Structural brain imaging studies in schizophrenia have demonstrated several abnormalities, particularly of the temporal lobes and constituent parts, both in people with established disease and in first-episode patients (Reference Suddath, Christison and TorreySuddath et al, 1990; Reference Shenton, Kikinis and JoleszShenton et al, 1992; Reference Lawrie and AbukmeilLawrie & Abukmeil, 1998; Reference Lawrie, Whalley and KestelmanLawrie et al, 1999; Reference Wright, Rabe-Hesketh and WoodruffWright et al, 2000). This has generally been interpreted as indicating that the brain changes are present early in life, but the timing is unknown. The Edinburgh High-Risk Study was designed to address this uncertainty. Participants were recruited as adolescents, having at least two affected relatives. Structural magnetic resonance imaging (MRI) of the brain at baseline revealed that the mean volumes of the amygdala—hippocampus complex in the brains of people at high risk were smaller than those of healthy participants but larger than in first-episode patients (Lawrie et al, Reference Lawrie, Whalley and Kestelman1999, Reference Lawrie, Whalley and Abukmeil2001). We scanned subgroups of high-risk and healthy control participants on two occasions about 2 years apart. Some of the high-risk participants had experienced psychotic symptoms during this time, several at baseline assessment. We therefore test two hypotheses in this report. First, we determined whether people at high risk generally show a reduction in the volumes of the temporal lobes and amygdala—hippocampus over time compared with a healthy control group. Second, we examined whether these structures reduced in volume in high-risk participants with psychotic symptoms.
METHOD
Ethical approval was obtained from all relevant health boards and enrolment began in 1995. After a complete description of the study had been given to participants, their written informed consent was obtained.
Participants
Details of the recruitment process have been described in previous papers (Reference Hodges, Byrne and GrantHodges et al, 1999; Reference Johnstone, Abukmeil and ByrneJohnstone et al, 2000). Briefly, individuals with schizophrenia, with a family history of schizophrenia and with adolescent relatives, were identified from psychiatric hospital case records in most areas of Scotland. Case-note diagnoses of schizophrenia were verified with the Operational Criteria Checklist (Reference McGuffin, Farmer and HarveyMcGuffin et al, 1991). We then approached their relatives, and high-risk subjects aged 16-25 who agreed to participate were given a detailed clinical, neuropsychological and brain imaging assessment. The clinical assessment included the Present State Examination (PSE, ninth edition), a structured psychiatric interview schedule which has been widely used in studies of schizophrenia (Reference Wing, Cooper and SartoriusWing et al, 1974). All these assessments were repeated after approximately 2 years in consenting participants who had enrolled in the first 2 years of the study.
A control group of healthy individuals without any family history of schizophrenia was recruited from the same areas of Scotland as the high-risk participants. These people were of similar age to the high-risk group and their numbers were comparable to the number of people expected to develop psychosis. Members of the control group were fully examined as above and consenting individuals reassessed after approximately 2 years.
Symptom measures
At each clinical assessment, psychotic and other symptoms were identified and measured on a videotaped PSE. Participants were initially divided into five groups on the basis of symptom severity (Reference Johnstone, Abukmeil and ByrneJohnstone et al, 2000):
-
• 0 — no symptom
-
• 1 — any fully rated non-psychotic symptom or behavioural item
-
• 2 — partially rated psychotic symptoms (mainly isolated perceptual disturbances or partially held delusions) or behaviours
-
• 3 — any fully rated psychotic symptoms (hallucinations and delusions) or behaviour
-
• 4 — schizophrenia diagnosed according to PSE and ICD-10 (World Health Organization, 1992) criteria.
For statistical analysis groups rated 0/1 and 2/3 were collapsed (absence or presence of psychotic symptoms), and those who developed schizophrenia before the second scan could not be included as they only had one scan. It should be noted that some of the high-risk participants had partially or fully rated psychotic symptoms at intake (n=12), but most were working or studying productively and none had schizophrenia or any other psychotic disorder. By 1999, a relatively small number of the whole cohort (n=7) had gone on to meet diagnostic criteria for schizophrenia and we are thus not yet able to examine the predictors and associations of psychosis per se. We should also stress that the current analyses were pre-planned, as were similar analyses of the neuro-psychological data (Reference Cosway, Byrne and ClaffertyCosway et al, 2000), as part of the first phase of the study (Reference Miller, Byrne and HodgesMiller et al, 2002).
Brain scanning
Details of the image acquisition and processing are given elsewhere (Reference Whalley, Kestelman and RimmingtonWhalley et al, 1999). Briefly, participants underwent MRI scanning on a 1T Magnetom scanner (Siemens, Erlangen, Germany). Midline sagittal localisation was followed by a double spin echo sequence to identify any gross brain lesions and a fast gradient echo sequence for volumetric analysis. The latter consisted of a 180° inversion pulse followed by a FLASH (fast low angle shot) collection (flip angle 12°, repetition/echo/inversion times=10/4/200 ms, relaxation delay time 500 ms, field-of-view 250 mm). This gave 128 contiguous 1.88 mm thick slices in the coronal plane. Semi-automated quality control checks of the signal-to-noise ratio and radio frequency field homogeneity were made daily. Inhomogeneity in the head coil was corrected for by scanning a flood phantom after each scan and normalising the data to this. Repeat scans were conducted on the same scanner, with exactly the same imaging protocol, after approximately 2 years. The scanner was not modified during the study.
Images were processed on Sun Micro-systems workstations using the software package Analyze (version 7.5, Mayo Foundation, Rochester, Minnesota, USA). Seeds were placed in regions of interest, thresholds adjusted by eye and limits placed manually to separate adjoining structures. The temporal lobes and amygdala—hippocampus complex volumes were defined according to the criteria of Suddath et al (Reference Suddath, Christison and Torrey1990) and Shenton et al (Reference Shenton, Kikinis and Jolesz1992). The temporal lobe measurements started at the temporal pole, the amygdala—hippocampus complex volume measurements were commenced when the temporal stem white matter was first observable, and the posterior boundary for both was taken as the first slice in which the crus fornicis fibres formed the medial wall of the lateral ventricle. The posterior boundary of the prefrontal lobes was taken as the first slice of the corpus callosum. Other structures were outlined by standard criteria or naturalistic boundaries as in our previous studies (Lawrie et al, Reference Lawrie, Whalley and Kestelman1999, Reference Lawrie, Whalley and Abukmeil2001; Reference Whalley, Kestelman and RimmingtonWhalley et al, 1999) for exploratory analyses.
Volumetric image processing was performed by three raters (H. C. W., S. S. A., J. N. K.) with good interrater reliability: mean intraclass correlation coefficient 0.92, range 0.78-0.99. The main rater (H. C. W.) also measured her intrarater reliability every 6 months (mean intraclass correlation coefficient 0.94, range 0.80-1.00). Measurement error was quantified by dividing the mean difference between a pair of ratings by the mean volume of the two. Expressed as a percentage, the mean error over time was less than 1% for the whole brain and temporal lobes, 3.2% for the amygdala—hippocampus and 1.7-5.5% for the remaining structures other than the third ventricle (Reference Whalley, Kestelman and RimmingtonWhalley et al 1999). The scans were identified by code number and date of birth only, so that the raters were masked to group membership.
Statistical analysis
All statistical testing was conducted using the Statistical Package for the Social Sciences (SPSS version 10.0 for PC). Demographics were compared between groups with analysis of variance and the chisquared test. In the high-risk group, symptom ratings on the PSE were scored as the highest symptom levels over the first 5 years of the study, dichotomised into groups of 0/1 (no psychotic symptoms ever) and 2/3 (psychotic symptoms). Any differential change over time in the high-risk and healthy control groups was examined with repeated measures analysis of variance (ANOVA), looking for group × time interactions. The same test was employed to compare change in high-risk individuals with and without symptoms. The mean absolute change in regional volumes was calculated as the mean difference between the two scans (scan 2—scan 1), such that a negative value indicates volume reduction. Relative change as a percentage was calculated with reference to the appropriate volume on the first scan, i.e. ([scan 2—scan 1]/scan 1) × 100.
RESULTS
Changes in regional brain volumes over time
Second scans were performed in 66 high-risk and 20 healthy participants an average of 1.8 (s.d.=0.4) years after the first assessment. The mean ages of the two groups were almost identical and there were no significant differences in the other descriptive variables (Table 1). Repeated measures ANOVA revealed no statistically significant group × time interactions. There were no significant differences in volume changes between control and high-risk participants in the left (F 1,84=2.9, P=0.09) and right (F 1,84=2.2, P=0.14) amygdala—hippocampus, nor in the left (F 1,84=2.3, P=0.13) and right (F 1,84=0.1, P=0.7) temporal lobes. The absolute and relative changes in these and other regional brain volumes in the two groups are listed in Table 2.
Table 1 Demographic characteristics of high-risk and control study participants
| High-risk group (n=66) | Control group (n=20) | P | |
|---|---|---|---|
| Mean age at second assessment (years) | 23.1 (s.d.=2.7) | 22.9 (s.d.=2.2) | 0.8 |
| Gender (male/female) | 34/32 | 13/7 | 0.3 |
| Mean height (cm) | 172.3 (s.d.=10.6) | 173.0 (s.d.=10.5) | 0.8 |
| Handedness (right/left/mixed) | 57/6/3 | 16/2/2 | 0.6 |
| Paternal social class: | 0.3 | ||
| Non-manual | 31 | 13 | |
| Manual | 33 | 7 | |
| Unknown | 2 | — |
Table 2 Mean absolute and relative changes in regional brain volumes in 66 high-risk and 20 control participants
| Region | Absolute change (scan 2 — scan 1) mean (s.d.) | Relative change ([scan 2 — scan 1]/scan 1) × 100 | ||
|---|---|---|---|---|
| High-risk (mm3) | Control (mm3) | High-risk (%) | Control (%) | |
| Brain | -2060 (35 590) | +3152 (31 378) | -0.2 | +0.3 |
| Third ventricle | -87 (158) | -96 (159) | -10.0 | -20.3 |
| Fourth ventricle | -134 (217) | -124 (208) | +0.2 | -15.8 |
| Left lateral ventricle | -434 (839) | -365 (702) | -7.5 | -11.0 |
| Right lateral ventricle | -399 (838) | -389 (793) | -4.7 | -11.3 |
| Left amygdala—hippocampus complex | -126 (445) | -321 (468) | -2.2 | -5.7 |
| Right amygdala—hippocampus complex | +116 (499) | -70 (464) | +3.5 | -1.2 |
| Left temporal lobe | -1063 (4290) | -2640 (3044) | -1.2 | -3.1 |
| Right temporal lobe | -692 (3373) | -991 (4205) | -0.8 | -1.1 |
| Left prefrontal lobe | -204 (5217) | +1034 (4976) | +0.1 | +1.0 |
| Right prefrontal lobe | +841 (5967) | +1044 (5967) | +1.6 | +1.3 |
| Left thalamus | -113 (661) | -348 (538) | -0.8 | -4.7 |
| Right thalamus | -114 (569) | -202 (465) | -1.2 | -3.0 |
| Left caudate | +45 (285) | -42 (354) | +1.3 | -0.4 |
| Right caudate | +53 (326) | +6 (302) | +1.5 | +0.3 |
| Left lenticular nucleus | +114 (570) | +36 (431) | +2.7 | +1.2 |
| Right lenticular nucleus | +98 (520) | +195 (473) | +2.3 | +4.1 |
Changes in regional brain volumes by symptoms
Nineteen of the high-risk participants had psychotic symptoms (12 at baseline) and 47 did not. The demographic characteristics of these two groups are given in Table 3. Women and shorter individuals were non-significantly overrepresented in the high-risk group with symptoms. There was little difference in the time between scans in the two groups: 1.7 (s.d.=0.2) years and 1.8 (s.d.=0.5) years, respectively.
Table 3 Demographic characteristics of high-risk participants with and without psychotic symptoms
| High-risk with symptoms (n=19) | High-risk without symptoms (n=47) | P | |
|---|---|---|---|
| Mean age at second assessment (years) | 23.0 (s.d.=2.7) | 23.2 (s.d.=2.7) | 0.7 |
| Gender (male/female) | 7/12 | 27/20 | 0.1 |
| Mean height (cm) | 169.5 (s.d.=9.6) | 173.4 (s.d.=10.9) | 0.2 |
| Handedness (right/left/mixed) | 18/0/1 | 39/6/2 | 0.3 |
| Paternal social class: | 0.3 | ||
| Non-manual | 6 | 25 | |
| Manual | 12 | 21 | |
| Unknown | 1 | 1 |
Repeated measures ANOVA found one significant group × time interaction, in the right temporal lobe (F 1,64=5.4,P=0.023). There was no significant interaction in the left (F 1,64=0.2, P=0.7) or right (F 1,64=0.7, P=0.4) amygdala—hippocampus, or in the left temporal lobe (F 1,64=1.0, P=0.3). Table 4 lists the absolute and relative changes in regional volumes in the two groups. The mean absolute reduction in the right temporal lobe in high-risk individuals with symptoms was 2163 mm3 compared with a reduction of 97 mm3 in those without symptoms. These represent relative reductions of 2.5% and 0.04%, respectively (Fig. 1). There are similar reductions in volume in the left temporal lobe (2.3% and 0.8%, respectively). The differences in absolute and relative changes are similar or greater in other structures such as the left and right prefrontal lobes, but the measurement error and variance are also higher.
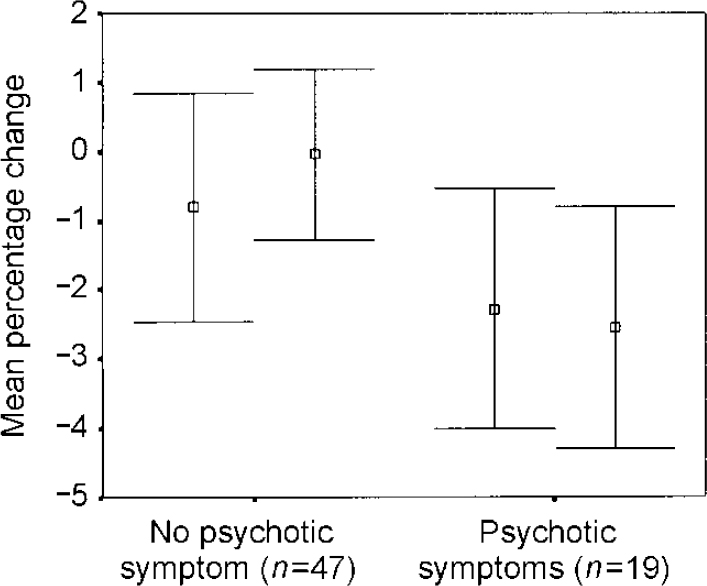
Fig. 1 Error bar plot (mean and 95% confidence interval) of relative (percentage) changes in the left and right temporal lobe volumes in 47 asymptomatic high-risk individuals and 19 individuals with psychotic symptoms.
Table 4 Mean absolute and relative changes in regional brain volumes in 19 high-risk participants with psychotic symptoms and 47 high-risk participants without psychotic symptoms
| Region | Absolute change (scan 2—scan 1) mean (s.d.) | Relative change ([scan 2—scan 1]/scan 1) × 100 | ||
|---|---|---|---|---|
| Symptoms (n=19) (mm3) | No symptoms (n=47) (mm3) | Symptoms (n=19) (%) | No symptoms (n=47) (%) | |
| Brain | -12 616 (31 302) | +2207 (36 331) | -0.9 | +0.2 |
| Third ventricle | -55 (145) | -100 (162) | +6.1 | -16.5 |
| Fourth ventricle | -86 (217) | -154 (216) | -9.7 | +4.2 |
| Left lateral ventricle | -428 (906) | -437 (821) | -1.1 | -10.0 |
| Right lateral ventricle | -423 (941) | -389 (803) | +1.4 | -7.1 |
| Left amygdala—hippocampus complex | -87 (492) | -141 (429) | -1.3 | -2.6 |
| Right amygdala—hippocampus complex | +32 (565) | +150 (472) | +1.5 | +3.8 |
| Left temporal lobe | -1901 (3050) | -723 (4685) | -2.3 | -0.8 |
| Right temporal lobe | -2163 (3093) | -97 (3328) | -2.5 | -0.04 |
| Left prefrontal lobe | -334 (4868) | -151 (5401) | -0.3 | +0.3 |
| Right prefrontal lobe | -718 (5845) | +1471 (5961) | -0.4 | +2.4 |
| Left thalamus | +68 (573) | -186 (685) | +2.4 | -2.2 |
| Right thalamus | +74 (473) | -190 (591) | +2.1 | -2.5 |
| Left caudate | -41 (292) | +79 (278) | -0.7 | +2.1 |
| Right caudate | -68 (324) | +102 (317) | -1.1 | +2.5 |
| Left lenticular nucleus | -20 (634) | +168 (540) | +0.2 | +3.7 |
| Right lenticular nucleus | -65 (633) | +165 (457) | -0.6 | +3.4 |
A post hoc repeated measures ANOVA of a group × time × gender interaction for the right temporal lobe volumes in high-risk participants was not significant (P=0.5). Neither of the high-risk groups significantly differed from the control group in the changes in right temporal lobe volume. The high-risk participants with psychotic symptoms at baseline and those who developed psychotic symptoms subsequently also did not differ significantly on this measure. As the numbers in the three main subject groups were unequal, we conducted paired t-tests for within-group changes in temporal lobe volumes: both left and right sides showed statistically significant reductions in those with symptoms (bothP<0.015) but not in those without (both P>0.25), and the brains of control subjects showed significant reductions only on the left side.
DISCUSSION
Main findings
We did not find evidence to support our first hypothesis, of a reduction in temporal lobe volumes in all high-risk individuals, as the control group showed non-significantly greater reductions. Our findings are, however, in keeping with our second hypothesis, as the right temporal lobes reduced in volume in high-risk participants with psychotic symptoms. This suggests that brain structure may change in association with psychotic symptoms.
Methodological considerations
This novel finding is unlikely to be artefactual. We tested two specific hypotheses — although we did so for bilateral structures in two different contrasts, these were not independent and would not, therefore, be suitable for a Bonferroni correction. The volume calculations were done by masked raters with good inter— and intrarater reliabilities, and measurement error was less than the main difference we found. High-risk participants with and without symptoms did not substantially differ in descriptive variables; the greatest difference was in gender distribution, but we found no symptom × time × gender interaction.
The results do, however, need cautious interpretation. We analysed the data by symptoms rather than psychosis both to optimise statistical power and because the causes of symptom development in schizophrenia are so poorly understood. It is not therefore possible to state whether these results apply to those who will develop psychosis rather than individual psychotic symptoms, although the symptomatic participants had at least partial or isolated delusions or hallucinations and the diagnosis of schizophrenia is largely made on the grounds of these symptoms. We do not expect all the high-risk group with individual psychotic symptoms to develop frank schizophrenia, and symptoms fluctuate over time for unknown reasons. We are also not able to state whether the changes in brain structure precede or follow symptoms, as many of the symptomatic high-risk individuals had symptoms at baseline assessment. It is unlikely that the symptoms themselves effect volume reductions, but even if the temporal lobe reductions are primary, an explanation is required.
The measurement error of the volumetric technique we used is more likely to have obscured differences where they actually existed rather than to lead to false positive results. This is a possible explanation for our failure to find volume reductions in the amygdala—hippocampus in high-risk participants, particularly those with psychotic symptoms. Measurement error is in the region of 5% for these and other relatively small structures. Our previous findings of reduced amygdala—hippocampus volumes at baseline could imply that those with the smallest volumes would be most likely to develop symptoms, but this is not the case — at least thus far (Reference Lawrie, Whalley and AbukmeilLawrie et al, 2001). Alternatively, the reduced volumes of the amygdala—hippocampus complex usually found in schizophrenia may only be manifested with the onset of psychosis per se.
Imaging brain development
The imaging literature on development changes in brain structure is relatively sparse. Most brain development is completed in the first few postnatal months, but competitive elimination of synapses, axonal myelination and dendritic arborisation continue throughout life (Reference HuttenlocherHuttenlocher, 1990; Reference Bourgeois and Goldman-RakicBourgeois & Goldman-Rakic, 1994; Reference Jernigan, Sowell, Keshavan and MurrayJernigan & Sowell, 1997). Some MRI studies have found age-related reductions inT 2-weighted signal suggestive of myelinatioin throughout the hemispheres in adolescence and early adulthood (Reference Jernigan, Sowell, Keshavan and MurrayJernigan & Sowell, 1997). We are aware of only three MRI studies employing similar measures of regional brain volumes in control groups of similar age to our own, two from the same research group in an overlapping sample, which suggest that the frontal and temporal lobes reduce in size during early adulthood (Reference Jernigan, Sowell, Keshavan and MurrayJernigan & Sowell, 1997; Reference Bartzokis, Beckson and LuBartzokis et al, 2001), possibly due to ‘synaptic pruning’. Automated voxel-based morphometry studies support these findings, but suggest the reductions are greater in the frontal lobes (Reference Giedd, Blumenthal and JeffriesGiedd et al, 1999; Reference Sowell, Thompson and HolmesSowell et al, 1999). Our results in healthy control participants are compatible with these findings, particularly if measurement error is taken into account. This could also explain the apparent reductions over time of ventricular volumes in the control group, but it is uncertain whether ventricular volumes begin to increase from the age of 20 years (Reference Jernigan, Trauner and HesselinkJernigan et al, 1991) or 30 years (Reference Pfefferbaum, Mathalon and SullivanPfefferbaumet al, 1994) in healthy individuals.
These processes do not appear from our current data to differ significantly in all the high-risk participants, or in either of the high-risk groups, compared with the healthy control group. We cannot, therefore, determine whether the reductions in the temporal lobes in symptomatic high-risk individuals are attributable to physiological or pathological processes. The patterns of change in the temporal lobes are similar in the symptomatic high-risk and control groups, suggesting that the development of symptoms may be triggered by physiological events in the otherwise predisposed (Reference FeinbergFeinberg, 1982; Reference WeinbergerWeinberger, 1987). It should be noted, however, that whole-brain volume and prefrontal lobe reductions are only apparent in the high-risk group with symptoms, which suggests that ‘synaptic pruning’ may be more widespread in these people but greatest in the temporal lobes. It should also be noted that post-mortem studies do not always find reductions of the amygdala—hippocampus and prefrontal lobes in schizophrenia (Reference HarrisonHarrison, 1999).
Clinical implications
Structural MRI studies have reported that abnormalities of the hemispheres (Reference DeLisi, Sakuma and TewDeLisi et al, 1997) and temporal lobes (Reference Rapoport, Giedd and BlumenthalRapoport et al, 1999) may progress in the first few years after the onset of schizophrenia in patients of similar ages to our study group and at a similar rate (about 1% per year). Other studies have, however, localised changes to the frontal lobes (Reference Gur, Cowell and TuretskyGur et al, 1998) or found them to be limited to the lateral ventricles in poor-outcome subgroups (Reference Lieberman, Chakos and WuLieberman et al, 2001). These changes could be due to antipsychotic medication effects, but none of the high-risk participants reported here was taking such medication when assessed or, indeed, at any previous time. The differences between reports may reflect differential measurement errors in semi-automated studies, and we are currently engaged in an entirely automated comparison. As far as psychotic symptoms can be localised, temporal lobe abnormalities have been linked to auditory hallucinations similar to those described by our high-risk participants (Reference Shenton, Kikinis and JoleszShenton et al, 1992; Reference Lawrie and AbukmeilLawrie & Abukmeil, 1998). We cannot tell from the present analysis whether particular parts of temporal lobes are reducing or whether reductions represent a general loss of temporal lobe tissue, but we are currently using more detailed techniques to determine this and any specific relationships with particular psychotic symptoms. These novel analytical methods may be sufficiently sensitive for clinical use.
Our scanning results are compatible with our neuropsychological findings, in the same study group, of a decline in memory (and executive) function as psychotic symptoms develop (Reference Cosway, Byrne and ClaffertyCosway et al, 2000). It may be that the development of psychotic symptoms is triggered by one or more processes associated with reduction in temporal lobe volume and that the processes lead to the development of a psychotic illness and continuing reduction in temporal lobe volumes in at least some people. These findings therefore raise the possibility that people destined to develop schizophrenia might be identifiable before (or at least while) the disorder develops, and might potentially benefit from treatment with antipsychotic or even neuroprotective drugs.
CLINICAL IMPLICATIONS
-
• Some abnormalities of brain structure in schizophrenia may precede the onset of schizophrenia.
-
• Reductions in temporal lobe volumes could conceivably predict the onset of schizophrenia.
-
• These findings suggest possibilities for early detection.
LIMITATIONS
-
• The number of high-risk participants in this study who have developed schizophrenia is, as yet, too small to determine if these findings hold in this group.
-
• Measurement error may have obscured changes in the amygdala—hippocampus.
-
• Temporal lobe reductions were similar in the control group.
Acknowledgements
This study was supported by the Medical Research Council of Great Britain. We thank Majella Byrne, Bobby Clafferty, Richard Cosway, Elizabeth Grant, Ann Hodges and Jane Morris for their help in acquiring the sample; Annette Blane and Ewen Rimmington for acquiring the brain scans and correcting for inhomogeneity; general practitioners and psychiatrists throughout Scotland; and the participants and their extended families. We also thank Norma Brearley for the careful preparation of the manuscript.








eLetters
No eLetters have been published for this article.