Early intervention for psychosis has been the major focus in mental healthcare development worldwide in the past two decades. Reference McGorry, Killackey and Yung1 Literature has demonstrated the superiority of early intervention services over standard care in improving the outcomes of patients with first-episode psychosis (FEP). Reference Harvey, Lepage and Malla2–Reference Nordentoft, Rasmussen, Melau, Hjorthoj and Thorup4 However, considerable concern has been raised regarding the sustainability of therapeutic benefits of early intervention for psychosis Reference Friis5,Reference Singh6 as there is evidence, albeit primarily based on two randomised controlled trials (RCTs), Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlaeger and Quach7–Reference Gafoor, Nitsch, McCrone, Craig, Garety and Power8 suggesting that the positive effects achieved by early intervention may not be maintained after service withdrawal. In the Danish OPUS trial, Reference Petersen, Jeppesen, Throup, Abel, Øhlenschlaeger and Christensen9 the largest RCT thus far evaluating the effectiveness of integrated early intervention service for psychosis, the findings of better symptom outcome and treatment adherence for early intervention over standard care at 2 years were no longer significant after 5 and 10 years of follow-up. Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlaeger and Quach7,Reference Secher, Hjorthoj, Austin, Thorup, Jeppesen and Mors10 Similarly, the British Lambeth Early Onset (LEO) study Reference Craig, Garety, Power, Rahaman, Colbert and Fornells-Ambrojo11,Reference Garety, Craig, Dunn, Fornells-Ambrojo, Colbert and Rahaman12 found that improved 18-month outcomes on functioning, quality of life and admission to hospital resulting from early intervention were not sustained at 5 years. Reference Gafoor, Nitsch, McCrone, Craig, Garety and Power8 Of note, one important possible explanation for the lack of sustained effect of early intervention is that 2-year specialised treatment (2 years in the OPUS trial; 18 months in the LEO trial) is insufficient to maintain superior outcomes in FEP after transition to standard care. Until now, empirical research evaluating the effectiveness of longer-term early intervention for psychosis has been scarce, Reference Nordentoft, Rasmussen, Melau, Hjorthoj and Thorup4,Reference Chang, Chan, Jim, Lau, Hui and Chan13–Reference Albert, Melau, Jensen, Emborg, Jepsen and Fagerlund15 and how long specialised treatment should be provided (usually offered for the first 1–2 years of illness) to consolidate and optimise the initial therapeutic gains remains unknown. One recently published RCT (the OPUS II trial) comparing 5-year extended early intervention with 2-year early intervention for FEP has revealed lack of a significant between-group difference in symptom and functional outcomes 5 years after service entry, although there was higher client satisfaction and a better working alliance in the 5-year intervention group, as well as general improvement in clinical and functioning ratings for both groups over the follow-up period. Reference Albert, Melau, Jensen, Emborg, Jepsen and Fagerlund15 There are no published RCT follow-up studies examining the durability of positive effects of early intervention services with its treatment duration extended beyond 2 years. It is also worth noting that evidence supporting the effectiveness of early intervention for psychosis was mainly derived from Western countries. However, substantial variation across regions with respect to the content and intensity of early psychosis programmes, characteristics of patients enrolled and sociocultural contexts Reference Edwards, Harris and Bapat16 limits generalisability of results and precludes the direct adoption of an early-intervention service model by non-Western countries, including some affluent Asian communities, where public mental healthcare is often overburdened and underresourced. Reference Gupta, Methuen, Kent, Chatain, Christie and Torales17
Hong Kong is among the few cities in Asia to have implemented an early intervention service for psychosis. The intervention programme Early Assessment Service for Young People with Psychosis (EASY) was launched in 2001 and comprises community-awareness programmes, an open referral system and a 2-year specialised intervention for young people presenting with FEP, followed by 1-year step-down care with preserved medical follow-up but no provision of case management. Reference Tang, Wong, Hui, Lam, Chiu and Chan18 Evaluation of the EASY programme using historical-control methods showed that patients receiving the early intervention had better functioning, milder symptom severity, fewer suicides and admissions to hospital, and a lower disengagement rate than those receiving standard care, despite a lack of significant between-group difference in duration of untreated psychosis (DUP). Reference Chen, Tang, Hui, Chiu, Lam and Law19 In an attempt to evaluate the effectiveness of longer-term early intervention for psychosis, we have conducted an RCT (EASY-Extension Trial) comparing a 1-year extension of the early intervention service (i.e. 3-year early intervention) with step-down care (i.e. 2-year early intervention) in a representative cohort of young Chinese patients who had completed 2-year treatment in the EASY programme for their FEP. Reference Chang, Chan, Jim, Lau, Hui and Chan13,Reference Chang, Kwong, Chan, Jim, Lau and Hui20 This was the first reported RCT to provide evidence of the efficacy of extending an early intervention service for psychosis beyond 2 years. Our results indicated that patients receiving extended early intervention displayed significantly better functioning, fewer negative and depressive symptoms, and lower treatment default rates than those managed by step-down care. Reference Chang, Chan, Jim, Lau, Hui and Chan13 In the current study, we aimed to address a critical question of the durability of therapeutic gains attained by extended early intervention for FEP. To the best of our knowledge, this is the first RCT follow-up study examining the sustainability of beneficial effects of an early intervention service with its treatment period extended beyond 2 years. Patients included in the EASY-Extension Trial were reassessed 1 and 2 years after completion of the RCT to investigate whether the better outcomes of the intervention group could be maintained after transition to generic psychiatric care. The trial was registered with ClinicalTrials.gov (NCT01202357).
Method
Participants
This was a 3-year follow-up of a single-blind RCT (2 years after the extended early intervention ended and 5 years after entry to the EASY programme) (online Fig. DS1, Fig. 1) comparing a 1-year extension of specialised early intervention (3-year early intervention) with step-down care (2-year early intervention) in 160 patients who had received 2 years of care from the early intervention service for FEP. Reference Chang, Chan, Jim, Lau, Hui and Chan13 Participants were recruited from the EASY programme between November 2010 and August 2011 and underwent a 12-month clinical trial. Patients with a DSM-IV 21 diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, brief psychotic disorder, delusional disorder, psychosis not otherwise specified, bipolar disorder with psychotic symptoms or depressive disorder with psychotic symptoms were included in the study. Exclusion criteria were intellectual disability, substance-induced psychosis, psychotic disorder because of a general medical condition or an inability to speak Cantonese Chinese for the research interview.
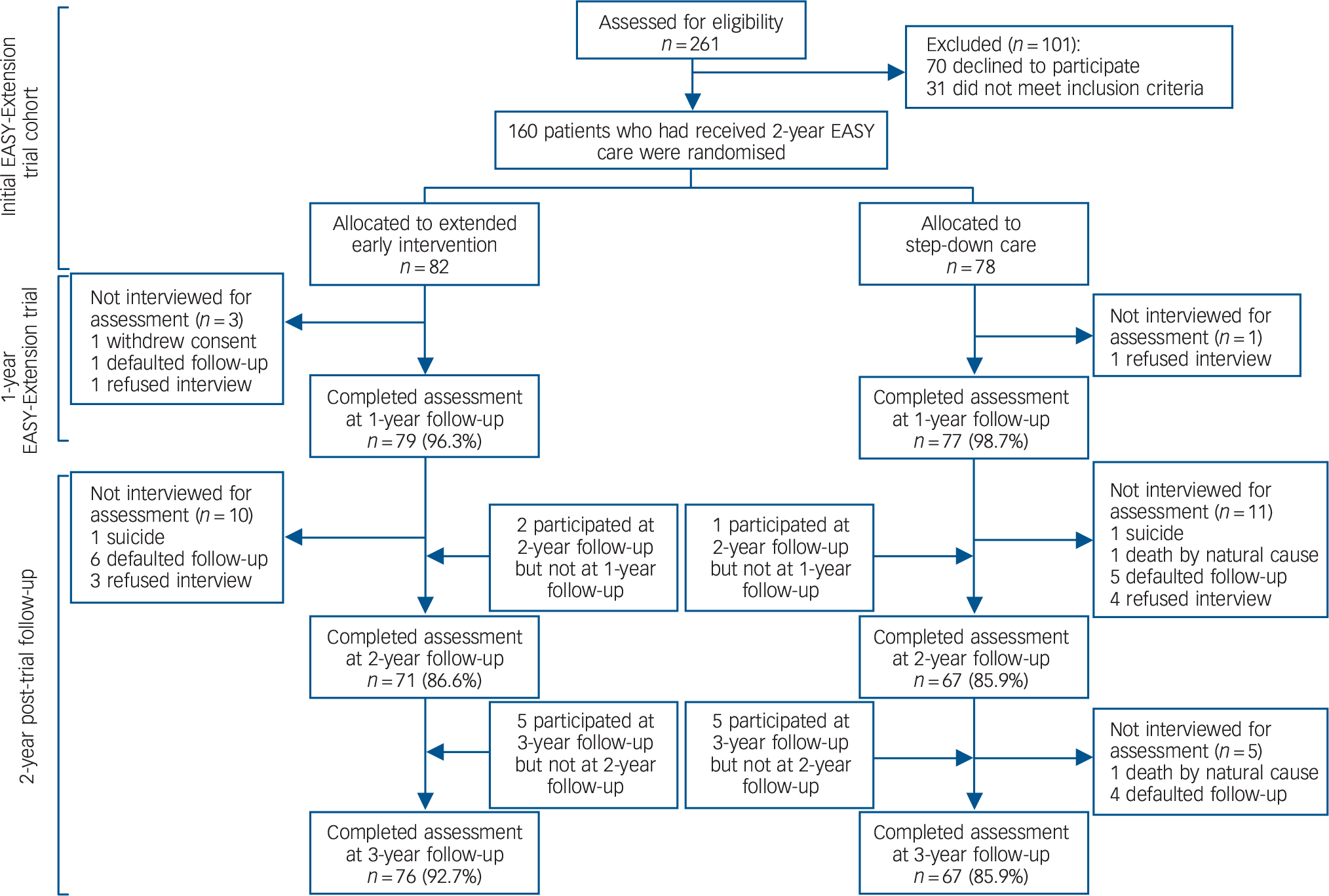
Fig. 1 Flow of patients through the study.
EASY, Early Assessment Service for Young people with Psychosis.
Details of the EASY programme have been reported elsewhere. Reference Tang, Wong, Hui, Lam, Chiu and Chan18 In brief, this is a publicly funded, territory-wide service providing comprehensive assessment and early intervention for individuals aged 15 to 25 years presenting with FEP in Hong Kong. Reference Tang, Wong, Hui, Lam, Chiu and Chan18 The service consists of five clinical teams, each covering a geographically defined catchment area and comprising two psychiatrists, three case managers and one social worker. The programme adopts a phase-specific, case-management approach in which each patient is assigned a case manager who provides protocol-based psychosocial interventions, Reference So, Chen, Lee, Wong and Wong22 based on the International Clinical Practice Guidelines for Early Psychosis 23 with local cultural adaptations. This standardised intervention package is offered to all patients and their family caregivers with an aim to enhance psychological adjustment to early psychosis through in-depth engagement, comprehensive psychoeducation, adherence to medication treatment, coping and stress management and relapse prevention. Reference So, Chen, Lee, Wong and Wong22 As case-loads of EASY case managers (approximately 1:80) are much heavier than that of those well-established early intervention services in the West, rather than providing intensive intervention such as cognitive-behavioural therapy (CBT) or specialised family therapy, case management in the EASY programme focuses on psychoeducation and supportive care. Emphasis is also placed on enhanced support and communications with family caregivers, who have a critical role in patient management, as most patients enrolled in the programme live with their families. Reference Tang, Wong, Hui, Lam, Chiu and Chan18 Family counselling and caregiver support groups are arranged if indicated. Patients with additional treatment needs such as the presence of residual symptoms or secondary depressive symptoms are referred to clinical psychologists for provision of CBT. The programme also closely collaborates with non-governmental organisations (NGOs) that organise community-based rehabilitation programmes and vocational training for patients recovering from early psychosis. Multidisciplinary case reviews are held on a regular basis to closely monitor patients' clinical progress and treatment outcomes. Patients are assertively followed up for 2 years, after which they are managed by a transitional step-down clinic in the third year of treatment, whereby medical follow-up is offered by psychiatrists who have been responsible for their care in the 2-year programme but no case management is provided (i.e. equivalent to standard psychiatric care but with 1-year continuous out-patient follow-up by the psychiatrists of the EASY programme). They are then transferred to generic psychiatric services for continuous care.
In this study, participants were followed up and re-interviewed 2 and 3 years after inclusion in the trial. The study was approved by the local institutional review boards. All participants provided written informed consent. For those aged under 18 years, consent was also obtained from a parent or guardian.
Randomisation
Following baseline assessment, participants were randomly assigned in a 1:1 ratio to either extended early intervention (the intervention group) or step-down care (the control group) for the next 12 months. An allocation sequence was computer-generated with a fixed block size of four. Randomisation and concealment procedures were conducted by an independent research staff member who was not involved in recruitment, clinical management and research assessments of study participants.
Treatment
Participants in both treatment conditions were managed by psychiatrists from their respective EASY clinical teams during the 12-month period of the RCT. After completion of the trial, all participants were transferred to standard psychiatric services for continuous care.
Extended early intervention
Specialised early intervention was continued in the form of an additional year of case management. A trained case manager took over cases of participants from the EASY programme and was responsible for providing care and coordinating treatment with clinicians, allied health professionals and NGOs to all participants in this group (n = 82) (i.e. a case-load comparable with the EASY programme). Case management closely aligned with the EASY treatment protocols, focusing specifically on functional enhancement by assisting participants to re-establish supportive social networks, resume leisure pursuits and return to work. Additionally, continuous supportive care, psychoeducation, coping and stress management were delivered to family caregivers of each participant in the intervention group by the case manager. Once every 2 weeks clinical supervision was provided to the case manager by senior psychiatrists who had extensive experience in early intervention for psychosis.
Step-down care
Step-down care provided out-patient medical follow-up with limited community support that focused mainly on crisis intervention.
The two treatment groups did not differ from each other with respect to the intensity of medical follow-up by psychiatrists, prescription of antipsychotic medications and availability of various psychosocial interventions and community-based services.
Assessment
Diagnosis of each participant was ascertained in consensus meetings attended by a senior psychiatrist and research assistants using all available information encompassing the entire follow-up period, including the Chinese-bilingual Structured Clinical Interview for DSM-IV (CB-SCID) Reference So, Kam, Leung, Chung, Liu and Fong24 (conducted at baseline, 1- and 3-year follow-up), informant histories and medical records. Premorbid functioning was measured with the Premorbid Adjustment Scale (PAS) Reference Cannon-Spoor, Potkin and Wyatt25 at study entry. The Interview for the Retrospective Assessment of the Onset of Schizophrenia (IRAOS) Reference Hafner, Riecher-Rossler, Hambrecht, Maurer, Meissner and Schmidtke26 was employed at baseline to determine DUP, age and mode of onset of psychosis. Psychopathology was assessed at baseline, 1-, 2- and 3-year follow-up using the Positive and Negative Syndrome Scale (PANSS) Reference Kay, Opler and Fiszbein27 and the Calgary Depression Scale (CDS). Reference Addington, Addington and Maticka-Tyndale28 Psychosocial functioning was measured with the Social and Occupational Functioning Assessment Scale (SOFAS) Reference Goldman, Skodol and Lave29 and the Role Functioning Scale (RFS). Reference Goodman, Sewell, Cooley and Leavitt30 The SOFAS provided a global functioning estimate for each participant, whereas the RFS, which comprised four subscales, was used to assess functional levels in various domains including work productivity, independent living and self-care and immediate and extended social networks. Occupational status was also assessed. Functional evaluation was conducted at baseline, at 6 months, 1, 2 and 3 years after study entry.
Follow-up information on service use including hospital admissions, defaults in out-patient appointments and service disengagement, treatment characteristics including use of second-generation antipsychotics and the dose of antipsychotic medication (chlorpromazine equivalent doses Reference Woods31 were computed for analysis), and other clinical outcome measures including relapse, all-cause mortality and suicide were obtained via systematic record review using out-patient and in-patient case notes as well as computerised clinical information from the hospital database. Data on mortality and cause of death were also verified with the Coroner's Register. Complete clinical record data over the 2-year post-trial follow-up period were available to all participants for analysis.
Trained research assistants masked to treatment allocation administered all assessments. Videotaped interviews of 10 participants were independently rated by all research assistants for interrater reliability evaluation. Intra-class correlation coefficients (ICCs) for PANSS general psychopathology, positive and negative symptom subscales, and CDS total score were 0.92, 0.95, 0.79 and 0.96, respectively, indicating good interrater reliability. A satisfactory level of concordance was also observed in functional measures, with ICCs for SOFAS and RFS total scores being 0.91 and 0.86, respectively.
Statistical analysis
Statistical analyses were performed on an intention-to-treat (ITT) basis. The primary outcome was psychosocial functioning as measured by SOFAS and RFS. Secondary outcome measures included symptom severity, service use and other clinical variables. We estimated sample size based on SOFAS as this was a key outcome measure of the study. To detect a clinically meaningful five-point difference in SOFAS, with a power of 0.8 and an alpha of 0.05, and to allow for 20% drop-out rate, a total of 160 participants were required for the study. Potential attrition bias was examined by comparing sociodemographic factors, baseline clinical profiles, symptom and functional scores at entry, and treatment characteristics in patients who participated in the 3-year follow-up assessment with those who did not participate. To determine group differences in functional and symptom outcomes during the 2-year post-trial follow-up, a series of linear mixed models (LMMs) with repeated measures (using data from baseline and all follow-up time points) were performed. Implementation of LMM analyses is recommended as a preferred statistical method of outcome analysis in clinical trials, as these models can address missing outcome data by allowing the analysis of all available data on the assumption that data are missing at random. Reference Gibbons, Hedeker and DuToit32 In our models, the treatment group, time and group × time interaction were treated as fixed factors, and unstructured covariance structure was employed. Interaction terms between treatment group and time were used to estimate whether longitudinal changes of outcome variables across 3-year follow-up differed between the two groups. Between-group comparisons on functional and symptom outcomes at individual follow-up time points were analysed based on the estimated mean differences and P-values of difference derived from LMMs. In addition, comparisons between treatment groups based on completers-only analyses on functional and symptom outcomes at 2- and 3-year follow-up were conducted. Treatment characteristics, service use and other clinical outcome variables during the 2-year post-trial follow-up were also compared between the two groups. DUP was log-transformed because of its skewed distribution. All statistical analyses were two-tailed with significance level set at P < 0.05. Statistical analyses were performed with IBM SPSS Statistics 24.0.
Results
The participant flow through the study is presented in Fig. 1. A total of 160 patients were enrolled and randomly assigned to the intervention group (n = 82) and control group (n = 78). Online Table DS1 shows the baseline characteristics of the 160 participants included in the trial and reveals no significant between-group difference in sociodemographic profile or baseline clinical, functional and treatment characteristics. A total of 138 (intervention group: n = 71, 86.6%; control group: n = 67, 85.9%) and 143 patients (intervention group: n = 76, 92.7%; control group: n = 67, 85.9%) participated in the 2- and 3-year follow-up assessment, respectively. There was no significant difference between the two groups in participation rate at 2-year (P = 0.90) and 3-year (P = 0.16) follow-up. For those who had completed 3-year follow-up, no significant between-group difference was observed in sociodemographic and other baseline characteristics (online Table DS2). Attrition analysis at the 3-year follow-up demonstrated no significant difference between participants and non-participants in sociodemographic characteristics or baseline clinical, functional and treatment variables, with the exception of RFS immediate social network score (participants had higher scores than non-participants, P = 0.03). At the end of 3-year follow-up, four participants were deceased (intervention group: n = 1; control group: n = 3, P = 0.36); two died by suicide and two from natural causes (Fig. 1).
Functional outcomes
Table 1 presents observed means (s.d.) as well as estimated mean differences and P-values of difference from LMMs at 1-, 2- and 3-year follow-up for functional outcomes. There were no significant differences between the two groups in any of the functional measures at 2- and 3-year follow-up. Similarly, comparisons based on completers-only analyses demonstrated lack of significant between-group differences in ratings of all functional measures at 2- and 3-year follow-up, with the exception that the intervention group had a significantly higher RFS extended social network score than the control group at 2-year follow-up (online Table DS3). Longitudinal analysis over the 3-year follow-up showed significant group × time interactions in SOFAS score (P < 0.01), and RFS work productivity score (P < 0.01), independent living score (P < 0.01) immediate social network score (P = 0.03), extended social network score (P = 0.01) and total score (P < 0.01). This indicates that significant differential courses of functioning over 3 years in treatment groups appeared to be driven mostly by between-group differences in the first year of follow-up (i.e. a 12-month trial period). A graphical illustration of the longitudinal trajectories of functional measures across 3-year follow-up in treatment groups is shown in Fig. 2.
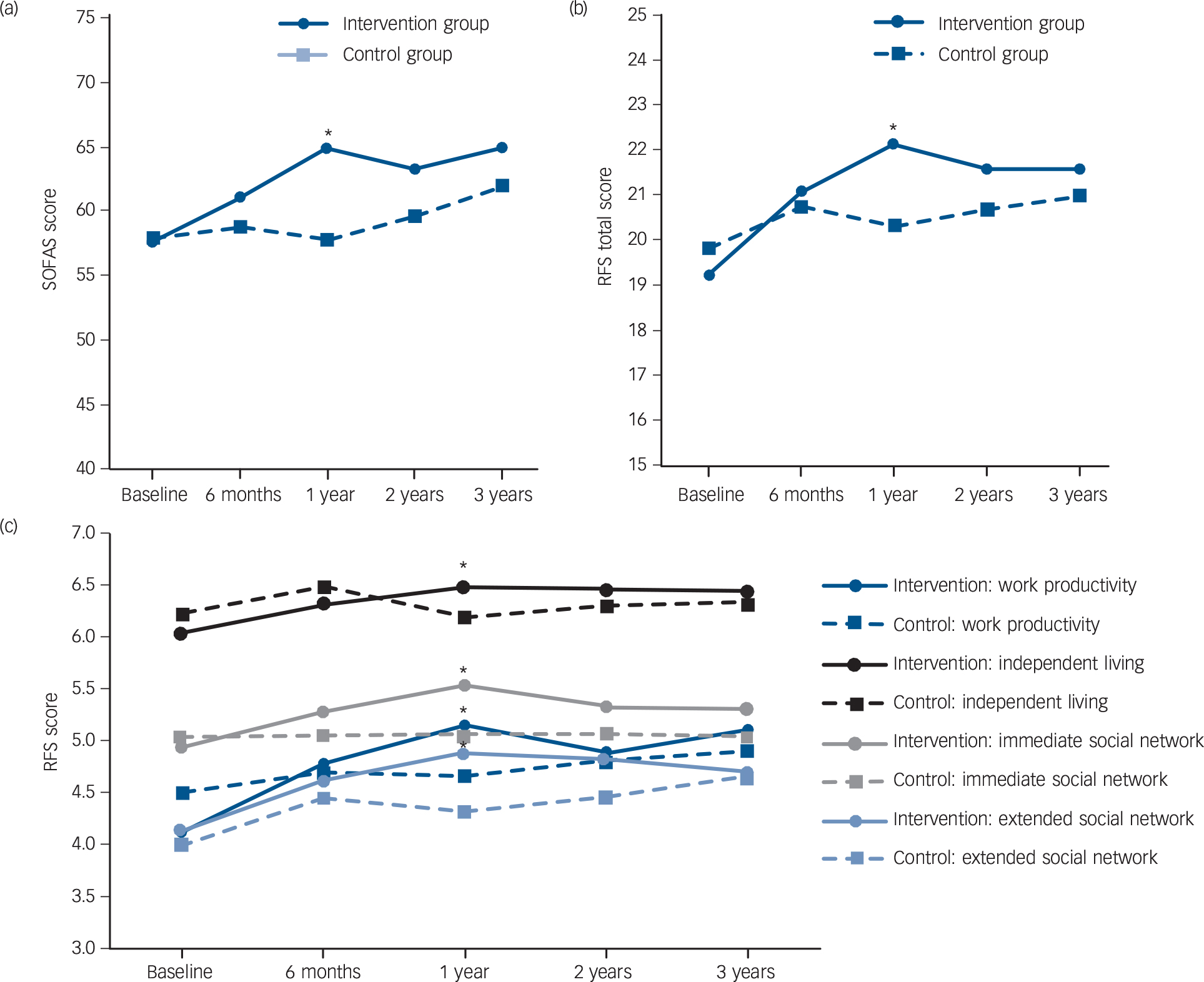
Fig. 2 Longitudinal change in functioning scores across 3-year follow-up in the extended early intervention group and step-down care control group.
(a) Change in the Social and Occupational Functioning Assessment Scale (SOFAS) score; (b) change in the Role Functioning Scale (RFS) total score; and (c) change in the RFS subdomains score. *P < 0.05.
Table 1 Functional outcomes at 1-, 2- and 3-year follow-up of the two study groups a

| Group, mean (s.d.) | Estimated mean difference a (95% CI) |
|||
|---|---|---|---|---|
| Variables | Intervention group | Control group | P | |
| Social and Occupational Functioning Assessment Scale score | ||||
| 1-year follow-up | 64.8 (13.1) | 57.9 (12.7) | 3.57 (1.14 to 5.99) | 0.004 |
| 2-year follow-up | 63.3 (13.6) | 59.6 (12.1) | 1.28 (−0.31 to 2.88) | 0.113 |
| 3-year follow-up | 64.8 (13.7) | 61.9 (12.5) | 1.11 (−1.04 to 3.27) | 0.311 |
| Role Functioning Scale | ||||
| Work productivity | ||||
| 1-year follow-up | 5.1 (1.4) | 4.7 (1.5) | 0.44 (−0.16 to 0.72) | 0.002 |
| 2-year follow-up | 4.9 (1.5) | 4.8 (1.4) | 0.15 (−0.01 to 0.30) | 0.060 |
| 3-year follow-up | 5.1 (1.5) | 4.9 (1.4) | 0.17 (−0.07 to 0.41) | 0.173 |
| Independent living | ||||
| 1-year follow-up | 6.5 (0.6) | 6.2 (1.0) | 0.23 (0.06 to 0.39) | 0.007 |
| 2-year follow-up | 6.5 (0.5) | 6.3 (0.7) | 0.11 (0.01 to 0.23) | 0.071 |
| 3-year follow-up | 6.4 (0.6) | 6.3 (0.7) | 0.08 (−0.02 to 0.18) | 0.112 |
| Immediate social network | ||||
| 1-year follow-up | 5.5 (0.9) | 5.1 (1.0) | 0.27 (0.07 to 0.47) | 0.008 |
| 2-year follow-up | 5.3 (0.8) | 5.1 (0.9) | 0.15 (−0.04 to 0.34) | 0.117 |
| 3-year follow-up | 5.3 (0.9) | 5.0 (1.0) | 0.08 (−0.01 to 0.17) | 0.059 |
| Extended social network | ||||
| 1-year follow-up | 4.9 (1.0) | 4.3 (1.3) | 0.20 (0.04 to 0.45) | 0.010 |
| 2-year follow-up | 4.8 (0.9) | 4.5 (1.1) | 0.08 (−0.06 to 0.22) | 0.268 |
| 3-year follow-up | 4.7 (0.9) | 4.7 (1.0) | 0.01 (−0.21 to 0.20) | 0.959 |
| Total score | ||||
| 1-year follow-up | 22.1 (3.2) | 20.3 (3.7) | 1.16 (0.59 to 1.74) | <0.001 |
| 2-year follow-up | 21.5 (3.3) | 20.7 (3.2) | 0.44 (−0.13 to 1.01) | 0.126 |
| 3-year follow-up | 21.5 (3.2) | 20.9 (3.2) | 0.35 (−0.23 to 0.95) | 0.251 |
a. Estimated mean difference and P-values were derived from linear mixed models for repeated measurements (at baseline, at 6-month, 1-year, 2-year and 3-year follow-up).
Symptoms and other secondary outcomes
Comparisons based on both LMMs and completers-only analyses revealed no significant differences between the two groups in outcomes on positive symptoms, negative symptoms, depressive symptoms and PANSS general psychopathology scores at 2- and 3-year follow-up (Table 2, online Table DS4). There were no significant between-group differences in medication treatment characteristics, length of in-patient stay, employment outcome and rates of relapse, psychiatric admission, out-patient treatment defaults and service disengagement across the 2-year post-trial follow-up period (Table 2).
Table 2 Clinical and service use outcomes of the two study groups during the 2-year post-trial follow-up period
| Variables | Intervention group | Control group | t or χ2 | P |
|---|---|---|---|---|
| Symptom severity at follow-up, a mean (s.d.) | ||||
| Positive and Negative Syndrome Scale, positive symptom score | ||||
| 2-year follow-up | 10.1 (3.7) | 10.3 (3.7) | −0.5 | 0.649 |
| 3-year follow-up | 9.9 (3.4) | 10.2 (3.6) | −0.6 | 0.577 |
| Positive and Negative Syndrome Scale, negative symptom score | ||||
| 2-year follow-up | 12.1 (5.1) | 11.3 (4.5) | 0.9 | 0.355 |
| 3-year follow-up | 12.0 (4.0) | 11.9 (4.0) | 0.1 | 0.941 |
| Positive and Negative Syndrome Scale, general psychopathology score | ||||
| 2-year follow-up | 21.3 (4.3) | 21.9 (4.0) | −0.9 | 0.364 |
| 3-year follow-up | 21.2 (5.4) | 22.1 (4.6) | −1.0 | 0.304 |
| Calgary Depression Scale, total score | ||||
| 2-year follow-up | 1.7 (2.3) | 2.7 (2.9) | −2.3 | 0.024 |
| 3-year follow-up | 1.6 (2.3) | 2.0 (2.8) | −1.1 | 0.271 |
| Service use outcomes during follow-up b | ||||
| Psychiatric hospital admission, % (n) | 17.1 (14) | 16.7 (13) | 0.0 | 0.945 |
| Length of hospital stay, days: mean (s.d.) | 131.5 (139.7) | 174.3 (259.0) | 0.5 | 0.594 |
| Default in out-patient appointment, % (n) | 31.7 (26) | 41.0 (32) | 1.502 | 0.220 |
| Service disengagement, % (n) | 6.1 (5) | 7.7 (6) | 0.2 c | 0.762 |
| Other outcome measure during follow-up | ||||
| Relapse of psychotic episode, b % (n) | 25.6 (21) | 37.2 (29) | 2.5 | 0.115 |
| All-cause mortality, b % (n) | 1.2 (1) | 3.8 (3) | 1.1 c | 0.358 |
| Suicide, b % (n) | 1.2 (1) | 1.3 (1) | 0.0 c | 1.000 |
| Total months in full-time work, a mean (s.d.) | 12.9 (10.0) | 11.8 (10.1) | 0.6 | 0.519 |
| Full-time work at 3-year follow-up, a % (n) | 56.6 (43) | 46.3 (31) | 1.6 | 0.218 |
| Treatment characteristics at follow-up d | ||||
| Antipsychotic treatment at 2-year follow-up, % (n) | ||||
| Not on antipsychotic | 16.0 (13) | 6.6 (5) | 3.6 c | 0.181 |
| Use of first-generation antipsychotic | 8.6 (7) | 7.9 (6) | ||
| Use of second-generation antipsychotic | 75.3 (61) | 85.5 (65) | ||
| Antipsychotic treatment at 3-year follow-up, % (n) | ||||
| Not on antipsychotic | 11.1 (9) | 12 (9) | 0.23 c | 0.911 |
| Use of first-generation antipsychotic | 8.6 (7) | 6.7 (5) | ||
| Use of second-generation antipsychotic | 80.2 (65) | 81.3 (61) | ||
| Chlorpromazine equivalent dose, mg: mean (s.d.) | ||||
| 2-year follow-up | 333.3 (344.2) | 308.2 (290.6) | 0.5 | 0.584 |
| 3-year follow-up | 364.9 (281.0) | 296.5 (261.7) | 1.5 | 0.142 |
a. A total of 71 participants in the intervention group and 67 participants in the control group were assessed at 2-year follow-up and 76 participants in the intervention group and 67 participants in the control group were assessed at 3-year follow-up.
b. Complete clinical record data were available for all participants.
c. Fisher's exact test was applied as the assumption of the chi-square test was not met.
d. A total of 81 participants in the intervention group and 76 participants in the control group had antipsychotic data at 2-year follow-up (3 participants died prior to 2-year follow-up); 81 participants in the intervention group and 75 participants in the control group had antipsychotic data at 3-year follow-up (4 participants died prior to 3-year follow-up).
Discussion
Main findings
The aim of the current study was to examine the sustainability of superior functional and clinical outcomes of 1-year extended early intervention compared with step-down care (3-year v. 2-year early intervention service) in patients with FEP, 1 and 2 years after the service ended. We found that there were no significant differences between the treatment groups in outcomes on functioning, symptom severity and service use during the 2-year post-trial follow-up period. Although significant time × intervention interaction effects were observed across 3-year follow-up in various functional measures, these findings appeared to be driven mainly by group differences that occurred in the first year of follow-up when extended specialised treatment was actively implemented. Our results thus indicate that despite extending the early intervention service to 3-year duration, superior outcomes achieved by specialised treatment still could not be maintained after transition to generic psychiatric service.
Of note, however, our negative findings concur with the results of two previous RCT follow-up studies, namely the OPUS and LEO trials, Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlaeger and Quach7,Reference Gafoor, Nitsch, McCrone, Craig, Garety and Power8 which also failed to demonstrate sustained superiority of early intervention over standard care in most treatment outcomes after service withdrawal. Nonetheless, despite lack of statistically significant between-group differences in functional ratings and employment outcome at post-trial follow-up, our results showed that patients randomised to the intervention group exhibited higher scores than those allocated to the control group in global functioning and most individual functional domains. Additionally, patients receiving extended early intervention attained a higher full-time employment rate and longer cumulative duration in full-time work than those managed by step-down care by the end of 3-year follow-up. Hence, this indicates that, overall, the intervention group still compared favourably with the control group in longer-term functional outcome, with the former having slightly better functioning, albeit statistically non-significant, than the latter group 2 years after service termination. It is also worth noting that although the intervention group exhibited functional decline in RFS domains of social networks after service withdrawal, improvement in work productivity and independent living was largely maintained. Subsequent loss of significant group difference in functioning was also partly because of gradual functional improvement in the control group during the post-trial follow-up.
Interpretation of our findings
Our findings, on the one hand, seem to support the proposition that positive effects of early intervention persist only as long as the service continues. Reference Linszen, Dingemans and Lenior33 This may further suggest that specialised treatment programmes do not alter the early course of illness in patients with FEP and hence lack lasting influence on longer-term outcome. On the other hand, a number of factors might contribute to an apparent loss of therapeutic benefits attained by extended early intervention, particularly on functional outcome, over the subsequent 2 years after transition to generic psychiatric care. First, it might be possible that a 3-year duration of early intervention for psychosis is still insufficient to maintain initial functional gains after the specialised service ended. Substantial evidence has also shown that a significant proportion of patients with FEP experience persistent functional impairment even in the presence of clinical remission. Reference Petersen, Thorup, Øqhlenschlaeger, Christensen, Jeppesen and Krarup34–Reference Chang, Tang, Hui, Lam, Chan and Wong36 A longer period of early intervention encompassing the entire hypothesised critical period (i.e. up to 5 years after onset of psychosis) Reference Birchwood, Todd and Jackson37 might be required to achieve sustained functional improvement (please refer to the two RCTs evaluating effectiveness of 5-year early intervention service for psychosis, namely the Danish OPUS II trial and the Canadian trial). Reference Lutgens, Lyer, Joober, Brown, Norman and Latimer14,Reference Albert, Melau, Jensen, Emborg, Jepsen and Fagerlund15
Second, the treatment intensity level of our early intervention might be significantly compromised by a high patient-to-case manager ratio, rendering it inadequate to maintain longer-term beneficial effects. Conversely, as our service is constrained by low resources and high case-loads compared with well-established early psychosis programmes implemented in some Western countries, our results should be generalised to other populations with caution.
Third, recent enhancement of community psychiatric services in Hong Kong Reference Chui, Mui, Chen and Cheung38 might, however, dilute the positive effect of an extended intervention on longer-term outcomes through an overall improvement in the treatment efficacy of generic psychiatric care received by participants during the post-trial period. This may in fact echo the recent findings of the OPUS II trial that suggested that the lack of superior effect of a 5-year extended intervention might partly be attributable to the high quality of standard community care provided to the control group. Reference Albert, Melau, Jensen, Emborg, Jepsen and Fagerlund15
Fourth, the potential disruptive effects of transfer of care from a specialised early intervention to a generic service, with subsequent withdrawal of case management and change of clinician for psychiatric follow-up, would likely lead to patients' perceived sense of loss, Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlaeger and Quach7 diminished treatment alliance Reference Secher, Hjorthoj, Austin, Thorup, Jeppesen and Mors10 and limited care coordination with significantly reduced multidisciplinary inputs. This may thus result in functional deterioration. In fact, our findings are partially in keeping with this postulation as functional decline in various domains, in particular the immediate and extended social networks of our cohort over the 2-year post-trial period mainly took place in the first year after service termination. A recent naturalistic study further revealed that extended continuity of care up to 5 years with lower treatment intensity after an initial 2-year intensive specialised intervention prevented loss of therapeutic gains on symptom and functional outcomes at 5-year follow-up in patients with FEP. Reference Norman, Manchanda, Malla, Winell, Harricharan and Northcott39
Fifth, it is plausible that the comparatively briefer DUP (median DUP: 13 weeks) of our cohort might obscure the potential differential effects of an extended intervention on longer-term outcomes between patients with short and prolonged untreated initial psychosis. Evidence from a recent RCT (RAISE study in the USA) has demonstrated that among patients with FEP who were allocated to a 2-year comprehensive treatment programme, those with a shorter DUP had significantly better symptom outcomes and quality of life at 2-year follow-up than their counterparts with prolonged DUP and those randomised to standard care. Reference Kane and Robinson40 Reassessment of the RAISE study cohort will help clarify whether such a differential treatment effect on patients with varying DUP would be critical in determining the durability of therapeutic benefits achieved by an early intervention service.
Strengths and limitations
The strengths of the study included a low drop-out rate (89.4% of the initial cohort completed the 3-year follow-up assessment), lack of differential attrition between treatment groups, masking of research staff assessing outcomes to treatment allocation, comprehensive evaluation of functional outcomes encompassing both global functioning and various specific functional dimensions, and availability of complete clinical record data regarding medication treatment, service use and other clinical variables for all participants. Several methodological limitations, however, warrant consideration in interpreting the study results. First, as the sample was recruited from the EASY programme, which treated patients aged 15–25 years only, our results may not be generalisable to people who are older at onset of psychosis. Second, data regarding the inputs of community psychiatric care and clinical psychologists after transition to generic services were not available, and thus precluded us from estimating the potential confounding effect of enhanced community services and provision of CBT on clinical and functional outcomes at post-trial follow-up.
Implications
This was the first RCT follow-up study examining the durability of treatment effects of extending an early intervention service for psychosis beyond 2 years. Our results indicate that superior symptom and functional outcomes attained by a 3-year extended early intervention (v. a 2-year early intervention) were not sustained after service withdrawal, even though initial improvement in some functional domains seem to be largely maintained during the post-trial follow-up. Aside from a genuine lack of efficacy of the specialised intervention on maintaining positive effects in patients with FEP, an absence of significant outcome difference between treatment groups at post-trial follow-up might also be attributable to an array of factors, which nonetheless could not be adequately addressed by the current study. Further investigation is warranted to clarify the roles of treatment delay, treatment intensity levels (such as case-load per case manager) and length of specialised service (for example, a 5-year intensive programme or extended continuity of care by a step-down service with lower treatment intensity) in determining the sustainability of early intervention on outcome improvement. Given the heterogeneous outcome trajectories in FEP, a universal provision of specialised service to all patients for an extended period might not be the most cost-effective approach in optimising long-term outcome. Future research is required to identify a subgroup of patients who may benefit most from extended intervention. More studies should also be conducted to delineate which specific treatment elements, from an integrated, multicomponent early intervention service, should be offered for an extended duration so as to maintain longer-term therapeutic benefits.
Funding
This study was supported by a grant from the Commissioned Research on Mental Health Policy and Services (SMH-29) of the Food and Health Bureau, the Government of Hong Kong Special Administrative Region. The funding body had no involvement in any aspect of the study or manuscript preparation.
Acknowledgements
The authors thank all the coordinating clinicians and staff from the psychiatric units involved in the study. We are also grateful to the individuals who participated in the study.







eLetters
No eLetters have been published for this article.