Depression is a leading cause of disability worldwide, with postpartum depression being a long-standing public health problem affecting women, their children and partners globally.Reference Howard, Molyneaux, Dennis, Rochat, Stein and Milgrom1–Reference Stein, Pearson, Goodman, Rapa, Rahman and McCallum3 Although effectively treated with pharmacotherapy or psychotherapy, women with mood disorders prefer psychotherapy threefold over medication.Reference McHugh, Whitton, Peckman, Welge and Otto4 Interpersonal psychotherapy (IPT) is an effective, time-limited structured depression treatment that is recommended in consensus guidelines.5–Reference Weissman, Markowitz and Klerman7 IPT's relationally and affective-focused approach is salient to postpartum women, with its therapeutic focus on the interpersonal context of depression, stressful life changes and unsatisfying relationships.Reference Miniati, Callari, Calugi, Rucci, Savino and Mauri8–Reference Stuart and Robertson12 Numerous barriers limit access to evidence-supported psychotherapies for postpartum depression, including the availability of mental health specialists, stigma, time availability, childcare needs and geographical barriers, especially in underserved rural areas. Most women experiencing postpartum depression remain untreated, with fewer than 20% pursuing treatment.Reference Ko, Farr, Dietz and Robbins13 Thus, different treatment delivery approaches are needed to improve equitable access and outcomes, including the use of non-specialist health workers such as nurses, who can be trained to provide effective psychotherapy in mental healthcare services.Reference van Ginneken, Tharyan, Lewin, Rao, Meera and Pian14
The majority of IPT studies establishing its efficacy as a treatment for postpartum depression have been delivered in a traditional face-to-face format by mental health specialists.Reference O'Hara, Stuart, Gorman and Wenzel15–Reference Grote, Swartz, Geibel, Zuckoff, Houck and Frank18 An alternative is telephone delivery, an under-utilised format for psychotherapies with considerable efficacy in depression treatment.Reference Mohr, Vella, Hart, Heckman and Simon19 Flexibly delivered, non-stigmatising telephone-based interventions reduce opportunity costs and care access barriers. Several telephone-IPT studies have demonstrated promising results, including a randomised controlled trial (RCT) with depressed individuals seropositive for HIV,Reference Heckman, Heckman, Markowitz, Woldu, Anderson and Shen20 a pilot for subsyndromal depression after miscarriageReference Neugebauer, Kline, Bleiberg, Baxi, Markowitz and Rosing21 and a small prospective cohort study of depression treatment provided by midwives.Reference Posmontier, Neugebauer, Stuart, Chittams and Shaughnessy22 To increase the clinical utility, scalability and accessibility of IPT for postpartum depression, we changed both the provider (from specialists to trained nurses) and the medium (from face-to-face to telephone delivery). We hypothesised that fewer women who received nurse-delivered telephone IPT would remain clinically depressed at 12 weeks post-randomisation than those who received standard postpartum depression care in their community, with follow-up at 24 and 36 weeks. We defined postpartum depression as meeting criteria for a major depressive episode 2–24 weeks postpartum on the Structured Clinical Interview for DSM-IV (SCID-I).Reference First, Spitzer, Gibbon and Williams23 We also administered the Edinburgh Postnatal Depression Scale (EPDS)Reference Cox, Holden and Sagovsky24 and explored changes in self-reported attachment,Reference Fraley, Heffernan, Vicary and Brumbaugh25 relationship qualityReference Spanier26 and comorbid anxiety.Reference Spielberger, Gorsuch and Lushene27
Method
Participants
Public health departments from 36 health regions in six provinces across Canada screened and referred postpartum women for depression and we further recruited participants through advertisements for self-referral. Women experiencing postpartum depressive symptoms (EPDS score >12) were eligible to be referred. The trial coordinator subsequently provided a detailed trial explanation and assessed eligibility using the SCID depression module by telephone. Women were eligible to participate in the trial if they were: English-speaking; clinically depressed as per a SCID interview; >18 years old; between 2 and 24 weeks postpartum; and discharged home from hospital with their infant. Exclusion criteria included current antidepressant or antipsychotic medication; receiving psychotherapy from a trained professional; active suicidal, self-harm or infanticidal thoughts; psychosis; and chronic depression (episode length >2 years).
The University of Toronto Research Ethics Board approved the trial and all participants provided written informed consent.
Design, randomisation and masking
Web-based randomisation (www.randomize.net) and stratification based on province was centrally controlled (Fig. 1). Women allocated to the control group had access to standard locally available postpartum care, including postpartum depression services from public health nurses, physicians and community resources at maternal discretion. Women in the intervention group had access to the same standard postpartum care in addition to telephone IPT. Telephone follow-up, masked to group allocation, was conducted at 12, 24 and 36 weeks post-randomisation to assess outcomes. All outcome data were entered directly into a Microsoft Access database with built-in logic and range checks to allow for immediate correction of errors and insertion of missing data. At 12 weeks post-randomisation (immediately post-treatment), an independent trained research assistant interviewed women in the intervention group regarding their IPT treatment experience or reasons for non-adherence. Although trial participants and IPT nurses could not be masked to group allocation, the post-treatment evaluators, trial coordinator and service providers of all standard postpartum care were not informed of any mother's participation in the trial or group allocation. The trial protocol was registered (ISRCTN88987377).

Fig. 1 Flow of participants through the trial.
Intervention
Women allocated to the intervention group received 12 weekly 60 min telephone-IPT sessions delivered by a trained nurse, with the first contact to initiate treatment occurring within 72 h of trial enrolment. The three phases of IPT were administered according to the manual by Weismann et al.Reference Weissman, Markowitz and Klerman7,Reference Stuart and Robertson12 In early sessions, the IPT nurses established a therapeutic alliance, provided psychoeducation about depression and IPT, placed the depression in an interpersonal context, reviewed the mother's current and past interpersonal relationships, identified the interpersonal problem area(s) most related to the current depressive episode and set treatment goals. During the middle phase, treatment focused on resolving interpersonal difficulties, such as conflicts with a partner or extended family (interpersonal disputes) and changes in social roles associated with the challenges of new parenthood and needed support (role transitions). The concluding phase reinforced the mother's efforts, gains and competence in working through the interpersonal problems and overcoming depression, with contingency planning in the event of depression recurrence. This trial defined intervention adherence as completing an IPT course of at least ten 30–60 min sessions within 16 weeks.
IPT nurse recruitment, training and supervision
Seven registered female nurses based in Toronto were trained to provide the IPT intervention. Three worked in a general mental health setting, two were public health nurses, one was a paediatric nurse and one an emergency room nurse. The nurses were selected on the basis of references, clinical experience and completing a telephone mock engagement session with an actor who portrayed a depressed mother in which they conveyed empathy and understanding. Only the public health nurses had clinical experience working with women with postpartum depression; however, they did not use structured psychotherapies in their practice. The three mental health nurses had some experience of using psychotherapy in practice, but not for postpartum depression. None of the nurses had clinical expertise in IPT. The nurses were trained and clinically supervised by IPT experts (P.R. and S.G.); two were trained to become peer supervisors. Each nurse attended 8 h of didactics and then conducted two 12-session clinically supervised telephone-IPT training cases with women experiencing postpartum depression who were not involved in the trial. The nurses were required to achieve satisfactory competence and adherence before treating any trial participants, with adherence rated on use of required IPT techniques (P. Ravitz and S. Grigoriadis, personal communication, 2019).28 During the trial, to enhance treatment fidelity, the nurses were continuously monitored for IPT adherence via a checklist and they used treatment-tracking forms with IPT phase- and focus-specific practice activity logs. Telephone-IPT sessions were digitally audiorecorded to guide supervision and ensure adherence. In-person or teleconferenced group supervision occurred weekly to uphold adherence and fidelity. A subset of 25% of randomly selected IPT session recordings from each of the three treatment phases and nurses was reviewed by an independent IPT-trained rater for treatment fidelity using an IPT adherence checklist; the rater was trained to achieve over 90% agreement with an IPT expert trainer on the adherence scale used for this trial.
Outcome measures
The primary outcome of postpartum depression was assessed using the SCID-I major depression module.Reference First, Spitzer, Gibbon and Williams23 We included the self-report EPDSReference Cox, Holden and Sagovsky24 to assess symptoms of depression, with a cut-off score >12. Secondary outcomes included: state anxiety, measured by the State–Trait Anxiety Inventory (STAI);Reference Spielberger, Gorsuch and Lushene27 relationship satisfaction, via the Dyadic Adjustment Scale (DAS);Reference Spanier26 and attachment, by the Experiences in Close Relationships scale (ECR).Reference Fraley, Heffernan, Vicary and Brumbaugh25 Health service utilisation and costs (e.g. walk-in clinics, emergency departments) were also measured,Reference Brown29 as were satisfaction and reasons for non-adherence with the intervention at 12 weeks post-randomisation. The IPT nurses documented all intervention activities (telephone discussions, left messages, missed sessions) in an activity log. Safety protocols were developed and adverse events were assessed through weekly IPT nurse discussions and review of completed questionnaires by the trial coordinator.
Sample size
As most postpartum depression treatment trials use a self-report measure to assess recovery instead of a diagnostic interview and as we anticipated a heterogeneous treatment sample, we conservatively estimated that 30% of women in the control group would recover from depression by 12 weeks post-randomisation. Sample size calculation was based on ability to detect a moderate decrease of 20 percentage points to a rate of 50% among women in the intervention group. To achieve 80% power, a 2-tailed alpha error of 0.05, using a test of 2 independent proportions to find a 20% reduction in the number of participants with depression at 12 weeks post-randomisation required a sample size of 188 (94 per group). We planned to enrol 240 participants, anticipating equal attrition in both conditions, to compensate for up to 20% loss to follow-up.
Statistical analysis
Data were analysed with SAS version 9.4 for Windows (SAS Institute, Cary, NC, USA) using an intention-to-treat approach where all follow-up data obtained were analysed according to participant randomisation. Given that not all participants provided follow-up data, we completed all analyses using case data. It was not possible to forward the last observation nor was it appropriate to complete any kind of model-based generation of replacement values, especially with the SCID. Descriptive statistics were calculated for all variables of interest. Continuous variables were summarised using means and standard deviations (s.d.), whereas categorical variables were summarised using counts and percentages. Between-group comparisons were carried out using two-sample two-sided t-tests for continuous variables (or Wilcoxon rank sum tests for non-normally distributed ones). For binary variables, we carried out χ2 analyses (or Fisher's exact tests in the case of low expected counts) and have presented odds ratios (OR) with 95% confidence intervals (CI). A logistic regression model compared groups adjusting for and identifying other variables predictive of depression (EPDS score >12) at 12 weeks post-randomisation. Prior to analysis, the predictor variables were assessed for the presence of multicollinearity using tolerance statistics. A tolerance statistic value <0.4 was considered to indicate the presence of multicollinearity and in such cases only one member of a correlated set would be retained for the multivariable model. To avoid over-parameterisation of the model, a change in estimate method was used to select variables for the final model. This approach involved running a starting logistic regression model with just group in relation to EPDS >12, and noting the parameter estimate for group, followed by a series of models containing group and only one of the other variables of interest. The change in the parameter estimate of group was noted in each case, and the final multivariable logistic regression model contained those variables with the greatest change in estimate. The final model results are displayed using ORs with their associated 95% CIs.
Binary outcome measures, such as EPDS >12, were compared between groups at each time point, with results reported as ORs and 95% CIs. Continuous measures were compared in a similar fashion but were also assessed using linear mixed models. The linear mixed models assessed the rate of change over time between groups and included a group variable, a time variable and the key group × time interaction term. The individual participant was treated as the random effect. The models used maximum likelihood estimation, which allows model approximation for those participants with missing data and therefore does not drop these individuals from the analysis. All models were run using SAS Version 9.3 or later for Windows (SAS Institute, Cary, NC, USA).
Results
Of 961 referrals received between January 2009 and May 2012, 901 (93.8%) were from public health nurses and other health professionals (e.g. social workers, lactation consultants) and only 60 (6.2%) were self-referrals from women who learned about the trial through health professionals, flyers, brochures and magazine advertisements. Of the 961 referrals, 260 women were not screened because they did not meet referral criteria (e.g. EPDS score >12) or we were unable to contact them after multiple attempts. Of the 701 women screened, 469 were excluded (463 did not meet our inclusion criterial and 6 declined participation). In total 241 women were recruited, 120 in the IPT group and 121 in the control group. Although over three-quarters of the trial participants (n = 193, 80.1%) were recruited from diverse health regions in Ontario, the most populous province in Canada, others were enrolled from the provinces of Nova Scotia (n = 6), Manitoba (n = 13), Saskatchewan (n = 7), Alberta (n = 12) and British Columbia (n = 10), demonstrating the feasibility of providing the intervention nationally (Fig. 1). Of the women recruited in Ontario, more than two-thirds (68.4%) lived in a rural region (n = 95) or a remote northern town (n = 37). Table 1 shows the participants’ baseline characteristics, with no clinically important differences between the two trial groups and no baseline differences between women included in the analysis and those lost to follow-up. As regards ethnicity, 48% (n = 116) identified as coming from ‘other’ (compared with ‘Canadian’) ethnic backgrounds, including South Asian (n = 11), African (n = 10), Asian (n = 8), Aboriginal (n = 9), Latin American (n = 9), Middle Eastern (n = 6) and Caribbean (n = 6). One in four women (24.9%, n = 60) had high-school education or less and one in three (33.2%, n = 80) reported an annual household income below CAD$40 000, with 14% (n = 34) at the poverty level (<CAD$20 000). Almost half the sample had a history of depression (n = 115) and many (n = 95) were equivocal or unsatisfied with the overall support they were receiving from the infant's father. Women were recruited on average at 12 weeks postpartum (s.d. = 6.74) and mean baseline EPDS and STAI scores were similar between groups (Table 1). At 12 weeks post-randomisation, 204 (84.7%) participants completed the follow-up telephone interview, decreasing to 202 (83.8%) at 24 weeks and 197 (81.7%) at 36 weeks.
Table 1 Baseline characteristics of randomised participants
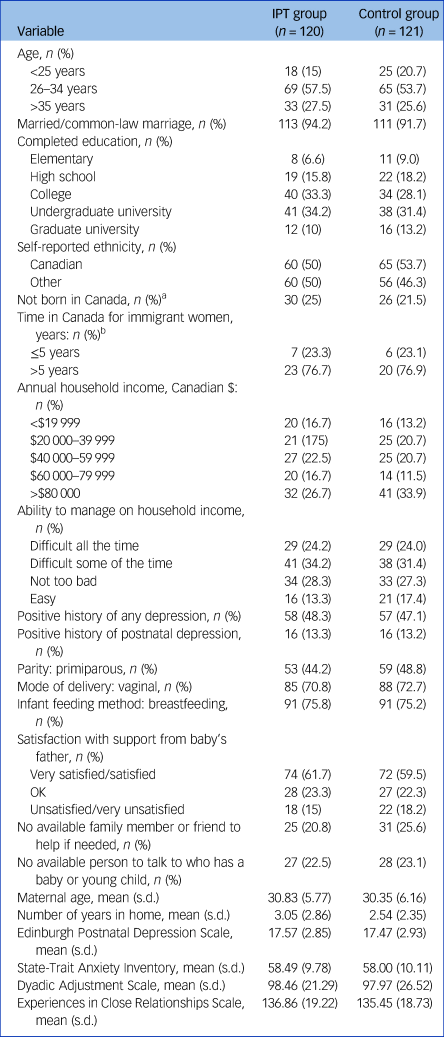
IPT, telephone interpersonal psychotherapy.
a. Among these participants, the following ethnic origins were most commonly self-identified according to Statistics Canada criteria: South Asian (e.g. Indian, Pakistani); East/Southeast Asian (e.g. Chinese); Caribbean; and African. Other ethnic origins included: Middle Eastern; South American; and Eastern/Southern European.
b. n = 30 for the IPT group; n = 26 for the control group.
There was high treatment fidelity demonstrated through adherence ratings (86%) to the telephone-IPT intervention. Women in the intervention group were significantly less likely to meet SCID depression criteria at the 12-week post-randomisation assessment than those in the control group. Specifically, 10.6% (11/104) of women in the intervention group had a diagnosis of clinical depression, compared with 35% (35/100) in the control group (χ2 = 17.41, P < 0.001; OR = 0.22, 95% CI 0.10–0.46; number needed to treat NNT = 4). Significant group differences were sustained at 24 weeks (χ2 = 15.13, P <0.001), when 10.9% (11/101) of women in the intervention group and 33.7% (34/101) in the control group had a depression diagnosis (OR = 0.24, 95% CI 0.11–0.51). At 36 weeks, no group differences were found, when 10.9% (11/101) of women in the intervention group and 15.6% (15/96) in the control group had a diagnosis of clinical depression (OR = 0.66, 95% CI 0.29–1.52). None of the women who had responded to IPT relapsed during any of the trial follow-up periods. At the 36-week follow-up, post hoc analyses suggest that significantly more women in the control group (n = 7) had subclinical depression (four or more symptoms) than in the intervention group (n = 0). When included in our analysis, 10.9% (11/101) of women in the intervention group, versus 22.9% (22/96) of those in the control group, had subclinical symptoms or a diagnosis of clinical depression (OR = 0.41, 95% CI 0.19–0.90). In terms of EPDS scores >12, similar significant results across time were found (Table 2). The logistic regression model indicated that three variables, beyond study group, predicted EPDS >12 at 12 weeks. Women were less likely to have significant depressive symptoms if they received telephone IPT and had a family member or friend to talk to (OR = 0.46, 95% CI 0.22–0.98); and more likely to remain depressed if they had a history of depression (OR = 1.99, 95% CI 1.01–3.93) and a higher level of anxiety at baseline (OR = 1.04, 95% CI 1.00–1.08).
Table 2 Between-group comparisons of postpartum depression, anxiety and comorbidity cases
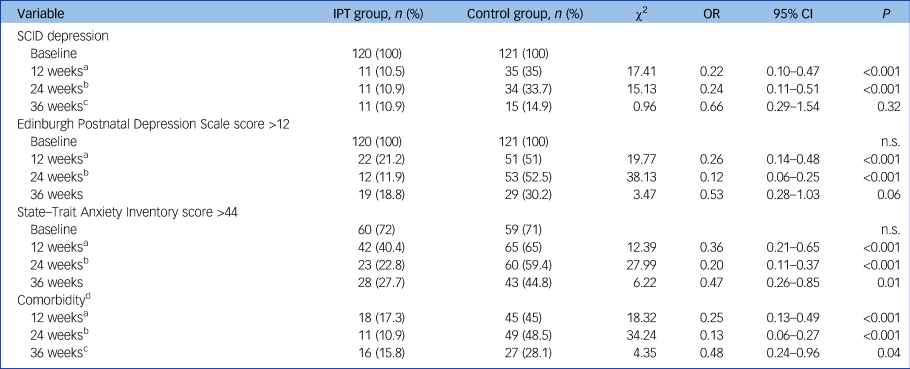
IPT, telephone interpersonal psychotherapy; SCID depression, diagnosed as clinically depressed according to the Structured Clinical Interview for DSM-IV; n.s., non-significant.
a. n = 104 for the IPT group; n = 100 for the control group.
b. n = 101 for the IPT group; n = 101 for the control group.
c. n = 101 for the IPT group; n = 96 for the control group.
d. Comorbidity is defined as an Edinburgh Postnatal Depression Scale score >12 and a State–trait Anxiety Inventory score >44.
At the 12-week assessment, 40.4% (42/104) of women in the intervention group had an anxiety score >44 on the STAI, compared with 65% (65/100) in the control group (OR = 0.36, 95% CI 0.21–0.65; χ2 = 12.39, P <0.001), with significant group differences maintained at 24 and 36 weeks favouring telephone IPT (Table 2). When we examined comorbid depression and anxiety (EPDS score >12 and STAI score >44), we found significant between-group differences at 12 (χ2 = 18.32, P <0.001), 24 (χ2 = 34.24, P <0.001) and 36 (χ2 = 4.35, P <0.001) weeks favouring telephone-IPT (Table 2). Women in the IPT group had higher overall mean scores on the DAS across time, indicating overall improved partner relationship quality. Further, significant differences in mean scores favoured telephone IPT on the affectional expression (t = 2.24, P = 0.02), cohesion (t = 2.86, P = 0.005) and consensus (t = 3.38, P = 0.001) subscales, but not on the relationship satisfaction subscale (t = 1.65, P = 0.10) at 12 weeks, continuing at 24 weeks for cohesion (t = 2.90, P = 0.004) and consensus (t = 2.98, P = 0.003), that were maintained until 36 weeks (cohesion: t = 1.97, P = 0.05; consensus: t = 2.01, P = 0.05). At 12 weeks, there was a significant difference in the dimensional attachment avoidance subscale of the ECR (t = 2.31, P = 0.02) favouring IPT, but not in dimensional attachment anxiety (t = −0.30, P = 0.77). No differences on dimensional attachment scores were noted at 24 or 36 weeks. Linear mixed models were run to assess change over time for the outcomes presented in Table 3. For EPDS scores the interaction between group and time was significant (P = 0.004), with the control group having a greater decrease over time. For STAI scores the interaction between group and time was significant (P = 0.0004), with the IPT group having a greater decrease over time. For DAS scores the interaction between group and time was significant (P = 0.002), with the IPT group having a greater increase over time. Last, generalised estimating equation (GEE) analyses were completed on the variables in Table 2 to assess changes over time between groups, adjusting for the correlation among observations taken on the same participant. The group × time interaction term was the key component of interest in these models. For SCID, this interaction was non-significant (P = 0.86). This was also the case for EPDS (P = 0.12), STAI (P = 0.16) and comorbid depression (P = 0.17).
Table 3 Between-group comparisons of mean scores on postpartum depression, anxiety and relationship satisfaction

IPT, telephone interpersonal psychotherapy.
a. n = 104 for the IPT group; n = 100 for the control group.
b. n = 101 for the IPT group; n = 101 for the control group.
c. n = 101 for the IPT group; n = 96 for the control group.
At 12 weeks, a comparable small number of women in the telephone-IPT (n = 14, 13.5%) and control (n = 16, 16%) groups were taking antidepressant medication (χ2 = 0.26, P = 0.61), suggesting that most women with postpartum depression prefer not to take medications. No significant group difference was found in antidepressant use at any time point (24 weeks: 18 (17.8%) v. 22 (21.8%), χ2 = 0.50, P = 0.48; 36 weeks: 23 (23%) v. 27 (28.1%), χ2 = 0.68, P = 0.41). At 12 weeks, health service use did not differ (telephone IPT: mean = 24.71, s.d. = 13.07; control group: mean = 26.04, s.d. = 16.80; z = 0.20, P = 0.84). There were no suicides or infanticides. The most frequently used health services were family physician visits (77.6%), home visits by public health nurses (75.5%), telephone contact with public health nurses (54.4%), 6-week follow-up visits to an obstetrician (43.6%) and visits to paediatricians (40.3%), with no total difference between groups (telephone-IPT group: mean = 14.18, s.d. = 7.89; control group: mean = 13.84, s.d. = 8.58; z = 0.71, P = 0.48).
Out of the 120 women randomised to telephone IPT, 104 (86.7%) adhered to the intervention by receiving ≥10 sessions lasting >30 min. There were 16 non-adherents, of whom 7 received no sessions, 4 had 1–3 sessions and 5 completed 4–6 sessions. Stated reasons for non-adherence from participant interviews conducted by the trial coordinator included starting in-person therapy (n = 1), being too busy (n = 1), feeling better (n = 2), inability to connect with participants after repeated attempts (n = 6), repeated missed appointments (n = 3) and maternal choice to discontinue after an IPT nurse contacted a provincial child welfare agency as required by law because of safety concerns for the infant (n = 3). Of the 1216 IPT sessions provided in the trial, 909 (74.8%) were initiated as scheduled. Once initiated, 1189 (97.8%) sessions were completed. Mean EPDS scores decreased across time in the following pattern: session 3, mean = 12.91, s.d. = 4.67; session 6, mean = 10.57, s.d. = 5.04; session 9, mean = 9.19, s.d. = 5.48; and session 12, mean = 7.14, s.d. = 5.28.
Of the 98 (81.7%) women who evaluated their IPT experience with a satisfaction questionnaire, most reported liking the telephone treatment (97.9%) and found it convenient (94.9%). They also perceived the IPT nurses to be competent and well trained (99%) and the quality of the IPT sessions to be excellent (99%). They endorsed that IPT helped with their problems (96.9%) and that they would like to receive it again if they became depressed in the future (96%). Interestingly, 57 (58.2%) women indicated that they would have liked more than the planned 12 IPT sessions, suggesting a need for ‘weaning’ booster sessions.
Discussion
Women experiencing postpartum depression need timely, effective and accessible treatments. This is the first large RCT to evaluate nurse-provided telephone IPT for the treatment of postpartum depression. In this trial, we strategically changed how and by whom IPT was delivered in order to increase the clinical utility, accessibility and ‘reach’ of this effective psychotherapy to an ethnically diverse group of women in underserved rural and urban areas across Canada. We demonstrated that IPT can be effectively provided by telephone to such women by nurses who are not mental health specialists, consistent with findings of mental healthcare in other low-resource settings.Reference Hoeft, Fortney, Patel and Unutzer30,Reference Singla, Kohrt, Murray, Anand, Chorpita and Patel31 This finding offers a potential solution to a global public health problem, including in low- and middle-income countries and underserved settings. In North America and other countries around the world that have widely dispersed urban and rural populaces, telemedicine facilitates access to care and services not otherwise locally available. Telephone interventions are flexible, private, non-stigmatising and highly accessible. Although healthcare services are increasingly being offered via the internet, the telephone still remains a more reliable and readily accessible option.Reference Eysenbach32 The women in our study who received telephone IPT were 4.5 times less likely to meet SCID criteria for depression at 12 weeks post-randomisation than those who received standard local treatment and there was no relapse on long-term follow-up. The intervention effect size was large, with only 10.6% of women remaining depressed after 12 weeks, compared with 25% in the control group. This large effect was maintained to 24 weeks post-randomisation. Women who received telephone IPT were also less likely to experience subsyndromal depression and comorbid anxiety and they reported improved partner relationship quality and reduced attachment avoidance. The telephone-based intervention was highly acceptable to women, with a drop-out (non-adherence) rate of <14%.
Comparison with other psychotherapies for depression
A meta-analysis of the effects of depression psychotherapies on remission, recovery and improvement in adults found that 62% of patients no longer met criteria for depression following treatment.Reference Cuijpers, Karyotaki, Weitz, Andersson, Hollon and Van Straten33 However, 48% of those in the ‘usual care’ conditions also no longer met criteria for depression, suggesting that the additional value of psychotherapy compared with usual care is 14%. Our trial found an added value for telephone IPT of 25%, based on a SCID diagnosis of depression. This larger effect could be the result of better adherence to telephone and nurse delivery (fewer dropping out) compared with standard treatment. The difference between groups in depression diagnosis at 36-week follow-up was not significant, which is attributable to a reduction in clinical symptoms among women in the control group. The decrease in group differences over time is typical of 1-year follow-up findings on the efficacy of acute-phase psychotherapy for depression.Reference Karyotaki, Smit, de Beurs, Henningsen, Robays and Huibers34 Approximately half of untreated individuals diagnosed with major depression will experience spontaneous remission within a year. Although health service utilisation and antidepressant use were similar between groups, it is unclear the extent to which women in the control group received or were on waiting lists for healthcare. Importantly, the longer period of unremitted depressive symptoms has well-documented negative consequences in terms of maternal suffering, family functioning and child developmental trajectories, as outlined in the 2014 Lancet Perinatal Mental Health Series.Reference Howard, Molyneaux, Dennis, Rochat, Stein and Milgrom1,Reference Stein, Pearson, Goodman, Rapa, Rahman and McCallum3
Effects on comorbid anxiety
One novel study finding was the effect of telephone IPT on comorbid symptoms of anxiety. Women treated with telephone IPT had significantly lower levels of anxiety at all follow-up time points. This adds to the growing evidence that IPT may effectively treat anxiety.Reference Cuijpers, Donker, Weissman, Ravitz and Cristea6 This is important because anxiety is highly prevalent among perinatal women. A meta-analysis including 102 studies of 221 974 women from 34 countries found a 15% prevalence of postpartum anxiety between 1 and 24 weeks.Reference Falah-Hassani, Shiri and Dennis35 Unlike postpartum depression, maternal anxiety overall and specifically its treatment have received little empirical attention. Comorbid anxiety and postpartum depression is common and disabling, with more severe symptoms, higher healthcare service utilisation and poorer treatment response.Reference Merikangas, Zhang, Avenevoli, Acharyya, Neuenschwander and Angst36 A meta-analysis of 66 studies from 30 countries found an 8.2% prevalence of comorbid anxiety and depressive symptoms between 1 and 24 weeks postpartum.Reference Falah-Hassani, Shiri and Dennis35 Our trial found that telephone IPT benefitted this subgroup of women with significant comorbidity.
Strengths and limitations
Our trial has multiple strengths. We received referrals from diverse regions and health professionals across Canada, including underserved rural communities, and our acceptance rate among screened and eligible women was high. Training and supervision of the IPT nurses standardised the interventions and ensured good adherence, as evidenced by external ratings. Intention-to-treat analysis showed no between-group differences in health service or antidepressant medication use. Postpartum depression was assessed using both a clinical diagnostic interview and the self-report EPDS. Data collection was masked to group allocation and trial attrition was low, at <20%. Providing treatment by telephone using nurses overcame traditional opportunity costs, stigma and geographical treatment barriers. Women in rural settings are likely to have poor access to specialists in postpartum depression, thus making the availability of a remote, telephone-based intervention crucial. As well, it may be that engaging in treatment with trained nurses was less stigmatising than receiving treatment from a mental health specialist. Participants identified themselves as diverse in ethnicity. One-third had low or poverty-level annual household income, and a quarter had an educational level of high school or less. Thus, the generalisability of this study and feasibility of implementation are excellent.
Despite these strengths, the exclusion of non-English speakers precludes fuller generalisability. The nurse selection and training processes were initially labour intensive; however, it is possible that the costs of training are offset by the ability to treat more women who would otherwise be unwilling or unable to have access to postpartum mental healthcare. Comparing telephone IPT with standard local postpartum care rather than an alternative active treatment condition limits the conclusions that can be made about treatment specificity relative to other psychological interventions for postpartum depression. Future research should address questions regarding outcomes of infants, and moderators and mediators of acute and long-term treatment outcomes.
Clinical implications
Many postpartum women are reluctant to take antidepressant medication, especially while breastfeeding, and are often reluctant to seek or follow up referral for specialist mental healthcare owing to multiple barriers. Equitable and timely access to effective psychotherapy is clinically important for the whole family. Compared with standard postpartum depression treatment, nurse-delivered telephone IPT significantly improved postpartum depression, anxiety and partner relationship quality at 12 and 24 weeks post-randomisation, with sustained between-group differences in anxiety and partner relationship quality at 36 months. Nurse-delivered telephone IPT offers a pragmatic, scalable treatment to improve postpartum depression and comorbid anxiety care outcomes and can help to address access disparities for this important public health problem.
Funding
This work was supported by the Canadian Institutes of Health Research grant number MCT 82332. This trial was conducted and data analysed with complete independence of the researchers from the Canadian Institutes of Health Research. S.G. reports receiving personal fees from Sage, Allergan, Pfizer and Eli Lilly while conducting the study for the submitted work.
Author contributions
C.-L.D. (principal investigator) conceptualised and designed the trial, obtained funding, directed implementation, completed data analysis and interpretation, wrote the draft manuscript, and is guarantor. S.G. (co-investigator and psychiatrist) trained and supervised the IPT nurses and assisted in all trial activities, including design, funding, implementation, data interpretation and manuscript preparation. J.Z. (co-investigator and health economist) assisted in designing the trial economic evaluation, obtaining funding and data interpretation. A.K. (co-investigator and biostatistician) assisted with funding, data analysis and manuscript preparation. P.R. (co-investigator, senior responsible author and psychiatrist) trained and supervised the IPT nurses and assisted in trial activities, including design, funding, implementation, data interpretation and co-writing of the draft manuscript. All authors have commented on the manuscript.







eLetters
No eLetters have been published for this article.