Background
The rates of post-traumatic stress disorder (PTSD) in UK veterans deployed to the conflicts in Afghanistan and Iraq is higher than non-deployed personnel.Reference Stevelink, Jones, Hull, Pernet, MacCrimmon and Goodwin1 This is most marked in veterans who have left the military having previously deployed in combat roles, with 17% of these individuals reporting symptoms suggestive of probable PTSD.Reference Stevelink, Jones, Hull, Pernet, MacCrimmon and Goodwin1 These rates are similar to those observed in Canadian, Australian and USA military samples involved in similar deployments.Reference Van Hooff, Forbes, Lawrence-Wood, Hodson, Saflre and Benassi2–Reference Thompson, VanTil, Zamorski, Garber, Dursun and Fikretoglu4 This is of particular importance since there is a body of evidence showing that some veterans with PTSD have poorer responses to treatments than members of the general public.Reference Kitchiner, Roberts, Wilcox and Bisson5 Latent class studies of PTSD treatment responses in USA, Australian and UK populations demonstrated the heterogeneity of treatment response.Reference Phelps, Steel, Metcalf, Alkemade, Kerr and O'Donnel6–Reference Currier, Holland and Kent8 Factors such as severity of PTSD presentations, comorbid mental difficulties, childhood adversity and dissociation are associated with poorer treatment responses.Reference Phelps, Steel, Metcalf, Alkemade, Kerr and O'Donnel6,Reference Murphy and Smith7,Reference Richardson, Contractor, Armour, St Cyr, Elhai and Sareen9 Taken together, a one-size-fits-all approach to understanding PTSD may not be adequate, and there is a need to better understand the complexity of PTSD presentations in military veterans and other trauma populations.
Complex PTSD
The latest version of the World Health Organization's ICD-11, released in 2018 and due to be implemented in January 2022, included a new definition of PTSD, comprising six symptoms, and a new diagnosis of complex PTSD (CPTSD), comprising 12 symptoms (six PTSD symptoms and six ‘disturbance in self-organisation’ (DSO) symptoms),10 each organised in three clusters of symptoms. The PTSD clusters include re-experiencing of the trauma in the present, avoidance of traumatic reminders and a sense of current threat. CPTSD comprises the three PTSD clusters and three additional symptom clusters that reflect DSO: affective dysregulation, negative self-concept, and disturbances in relationships. To fulfil the diagnosis, both PTSD and CPTSD also require traumatic exposure and significant impairment in functioning.
The International Trauma Questionnaire (ITQ) is the only validated measure for the assessment of ICD-11 PTSD and CPTSD.Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker11 Using the ITQ, initial population-based studies suggest that CPTSD is a more marginally common condition that PTSD. For example, in the USA, 7.2% of adults were found to have either ICD-11 PTSD (3.4%) or CPTSD (3.8%).Reference Cloitre, Hyland, Bisson, Brewin, Roberts and Karatzias12 This prevalence is similar to that reported using DSM-based PTSD criteria, as per the National Comorbidity Survey (7.8%).Reference Kessler, Chiu, Demler and Walter13 In a population-based trauma-exposed sample in the UK, it was also found that 5.3% met the diagnostic criteria for PTSD and 12.9% for CPTSD.Reference Karatzias, Hyland, Bradley, Cloitre, Roberts and Bisson14 Preliminary evidence also suggests that CPTSD is a more common condition in treatment-seeking populations compared with PTSD. In one study, 76% met diagnostic criteria for CPTSD v. 24% for PTSD in treatment-seeking adults.Reference Karatzias, Shevlin, Fyvie, Hyland, Efthymiadou and Wilson15 In the same study it was also reported that multiple exposure to trauma and childhood trauma were both significant risk factors for CPTSD.
There is now evidence that a high percentage of military personnel will have been exposed to childhood trauma or multiple combat stressors, commonly associated with CPTSD. High rates of pre-service adversity in military populations have been reported in the literature.Reference Murphy, Ashwick, Palmer and Busuttil16 Veterans who have served in conflict zones may also have been exposed to multiple traumatic experiences. Understanding the prevalence and patterns of CPTSD within veteran populations may help with both the identification of individuals who might be less likely to respond to standard treatments for PTSD, and stimulate research for better treatments for CPTSD.
This study had two primary aims, first to validate the ITQ by testing alternative factor analytic models, and second, to explore the prevalence of PTSD and CPTSD in a nationally representative study of treatment-seeking veterans in the UK. It was hypothesised, based on a recent review on research evidence on CPTSD,Reference Brewin, Cloitre, Hyland, Shevlin, Maercker and Bryant17 that the best-fitting factor analytic model of the ITQ would be a model with two correlated second-order factors (PTSD and DSO), each being measured by three first-order factors (PTSD measured by the three PTSD clusters; DSO measured by the three CPTSD DSO clusters).
Method
Setting
Participants were recruited from a national charity in the UK that offers mental health treatments to veterans. The charity is the largest provider of veteran-specific services in the UK and receives approximately 2000 referral and supports approximately 3000 veterans annually. For the charity to accept a referral, individuals have to be currently experiencing a mental health difficulty, be a British veteran (in the UK this is defined as having completed 1 day of paid employment with the military) and reside in the UK. Exclusion criteria for a referral to be accepted to the charity included being actively psychotic, actively suicidal or having a primary diagnosis of a personality disorder. The presence of PTSD symptoms is not an inclusion criterion for a referral to be accepted by the charity. In 2017, a previous study had selected a nationally representative sample of treatment-seeking veterans by randomly sampling 20% of veterans engaged with the charity and recruited 403 out of 600 (67.2%) of these to participate in a project about the health and well-being of veterans.Reference Murphy, Ashwick, Palmer and Busuttil16 Engagement was defined as having attended one or more appointments over a 12-month period that were not an initial assessment. The current study aimed to follow up on 403 participants of that study.
Participants
A total of 69 individuals were excluded from the current study because they had either died (n = 8), opted out of being followed up (n = 5) or incomplete contact details that prohibited being re-contacted (n = 56). This left a sample of 334 individuals who were eligible to participate in the current study and invited to participate. Individuals were requested to complete questionnaires via a three-wave postal mail-out strategy. This was followed by attempting to call individuals to remind them about the study. Data was collected between October 2018 and April 2019; 177 of the 334 eligible participants returned completed questionnaires (53.0%).
Materials
ICD-11 PTSD and CPTSD
The ITQ is the only self-report measure of ICD-11 PTSD and CPTSD symptoms.Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker11 Six symptoms and three items assessing functional impairment were used to assess PTSD. Participants indicate how much they have been bothered by each of their core symptoms in the past month, considering their most traumatic event, using a five-point Likert scale ranging from ‘not at all’ (0) to ‘extremely’ (4). Two symptoms reflect the ‘re-experiencing’ cluster (i.e., upsetting dreams and feeling the experience is happening again in the here and now), the ‘avoidance’ cluster (internal reminders and external reminders) and the ‘sense of threat’ cluster (hypervigilance and exaggerated startle response). Three items screened for functional impairment associated with relationships and social life, work or ability to work, and other important aspects of life, such as parenting, school/college work or other important activities. To assess DSO, participants are asked how they typically feel, think about oneself and relate to others. Two items capture the ‘affective dysregulation’ cluster (When I am upset, it takes me a long time to calm down and I feel numb or emotionally shut down), ‘negative self-concept’ cluster (I feel like a failure and I feel worthless) and ‘disturbed relationships’ cluster (I feel distant or cut off from people and I find it hard to stay emotionally close to people). The DSO symptoms are measured using a five-point Likert scale ranging from ‘not at all’ (0) to ‘extremely’ (4). As with the PTSD symptoms, there are three items that screen for functional impairment associated with DSO symptoms.
Diagnostic criteria for PTSD require a score of ≥2 (‘moderately’) for at least one of two symptoms from each of the re-experiencing, avoidance and threat clusters, and at least one functional impairment item to be endorsed (≥2). The diagnostic criteria for CPTSD include satisfying PTSD criteria in addition to scoring ≥2 (‘moderately’) for at least one symptom from each of the affective dysregulation, negative self-concept and disturbed relationships clusters, and at least one functional impairment item to be endorsed (≥2). Based on the ICD-11 diagnostic rules, a diagnosis of PTSD or CPTSD, but not both, can be made. In the present study high levels of internal consistency were found for the PTSD items (α = 0.88), the DSO items (α = 0.90) and the total scale (α = 0.91).
Childhood trauma
The Childhood Trauma Questionnaire (CTQ) is a 28-item, self-report questionnaire that assesses exposure to a range of different childhood traumas.Reference Bernstein and Fink18 The scale produces five subscales, each with five items: emotional abuse, physical abuse, sexual abuse, emotional neglect and physical neglect. Items are responded to using a five-point scale ranging from ‘never true’ (1) to ‘very often true’ (5), and summed scores for the subscales (possible range 5–25) and a total scale score (possible range 25–125) were calculated, with higher scores suggesting more severe maltreatment. Bernstein and Fink also provided cut-off scores to categorise scores as ‘none’, ‘low’, ‘moderate’ and ‘severe’. The CTQ scores have previously demonstrated good internal consistency, test-retest reliability, and convergent validity.Reference Vallieres, Ceannt, Daccache, Daher, Sleiman and Gilmore19 In the present study, high levels of internal consistency were found for each of the subscales, (emotional abuse α = 0.91, physical abuse α = 0.89, sexual abuse α = 0.75, emotional neglect α = 0.91 and physical neglect α = 0.97) and for the total scale (α = 0.93).
Traumatic life events
We used a modified version of the Life Events Checklist (LEC).Reference Gray, Litz, Hsu and Lombardo20 This is a 17-item, self-report measure to screen for exposure to potentially traumatic events. The LEC assesses lifetime exposure to 16 traumatic events (e.g. natural disaster, physical assault, life threatening illness/injury) and the 17th item, ‘any other very stressful event/experience’, can be used to indicate exposure to a trauma that was not listed. For each item, the respondent checks whether the event ‘happened in childhood (before age of 18)’ or ‘happened in adulthood (at or after age 18)’; a ‘yes’ (1) and ‘no’ (0) response format was used. A total cumulative variable was created for both childhood and adult trauma with possible scores ranging from 0 to 16; item 17 was not included as the nature of the trauma could not be identified.
Statistical analysis
The latent structure of the ITQ was tested using confirmatory factor analysis (CFA) based on responses to the 12 core symptom items. Three factor analytic models, along with a baseline comparison model (model 1), that can be most directly derived from the ICD-11 description of CPTSD were specified and tested as representations of PTSD and CPTSD (Fig. 1).Reference Brewin, Cloitre, Hyland, Shevlin, Maercker and Bryant17 Model 1 is a one-factor model where all symptoms load on a single latent variable representing CPTSD. Model 2 is a correlated six-factor model based on the ICD-11 specification of three PTSD and three DSO symptom clusters, each measured by their respective indicators. Model 3 replaced the factor correlations in model 2 with a single second-order factor representing CPTSD. This model proposes that there is no distinction between PTSD and DSO at the second-order level. Model 4 specified two correlated second-order factors (PTSD and DSO) to explain the covariation among the six first-order factors, with the three PTSD symptom clusters loading on the PTSD factor and the three DSO symptom clusters loading on the DSO factor. For all models the error variances were specified to be uncorrelated.

Fig. 1 Alternative factor analytic models of PTSD and CPTSD.
All models were estimated using robust maximum likelihood estimation, which has been shown to produce correct parameter estimates, s.e. and test statisticsReference Van Hooff, Forbes, Lawrence-Wood, Hodson, Saflre and Benassi2 using Mplus version 7.0 for Windows (Mplus, Muthén & Muthén, USA; https://www.statmodel.com/). The criteria for acceptable model fit were a non-significant χ2 test, Comparative Fit Index and Tucker-Lewis Index values >0.90 and root-mean-square error of approximation and standardised root-mean-square residual values of ≤0.08. In addition, the Bayesian Information Criterion (BIC) was used to evaluate alternative models, with the lower value indicating the better-fitting model. Not all models were hierarchically nested, so χ2 difference tests were not appropriate for all comparisons and the BIC was also used as the primary index for model comparison, with the lowest value indicating the best-fitting model. A difference of >10 is considered to be indicative of a ‘significant’ difference.Reference Raftery21 Concurrent validity of the best-fitting model was further examined by calculating the correlations between the latent factors from the best-fitting model and scores from the five subscales of the CTQ and the childhood and adult cumulative scores from the LEC.
For the ITQ there was a small amount of missing data at the item level ranging from 0.6% to 1.7%, and the missingness was considered to be missing completely at random (Little's test: χ2 = 58.08, d.f. = 53, P = 0.29). Missing values were handled using the EM algorithm for single imputation using SPSS version 25 for Windows.
Ethics and consent
The study was granted ethical approval from the research ethics committee of Edinburgh Napier University (ref: SHSC0030) and approved by the Combat Stress research committee. Written consent was obtained from all participants.
Results
Participants reported multiple trauma exposure in childhood and adulthood. The cumulative scores on the childhood LEC ranged from 0 to 11, with a mean of 2.52 (s.d. 2.56, median 2.00), and for the adult LEC ranged from 0 to 16, with a mean of 7.55 (s.d. 3.13, median 7.50). The most commonly reported traumas during childhood were ‘physical assault’ (51.2%), ‘sudden, unexpected death of someone close to you’ (30.2%) and ‘other unwanted or uncomfortable sexual experience’ (17.5%). During adulthood the most commonly reported traumas were ‘combat or exposure to a war zone’ (86.4%), ‘fire or explosion’ (79.2%) and ‘sudden, unexpected death of someone close to you’ (78.6%). The mean scores on the CTQ generally indicated borderline ‘low’ to ‘moderate’ levels of trauma: emotional abuse (mean 10.29, s.d. 6.20), physical abuse (mean 9.28, s.d. 5.46), emotional neglect (mean 12.38, s.d. 6.26), physical neglect (mean 8.75, s.d. 3.86), sexual abuse (mean 7.56, s.d. 5.87).
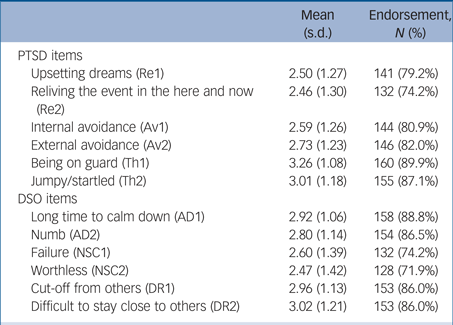
The mean scores and endorsement rates (scores ≥2) of the ITQ items are presented in Table 1. The mean score and endorsement rates were all very high. The ITQ diagnostic rules were applied and the prevalence rates were 56.7% for CPTSD and 14.0% for PTSD.
Table 1 Mean scores and item endorsement of the International Trauma Questionnaire
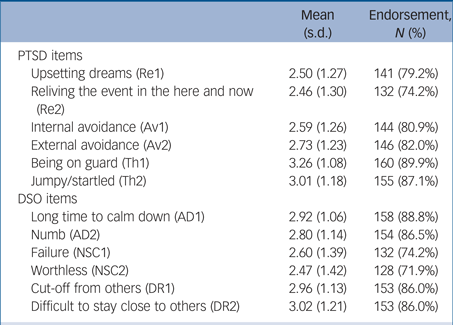
PTSD, post-traumatic stress disorder; Re, re-experiencing; Av, avoidance; Th, sense of threat; DSO, disturbance in self-organisation; AD, affect dysregulation; NSC, negative self-concept; DR, disturbed relationships.
The fit statistics for the CFA models are reported in Table 2. Models 1 and 3 were rejected as they failed to meet the criteria of acceptable model fit. The correlated six-factor model (model 2) and the second-order variant (model 4) were both well-fitting models based on the Comparative Fit Index, Tucker-Lewis Index, root-mean-square error of approximation and standardised root-mean-square residual. For both of these models the χ2 was highly relative to the d.f., but this should lead to a rejection of the model as the value of the χ2 is positively associated with sample size. The models did not differ in the adjusted χ2 (Dc2 = 13.20, Ddf = 8, P = 0.11), but the BIC was lower for model 4, and therefore it was judged to be the best model.
Table 2 Fit statistics for the alternative models of the International Trauma Questionnaire

RMSEA, root-mean-square error of approximation; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; SRMR, standardised root-mean residual; BIC, Bayesian Information Criterion.
* P < 0.05.
The correlations between the summed scores on the PTSD, DSO scales and total scale from the ITQ and scores on the CTQ and child and adult LEC are reported in Table 3.
Table 3 Correlations between PTSD and DSO scores and Childhood Trauma Questionnaire and Life Events Checklist scores

PTSD, post-traumatic stress disorder; DSO, disturbance in self-organisation; LEC, Life Events Checklist; ITQ, International Trauma Questionnaire.
* P < 0.05; **P < 0.01; ***P < 0.001.
The total ITQ scores were positively and significantly correlated with all trauma-related variables, with correlations ranging from 0.169 to 0.278. There was evidence of specificity, with PTSD being uniquely associated with physical neglect and sexual abuse, and DSO being uniquely associated with physical abuse; PTSD and DSO were both significantly associated with emotional abuse and emotional neglect. Child trauma as measured by the LEC was more strongly associated with DSO compared with PTSD, and adult trauma was more strongly associated with PTSD compared with DSO, although the magnitude of the differences were small.
Discussion
We assessed for the first time the latent structure of the ITQ in a sample of UK treatment-seeking veterans. The results of the CFA analyses indicated that the model with two second-order factors, representing PTSD and DSO, was the best-fitting model, providing evidence for two conditions PTSD and CPTSD, as a result of exposure to traumatic life events. The ITQ was able to adequately distinguish between PTSD and CPTSD, in line with previous research in clinical and general populations.Reference Karatzias, Shevlin, Fyvie, Hyland, Efthymiadou and Wilson15 Findings are consistent with findings from other populations that typically report exposure to multiple traumas, such as refugees,Reference Vallieres, Ceannt, Daccache, Daher, Sleiman and Gilmore19 war-exposed youthsReference Murphy, Elklit, Dokkedahl and Shevlin22 and victims of interpersonal trauma,Reference Hyland, Shevlin, Brewin, Cloitre, Downes and Jumbe23 and adds to the body of evidence that supports the construct validity of the ITQ. In addition, the PTSD and DSO scores were associated with individual childhood trauma variables, and cumulative childhood and adulthood trauma exposure. The second aim was to estimate the prevalence of PTSD and CPTSD. It was found that 70.7% of veterans seeking support for mental health difficulties from combat stress meet the case criteria for PTSD or CPTSD, using the ICD-11 definitions as measured by the ITQ. Of these, the majority met the criteria for CPTSD (56.7%) compared with PTSD (14.0%), suggesting that CPTSD is a more common condition than PTSD and presents with more complex mental health presentations in veterans’ services. Higher rates of CPTSD compared with PTSD has previously been reported in other clinical populations and the general public.Reference Karatzias, Hyland, Bradley, Cloitre, Roberts and Bisson14,Reference Karatzias, Shevlin, Fyvie, Hyland, Efthymiadou and Wilson15
We also observed that the participants in this study reported exposure to multiple traumatic events (mean 2.6 and 7.6 events in childhood and adulthood, respectively). Overall, low-to-moderate trauma exposure was reported across a range of domains: emotional abuse, physical abuse, emotional neglect, physical neglect and sexual abuse. In line with previous research, reporting exposure to multiple traumas is the norm in this population group.Reference Mark, Murphy, Stevelink and Fear24 Exposure to multiple traumas is commonly associated with CPTSD, which might partially explain why veterans profit less from PTSD treatments than other populations. Existing gold-standard trauma treatments may not address the effect of multiple and different types of traumatic events, and likewise, there is evidence that CPTSD symptoms that result from childhood trauma might benefit less from exposure-based interventions such as cognitive–behavioural therapy and eye movement desensitisation and reprocessing.Reference Karatzias, Murphy, Cloitre, Bisson, Roberts and Shevlin25
Clinical implications
We conclude that the ITQ is useful in the assessment of both PTSD and CPTSD in treatment-seeking veterans. The presence of childhood trauma was more strongly associated with the DSO symptoms unique to CPTSD. This implies the need to move away from simply focusing on military-related traumas and instead address traumatic distress resulting from childhood traumas as well as military traumas. Considering that CPTSD was more common than PTSD, we recommend routine assessment of CPTSD among help-seeking military personnel. We also conclude that there is a need to develop appropriate interventions for veterans with CPTSDReference Karatzias, Murphy, Cloitre, Bisson, Roberts and Shevlin25 and not rely on existing PTSD interventions. We base this on first, the presence of two disorders (PTSD and CPTSD) rather than just one; second, differences in risk factors (e.g. childhood trauma) and third, different pattern of symptoms.
Looking at the pattern of symptoms reported by participants may provide important information as to how best to support this population. For example, the two most frequently endorsed PTSD symptoms were ‘being on guard’ and feeling ‘jumpy/easily startled’. It may be beneficial for PTSD treatments to focus on these symptoms explicitly rather than simply re-experiencing symptoms that are typically the target for current recommended psychological therapy (e.g. prolonged exposure or trauma-focused cognitive-behavioural therapy). Similarly, the two most frequently reported symptoms unique to CPTSD were feeling ‘cut-off from others’ and finding it ‘difficult to stay close to others’. These symptoms appear similar to the DSM-5 PTSD symptoms of ‘detachment’ and ‘diminished interest’ that have previously been shown to be associated with greater levels of functional impairment in veterans with PTSD.Reference Ross, Murphy and Armour26 Again, this could imply the need to specifically target these symptoms during treatment. It is also important to acknowledge that the ITQ may not be able to differentiate between CPTSD and personality disorder and that future research should aim to explore this further.
Strengths and limitations
The current study profited from sampling from a nationally representative study of treatment-seeking veterans. However, there are a number of limitations. First, only treatment-seeking veterans were included in the study. Evidence suggests that severity of mental health symptoms and PTSD in particular, can be a barrier for veterans engaging support,Reference Stevelink, Jones, Jones, Dyball, Khera and Pernet27 so those with more complex presentations may be underrepresented in the sample, which may have resulted in underestimating the prevalence of CPTSD. Second, the sample size for the current study was modest. Comparison of the mental health and demographic profiles of veterans engaged with the service where recruitment occurred, and a comparable national Australian treatment service for veterans suggests that the mental health profiles of these two population are very similar.Reference Murphy, Howard, Forbes, Busuttil and Phelps28 In addition, a recent review of USA veterans accessing secondary care support suggests that the current studies population would also be comparable with USA treatment-seeking veterans.Reference Mark, Murphy, Stevelink and Fear24 Taken together with the random method of sampling employed within the current study, this could go some way to address issues of generalisability. Third, the majority of the participants met criteria for either PTSD or CPTSD. This is not surprising given this was a clinical population, but means that we cannot extrapolate to true population samples. Fourth, the UK definition of a veteran is very broad and the study could have profited from exploring the specific military experiences that may be associated with PTSD or CPTSD (e.g. combat exposure or length of service).
In conclusion, the study provides evidence that suggests the utility of the ITQ in assessing ICD-11 symptoms of PTSD and CPTSD within clinical populations of veterans. The prevalence of PTSD symptoms were high, with 56.7% and 14.0% meeting criteria for CPTSD and PTSD, respectively. Childhood trauma appeared more strongly associated with CPTSD than PTSD and different types of traumas were associated with PTSD (physical neglect and sexual abuse), CPTSD (physical abuse) and both disorders (emotional abuse and emotional neglect). We conclude it is time to move away from attempting to treat PTSD and CPTSD with the same treatment models and consider how best to develop novel ways, or combine existing treatments by potentially combining trauma-focused therapies with other approaches (e.g. behavioural activation, support to individuals meeting criteria for CPTSD).
Funding
Funding for this study was provided by the Forces in Mind Trust.
Acknowledgements
We would like to thank the participants who took part in this study and Combat Stress staff who supported data collection.
Author contributions
All authors made substantial contributions to the design of this research project, drafting and editing the manuscript, approving the final version and agree to the integrity of the work presented. D.M. was responsible for producing the first draft of the manuscript and M.S. was responsible for conducting the statistical analysis.






eLetters
No eLetters have been published for this article.