010). When taken together, it could be argued that the higher rates of HD reported in older adults are perhaps more reflective of the progressive nature of the condition, lack of early intervention and impact of stressful or traumatic life events, which result in more clinically significant levels of hoarding behaviours, rather than a later age on onset. Further research is required to explicate the influence of age on the development and/or maintenance of HD. Indeed, greater understanding of the risk and mediating factors for the development of HD, could aid the development of more efficacious evidence-based interventions (Brakoulias and Milicevic, Reference Brakoulias and Milicevic2015; Thompson et al., Reference Thompson, Fernández de la Cruz, Mataix-Cols and Onwumere2017). Given the high personal and societal costs, establishing an effective treatment for HD demonstrates clinical and public health importance (Chou et al., Reference Chou, Tsoh, Shumway, Smith, Chan, Delucchi, Tirch, Gilbert and Mathews2020).
Despite its inclusion in the DSM-V as a distinct condition (American Psychiatric Association, 2013), HD is still encompassed within obsessive compulsive disorder (OCD) in the NICE (National Institute for Health and Care Excellence, 2005) treatment guidelines. Moreover, standard OCD interventions, namely exposure and response prevention (ERP), appear at best to be partially effective in treating HD (Abramowitz et al., Reference Abramowitz, Schwartz, Franklin and Furr2003; Williams and Viscusi, Reference Williams and Viscusi2016). The strongest evidence base for HD thus far is cognitive behavioural therapy (CBT), with key components based on Frost and Hartl’s (Reference Frost and Hartl1996) cognitive behavioural model of HD. Frost and Hartl (Reference Frost and Hartl1996) proposed that HD was a multifaceted disorder emanating from information processing and executive functioning related deficits, emotional attachment difficulties, behavioural avoidance and maladaptive beliefs about objects and the self. These beliefs are associated with intense emotional responses, which in turn reinforce hoarding behaviours (Vilaverde et al., Reference Vilaverde, Gonçalves and Morgado2017). For instance, emotions such as anxiety or shame fuel an avoidance of discarding objects (Chou et al., Reference Chou, Tsoh, Vigil, Bain, Uhm, Howell, Chan, Eckfield, Plumadore, Chan, Komaiko, Smith, Franklin, Vega, Delucchi and Mathews2018), while joy or pride reinforce decisions to acquire or save items (Steketee and Frost, Reference Steketee and Frost2003). This high degree of emotional attachment to possessions has been consistently noted across other models of HD (e.g. Gordon et al., Reference Gordon, Salkovskis and Oldfield2013; Seaman et al., Reference Seaman, Oldfield, Gordon and Forrester2010), with a suggestion that this attachment may reflect a lack of emotional connection to other individuals or function as a replacement for interpersonal contact (Tolin et al., Reference Tolin, Frost and Steketee2007). As such, there appears to be a range of cognitive, emotional and social factors that play a role in the maintenance of HD and thus represent the focus of intervention. Critically, however, while CBT for HD demonstrates effectiveness in alleviating symptom severity in both individual and group format (Mathews et al., Reference Mathews, Mackin, Chou, Uhm, Bain, Stark, Gause, Vigil, Franklin, Salazar, Plumadore, Smith, Komaiko, Howell, Vega, Chan, Eckfield, Tsoh and Delucchi2018; Thompson et al., Reference Thompson, Fernández de la Cruz, Mataix-Cols and Onwumere2017; Tolin et al., Reference Tolin, Frost, Steketee and Muroff2015), only one third of individuals achieve clinically significant improvement (Muroff et al., Reference Muroff, Steketee, Bratiotis and Ross2012; Steketee et al., Reference Steketee, Frost, Tolin, Rasmussen and Brown2010). These findings suggest there may be aspects of HD in this population which may not be sufficiently targeted by CBT (Chou et al., Reference Chou, Tsoh, Shumway, Smith, Chan, Delucchi, Tirch, Gilbert and Mathews2020). Additionally, CBT outcomes for older adults with HD have also been limited (e.g. Ayers et al., Reference Ayers, Wetherell, Golshan and Saxena2011), although it has been questioned whether difficulties with age-related neurocognitive impairment may be associated with this poorer response to CBT, as noted in other older adult populations (Mohlman and Gorman, Reference Mohlman and Gorman2005). Indeed, cognitive rehabilitative training, alongside behavioural exposure, has been found to produce positive results in older adults with HD (Ayers et al., Reference Ayers, Bratiotis, Saxena and Wetherell2012).
The evidence base on the effectiveness of remote-CBT interventions for HD in older adults is also limited. Preliminary research by Muroff and Steketee (Reference Muroff and Steketee2018) found that remote-CBT interventions for HD, delivered via video-conferencing software, demonstrated encouraging levels of acceptability and feasibility. More recently, Ong and colleagues (Reference Ong, Krafft, Panoussi, Petersen, Levin and Twohig2021) used video-conferencing software to trial a remote acceptance and commitment therapy intervention for HD with promising findings of its effectiveness compared with in-person intervention. It is also worth noting the greater intervention outcomes produced by CBT interventions for HD when supplemented with online support between sessions (Ivanov et al., Reference Ivanov, Enander, Mataix-Cols, Serlachius, Månsson, Andersson, Flygare, Tolin and Rück2018).
However, a more robust evidence base is required, particularly when considering the ongoing need presented by the COVID-19 pandemic to engage in therapeutic work remotely and the potential opportunity to increase access to evidence-based intervention. This case study presents an account of a remote-CBT intervention for HD in an older adult, demonstrating the challenges, strengths and overall effectiveness of this approach.
Presenting problem
Mary (a pseudonym) was a female in her mid-60s, referred to an adult mental health service by her General Practitioner for psychological input, due to ongoing difficulties with anxiety, low mood and ‘clutter’, which were having a significant impact on her personal, social and occupational functioning and overall quality of life (QOL).
A detailed assessment occurred across three sessions. This involved clinical interviews and a number of self-report psychometric measures to explore factors maintaining these hoarding behaviours. Mary described excessive acquisition of objects and experienced distress when thinking about discarding items, even when broken or unneeded. This purposeful saving of items resulted in emotional distress, functional impairment and reduced QOL. Mary met DSM-V (American Psychiatric Association, 2013) criteria for HD.
Mary’s parents were described as being prudent with their money, and as a result were frugal and resourceful, teaching her from a young age it was wrong to waste. She experienced a close relationship with her father, but spoke of a difficult relationship with her mother who held her to often-unattainable standards. When Mary could not meet these expectations, her mother’s response was excessively critical, leaving her feeling she could never please her mother. Mary recalled enjoying shopping for clothes and shoes at this time, which she would use to express herself. This resulted in her wardrobe always being ‘full’, but she never felt it was a problem until about 10 years ago. Mary reported a period of significant difficulty with anxiety and low mood when she was teenager, which she has also experienced intermittently throughout life.
Mary shared that her mother and father have now passed, with the death of the latter occurring approximately 10 years ago. Mary noted that boxes, many of which were storing items from her late parents’ house, were stacked in each room of her house, with surfaces also cluttered with paper and miscellaneous items. The clutter had impaired Mary’s ability to use living spaces as intended, citing a difficulty navigating safely around the house or locating possessions. A number of home appliances had stopped working over the past 18 months and the embarrassment and shame associated with clutter in her home, meant Mary felt uncomfortable allowing service-people in to fix these faults. This restriction of access also extended to family and friends, contributing to her level of social isolation. Mary described feeling sad, irritable and lonely and had stopped interacting with peers or engaging with previous activities of interest as she got older, relating to age-related beliefs she had about what was appropriate as she became older. At this point, Mary was engaged in full-time employment, but was aware of her impending retirement in the coming years and the significant transition this would represent. Mary’s physical health had also started to decline and the impact of this was beginning to hinder her mobility. Mary was not currently engaged in any romantic relationships and lived alone. While Mary had one younger sibling who lived abroad, she reported a distant relationship with him which involved little communication, and did not note interactions with any other family members.
Mary identified intervention goals of better understanding her difficulties with hoarding, and through clutter reduction, allowing for broken appliances in her home to be repaired.
Outcome measures
The following represent the main outcome measures upon which intervention progress was evaluated:
Hoarding Rating Scale (HRS; Tolin et al., 2008; Tolin et al., 2010)
The HRS is a brief measure assessing the main characteristics of HD. Mary scored 31 at baseline, which is above average for individuals with HD.
Clutter Image Rating (CIR; Frost et al., 2008)
The CIR allows for standardised evaluations of clutter, with service-users selecting from a series of images depicting various levels of clutter, the image which is most reflective of their house. Mary scored highly on her clutter rating in the living room (5), kitchen (5), dining room (6) and spare bedroom (7).
CORE-OM (Evans et al., 2000)
The CORE-OM is a 34-item measure of general psychological wellbeing and distress. It assesses domains of wellbeing, problems and symptoms, functioning and risk. Mary’s score on the CORE-OM demonstrated she was experiencing severe psychological distress (85).
Work and Social Adjustment Scale (WSAS; Mundt et al., 2002)
The WSAS measures impairment in functioning across five domains, namely work, home-management, social leisure activities, private leisure activities and family/relationships. Mary scored 30 (severe), with difficulties across all domains.
The following outcome measures were used for information-gathering purposes:
Savings Inventory-Revised (SI-R; Muroff et al., 2014)
The SI-R examines features of compulsive hoarding, including acquisition, discarding and clutter. Mary exhibited strong features across all domains of the SI-R.
Saving Cognitions Inventory (SCI; Steketee et al., 2003)
The SCI explores beliefs and attitudes relating to attachment to items, including emotional attachment, responsibility, memory and control. Mary’s responses indicate maladaptive beliefs of emotional attachment, responsibility, and control of items.
Formulation
In line with Steketee and Frost’s (Reference Steketee and Frost2014) CBT model of HD, an adapted hoarding-specific formulation was developed and used to guide intervention (see Fig. 1). Maintenance cycles of specific hoarding incidents (Steketee and Frost, Reference Steketee and Frost2014) were developed during sessions to guide learning (see Figs 2 and 3). Whilst absent from the HD model, it is important to acknowledge Mary’s many protective factors, including her joy for her animals, her openness to engaging in psychological intervention and her willingness to engage in reflective activities and develop greater self- and other-oriented insight.

Figure 1. Diagrammatic formulation.
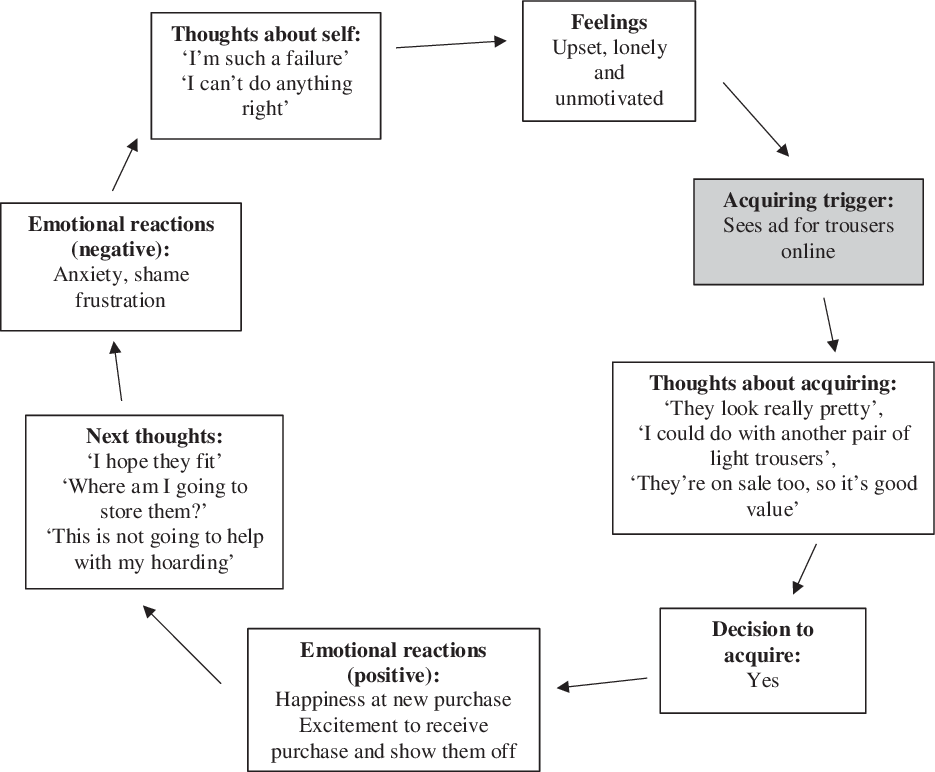
Figure 2. Maintenance cycle of acquiring episode.

Figure 3. Maintenance cycle of discarding episode.
A number of personal and family factors, relating to her early experiences and core beliefs, may have increased Mary’s vulnerability to developing HD. Whilst the frugality of her parents and their emphasis on not wasting can be seen as contextually appropriate, Mary’s perception of these experiences appear to have bestowed a vulnerability to the development of a number of core beliefs and the negative nature of her cognitive appraisals. More specifically, the difficult dynamic in her relationship with her mother and the high standards she set for her, appears to have influenced Mary’s self-esteem and beliefs about herself, as indicated by the development of a number of core beliefs relating to worthlessness and being a failure. These have intensified over the years, fuelling perfectionistic and self-critical thought patterns, which are common in HD (Plimpton et al., Reference Plimpton, Frost, Abbey and Dorer2009). The combination of these factors likely contributes to the beliefs Mary holds about objects and about herself, particularly when considering the inter-generational linkages and interactions with cohort beliefs and those relating to family structures, roles and responsibilities (Evans, Reference Evans2007). The impact of her current declining physical health and her health history may also be pertinent, with research identifying high levels of co-morbidity between HD, depression and anxiety (Ayers et al., Reference Ayers, Dozier, Pachana and Oude Voshaar2015).
The exacerbation of Mary’s hoarding behaviours over the past 10 years appears to coincide with the loss of a parent. As research indicates the exacerbation of hoarding behaviours in adults may be related to stressful or traumatic events (Grisham et al., Reference Grisham, Frost, Steketee, Kim and Hood2006), it is possible these experiences increased Mary’s level of vulnerability to HD. This must be considered from an older-age perspective and through the lens of Thompson’s (Reference Thompson1996) identified themes of ‘loss and transition points’, which often precipitate an older adult’s presentation for psychological support. In this sense, the loss experienced by Mary, in terms of the loss of parental relationships, the loss of control relating to ageing and her physical health and strength alongside the transition she is experiencing in relation to her life stage and age, may also be prominent when considering her presentation.
In relation to information processing, Mary reported perceived difficulties with decision-making, organisation, concentration and memory, which is consistent with research identifying sub-clinical deficits in information processing in HD populations (Grisham et al., Reference Grisham, Brown, Savage, Steketee and Barlow2007; Samuels et al., Reference Samuels, Bienvenu, Pinto, Fyer, McCracken, Rauch, Murphy, Grados, Greenberg, Knowles, Piacentini, Cannistraro, Cullen, Riddle, Rasmussen, Pauls, Willour, Shugart, Yee and Nestadt2007). Research has identified greater levels of executive dysfunction in older adults with HD, particularly in areas of mental control, working memory, inhibition and set shifting (Ayers et al., Reference Ayers, Wetherall, Schiehser, Almklov, Golshan and Saxena2013). These difficulties influence Mary’s beliefs about the meaning of items, and impact her ability to categorise, organise or discard possessions (Grisham and Norberg, Reference Grisham and Norberg2010). It is possible these difficulties are perpetuated by her level of anxiety and low mood. Moreover, research (Hartl et al., Reference Hartl, Frost, Allen, Deckersbach, Steketee, Duffany and Savage2004) indicates these difficulties are more often better explained by deficits in confidence rather than ability. Indeed, while the ability to conduct a formal assessment of cognition was constrained, therapeutic exercises revealed that Mary appeared to under-estimate her memory and cognitive abilities.
Mary identified maladaptive beliefs relating to items, largely pertaining to her perceived sense of responsibility for objects, the beauty and utility of possessions, and the safety these items provided. Mary’s also viewed items as memory cues, probably related to her poor confidence in her memory (Steketee et al., Reference Steketee, Frost and Kyrios2003). These beliefs elicited what was perceived as positive and negative emotional reactions for Mary. These include joy from buying a new possession and the social encounter this affords, and happiness at the memories items may remind her of. Mary also reported guilt at the thought of discarding items that meant a lot to her parents or that could be re-used.
Mary’s emotional responses to items and associated appraisals functioned to maintain her hoarding behaviours. For instance, positive emotional reactions experienced when purchasing an item served to reinforce her acquiring habits. Similarly, the joy experienced when thinking about possessions increased her likelihood of saving items, thus further positively reinforcing her hoarding behaviours. On the other hand, distressing emotions such as guilt, shame or anxiety associated with thoughts of discarding items, fuelled an avoidance of discarding objects, thus Mary continued saving. Mary’s avoidance of uncomfortable feelings ultimately negatively reinforced her hoarding behaviours. The resultant behaviours of excessive acquisition and saving of possessions, resulted in the accumulation of significant clutter, which subsequently influenced her beliefs about the meaning of items and of herself.
Course of therapy
Mary consented to individual psychological intervention, guided by a CBT approach. The therapist was a trainee clinical psychologist, under the supervision of a specialist clinical psychologist. An intervention plan was developed with consideration of her formulation, and Mary engaged in 26 weekly CBT sessions, as recommended by Steketee and Frost (Reference Steketee and Frost2014). Due to the onset of the COVID-19 pandemic early on in the course of intervention, a remote-working approach was adopted with the remaining 18 of these sessions conducted via telephone. However, Mary quickly adapted to remote therapy with minimal interruption or difficulty, reportedly finding it more accessible.
In line with common adaptations for CBT interventions with older adults (Chand and Grossberg, Reference Chand and Grossberg2013), information was presented slowly with frequent repetitions and summaries. Worksheets and key session notes were provided in written format prior to each session, and Mary was offered the opportunity to record important pieces of information to listen to between sessions as reminders. Additionally, it was decided that at the end of each session, a short summary of the main points covered and the between-session tasks would be collaboratively developed and provided to Mary. The use of telephone prompts, through alarms and reminders to engage with exercises and between-session tasks, was also found beneficial. Mary was encouraged to keep notes during the week of her practice and any questions that arose, which could then be addressed during the session. Mary reportedly found these adaptations helpful for recalling the content covered in sessions and engaging with the material outside of a therapeutic context.
Each session began with a check-in, collaborative agenda-setting, a review of between-session tasks and new content. The main components of this intervention involved psychoeducation, motivation enhancement, skills work, cognitive restructuring and behavioural intervention.
Psychoeducation was ongoing throughout intervention, and significant time was spent developing a shared understanding of Mary’s experiences of hoarding, through Steketee and Frost’s (Reference Steketee and Frost2014) model. A process of guided discovery (Westbrook et al., Reference Westbrook, Kennerley and Kirk2016) allowed for reformulation and adjustment of the intervention plan as needed throughout. Basic principles of CBT were discussed such as the interactive nature of cognitions, emotions and behavioural responses and the value of behavioural activation. Psychoeducation about maladaptive beliefs and the futility of safety behaviours also proved advantageous.
Motivational enhancement is consistently noted as a key component in facilitating change in individuals with HD (Mathews et al., Reference Mathews, Mackin, Chou, Uhm, Bain, Stark, Gause, Vigil, Franklin, Salazar, Plumadore, Smith, Komaiko, Howell, Vega, Chan, Eckfield, Tsoh and Delucchi2018). Thus, the use of goal-setting, decisional-balance and visualisation exercises were used to better understand Mary’s motivations for engaging in intervention. These also served as reminders of the value of change when facing challenging periods throughout intervention.
An important component of Mary’s intervention involved reducing her level of acquisition. Developing maintenance cycles of recent acquisitions allowed us explore how these could be understood in terms of Mary’s formulation. A number of strategies were used to help Mary practise non-acquiring, such as generating questions and rules she had to satisfy before acquiring a new possession, identifying the advantages and disadvantages of acquiring that item and evaluating her need versus want for the item. Typically, graded exposure to practise non-acquiring skills in various settings is conducted, but the onset of strict COVID19 restrictions and remote working proscribed this. Practice was conducted during essential shopping trips and online shopping settings.
A period of skills training ensued which aimed to target Mary’s difficulties with decision-making, organisation and problem-solving (Williams and Viscusi, Reference Williams and Viscusi2016). This was framed as a period of preparation for reducing clutter. As Mary often struggled to remember between-session tasks, she found utilising to-do lists helped her keep track of tasks she wanted to complete. Not only did this increase her level of engagement with the intervention, it also enhanced her confidence in her information-processing abilities. This provided further opportunity to challenge Mary’s beliefs about herself and her information-processing abilities, as in line with a CBT model of HD, difficulties in these areas are often better explained by deficits in confidence rather than function (Hartl et al., Reference Hartl, Frost, Allen, Deckersbach, Steketee, Duffany and Savage2004).
Making decisions about saving and discarding items represented a critical intervention phase, consisting of decision-making exercises and graded exposure tasks to practise discarding items, while targeting avoidant safety behaviours. Mary acknowledged feeling overwhelmed at the thought of beginning to declutter, but her anxiety reportedly decreased when breaking it down into small, manageable tasks. We also agreed a plan for Mary if she became overwhelmed, such as engaging in mindfulness-based exercises or self-soothing, such as petting her dog. The decision was made to pick one area within the house that Mary could focus her efforts on de-cluttering, with the skills learnt during this time then generalised to other areas around the house. Mary began by choosing objects that were ‘easier’ from an exposure hierarchy to practise discarding in-session. This allowed for direct support and coaching through any barriers which arose. Imaginal exposure tasks were used for items which were placed higher up on Mary’s hierarchy list, to explore what would happen if she exposed herself to distressing thoughts and feelings associated with discarding items. Similar to strategies for non-acquiring, Mary found generating questions to ask herself when deciding whether to discard an item, to be helpful. Through behavioural experiments, Mary began testing her beliefs about what would happen if she discarded items which held great personal value or significance.
Cognitive restructuring, used to address Mary’s unhelpful beliefs and thought patterns, was one of the most influential strategies encompassed in this HD intervention. This highlighted the importance of appraisals, beliefs and cognitions in maintaining hoarding behaviours in this disorder. Some unhelpful thinking styles which Mary could relate to included jumping to conclusions, catastrophising, discounting the positive and moral reasoning. The use of thought record forms encouraged Mary to challenge these thoughts and to gather evidence against her rationale for hoarding. Using the downward arrow strategy, Mary identified a core belief of worthlessness, which also resulted in the attribution of the critical voice in her head to that of her mother while she was younger. This allowed Mary to better understand the perfectionistic and self-critical thoughts she experienced and cultivated greater insight into her difficulties. Mary found the process of acknowledging and externalising these thoughts (e.g. ‘That’s just “Negative Nelly” talking’) afforded reduced distress and greater ability to challenge this unhelpful style of thinking, rather than engaging in rumination or thought suppression, which were her previous automatic responses. Over time, Mary began to recognise the persistent nature of these self-critical and perfectionistic thoughts and appreciated the likely need for continued practice in challenging these going forward.
Relapse management represented an important intervention phase for Mary, allowing her to review the skills she had developed and how these fit within her initial formulation. It was important to identify any challenges which might arise or stressors which might trigger urges to hoard and how these could be managed (Williams and Viscusi, Reference Williams and Viscusi2016). A collaborative planning process explored how Mary could continue this work independently. The preparation for ending was an important feature of this intervention, particularly when considering of the length of intervention and strength of the therapeutic relationship. As such, markers for sessions remaining were provided intermittently and beliefs around what ending therapy might mean for Mary were discussed.
A number of challenges arose throughout the course of this intervention, including the onset of the COVID-19 pandemic, which necessitated a remote approach. This precluded the ability to conduct home visits or complete graded exposure exercises for non-acquiring. It is recommended that at least one, but up to 25% of sessions are conducted in service-users’ homes for maximum progress in clutter reduction (Mataix-Cols et al., Reference Mataix-Cols, Billotti, Fernández De La Cruz and Nordsletten2013; Steketee and Frost, Reference Steketee and Frost2014). This is probably due to the increased opportunity to practise sorting skills in the most challenging context, with the therapist providing accountability to ensure commitment and adherence to tasks and for extra-therapeutic factors, namely support, guidance and empathic feedback from the therapist (Fitzpatrick et al., Reference Fitzpatrick, Nedeljkovic, Abbott, Kyrios and Moulding2018). Additionally, as Mary did not have access to video technologies in her home, this confined therapeutic engagement to telephone only. These represented significant challenges in this work, as despite the gains made in Mary’s recovery, it is feasible that she might have experienced greater improvements in clutter reduction if home visits or engagement through video technologies were possible. Broadly speaking, the potential for remote-CBT delivered via video therapy to increase the effectiveness of CBT interventions for HD must be considered, due to the distinct advantage video therapy presents in affording greater opportunities to access and thus practise skills in the home environment.
Moreover, the impact of isolation and social distancing as a result of COVID-19 restrictions on Mary’s general mental health and her mood in particular, also created significant difficulty. While this was discussed and normalised in the current context, it nevertheless complicated progress through a number of intervention phases, which had a contagion effect on Mary’s levels of motivation, both due to the low mood she was experiencing and also her perceived lack of ‘real’ progress. Renewed use of motivational interviewing techniques included visualisation to encourage Mary to visualise what she wanted her home to look like and devising strategies to allow her to track her progress in a more tangible manner. These appeared to be beneficial in improving her level of motivation and engagement. It was hoped that by increasing Mary’s level of motivation, she might experience a mood-enhancing effect upon seeing continuing levels of progress.
The strength of the therapeutic relationship represented both a strength and a challenge throughout intervention. The therapeutic relationship has been cited as one of the most influential factors in HD intervention outcomes, from both a therapist and service-user perspective (Ayers et al., Reference Ayers, Bratiotis, Saxena and Wetherell2012). As typically the shame associated with HD makes individuals reluctant to share the extent of their hoarding behaviours (Millen et al., Reference Millen, Linkovski, Dunn and Rodriguez2017), the importance of extra-therapeutic factors in intervention was illuminated. However, it became apparent that Mary was becoming attached to her role in therapy and the support of her therapist. The greater dependence on the therapeutic relationship can also be considered from an age perspective in relation to the feelings of loneliness reported by Mary, as a result of the loss of important people in her life (Evans, Reference Evans2007). Through the use of supervision, and reflecting on her formulation, whereby Mary experienced attachment towards items which might provide comfort or safety, it was understandable that she might experience the ‘discarding’ of her therapist and her role in therapy to be difficult. This was explored with Mary, who subsequently acknowledged her fear of completing intervention. This reflects the importance of addressing boundaries and dependency in the therapeutic relationship when working with this presentation.
Outcome
In relation to the main progress indicators, such as the HRS, Mary reported a 22.6% improvement in scores at the end of intervention (see Table 1). This is in line with previous literature, reporting up to 25–30% reductions in HRS scores following face-to-face interventions (Muroff et al., Reference Muroff, Steketee, Bratiotis and Ross2012; Steketee et al., Reference Steketee, Frost, Tolin, Rasmussen and Brown2010). It is significant to note that by the end of intervention, Mary’s level of acquisition was no longer excessive and she was making progress in sorting through her possessions, reporting great improvements in the level of clutter in her home. This is supported by her post-intervention scores on the CIR, whereby she reported marked improvements in eight of nine categories and a stable score in the remaining category.
Table 1. An overview of main pre- and post-intervention scores on general and hoarding-specific outcome measures

Overall, Mary reported less distress, greater social involvement with peers and her community, and increased motivation to engage in clutter reduction. These represent marked improvements from her initial presentation. These are also supported by her scores on measures of general psychological wellbeing (CORE-OM) and impairment of daily functioning (WSAS) which were completed at assessment and following completion of her intervention. Mary’s scores on the CORE-OM reduced from ‘severe’ to ‘moderate’, representing reliable change (Evans et al., Reference Evans, Mellor-Clark, Margison, Barkham, Audin, Connell and McGrath2000). While these intervention outcomes could be deemed modest, smaller effects on low mood following HD interventions are often observed, due to the anxiety-provoking nature of intervention itself (Timpano et al., Reference Timpano, Exner, Glaesmer, Rief, Keshaviah, Brähler and Wilhelm2011). Similarly, Mary demonstrated a reduction on scores on the WSAS from the ‘severe’ to the ‘moderate’ category. It is noted, however, that the moderate level of impairment reported by the WSAS was probably biased by ongoing COVID-19 restrictions, with Mary self-reporting her responses were determined more by these rather than direct impacts of her hoarding. Therefore, it is likely that greater reductions would have been observed in this regard for Mary, were it not for COVID-19 restrictions.
Discussion
This research presents a number of treatment implications going forward, particularly in the application and effectiveness of a remote-CBT intervention for HD in older female adults. Whilst perhaps requiring more time and creativity, this case report finds that remote-CBT interventions for HD appear at least as effective as face-to-face CBT interventions in reducing the frequency and intensity of clinically significant hoarding behaviours and their resultant impact on QOL. This is demonstrated by the reductions noted on the HRS, CIR and measures of general psychological wellbeing.
Despite the significant reduction observed in measures of general hoarding behaviours and psychological wellbeing, an increase of scores across SI-R and SCI categories was observed post-intervention. Similar findings were reported in a case study by Farquhar and Caiazza (Reference Farquhar and Caiazza2020) whereby increases in scores on the SI-R were noted post intervention, despite significant reductions in hoarding behaviours and low mood, which were consistent with subjective reports. This is interesting, as it would be expected that a decline in characteristics related to hoarding, and thus scores across all measures, would occur following intervention. One explanation which holds pertinency in this instance relates to the post-intervention administration procedure of these two measures, which, due to running out of time in the clinical session, were given to the client to complete independently at home without sufficient guidance or instructions. This is particularly of relevance to the SI-R which could be perceived as challenging due to the level of cognitive-switching required, with individuals presented with four interchanging rating scales within the space of 23 questions. This is in contrast to the pre-intervention measures, and indeed other post-intervention measures including the HRS, CIR, CORE-OM and WSAS, which were administered in a verbal fashion, with the therapist calling out questions and possible responses, and inputting the correct rating on behalf of the client. This may account for the disparity in scores on these measures. It is noted that previous studies exploring the use of these measures with older adult populations have appeared to rely on verbal administration, rather than client self-report (e.g. Frost et al., Reference Frost, Steketee and Grisham2004). Additionally, there are no published norms for older adults on these measures, despite previous research indicating a different measure structure in older adults compared with their younger counterparts (Ayers et al., Reference Ayers, Dozier, Twamley, Saxena, Granholm, Mayes and Wetherell2018). As the client and therapist subjective reports are more in line with outcomes identified on the HRS and CIR in this report, and due to the potentially unreliable administration of the SCI and SI-R, it is suggested that these latter scores are interpreted with these caveats in mind.
While progress on hoarding-specific measures appear auspicious for a remote intervention in line with previous reports on face-to-face interventions (Steketee et al., Reference Steketee, Frost, Wincze, Greene and Douglass2000), they nevertheless indicate remaining functional impairment as a result of hoarding. However, greater rates of recovery are typically noted in cases of early intervention (Tolin et al., Reference Tolin, Frost, Steketee, Gray and Fitch2008), and as Mary exhibited significant hoarding behaviours for at least 8–10 years prior to seeking help, this may culminate in a slower rate of recovery. In addition to delayed treatment-seeking, Mary’s older age may also be relevant, as the process of restructuring these hoarding-related cognitions in older adults is thought to require longer and more intensive input compared with their younger counterparts, probably due to the strength of these cognitive beliefs which have been reinforced over years (Chand and Grossberg, Reference Chand and Grossberg2013). Furthermore, if complemented with home visits as recommended in the literature (Steketee and Frost, Reference Steketee and Frost2014), or delivered with the use of video technologies, it is plausible that outcomes from remote-CBT interventions might demonstrate similar, if not greater reductions in hoarding behaviours and functional impairment and increased QOL, due to increased levels of access to the cluttered environment.
Moreover, it is interesting that despite outcome measures indicating Mary demonstrated just 22.6% improvement in hoarding-related behaviours, Mary’s own subjective report indicates marked improvements compared with her initial presentation. Indeed, this appears to echo previous research whereby when asked to rate their own subjective progress, 76% of service-users typically report their behaviours as improved (Steketee et al., Reference Steketee, Frost, Tolin, Rasmussen and Brown2010), yet when measured by standard outcome measures, only 30% appear to achieve clinically significant change (Muroff et al., Reference Muroff, Steketee, Bratiotis and Ross2012). This highlights the importance of taking an integrative approach to measuring progress within HD populations, where progress is not only fixated on the complete eradication of clutter, but incorporates goals, skill-development, QOL, reduction of distress and functional impairment.
Whilst demonstrating promise, it is clear, however, that CBT interventions for HD are in their nascency, and continued efforts are required to develop maximally effective interventions. Indeed, while there is burgeoning evidence as to the effectiveness of a CBT intervention for HD, an augmented account of the mechanisms through which these outcomes are achieved is required. Gaining a more nuanced understanding of the various mechanisms of change in CBT for HD will allow for greater tailoring of the intervention to suit the unique presentation of service-users. Of note, complementing standard CBT for HD with clinician support between sessions has been found to produce larger effect sizes, which are maintained 3 months following treatment completion (Ivanov et al., Reference Ivanov, Enander, Mataix-Cols, Serlachius, Månsson, Andersson, Flygare, Tolin and Rück2018). It is likely this between-session support could also address some barriers to engagement in remote-CBT interventions for HD, through enhancing motivation, support in completing homework tasks, providing memory aids and delivering further individualised feedback (Aguilera and Muench, Reference Aguilera and Muench2012). Additionally, if delivering a HD intervention remotely, it may be advantageous to encourage the use of a friend or family member to act as a coach or a ‘buddy’ throughout the intervention to provide support, both practical and emotional, to the service-user in carrying out between-session tasks. This will also allow for a smoother transition in the client becoming their own therapist following completion of formal psychological intervention (Steketee and Frost, Reference Steketee and Frost2014). This is consistent with standard adaptations to CBT whilst working with older adults, where involvement from significant others appears to support therapeutic engagement (Spector et al., Reference Spector, Charlesworth, King, Lattimer, Sadek, Marston, Rehill, Hoe, Qazi, Knapp and Orrell2015).
It appears, however, that the chronicity of HD may necessitate ongoing therapeutic support for skill refreshment to ensure continued clutter reduction, particularly in older adults (Ayers et al., Reference Ayers, Wetherell, Golshan and Saxena2011; Fitzpatrick et al., Reference Fitzpatrick, Nedeljkovic, Abbott, Kyrios and Moulding2018). It is possible older-adult presentations may be responsive to more intensive forms of intervention, with research indicating that greater outcomes were achieved in this population when they engaged in multiple sessions a week when compared with weekly sessions (Saxena et al., Reference Saxena, Maidment, Vapnik, Golden, Rishwain, Rosen, Tarlow and Bystritsky2002). However, further research would need to assess the cost- and time-effectiveness of this, along with acceptability to service-users.
The inclusion of motivational enhancement strategies were found to be particularly beneficial in eliciting greater levels of change talk and self-efficacy from Mary, through the use of goal setting and visualisation, along with standard motivational interviewing techniques, such as open-ended questioning, affirming, reflecting and summarising. As such, it is notable that there is not greater emphasis in Steketee and Frost’s (Reference Steketee and Frost2014) model for enhancing motivation. This is pivotal as research indicates that Mary, as an older adult living alone, is more likely to experience greater difficulties with motivation throughout HD interventions (Samuels et al., Reference Samuels, Bienvenu, Grados, Cullen, Riddle and Liang2008) and perhaps more so if engaging remotely. The inclusion of additional motivational enhancement techniques could question model fidelity, but the rationale for incorporating these appears justified in line with research (Simpson and Zuckoff, Reference Simpson and Zuckoff2011) to ensure sufficient engagement with intervention within this population. The significance of beliefs and cognitive appraisals in the maintenance of hoarding behaviours must also be considered, particularly, as observed in this case report, insight into the origin of unhelpful thinking patterns and the introduction of cognitive restructuring appear to elicit significant behaviour change. It is therefore conceivable that this model might benefit from more extensively highlighting these factors throughout both formulation and intervention to achieve maximum intervention success. This is in line with previous cognitive models highlighted by Seaman and colleagues (Reference Seaman, Oldfield, Gordon and Forrester2010) and Gordon and colleagues (Reference Gordon, Salkovskis and Oldfield2013), which identified the significance of key cognitions in the maintenance of HD, including harm avoidance and emotional attachments to objects. If these appear pertinent, clinicians should also consider the evidence base of ERP (Abramowitz et al., Reference Abramowitz, Schwartz, Franklin and Furr2003; Williams and Viscusi, Reference Williams and Viscusi2016) for HD, if this appears to be a more appropriate or fitting intervention, guided by a client’s formulation and presenting difficulties.
It has also been suggested that incorporating aspects of a compassion-focused approach to CBT for HD may improve the high levels of self-criticism and perfectionistic traits commonly observed in individuals with HD (Chou et al., Reference Chou, Tsoh, Shumway, Smith, Chan, Delucchi, Tirch, Gilbert and Mathews2020). This may be particularly beneficial for individuals like Mary, whose progress was probably moderated by unrelenting standards for herself, low self-esteem and high levels of shame. Additionally, as standard CBT interventions for HD do not appear wholly effective for addressing low mood in individuals with HD, this highlights a role for the inclusion of further emotional regulation strategies, to support individuals presenting with co-morbid anxiety and low mood (Fitzpatrick et al., Reference Fitzpatrick, Nedeljkovic, Abbott, Kyrios and Moulding2018). Moreover, integrating elements from other therapeutic interventions, such as Ayers and colleagues’ (Reference Ayers, Bratiotis, Saxena and Wetherell2012) cognitive rehabilitation and exposure/sorting therapy, which targets executive dysfunction through compensatory cognitive training, should be considered where significant neurocognitive impairment is indicated.
When engaging in any intervention, the importance of the therapeutic relationship must be recognised, but particularly when working with a service-user presenting with HD. In creating a therapeutic space which is non-judgemental, compassionate and safe, a trusting and supportive relationship can be nurtured, which can encourage the individual to open up about the difficult thoughts, feelings and urges they may have been experiencing without fear of stigma or judgement (Moorey and Lavender, Reference Moorey and Lavender2018). However, it is worth noting that the strength of this relationship must be balanced with the risk of dependency and as such, may add complexity to the termination of the client–therapist relationship. This requires a collaborate discussion on endings and how these may be interpreted in consideration of the service-user’s current beliefs and appraisals.
In consideration of the current need to engage in remote intervention, and the likely ongoing demand for remote therapy going forward, these findings build on previous evidence (Muroff and Steketee, Reference Muroff and Steketee2018; Ong et al., Reference Ong, Krafft, Panoussi, Petersen, Levin and Twohig2021) and provide further support for the effectiveness of a remote-CBT intervention for individuals presenting with HD. This paper also highlights considerations for engaging with this remote intervention. Critically, observations from this case report suggest that outcomes in remote-CBT interventions for HD are largely congruous with those produced by face-to-face interventions. Thus, in line with concurrent literature on remote-CBT interventions (Luo, Reference Luo, Sanger, Singhal, Pattrick, Shams, Shahid, Hoang, Schmidt, Lee, Haber, Puckering, Buchanan, Lee, Ng, Sun, Kheyson, Chung, Sanger, Thabane and Samaan2020; Wootton, Reference Wootton2016), this therefore suggests that the effectiveness of CBT interventions do not appear to be meaningfully different when delivered in a remote setting. Broadly speaking, this case report indicates that remote-CBT appears to be both an acceptable and effective endeavour for treating older adults with HD in a community mental health setting.
Key practice points
-
(1) The opportunity to deliver CBT for HD via video technologies presents a distinct advantage for behaviour change through offering unprecedented opportunities to access and practise skills in the home environment.
-
(2) Weekly written summaries of the main points covered and between-session tasks agreed appear beneficial in reinforcing learning. They also function to provide additional support for any information-processing difficulties reported.
-
(3) Friends or family members can act as a ‘buddy’ throughout intervention; providing invaluable support, both practical and emotional, to the service-user in carrying out between-session tasks and ensuring continuance of practice following completion of formal intervention.
-
(4) A significant focus on beliefs and cognitive appraisals should occur throughout both formulation and intervention to achieve maximum progress. It is possible, however, that these may become increasingly activated during intervention through greater insight and awareness, and thus may be slower to respond to intervention.
-
(5) Pre- and post-intervention outcome measures should be administered in a collaborative manner, to ensure greater accuracy and reliability of data. However, an integrative approach, which takes a more holistic view of measuring progress, should be adopted within this population.
Data availability statement
The data that support the findings of this study are available within the article. No further data are available as they contain information which could comprise the privacy of the case study participant.
Acknowledgements
Thank you to all those who provided support and feedback on this piece of work, both in Queens University, Belfast and the Psychological Therapies Service.
Author contributions
Aoife Malone: Conceptualization (lead), Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (lead), Project administration (lead), Resources (equal), Writing – original draft (lead), Writing – review & editing (equal); David McCormack: Formal analysis (supporting), Supervision (equal), Writing – review & editing (equal); Emma McCullough: Resources (equal), Supervision (equal), Writing – review & editing (equal).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors declare none.
Ethical standards
Ethical approval was not needed for this case study, but the authors abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the relevant representative bodies (BPS, HCPC, BABCP) and worked under the guidance of standard university research governance procedures at all times. Mary provided verbal and written consent for this work to be written up for publication.







Comments
No Comments have been published for this article.