The National Health Service (NHS) is one of the largest employers in the UK with the healthcare sector having one of the highest sickness absence rates in comparison with other industries. 1 There have been concerns regarding increasing demands, and constraints on resources and staffing within the NHS. 2 Doctors have reported feeling increasingly stressed, which could be caused by increasing workloads, poor morale and staff shortages. 2 A higher prevalence of occupational stress and mental ill health has been reported in doctors in comparison with other professions such as teachers, accountants and health service managers. Reference McKevitt, Morgan, Dundas and Holland3–8 Other studies have demonstrated that doctors tend to take less sickness absence in comparison with other professions such as nurses, despite having similar health statuses. Reference McKevitt, Morgan, Dundas and Holland3,Reference Chambers and Belcher5,Reference Kivimaki, Sutinen, Elovainio, Vahterad, Räsänend and Töyryd9 This could be because of increased ‘sickness presenteeism’, commitment to work and inadequate staff cover. Reference McKevitt, Morgan, Dundas and Holland3,Reference Chambers and Belcher5 Although previous studies have explored the prevalence of stress and mental ill health in doctors, Reference Caplan4,Reference Johnson, Cooper, Cartwright, Donald, Taylor and Millet7,Reference Siegrist, Shackelton, Link, Marceau, von dem Knesebeck and McKinlay10–Reference Taylor, Graham, Potts, Richards and Ramirez17 there have not been any studies investigating whether incidence and trends in incidence of work-related mental ill health (WRMIH) in doctors working in Great Britain is increasing. Incidence rates and trends in incidence rates can be used to estimate risk, whereas prevalence studies can only estimate the current burden of disease. A previous study of trends in work-related ill health (WRIH) incidence using occupational physicians' reported incidence data has shown that the reported incidence of WRMIH has been increasing over recent years in the health and social care sector. Reference Carder, McNamee, Turner, Hodgson, Holland and Agius18 Moreover, it is not known whether the trend in incidence of WRIH and WRMIH in doctors is similar to other public service occupations such as nurses, ambulance staff, social workers and teachers. The aim of this study was therefore to estimate and then compare the incidence and time trends in incidence of WRIH and WRMIH in doctors with other public service professions (nurses, social workers, ambulance staff and teachers). For the purpose of this study, WRIH cases include all cases of ill health that are caused or aggravated by work, which will include WRMIH cases too. WRMIH cases will only include cases of mental ill health that are caused or aggravated by work. This is therefore a subset of WRIH.
Method
The Health and Occupation Research (THOR) Network is the only UK-wide medically diagnosed data source of individual incident case reports of all WRIH. 19 THOR consists of a number of physician-reported surveillance schemes for WRIH, through which participating clinical consultants, occupational physicians and general practitioners (GPs) report incident cases of WRIH seen during their usual clinical practice. 19 One of the surveillance schemes within the THOR network is Occupational Physicians Reporting Activity (OPRA), which collects data on occupational-physician-reported incident cases of WRIH. There is good occupational physician coverage in the health and social care sector by OPRA reporters Reference Carder, Money, Turner and Agius20 and therefore OPRA as a data source can provide accurate estimations of incidence and trends in incidence for workers within this sector.
The methods used in THOR and OPRA have been documented previously. Reference Carder, McNamee, Turner, Hodgson, Holland and Agius18,Reference Carder, McNamee, Turner, Hussey, Money and Agius21 In brief, reporting physicians are asked to report newly diagnosed (i.e. incident) cases of WRIH and which they judge to have been caused or aggravated by work. For each case, the occupational physician is asked to report the diagnosis, age, gender, occupation, industry, suspected agent (the hazard/agent causing or contributing to WRIH), reason for referral to an occupational physician and date of symptom onset. The reported cases provide the numerator data to estimate incidence and trends in incidence. Information on occupation is subsequently classified using the Standard Occupation Classification 2000 (SOC 2000) 22 Physicians participate in OPRA on either a continuous monthly basis (‘core’ reporting) or for one randomly selected month each year (‘sample’ reporting) to avoid seasonal bias. Sample reporting was used to reduce the burden and fatigue of reporting. Annual estimated cases were calculated by multiplying the cases reported by ‘sample’ reporters by 12 and then adding them to the cases reported by core reporters.
Case reports in Great Britain for the group of interest (doctors) and the comparison groups (nurses, social workers, ambulance staff and teachers) were extracted from the OPRA database for the period 2001 to 2014. This enabled comparisons of doctors to be made with other selected public sector occupations working in education and healthcare. Furthermore, teachers were in the same SOC classification as doctors. This means that both occupations are in the same category based on skill level and skill content. 22 The chi-squared test was used to compare the gender distribution of the reported cases compared with the population using the Labour Force Survey data (LFS) 23 across each of the occupations.
Calculating incidence rates
As a result of the uneven access to occupational physicians across Great Britain, it is estimated that only 12% of the workforce have access to an occupational physician. Reference Carder, Money, Turner and Agius20 However, there is disproportionate occupational physician coverage between different industry sectors, with public sectors and larger employers having better coverage in comparison with other industries such as agriculture. Reference Carder, Money, Turner and Agius20 Hence, applying the total workforce calculated from the LFS 23 as the denominator could lead to inaccurate incidence rates. In order to improve the quality of the underlying denominator, a 3-year rolling denominator survey was initiated to investigate the workforce covered by OPRA reporters. Reference Carder, Money, Turner and Agius20 The type of workforce that occupational physician reporters covered was classified according to major industries using the Standard Industrial Classification (SIC) 2003 and 2007. 24 This was done for two triennia: 2005–2007 and 2008–2010. The numerator was the annual average number of estimated cases reported to OPRA (in each triennium). Cases of interest were initially identified by industry (health and social care sector, education sector) and by occupation (doctors, nurses, social workers, ambulance staff and teachers). Cases were only included if the occupational physician who reported them had provided denominator information (in one or both of the occupational physician denominator surveys) for the industry from which the cases arose. Incidence rates by industry (health and social care or education) were calculated by applying the number of people employed in each sector according to the occupational physician denominator surveys (2005–2007 or 2008–2010) as the denominator. To calculate incident rates by occupation, the denominator of the industry covered by the occupational physician were adjusted according to the proportion of an occupation within an industry. The proportion of an occupation within an industry was calculated using the LFS data. A flow chart summarising how incidence rates were calculated is shown in Fig. 1.
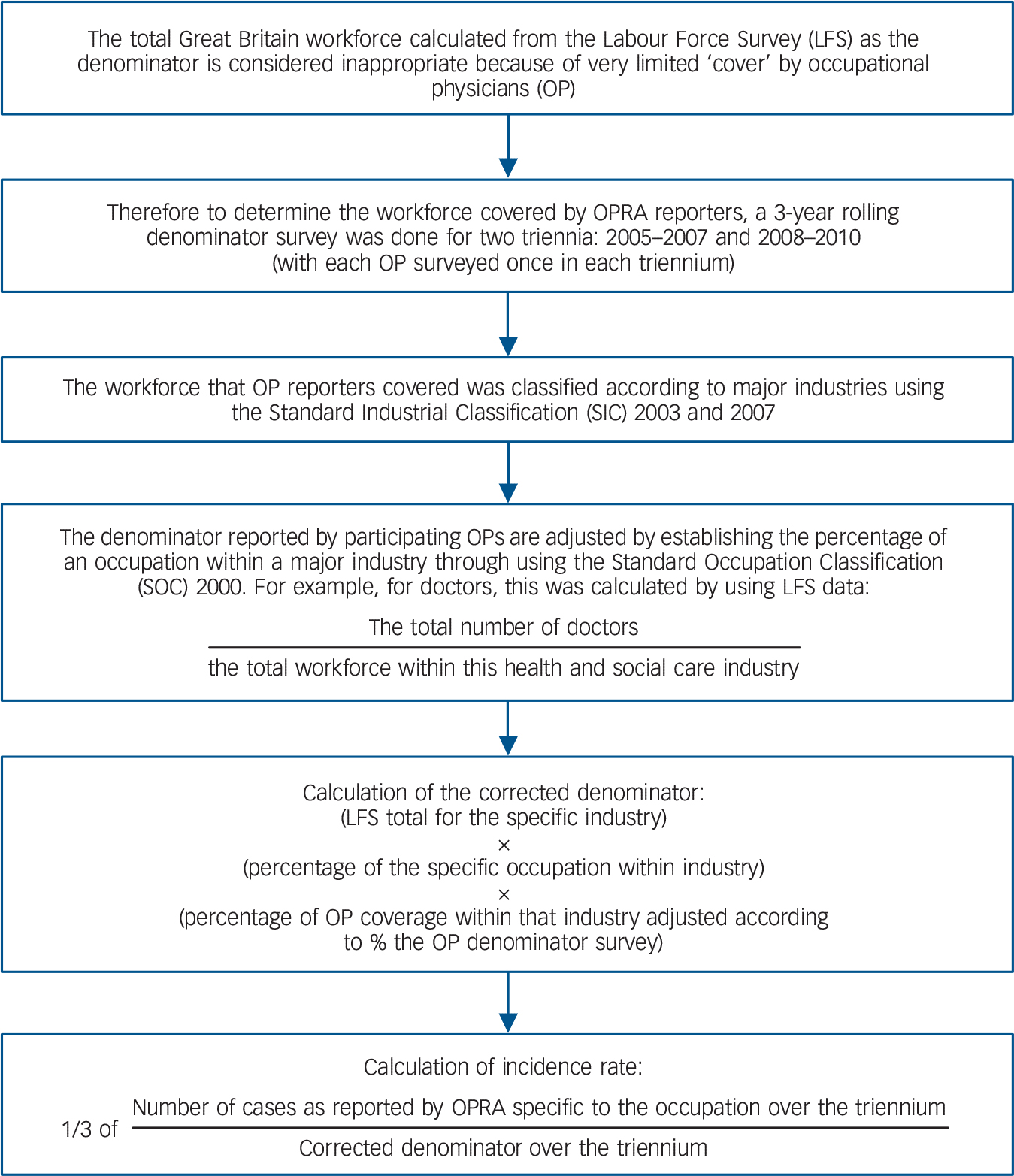
Fig. 1 Flow chart summarising the methods used to calculate incidence rates.
Occupational Physicians Reporting Activity.
To calculate the confidence intervals for incidence rates, a normal approximation to the Poisson distribution was assumed and complex sample survey methodology employed in the form of a first-order Taylor linearised variance estimator. Reference Wolter25
Time trends analyses
The methods used to analyse trends in WRIH and WRMIH incidence based on data from the THOR surveillance scheme have been described previously. Reference Carder, McNamee, Turner, Hodgson, Holland and Agius18,Reference McNamee, Carder, Chen and Agius26 In brief, estimated changes in incidence across calendar time (2001–2014) were investigated using multilevel longitudinal, negative binomial models with random repetitive effects. This method accounts for within- and between-reporter variation in responses because of clustering, i.e. 12 responses per year for core reporters and 1 per year for sample reporters. Reference McNamee, Carder, Chen and Agius26 The dependent variable was the number of reported cases per reporter per month (which includes zero responses). The main predictor of interest, mean centred calendar time, was represented as a continuous variable with a scale of years. Variables representing other potential confounders such as season, reporter type (core or sample reporter), first month as new core reporter, membership time, first month as new reporter and industrial group were also included as covariates. Reference McNamee, Carder, Chen and Agius26 To account for changes in population base, an offset variable representing the number of people employed in Great Britain each year (i.e. 2001–2014) in the occupational group under investigation was included. Finally, to assess whether there were differences in trends between doctors and other occupational groups, a statistical interaction term between occupation group and calendar years was added to the model. All analysis was performed in Stata vl4. Multicentre Research Ethics Committee approval has been granted to THOR (reference number MREC 02/8/72).
Results
Descriptive characteristics and incidence rates
Between 2005 and 2010, the total number of estimated incident cases from the occupational physician reporting scheme were: doctors 1097, nurses 4946, social workers 433, ambulance staff 268 and teachers 1649. The percentage proportions of gender mixes found in our results were representative of the gender mix found in these occupations in the population (according to the LFS data). The chi-squared test of distribution showed that the gender proportions found in our results were representative of the working population for doctors, but not for nurses, ambulance staff, social workers and teachers (P<0.001). From 2005–2010, 82.5% of WRIH cases in doctors were WRMIH. Less than half of WRIH cases in ambulance staff were WRMIH cases, whereas for the other occupations, a significant proportion of WRIH cases (>60%) were WRMIH cases (Table 1).
Table 1 Descriptive demographics of the different occupations based on the Occupational Physicians Reporting Activity (OPRA) database between 2005 and 2010, and overall incidence rates (per 100 000 persons employed) for both work-related ill health and work-related mental ill health
| Occupation | Sector | ||||||
|---|---|---|---|---|---|---|---|
| Cases of ill health, 2005–2010 | Doctors | Nurses | Social workers | Ambulance staff | Teachers | Health and social care | Education |
| Work-related ill health | |||||||
| Age, years: median | 44 | 44 | 50 | 43 | 49 | – | – |
| Age, years: range | 22–65 | 18–68 | 25–64 | 26–53 | 22–63 | – | – |
| Female, n (%) | 437 (40) | 4162 (84) | 305 (70) | 80 (30) | 952 (58) | – | – |
| Male, n (%) | 660 (60) | 784 (16) | 128 (30) | 188 (70) | 697 (42) | – | – |
| Total, n | 1097 | 4946 | 433 | 268 | 1649 | – | – |
| Incidence rates/100 000 people employed (95% CI) |
515 (409–621) | 964 (760–1167) | 227 (128–327) | 1611 (306–2917) | 228 (171–285) | 461 (378–544) | 225 (169–281) |
| Work-related mental ill health | |||||||
| Age, years: median | 46 | 45 | 49 | 44 | 50 | – | – |
| Age, years: range | 22–65 | 22–62 | 25–64 | 27–53 | 25–63 | – | – |
| Female, n (%) | 314 (35) | 2608 (83) | 276 (71) | 36 (31) | 817 (56) | – | – |
| Male, n (%) | 591 (65) | 553 (17) | 116 (30) | 79 (69) | 631 (44) | – | – |
| Total, n | 905 | 3161 | 390 | 115 | 1448 | – | – |
| Percentage of total cases of work-related ill health |
83 | 64 | 90 | 43 | 88 | ||
| Incidence rates/100 000 people employed (95% CI) |
431 (335–528) | 641 (497–785) | 221 (123–320) | 610 (0–1313) | 201 (156–247) | 286 (235–337) | 165 (125–205) |
Adjusted incidence rates taking account of the corrected denominator for both triennia are shown in Table 1. Incidence rates between the two triennia showed little variation and therefore are presented as an average incidence rate over both, i.e. from 2005 to 2010. Both ambulance staff and nurses indicated a higher incidence of WRIH and WRMIH compared with doctors, which in turn were higher than for teachers and social workers. Overall, higher incidence rates were found in the health and social care sector in comparison with the education sector.
Time trends analyses
The total number of cases and estimated annual percentage changes for WRIH, WRMIH and WRIH without mental health are presented in Table 2. From 2001 to 2014, a statistically significant increase in WRIH was demonstrated for doctors only, with an annual average increase of +6.1% (95% CI +2.2% to +10.1%), and similar trends for both female and male doctors (Table 2). For nurses, ambulance staff and teachers, all three occupations showed an annual average decrease in incidence of −3.2% (95% CI −5.3% to −1.0%), −10.8% (95% CI −18.2% to −2.5%) and −4.3% (95% CI −5.3% to −1.0%), respectively with no trend observed in social workers. Statistically significant interaction effects indicated differences in the calendar trend of WRIH in nurses (P<0.001), ambulance staff (P<0.001) and teachers (P<0.001) compared with doctors.
Table 2 Total number of actual cases and estimated annual percentage changes in incidence rates for incidence of work-related ill health, work-related mental ill health and work-related ill health without mental health cases from 2001 to 2014
| Work-related ill health (WRIH) cases | Work-related ill health (WRIH) without mental health cases |
Work-related mental ill health (WRMIH) cases only |
||||
|---|---|---|---|---|---|---|
| Occupation | Actual cases, n |
Annual percentage change in incidence rate (95% CI) |
Actual cases, n |
Annual percentage change in incidence rate (95% CI) |
Actual cases, n |
Annual percentage change in incidence rate (95% CI) |
| Doctors | 334 | +6.1 (+2.2 to +10.1) | 69 | +1.9 (−5.4 to +9.7) | 265 | +6.5 (+2.2 to +11) |
| Female | 152 | +6.4 (+0.6 to +12.5) | 39 | −2.6 (−11.6 to +7.4) | 113 | +8.6 (+1.7 to +16.0) |
| Male | 182 | +5.1 (+0.3 to +10.2) | 30 | – a | 152 | +4.4 (−0.7 to +9.9) |
| Nurses | 1617 | −3.2 (−5.3 to −1.0) | 612 | −5.7 (−8.7 to −2.7) | 1005 | −1.3 (−4.0 to +1.4) |
| Female | 1390 | −3.5 (−5.8 to −1.2) | 544 | −6.9 (−10.0 to −3.7) | 846 | +1 (−3.8 to +1.9) |
| Male | 227 | −2.3 (−6.8 to +2.3) | 68 | +0.8 (−6.4 to +8.5) | 159 | −4.3 (−9.6 to +1.3) |
| Social workers | 209 | 0 (−4.8 to +5.9) | 18 | – a | 191 | 1.2 (−4.3 to +7.0) |
| Female | 155 | +2.8 (−3.1 to +9.1) | 16 | – a | 139 | +3.8 (−2.5 to +10.4) |
| Male | 54 | −2.6 (−11.7 to +7.4) | 2 | – a | 52 | −1.8 (−11.0 to +8.4) |
| Ambulance staff | 95 | −10.8 (−18.2 to −2.5) | 64 | −10.9 (−20 to −0.9) | 31 | −4.9 (−15.7 to +7.2) |
| Female | 34 | −0.3 (−12.3 to +13.3) | 29 | −3.3 (−16.1 to +11.5) | 5 | – a |
| Male | 61 | −11.3 (−19.8 to −1.9) | 35 | −12.4 (−13.6 to 0.0) | 26 | – a |
| Teachers | 977 | −4.3 (−5.3 to −1.0) | 101 | −8.5 (−15 to −1.6) | 876 | −3.9 (−6.5 to −1.2) |
| Female | 608 | −3.8 (−6.8 to −0.7) | 78 | −10.6 (−17.9 to −2.6) | 346 | −2.6 (−5.9 to +0.7) |
| Male | 369 | −6.7 (−10.3 to −2.9) | 23 | −3.4 (−14.7 to +9.4) | 530 | −6.9 (−10.7 to −3.0) |
a. Insufficient cases.
For WRMIH, only doctors showed a statistically significant annual average increase in incidence of +6.5% (95% CI +2.2% to +11%). Teachers showed a statistically significant average annual decrease of −3.9% (95% CI −6.5% to −1.2%). Nurses, ambulance staff and social workers did not show a statistically significant annual average change between 2001 and 2014. Statistically significant interaction effects indicated differences in the calendar trend of WRMIH in nurses (P = 0.01), ambulance staff (P = 0.03) and teachers (P < 0.001) compared with doctors.
For WRIH without mental ill health cases, an annual average increase in incidence for doctors was not observed. However, for nurses, ambulance staff and teachers, all three groups showed a statistically significant annual average decrease in incidence of −5.7% (95% CI −8.7% to −2.7%), −10.9% (95% CI −20% to −0.9%) and −8.5% (95% CI −15% to −1.6%), respectively. Statistically significant interaction effects indicated differences in the calendar trend of WRIH without mental ill health cases in ambulance staff (P = 0.01) and teachers (P = 0.05) compared with doctors.
Discussion
Summary of the results
This study indicated that compared with doctors, incidence rates were highest in ambulance staff for reported WRIH and nurses for reported WRMIH. However, the trends analyses suggested that the incidence of both reported WRIH and WRMIH has been increasing in doctors since 2001, especially in female doctors. On the other hand, other occupations such as ambulance staff, nurses and teachers have largely shown either a decreasing trend or no significant change in incidence since 2001.
Meaning of the results
Our time trends analyses for WRIH and WRMIH in doctors showed an increase over time whereas other occupations showed a decrease or no significant change in incidence of reported ill health and mental ill health. This could be the result of a number of reasons that may affect doctors more as a profession such as poor training in management skills, work overload in both clinical and non-clinical duties, staff shortages, perceived lack of control and feedback especially when it comes to patient care, high responsibility, lack of support, poor work–life balance and pressures on continuing professional development. 2,Reference McKevitt, Morgan, Dundas and Holland3,Reference Siegrist, Shackelton, Link, Marceau, von dem Knesebeck and McKinlay10,Reference Ramirez, Graham, Richards, Cull and Gregory11,Reference Agius, Blenkin, Deary, Zealley and Wood13,Reference Graham, Ramirez, Cull, Finlay, Hoy and Richards14,Reference Tomioka, Morita, Saeki, Okamoto and Kurumatani16,Reference Rich, Viney, Needleman, Griffin and Woolf27 Although some of the above reasons may not be exclusive to doctors, it is likely that multiple factors would be occurring simultaneously in doctors who have ultimate responsibility for clinical care, which in turn is more likely to have an impact on their well-being. The above reasons are supported by a recent systematic meta-review that has identified three broad work-related factors that could contribute to the development of common mental health conditions such as depression and anxiety: unsuitable job designs, job uncertainty and lack of workplace value and respect. Reference Harvey, Modini, Joyce, Milligan-Saville, Tan and Mykletun28 These factors could also be relevant to WRMIH in the medical profession and our data show that out of 1944 precipitating events from 2001 to 2014, the most common ones were workload (29%, n = 572) (unsuitable job design), work stress (14%, n = 267) (unsuitable job design) and organisation factors such as poor management, poor role and low job control and perceived lack of support (9%, n = 167) (job uncertainty and lack of workplace value and respect).
Within our analysis, female doctors showed a statistically significant annual average increase in WRMIH over time. There has been discussion within the literature suggesting that women are more susceptible to stress and depression. Reference Firth-Cozens, Cox, Hutchinson and McAvoy29 This could be because female doctors may be more likely to experience conflicts between their career and personal commitments which in turn, could more likely have an impact on their work–life balance and mental well-being compared with men. Reference Rich, Viney, Needleman, Griffin and Woolf27,Reference Firth-Cozens, Cox, Hutchinson and McAvoy29,Reference Firth-Cozens30 The subsequent effects of WRMIH in both genders could lead to increased sickness absence, substance misuse and negative effects on work performance, morale and relations with patients. 2,Reference Brooks, Gerada and Chalder15,Reference Firth-Cozens and Greenhalgh31,Reference Taylor, Graham, Potts, Candy, Richards and Ramirez32 Furthermore, WRMIH has been associated with perceived lower standards of care as well as lower performance standards. Reference Taylor, Graham, Potts, Candy, Richards and Ramirez32
Although doctors were not found to have the highest incidence rate of WRIH and WRMIH, previous studies suggest that doctors may be reluctant to access help even though there are formal support systems within the NHS and through charities. Reference Harrison33 This could suggest that our results may be an underestimation of the extent of WRIH and WRMIH in doctors. Even at early stages of their career, medical students have already shown a preference to seek informal help from family and friends rather than to access formal support systems. Reference Chew-Graham, Rogers and Yassin34 Furthermore, it is possible that a significant proportion of doctors who are referred to occupational physicians may avoid discussing the extent of their problem Reference Harrison33 and underestimate the actual severity of the impact on their well-being. Adams et al showed that despite the high prevalence of depression in doctors within their study, only a small proportion of doctors took sickness absence for their mental health and those doctors with depression were more likely to take time off for a physical problem rather than for their depression. Reference Adams, Lee, Pritchard and White35 Many doctors were still reluctant to disclose mental health problems, citing career implications, professional integrity and stigmatisation as the main barriers to disclosure, and there was a strong preference to be treated in a private institution for their mental ill health. Reference Hassan, Ahmed, White and Galbraith36 Sadly, over 40% of those surveyed still preferred to have informal advice as their first treatment preference, Reference Hassan, Ahmed, White and Galbraith36 suggesting that the increasing trend of WRMIH diagnoses between 2001 and 2014, as reported by occupational physicians within our study could be underestimated because of underreporting.
Within our study, occupations such as nurses, ambulance staff and teachers showed a decrease in average annual incidence for non-WRMIH. Johnson et al found that ambulance staff and teachers self-reported the lowest physical health compared with other professions, which included doctors. Reference Johnson, Cooper, Cartwright, Donald, Taylor and Millet7 Furthermore, manual handling injuries are not uncommon in nursing staff. Reference Hignett, Fray, Rossi, Tamminen-Peter, Hermann and Lomi37 The manual nature of these jobs may have initially led to higher incidence rates of WRIH and non-WRMIH cases within the OPRA scheme compared with doctors. However, the decrease in average annual incidence rate may have been contributed by the introduction of legislation, intervention and greater awareness on preventing physical injuries in the workplace. Reference Hignett, Fray, Rossi, Tamminen-Peter, Hermann and Lomi37
Strengths and limitations
To our knowledge, this is the first study that has investigated the trend in incidence of WRIH and WRMIH in doctors. Although other studies have demonstrated the extent of mental ill health in doctors, those studies examined prevalence rather than incidence and trends in incidence. Reference Caplan4,Reference Chambers and Belcher5,Reference Johnson, Cooper, Cartwright, Donald, Taylor and Millet7,Reference Siegrist, Shackelton, Link, Marceau, von dem Knesebeck and McKinlay10–Reference Agius, Blenkin, Deary, Zealley and Wood13,Reference Tomioka, Morita, Saeki, Okamoto and Kurumatani16,Reference Taylor, Graham, Potts, Richards and Ramirez17,Reference Firth-Cozens, Cox, Hutchinson and McAvoy29 The present surveillance-based study, besides estimating incidence rates of WRMIH in doctors, also enables comparisons with different occupations of both incidence rates and trends of incidence rates. Self-reported data of WRIH and WRMIH could be biased by attitudes and beliefs as well as underreporting, therefore making it difficult to reliably assess the actual extent of WRIH and WRMIH among doctors. In contrast, our study used data reported by physicians seeing the doctors in which incidence rates and trends in incidence rates can be used to estimate risk, whereas prevalence studies can only estimate the burden of disease. Data collected by occupational disease surveillance systems such as OPRA contribute to national statistics and identify changes in incidence over time. Reference Agius, Bonneterre and Venables38,39 In turn, this can provide evidence to guide further research that can potentially influence policy at a government level so that interventions and services can be targeted to improve managing WRIH and WRIMIH in doctors.
One limitation of the denominator survey was that the occupational physician denominator surveys only covered two triennia reducing the sample size available. Moreover, denominator estimation could be subject to recall bias and generalisations because of potential difficulties in accurately defining the workforce they cover. Reference Carder, Money, Turner and Agius20 Furthermore, it could be possible that non-responder bias was present, as not all OPRA reporters participated in the denominator survey in both triennia. To calculate incidence rates by occupation, the industry denominators were adjusted by the proportion of an occupation within an industry, according to the LFS. However, the workforce coverage by the individual occupational physicians may not be representative of the proportion within an industry as found in the LFS data because of the case mix that occupational physicians review. This could lead to overestimation if occupational physicians see a higher proportion of a certain occupation or underestimation of incidence rates if occupational physicians review a lower proportion of another occupation. Nevertheless, by using the data from the denominator surveys, this enables the incidence rates of WRIH to be calculated more accurately than using LFS as the denominator and results could therefore be generalised and triangulated with other data sources, both within and external to THOR. Reference Carder, McNamee, Turner, Hodgson, Holland and Agius18,Reference Carder, Money, Turner and Agius20
This study has presented both ‘unadjusted’ and ‘adjusted’ incidence rates, with the latter adjusting the numerator to allow for cases not captured as a result of non-participation and non-response. Reference Carder, McNamee, Turner, Hussey, Money and Agius21 Furthermore, random selection of sample reporters' 1-month reporting period can minimise seasonal bias. This approach might overestimate rates as it assumes that physicians not participating/responding would report (on average) at the same density as those that are. However, even with these adjustments, given the difficulty of work attribution for mental ill health diagnoses, it is possible that the adjusted rates underestimate the true incidence of WRMIH in Britain. Further methodological assumptions regarding sampling frequency or estimation of denominators may also have led to rates being under- or overestimated. Although not directly addressed in the current study, the sensitivity of incidence rate calculations to these assumptions has been extensively addressed previously in the THOR data-set. Reference Carder, Money, Turner and Agius20,Reference Carder, McNamee, Turner, Hussey, Money and Agius21,Reference McNamee, Chen, Hussey and Agius40
Another limitation of the present study is that because of the constraints of the data collection, it was not possible to differentiate between the grade and specialty of the doctors. Certain specialties such as accident and emergency, psychiatry and general practice have been shown to have higher prevalence of mental ill health compared with other specialties. Reference Caplan4,Reference Ramirez, Graham, Richards, Cull and Gregory11,Reference Burbeck, Coomber, Robinson and Todd12,Reference Graham, Ramirez, Cull, Finlay, Hoy and Richards14,Reference Firth-Cozens, Cox, Hutchinson and McAvoy29 However, even if our data were able to differentiate between grade and specialty, trends analyses may not have been possible because of small numbers of cases within each subgroup. Furthermore, as a result of limitations in the type of data collected, we were not able to investigate sickness absence rates or health-seeking behaviours that could have complimented our results.
Suggestions for future research
This study shows that the incidence of WRIH and WRMIH is increasing in doctors as reported by occupational physicians, especially in female doctors, whereas the other compared occupations largely showed either a decreasing trend or no significant change since 2001. Further research is required to explore the underlying factors contributing to this finding in order to identify modifiable factors. By identifying the underlying contributing factors, research can then be tailored to investigate and assess interventions that optimise the management of both WRIH and WRMIH in doctors. This in turn could contribute to improving and maintaining excellent patient care and safety in the long term.
Funding
THOR in the UK is largely funded by the Health and Safety Executive (HSE). The opinions in this paper are those of the authors and not of the funders. The funders did not contribute to this study. The funders had no role in study design, data collection, data interpretation, writing report or decision to submit the article for publication.
Acknowledgements
The authors would like to thank all the doctors who participate in the OPRA surveillance scheme. We would like to thank the Health and Safety Executive (HSE) for partially funding the OPRA surveillance scheme.






eLetters
No eLetters have been published for this article.