To advance knowledge on schizoaffective disorder and whether its clinical course and outcome are more similar to schizophrenia or affective disorders (Reference Brockington and LeffBrockington & Leff, 1979; Reference Harrow and GrossmanHarrow & Grossman, 1984; Reference Van Praag and NijoVan Praag & Nijo, 1984; Reference MajMaj, 1989; Reference Marneros, Deister and RohdeMarneros et al, 1989, 1993; Reference McGlashan and WilliamsMcGlashan & Williams, 1990; Reference Kendler, McGuire and GruenbergKendler et al, 1995; Reference Stephens, Richard and McHughStephens et al, 1997), we conducted five successive assessments over a 10-year period of 210 patients with schizoaffective disorders, schizophrenia and affective disorders. We also provided balanced data to assess whether the presence of mood-incongruent psychotic symptoms at the acute phase has negative prognostic implications for subsequent course and outcome (Reference Coryell and TsuangCoryell & Tsuang, 1985; Reference Tohen, Tsuang and GoodwinTohen et al, 1992; Reference Fennig, Bromet and KarantFenning et al, 1996). The following questions were addressed. What is the clinical course and outcome for patients with schizoaffective disorders over a 10-year period? Is their course of illness more similar to that of patients with schizophrenia or affective disorders? Do mood-incongruent psychotic symptoms at the acute phase have negative prognostic significance?
METHOD
Patient sample
The current sample of 210 patients with research diagnostic criteria (RDC) diagnoses includes 36 patients with schizoaffective disorders, 70 patients with schizophrenia and control groups of 44 patients with psychotic affective disorders (26 with psychotic bipolar manic disorders and 18 with unipolar psychotic depression) and 60 patients with unipolar non-psychotic depression. The non-psychotic depression sample did not include patients with borderline diagnoses, anxiety disorders, severe anorexia, panic disorders, antisocial personality disorders, etc. The RDC diagnosis of schizoaffective disorder is similar in some ways to that of the ICD-10 (World Health Organization, 1992) diagnosis, with both diagnoses requiring the simultaneous presence of pronounced mood disorders (or full affective syndromes) and psychotic schizophrenic symptoms. The RDC diagnosis contains both inclusion and exclusion criteria. To form a control group for schizoaffective disorders, all patients with psychotic affective disorders were psychotic at the acute phase (i.e. they had delusions and/or hallucinations) and all had a full affective syndrome at the acute phase.
The sample is derived from the Chicago Follow-up Study, a rare sample of schizophrenia, schizoaffective, bipolar and other affective disorders studied prospectively at the acute phase and then studied longitudinally at successive follow-ups over many years. The investigation was planned to study prognosis, course and outcome longitudinally (Reference Grossman, Harrow and FudalaGrossman et al, 1984; Reference Harrow, Goldberg and GrossmanHarrow et al, 1990; Reference Grossman, Harrow and GoldbergGrossman et al, 1991; Reference Goldberg, Harrow and GrossmanGoldberg et al, 1995; Reference Harrow, Sands and SilversteinHarrow et al, 1997; Reference Sands and HarrowSands & Harrow, 1999) and to investigate factors involved in thought disorder and positive and negative symptoms on a longitudinal basis (Reference Grossman, Harrow and SandsGrossman et al, 1986; Reference Sands and HarrowSands & Harrow, 1994; Reference Harrow, MacDonald and SandsHarrow et al, 1995; Reference Harrow, Green and SandsHarrow et al, 2000).
The diagnoses were based on structured research interviews administered at index hospitalisation: the Schedule for Affective Disorders and Schizophrenia (SADS) and/or the Schizophrenia State Interview (see Reference Grinker and HarrowGrinker & Harrow, 1987). Using κ to assess interrater reliability for diagnosis for the largest group - the schizophrenia patients - we obtained κ=0.08.
At index hospitalisation the patients were consecutive or successive admissions within the limitation of giving preference to younger (17-30 years at index) patients with fewer previous hospitalisations. This was done to study relatively early young patients, thus diminishing the effects of long-term treatment and chronicity (Reference Grinker and HarrowGrinker & Harrow, 1987; Reference Harrow, Sands and SilversteinHarrow et al, 1997). Patients were assessed prospectively at index and then reassessed at four successive follow-ups (at 2, 4.5, 7.5 and 10 years after the index hospitalisation). Outcome data at the 10-year follow-up were available for slightly over 80% of the original sample studied as inpatients. Of the 210 patients in the current sample, all had a 10-year follow-up, with 191 (91%) having four successive follow-ups and the other 19 (9%) having three of the four follow-ups, including a 10-year follow-up. Within each diagnostic group, patients in the current sample did not differ significantly in age, education, gender distribution or number of pre-index hospitalisations from the subsample of patients who were assessed at the 2-year follow-up but not assessed at the 10-year follow-up. In addition, there were no significant differences at the 2-year follow-up on overall outcome, on working functioning or on rehospitalisations between the current sample of patients with schizoaffective disorders and the small subsample who also were assessed at the 2-year follow-ups but were not available for assessment at the 10-year follow-ups (P>0.20).
The mean age of the sample was 22.9 years at index hospitalisation. Seventy-two per cent had either one or no previous hospitalisations prior to index hospitalisation. The mean education level was 13.2 years at index. There were no significant age differences between the diagnostic groups. Written informed consent was obtained from all subjects.
Forty-seven per cent of the patients with schizoaffective disorder were women. A larger percentage of the patients with unipolar disorders were women and a larger percentage of the patients with schizophrenia were men. These gender differences are in accord with the typical, modern distribution of depression and schizophrenia.
Follow-up assessments
The sample was followed up at a mean of 2, 4.5, 7.5 and 10 years after initial assessment at index hospitalisation, using the SADS and the Harrow Functioning Interview (Reference Grinker and HarrowGrinker & Harrow, 1987; Reference Harrow, Sands and SilversteinHarrow et al, 1997).
To rate overall post-hospitalisation functioning and adjustment at each follow-up we employed the Levenstein-Klein-Pollack (LKP) scale (Reference Levenstein, Klein and PollackLevenstein et al, 1966) and a system to evaluate instrumental work performance and rehospitalisation developed by Strauss & Carpenter (Reference Strauss and Carpenter1972). The LKP scale has been used successfully by our research team and others (Reference Levenstein, Klein and PollackLevenstein et al, 1966; Reference Grinker and HarrowGrinker & Harrow, 1987; Reference Harrow, MacDonald and SandsGoldberg et al, 1995; Reference Harrow, Sands and SilversteinHarrow et al, 1997). The eight-point LKP scale takes into account work and social functioning, life adjustment, self-support, major symptoms, relapses and rehospitalisations. In assessing interrater reliability for the LKP scale, we obtained an intraclass correlation coefficient of r=0.92 (P<0.01). The LKP scale also allows for separation of the sample into three groups: good outcome, remission or recovery during the follow-up year (scores of 1 or 2), indicating adequate or near-adequate functioning in all areas in the past year; moderate impairment (scores of 3 to 6), indicating difficulties in some but not all areas of adjustment during the year; and uniformly poor outcome during the past year (scores of 7 or 8), indicating uniformly poor functioning, including poor psychosocial functioning and major symptoms. We found a correlation of r=0.85 (P<0.001) between the eight-point LKP scale and scores on the Global Assessment Scale, providing an indication that different outcome measures often tap similar concepts and produce similar results, although this does not guarantee validity.
The SADS data on psychosis at index hospitalisation were used to assess mood congruence or incongruence of psychotic symptoms for those patients who had both psychotic symptoms and a full affective syndrome (the patients with schizoaffective disorder and the patients with psychotic depression). We employed the definitions of mood congruence from DSM-III-R and DSM-IV (American Psychiatric Association 1987, 1994). Because many patients had both some mood-congruent and some mood-incongruent psychotic symptoms, the preponderance of mood congruence at index hospitalisation was determined by whether the majority of psychotic symptoms were mood congruent or incongruent (number of mood-congruent psychotic symptoms divided by total number of psychotic symptoms). This rating scale was applied at index to a subsample of 47 patients with schizoaffective (n=31) and psychotic affective disorders (n=16). Among the patients with schizoaffective disorders for whom complete assessments in this area were possible, all had some mood-incongruent psychotic symptoms and most (25/31 or 81%) had psychotic symptoms that were predominantly mood incongruent. Among 16 patients with psychotic depression most, but not all (9/16 or 56%), had psychotic symptoms that were predominantly mood congruent.
Statistical analysis
The data on overall outcome for the four diagnostic groups at the four successive follow-ups were analysed using a 4 × 4 (mixed design) repeated-measures analysis of variance (ANOVA), with diagnosis as a between-subjects factor and time as a within-subjects factor. One-way ANOVAs were conducted to test for differences between the diagnostic groups at each follow-up, with contrasts (cf. Reference Rosenthal and RosnowRosenthal & Rosnow, 1991) used to test predictions regarding the rank ordering of group performance in each analysis. Newman-Keuls post hoc analyses were also used to test differences between individual diagnostic groups. In some cases logistic regression analyses were used to test the relationship between diagnosis and outcome (Reference Hosmer and LemeshowHosmer & Lemeshow, 1989). Again, more specific hypotheses regarding the rank ordering of diagnostic group were tested via linear contrasts.
RESULTS
Overall outcome at four successive follow-ups
The mean scores on overall outcome at each of the four successive follow-ups for the patients with schizoaffective disorders and the comparison groups are depicted in Fig. 1. Analysis of the data from Fig. 1 indicated the following.
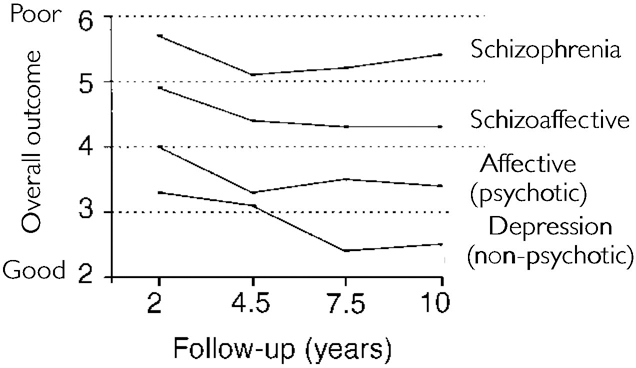
Fig. 1 Outcome for schizoaffective disorder, schizophrenia and affective disorder groups (Levenstein—Klein—Pollack scale) at four consecutive follow-ups.
-
(a) In the comparisons of overall outcome (using the eight-point LKP scale), the main effect for diagnosis in the 4 × 4 ANOVA showed statistically significant differences (F=22.83, d.f.=3, 187, P<0.001).
-
(b) The one-way ANOVAs on overall outcome for diagnosis showed statistically significant differences at each of the four follow-ups (P<0.001). Using Newman-Keuls post hoc tests, at each follow-up the patients with schizoaffective disorders showed significantly poorer outcome than those with non-psychotic depression (P<0.05). The patients with schizoaffective disorders also showed significantly better outcomes (P<0.05) than those with schizophrenia at the 7.5-year and 10-year follow-ups. They showed significantly poorer outcomes than the patients with psychotic affective disorders at the 4.5-year follow-up.
-
(c) A rank order of outcomes had been predicted for the four diagnostic groups, with successively better outcomes as one moved from schizophrenia to schizoaffective disorder to psychotic affective disorder to non-psychotic disorder. As can be seen in Fig 1, at each of the four follow-ups this exact rank order occurred for the four groups. Contrast analyses (Reference Rosenthal and RosnowRosenthal & Rosnow, 1991) assessing the fit of a linear model for the relationship between the four diagnostic groups was statistically significant (P<0.01) at each assessment.
-
(d) Only a limited number of patients with schizoaffective disorders showed complete recovery during each follow-up year (always less than 40%).
-
(e) Overall, the patients with schizoaffective disorders showed more favourable outcome than those with schizophrenia. At each of the four follow-ups fewer of the patients with schizoaffective disorders (28-37%) than with schizophrenia (40-52%) showed uniformly poor outcome. We used a logistic regression analysis (Reference Hosmer and LemeshowHosmer & Lemeshow, 1989) to test the relationship between diagnosis and uniformly poor outcome at each follow-up assessment, and used polynomial contrasts to assess the relationship between membership in each diagnostic group and uniformly poor outcome. The linear contrasts tested the hypothesis that patients with schizophrenia would have more uniformly poor outcome, followed by patients with schizoaffective disorders, psychotic affective disorders and finally non-psychotic disorders. At each of the four follow-ups diagnosis made a statistically significant contribution to outcome predictions, and the linear trend was significant (P<0.001).
Outcome and medication
At the 10-year follow-up 50% of the patients with schizoaffective disorders, 26% of those with non-schizophrenic psychotic disorders and 56% of those with schizophrenia were being treated with antipsychotic medication, either alone or in combination with other medication. At the 10-year follow-up 46% of the subsample of patients with bipolar manic disorders and 20% of those with schizoaffective disorders were on mood stabilisers. Similarly, at the 10-year follow-up 18% of the patients with non-psychotic depression were on antidepressants, as were 17% of those with schizoaffective disorders and 7% of those with psychotic affective disorders.
Comparisons of outcome for patients on antipsychotic medication with schizophrenia, schizoaffective disorders and psychotic affective disorders produced results similar to the comparisons found using the entire sample. Thus, at the 10-year follow-up, the patients with schizoaffective disorders who were on antipsychotic medication showed poorer outcome than those with psychotic affective disorders on antipsychotic medication and slightly better outcome than those with schizophrenia on antipsychotic medication. However, these differences were not statistically significant.
Comparisons of the subsample of patients not on any medication showed some similarity in results, with the patients with schizoaffective disorders showing slightly better outcome than those with schizophrenia but slightly poorer outcome than those with psychotic affective disorders. These differences were not statistically significant, partly due to the small sample sizes.
Instrumental work functioning and rehospitalisation over 10 years
Table 1 reports the mean scores on the Strauss-Carpenter Work Functioning and Rehospitalisation Scales for the four diagnostic groups at each follow-up.
Table 1 Instrumental work functioning and rehospitalisation for schizophrenia, schizoaffective disorder and affective disorder groups at four consecutive follow-ups over 10 years1

| Follow-up (years) | Diagnostic group | |||
|---|---|---|---|---|
| Schizophrenia (n=70) Mean (s.d.) | Schizoaffective disorder (n=36) Mean (s.d.) | Psychotic affective disorder (n=44) Mean (s.d.) | Non-psychotic affective disorder (n=60) Mean (s.d.) | |
| Work functioning | ||||
| 2 | 1.69 (1.66) | 2.29 (1.62) | 2.59 (1.73) | 3.34 (1.25) |
| 4.5 | 1.93 (1.71) | 2.43 (1.60) | 3.07 (1.35) | 3.13 (1.42) |
| 7.5 | 1.43 (1.57) | 2.14 (1.65) | 2.95 (1.40) | 3.29 (1.25) |
| 10 | 1.47 (1.73) | 2.47 (1.65) | 2.80 (1.61) | 3.38 (1.19) |
| Rehospitalisation | ||||
| 2 | 3.11 (1.10) | 3.40 (1.09) | 3.41 (1.07) | 3.51 (0.89) |
| 4.5 | 3.43 (0.89) | 3.34 (1.06) | 3.66 (0.68) | 3.72 (0.69) |
| 7.5 | 3.33 (1.11) | 3.66 (0.84) | 3.73 (0.54) | 3.76 (0.68) |
| 10 | 3.29 (1.08) | 3.49 (1.71) | 3.75 (0.49) | 3.80 (0.75) |
-
(a) An overall 4 × 4 repeated-measures ANOVA on instrumental work functioning showed large statistically significant diagnostic differences (F=23.69, d.f.=3, 185, P<0.0001).
-
(b) One-way ANOVA and post hoc analyses on work functioning, comparing the four diagnostic groups, showed statistically significant diagnostic differences at all four follow-ups. Patients with schizoaffective disorders showed significantly poorer work functioning than those with non-psychotic affective disorders at all four follow-ups (P<0.05).
-
(c) The patients with schizoaffective disorders did not show as poor work functioning as those with schizophrenia. The difference in work performance (Strauss-Carpenter scale) was statistically significant at both the 7.5-year and the 10-year follow-ups.
-
(d) There were differences between the schizoaffective and the psychotic affective disorders (in terms of significantly poorer work functioning by the patients with schizoaffective disorders) at the 7.5-year follow-up, but overall these differences were not as consistent as the comparison with the patients with schizophrenia.
-
(e) A 4 × 4 repeated-measures ANOVA on rehospitalisation showed statistically significant diagnostic differences (F=4.82, d.f.=3, 185, P<0.01).
-
(f) One-way ANOVAs on rehospitalisation and subsequent Newman-Keuls tests indicated significantly less rehospitalisation for the non-psychosis patients but fewer differences between the patients with schizoaffective disorders versus those with schizophrenia and psychotic affective disorders.
-
(g) However, the patients with schizoaffective disorders were rehospitalised significantly less frequently than those with schizophrenia at the 2-year follow-ups and showed statistically non-significant trends towards fewer rehospitalisations at the 7.5-year and 10-year follow-ups.
Schizoaffective disorder and acute-phase mood-incongruent psychotic symptoms: prognostic significance
Figure 2 presents data on potential differences in later outcome between patients with psychotic and affective disorders who, during the acute phase at index hospitalisation, had a predominance of mood-incongruent psychotic symptoms compared with patients with a predominance of mood-congruent psychotic symptoms.
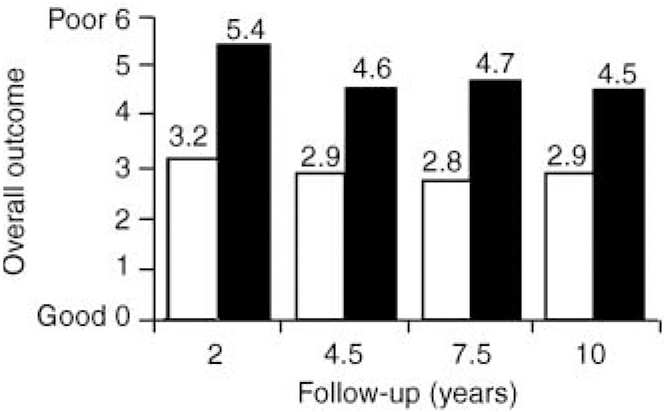
Fig. 2 Ten-year outcome for patients who, at the acute phase, had affective disorders and either mood-congruent or mood-incongruent psychotic symptoms: □ congruent; ▪ incongruent.
-
(a) The data on overall outcome were analysed using a 2 × 4 (mixed design) repeated-measures ANOVA. This ANOVA showed large statistically significant differences in outcome between the mood-incongruent and mood-congruent groups (F=9.91, d.f.=1, 42, P<0.01).
-
(b) Mean scores on outcome for the two groups are reported in Fig. 2. Post hoc tests at each follow-up indicated that patients with predominantly mood-incongruent psychotic features at index hospitalisation showed significantly poorer outcomes than patients with mood-congruent psychotic symptoms (P<0.05).
-
(c) At each follow-up, patients with mood-incongruent psychotic symptoms showed significantly poorer work functioning (P<0.05).
-
(d) Unlike the data on overall outcome, there were no statistically significant differences between patients with predominantly mood-incongruent and mood-congruent symptoms in extent of subsequent psychosis at any of the four follow-ups.
DISCUSSION
The major questions posed involve the outcome and clinical course of schizoaffective disorders. Prospective data on large samples of young patients from diverse diagnostic groups involving multiple assessments over a 10-year period have been rare in the literature.
Overall outcome at four successive follow-ups over 10 years
On some outcome dimensions the patients with schizoaffective disorders looked more like those with psychotic affective disorders and on other dimensions they looked more like those with schizophrenia. Thus, unlike the psychotic affective disorders, at each follow-up year only a limited number of patients with schizoaffective disorders (less than 40%) showed complete recovery.
The overall outcome of the patients with schizoaffective disorders was consistently better than that of those with schizophrenia and poorer than that of those with psychotic affective disorders over the 10-year period. The mean outcome scores for schizoaffective disorders lay between those for schizophrenia and the psychotic affective disorders.
Uniformly poor outcome
Although uniformly poor outcome was extremely prominent for many patients with schizophrenia, at each follow-up a larger percentage of schizoaffective than psychotic affective or non-psychotic disorders showed uniformly poor outcome. The linear ranking of the four diagnostic groups in the logistic regression analysis (schizophrenia, schizoaffective disorders, psychotic affective disorders and non-psychotic depression) best accounted for variance in the contribution of diagnosis to poor outcome (P<0.01).
These and other data (Grossman et al, Reference Grossman, Harrow and Fudala1984, Reference Grossman, Harrow and Goldberg1991) suggest that fewer patients with schizoaffective disorders and some of those with psychotic depression show the uniformly poor outcome in multiple areas shown by a number of those with schizophrenia.
Does acute-phase psychosis matter?
The current data indicating large differences in outcome between patients with schizoaffective disorders (who initially had an affective syndrome) and those with non-psychotic depression (who also had an affective syndrome) are not in accord with proposals that de-emphasise the importance of psychotic symptoms.
The large significant differences in course and outcome between patients with schizoaffective disorders and those with unipolar non-psychotic depression fit with theoretical views suggesting the importance of delusions and psychosis (Reference Bentall, Jackson and PilgrimBentall, 1988; Reference BrockingtonBrockington, 1991; Reference Harrow, MacDonald and SandsHarrow et al, 1995), and with data indicating poorer outcome for patients with schizophrenia and those with psychotic affective disorders compared with those with non-psychotic depression. The current data and other data (Reference Sands and HarrowSands & Harrow, 1994; Reference Harrow, MacDonald and SandsHarrow et al, 1995) suggest that patients with psychotic symptoms at the acute phase are more vulnerable to subsequent recurrence of psychosis and subsequent difficulties in outcome.
Does mood-incongruent psychosis matter?
Although the data indicate that psychosis is a risk factor, the issue of the prognostic significance of mood-incongruent psychotic symptoms is also important and is closely linked to basic issues about schizophrenia and schizoaffective disorders. The present research investigated whether poor outcome for patients with schizoaffective disorders and some patients with psychotic depression is associated with their vulnerability to mood-incongruent psychotic symptoms.
Previous research (Reference Coryell and TsuangCoryell & Tsuang, 1985; Reference Tohen, Tsuang and GoodwinTohen et al, 1992; Reference Davies and HarrowDavies & Harrow, 1994) has suggested that the presence of mood-incongruent, schizophrenic-like psychotic symptoms at initial acute hospitalisation may mark a potential vulnerability to poor outcome, both in patients with schizoaffective disorders who have major affective symptoms and in those with schizophrenia who do not have major affective symptoms during acute hospitalisation.
The current data support the hypothesis that patients with a predominance of mood-incongruent psychotic symptoms are more vulnerable to subsequent outcome difficulties in other areas. Surprisingly, the results did not show more subsequent psychosis by patients with mood-incongruent psychotic symptoms. This is in accord with other data on the presence of mood-incongruent psychotic symptoms (Reference Davies and HarrowDavies & Harrow, 1994).
It is possible that the presence of acute-phase psychotic symptoms indicates a trait-like tendency to subsequent psychosis (Reference Harrow, MacDonald and SandsHarrow et al, 1995), but this tendency may not be increased by the presence of mood-incongruent psychotic symptoms. Rather, mood-incongruent psychotic symptoms may be associated with personal vulnerabilities that can negatively influence later adjustment and dysfunction in multiple areas other than psychosis, and may affect the severity of subsequent psychotic symptoms when they do occur (Reference Harrow, MacDonald and SandsHarrow et al, 1995).
Symptom dimension view of schizoaffective outcome
An alternative outlook to help account for the results obtained on outcome of patients with schizoaffective disorders over time involves a dimensional view of symptoms (Reference Bentall, Jackson and PilgrimBentall et al, 1988; Reference Bentall and BentallBentall, 1990; Reference Costello and CostelloCostello, 1993; Reference Harrow, MacDonald and SandsHarrow et al, 1995). This approach de-emphasises the importance of specific diagnostic labels (such as schizoaffective disorder, schizophrenia and psychotic affective disorder) and instead focuses on major symptoms such as psychosis, affective syndromes and mood-incongruent delusions.
Using this view, which de-emphasises diagnosis and focuses on separate features and symptoms, psychosis (associated with poor prognosis), affective symptoms (at the acute phase traditionally associated with more favourable prognosis for psychotic patients) and mood-incongruent psychotic symptoms (a negative prognostic feature) are seen as symptom dimensions that can account for some of the variance associated with functioning and outcome years later. Thus, at the acute phase, patients with schizophrenia have negative features on all three of these dimensions, patients with schizoaffective disorders have negative features on two of them, patients with psychotic affective disorders have negative features on one of them and patients with non-psychotic affective disorders have negative features on none of them. Outcome predictions from this constellation of symptoms match the results obtained at all four follow-ups from the contrast analysis presented in the Results. Overall, if one adopts a symptom dimension view concerning the major aspects of psychopathology, the model accounts for some of the outcome differences that emerged. The most promising view could be an outlook that utilises a combination approach in which both diagnosis and symptom dimensions are important, with each involving factors contributing to major features of outcome. However, functioning and outcome are obviously complex variables with multiple determinants.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The presence of mood-incongruent psychotic symptoms in patients with schizoaffective disorders and those with psychotic depression have negative prognostic implications.
-
▪ Disorders involving psychotic symptoms at the acute phase are more vulnerable to subsequent recurring psychosis and subsequent difficulties in course and outcome adjustment.
-
▪ Although a number of patients with schizophrenia show uniformly poor outcome, not as many patients with schizoaffective disorders show this.
LIMITATIONS
-
▪ In a prospective research design involving successive follow-ups over time, it would have been preferable to have looked at outcome every year instead of every 2.5 years over the 10-year period.
-
▪ It is unclear whether non-psychotic disorders without affective syndromes would have the same source and outcome as the current control sample of patients with psychotic affective disorders.
-
▪ It is unclear whether an older, more chronic, schizoaffective sample might have .






eLetters
No eLetters have been published for this article.