Bipolar disorder is associated with a high risk of episode relapse and the risk of relapse increases as the number of previous episodes increases, Reference Kessing, Hansen and Andersen1 with decreasing psychosocial Reference Tohen, Hennen, Zarate, Baldessarini, Strakowski and Stoll2 and cognitive function Reference Bourne, Aydemir, Balanza-Martinez, Bora, Brissos and Cavanagh3 as well as there being an increased risk of developing dementia in the long term. Reference Kessing and Nilsson4 Thus, the nature of bipolar disorder seems to imply the presence of an active process of neuroprogression that is considered to be at least partly mediated by inflammation, oxidative stress, apoptosis and changes in neurogenesis. Reference Berk, Berk, Dodd, Cotton, Macneil and Daglas5 For more than 60 years, lithium has been a first-line maintenance treatment for bipolar disorder Reference Goodwin and Geddes6,Reference Coryell7 and although the mechanisms of actions are not clarified, a wealth of data indicate that lithium may facilitate neural plasticity, Reference Gray and McEwen8 suggesting advantages of early intervention with the drug. However, it is unclear when to start prophylaxis. Not all patients will have an additional episode and the number needed to treat (NNT) to show a beneficial effect of lithium will be higher, the lower the risk is early in the course of illness. Reference Grunze, Vieta, Goodwin, Bowden, Licht and Möller9 Further, it is often claimed that the acceptance of prophylactic lithium treatment may be low in the early stages, Reference Grunze, Vieta, Goodwin, Bowden, Licht and Möller9 although this assumption does not seem to be correct. Reference Kessing, Hansen, Christensen, Dam, Gluud and Wettersley10
No randomised controlled trial has investigated the effect of lithium intervention early v. late in bipolar disorder and no observational longitudinal study has specifically focused on this issue. Nevertheless, there are some clinical indications that early initiation of lithium may increase the chances of a positive response to the drug. A meta-analysis including four observational studies with a total of 677 patients with bipolar disorder, Reference Kleindienst, Engel and Greil11 and a subsequent register-based nationwide study including 3762 patients with mania/bipolar disorder, Reference Kessing, Hellmund and Andersen12 have found that a higher number of prior admissions to psychiatric hospitals is related to poor response to lithium. Nevertheless, the focus of these studies was not on early v. late start of lithium but to broadly identify predictors of lithium response. Further, no association has been found regarding the number of previous episodes and response to prophylactic lithium in a meta-analysis of 1204 patients from 15 studies, Reference Kleindienst, Engel and Greil11 although it was concluded that for most potential predictors the evidence is not clear owing to a number of shortcomings of the included studies (see later).
In accordance with the poor evidence within the area, recommendations of when preventive treatment should be initiated differ among guidelines, as reviewed in the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines: Reference Grunze, Vieta, Goodwin, Bowden, Licht and Möller9 US guidelines favour commencement of maintenance treatment with the first manic episode Reference Sachs, Printz, Kahn, Carpenter and Docherty13 but, in contrast, the Danish guidelines state waiting for at least a second episode of illness, and only recommend maintenance treatment if these episodes occur within a rather short time interval (5 years). Reference Licht, Vestergaard, Kessing, Larsen and Thomsen14 The Dutch guidelines recommend maintenance treatment after one episode only if it is severely manic and there is a family history. Reference Grunze, Vieta, Goodwin, Bowden, Licht and Möller9,Reference Nolen, Kupka, Schulte, Knoppert-van der Klein and Honig15 Otherwise, with two episodes (one of them manic), maintenance treatment should be initiated if at least one episode is of particular severity or the patient has a positive family history, and following three episodes, prophylaxis is always recommended. Nevertheless, most guidelines - for example the WFSBP guidelines, Reference Grunze, Vieta, Goodwin, Bowden, Licht and Möller9 the Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines Reference Yatham, Kennedy, Parikh, Schaffer, Beaulieu and Alda16 and the British Association for Psychopharmcology guidelines Reference Goodwin17 - do not specify when long-term prophylactic treatment should be initiated,
The aim of the present study was to compare non-response rates among patients with bipolar disorder starting lithium early v. late during a 16-year follow-up period, using Danish nation-wide register-based linkage data including all patients with a diagnosis of mania/bipolar disorder in psychiatric hospital settings who subsequent to their diagnosis had started lithium. We hypothesised that starting lithium early is associated with an increased probability of lithium response.
Method
Danish register data
Data were obtained by linking Danish population-based registers using the unique personal identification number (CPR number), which is assigned to all 5.3 million persons living in Denmark, thus ensuring accurate linkage of information between registers, irrespective of changes in name, etc. In this way, the Danish Psychiatric Central Register Reference Munk-Jorgensen and Mortensen18 was linked with the Medicinal Product Statistics 19 and the Danish Medical Register on Vital Statistics. Reference Juel and Helweg-Larsen20
The Danish Psychiatric Central Register Reference Munk-Jorgensen and Mortensen18 contains data on all in-patients and out-patients treated at all psychiatric hospitals in Denmark from 1 January 1995 onwards as a part of the official Danish health survey. Reference Andersen, Madsen, Jorgensen, Mellemkjaer and Olsen21 Since 1 January 1994 the ICD-10 has been in use in the register. 22
The Medicinal Product Statistics contains data on all prescribed medication purchased at pharmacies from 1 January 1995 onwards. 19 In Denmark, all medication prescribed by doctors, such as lithium and anticonvulsants, is purchased only at pharmacies and the following data are electronically recorded in the Medicinal Product Statistics: the CPR number of the patient, the Anatomical Therapeutical Chemical (ATC) classification code 23 of the drug, and the dose and the number of tablets of the drug. Medication received during hospitalisation is not recorded in the register; neither is the daily dosing of the medication nor the indication for treatment.
The Danish Medical Register on Vital Statistics Reference Juel and Helweg-Larsen20 contains data on death.
Study sample
We identified all individuals who received a main ICD-10 22 index diagnosis of a single manic/mixed episode or bipolar disorder (ICD-10 code: DF30-31.9, 38.0) at any contact with psychiatric in-patient or out-patient service (the ‘index diagnosis’) and who subsequently purchased lithium (ATC codes: N05AN, N05AN01) (the ‘index purchase’) during the study period from 1 January 1996 to 31 December 2012. From this population we excluded all patients who (a) had received a diagnosis of schizophrenia between the index diagnosis and the index purchase, and (b) purchased lithium once only, in a period from the index purchase to half a year after this date.
Definition of early v. late intervention with lithium
We defined early v. late intervention with lithium in two ways: (a) patients with a diagnosis of a single manic episode/bipolar disorder who started lithium following their first contact v. patients who started lithium following later contacts; and (b) patients who started lithium following a diagnosis of a single manic episode (ICD-10 code: DF30) or a single mixed episode (ICD-10 code: DF38, 38.0, 38.00) v. those who started lithium following a diagnosis of bipolar disorder (ICD-10 code: DF31-31.9), as at least two affective episodes (with at least one hypomanic, manic or mixed episode) are required to fulfil ICD-10 criteria for a diagnosis of bipolar disorder. 22
Definition of excellent responders and non-responders to lithium
We used the same definition of lithium (non-)response as in our prior study. Reference Kessing, Hellmund and Andersen12 Any definition of response depends on the time period at risk in contrast to non-response that is defined accurately in time (i.e. at a given date). Thus, patients with non-response to lithium at a given time during follow-up were defined as patients who, in a period starting half a year after the index purchase of lithium, at that time received polypharmacy or were admitted to a psychiatric ward. Polypharmacy was defined as lithium combined with at least one other psychotropic drug (antidepressant, antipsychotic or anti-epileptic). Non-responders as well as responders were allowed to receive antidepressants, antipsychotics or anti-epileptics for the treatment of acute episodes during the initial half-year stabilisation period following the index lithium treatment. In addition, non-responders and responders were allowed to receive hypnotics or tranquilisers throughout the course of their illness. In this way, an excellent responder to lithium monotherapy was defined as a patient who was not (yet) a non-responder at a given time.
The response type was defined within the study period from 1 January 1995 to 31 December 2012 (with a first purchase at least half a year before the end of the study period).
Statistical analyses
We used survival analysis to take time at risk into consideration, with non-response to lithium monotherapy as the outcome. Non-response is defined accurately in time (i.e. at a given date) in contrast to response. Thus, hazard ratios (HRs) for lithium non-response were estimated in a Cox regression model, with risk time starting from half a year following the index purchase of lithium (or from the date of discharge from hospital if the hospitalisation period extended this date by more than half a year). Censoring was done at the date of death, at a diagnosis of schizophrenia during follow-up and at the end of the study period (31 December 2012).
Results are presented unadjusted and adjusted for important covariates. A priori, we found no indications from the literature or from clinical experience that patients who start lithium early should have a more severe or, in contrast, a more mild form of mania/bipolar disorder than those patients who have lithium prescribed later. Nevertheless, a priori we decided to adjust the analyses for covariates that are well known to influence the rate of recurrence or the effect of or adherence to mood stabilisers in bipolar disorder: gender; Reference Kessing, Hansen and Andersen1,Reference Kessing, Andersen and Mortensen24,Reference Kessing, Sondergard, Kvist and Andersen25 age (age at inclusion as a continuous variable); Reference Kessing, Andersen and Mortensen24,Reference Kessing, Sondergard, Kvist and Andersen25 socioeconomic status (unemployed, passive, student, missing information; ‘employed’ was the reference); Reference Kessing, Andersen and Mortensen24 bipolar index diagnosis (depressive, manic, mixed; ‘remission, other or unspecified’ was the reference); Reference Kessing, Hellmund and Andersen12 and auxiliary diagnoses (auxiliary somatic diagnoses: yes/no; auxiliary diagnoses related to substance misuse: yes/no; auxiliary psychiatric diagnoses: yes/no). Reference Kessing26,Reference Farren, Hill and Weiss27
To get a graphical presentation over time for patients with early v. late lithium intervention, we estimated the probabilities of being an excellent responder using the Kaplan-Meier estimator.
A P-value less than 5% (0.05) indicated significance throughout the analysis.
Results
We identified a total of 4714 patients with a main ICD-10 index diagnosis of mania or bipolar disorder who subsequently purchased lithium, and more than twice during the first half a year after the index purchase, and who had not had a diagnosis of schizophrenia prior to initial purchase of lithium. Among these 4714 patients, 3496 (74.2%) received an antidepressant before the index purchase of lithium (median time from start of antidepressant use to index mania/bipolar diagnosis: 3.3 years, quartiles 1.2-6.7), 2821 (59.8%) received an antipsychotic (median time from start of antipsychotic use to index mania/bipolar diagnosis: 1.9 years, quartiles 0.4-5.1) and 1384 (29.4%) received an anti-epileptic prior to starting lithium (median time from start of anti-epileptic use to index mania/bipolar diagnosis: 1.6 years, quartiles 0.4-4.4).
Results are presented according to our two definitions of early v. late intervention with lithium. The first definition divided the sample into patients starting lithium following first contact ever with hospital psychiatry (as an in-patient or out-patient) v. those starting lithium at later contacts. Using this definition, a total of 715 patients (15.2%) started lithium following their first contact ever and 3999 patients (84.8%) started lithium at later contacts.
Figure 1 shows the Kaplan-Meier estimates of non-response to lithium in monotherapy. The probability of still being an excellent responder for patients starting lithium following first contact was 13.3% (95% CI 10.9-16.2) at 5 years’ follow-up and 8.7% (95% CI 6.6-11.5) at 10 years’ follow-up. The corresponding probabilities for patients starting lithium at later contacts were 6.3% (95% CI 5.5-7.0) at 5 years’ follow-up and 4.0% (95% CI 3.4-4.7) at 10 years’ follow-up. In a Cox regression model, patients who started lithium following their first contact had a significantly decreased rate of non-response to lithium, as they switched to or added other psychotropics or were admitted to hospital, compared with patients who started lithium following later contacts (unadjusted analyses: P<0.0001; HR = 0.73, 95% CI 0.67-0.90). This association was somewhat decreased (adjusted analyses: P<0.0001; HR = 0.87, 95% CI 0.76-0.91) when adjusting for the a priori defined covariates (gender, age, socioeconomic status, bipolar index diagnosis, auxiliary somatic diagnoses, auxiliary diagnoses related to substance abuse, and auxiliary psychiatric diagnoses).

Fig. 1 Rate of non-response to lithium monotherapy: first v. later contacts.
Table 1 Distribution and effect of predictors of non-response to lithium following first v. later contactsFootnote a

| Start of lithium following first contact |
Start of lithium following later contact |
Hazard ratio (95 % CI) |
P | |
|---|---|---|---|---|
| n (%) | 715 (15.2) | 3999 (84.8) | ||
| Gender, % | ||||
| Male | 49.7 | 41.3 | 1 | <0.0001 |
| Female | 50.4 | 58.7 | 1.19 (1.12-1.26) | |
| Age at first purchase, years: median (quartiles) | 46.7 (34.2-58.1) | 49.1 (37.8-59.3) | 1.02 (0.99-1.05) | 0.2 |
| Socioeconomic status, % | ||||
| Employed | 46.7 | 28.5 | 1 | |
| Unemployed | 9.4 | 8.4 | 1.20 (1.06-1.35) | |
| Early retired | 8.0 | 28.4 | 1.63 (1.50-1.78) | <0.0001 |
| Retired | 14.7 | 16.8 | 1.28 (1.13-1.45) | |
| Student | 6.2 | 3.3 | 0.86 (0.72-1.04) | |
| Missing | 0.1 | 14.7 | 0.71 (0.18-2.86) | |
| Other | 15.0 | 0.1 | 1.21 (1.10-1.38) | |
| Bipolar index diagnosis, % | ||||
| Remission, other, unspecified | 10.4 | 15.1 | 1 | |
| Depressive | 24.9 | 29.9 | 1.11 (1.00-1.22) | <0.0001 |
| Manic | 56.1 | 44.5 | 0.93 (0.85-1.02) | |
| Mixed | 8.7 | 10.4 | 1.13 (1.00-1.28) | |
| Auxilliary diagnosis, % | ||||
| No auxiliary diagnosis | - | - | 1 | |
| Psychiatric | 3.2 | 6.7 | 1.14 (1.01-1.29) | 0.04 |
| Substance misuse | 6.2 | 9.3 | 1.16 (1.04-1.30) | 0.007 |
| Somatic | 5.2 | 5.3 | 1.18 (0.98-1.29) | 0.08 |
a. Adjusted for all variables in the table.
Results in bold are significant.
Table 1 shows predictors of non-response to lithium monotherapy as estimated in the Cox regression model with adjustment of all variables listed in the table. As can be seen, female gender, being unemployed, early retired or retired, having a depressive or mixed index episode and an auxiliary psychiatric diagnosis including substance misuse were all associated with significantly increased rates of non-response to lithium. There were no significant associations with age or somatic comorbidity.
According to the second definition of early v. late intervention with lithium, the sample was divided into 410 patients (8.7%) who started lithium following a diagnosis of a single manic/mixed episode v. 4304 patients (91.3%) who started lithium following a diagnosis of bipolar disorder.
For patients who started lithium following a diagnosis of a single manic/mixed episode, the probability of still being an excellent responder to lithium was 13.2% (95% CI 10.2-17.2) at 5-years’ follow-up and 10.1% (95% CI 7.3-13.8) at 10-years’ follow-up (Fig. 2). The corresponding probabilities for patients starting lithium following a diagnosis of bipolar disorder were 6.7% (95% CI 5.9-7.5) at 5-years’ follow-up and 4.2% (95% CI 3.6-4.9) at 10-years’ follow-up. Thus, patients who started lithium following a diagnosis of a single manic/mixed episode had a significantly decreased rate of non-response to lithium compared with patients who started lithium following a diagnosis of bipolar disorder (unadjusted analyses: P<0.0001; HR = 0.70, 95% CI 0.63-0.78). The association was changed only slightly when adjusting for the a priori defined covariates (adjusted analyses: P<0.0001; HR = 0.75, 95% CI 0.67-0.84).
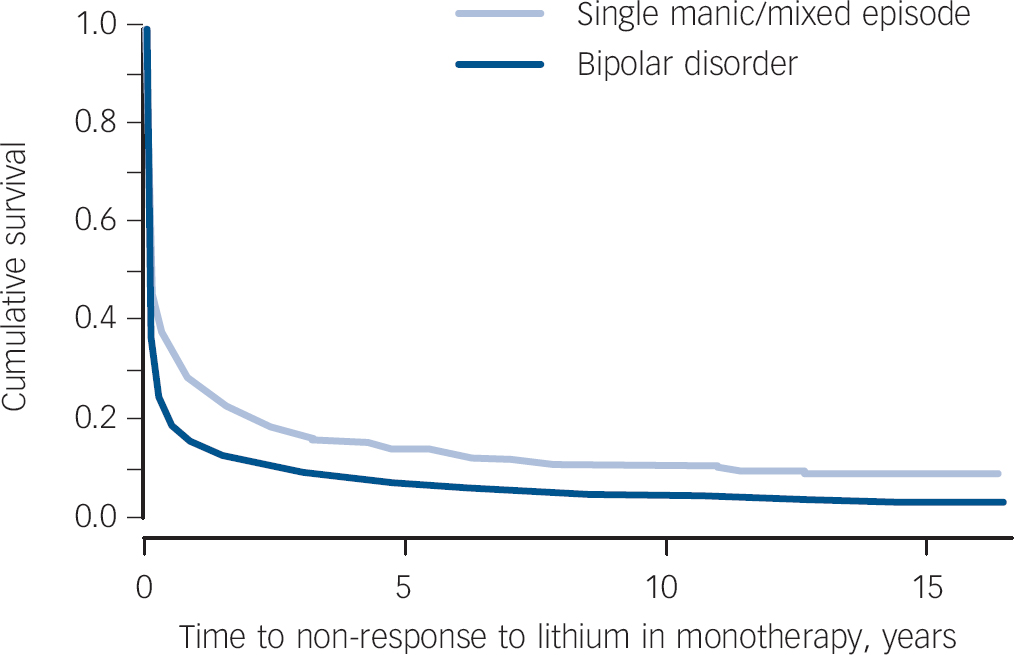
Fig. 2 Rate of non-response to lithium monotherapy: single manic/mixed episode v. a diagnosis of bipolar disorder.
Similar to Table 1, Table 2 presents predictors of non-response using the second definition of early v. late intervention with lithium (in this table the index bipolar disorder diagnosis is not relevant). As one would expect, the pattern of predictors in Table 2 is identical to that in Table 1.
Discussion
This is the first study to compare response rates among patients with mania/bipolar disorder starting prophylactic lithium early v. late. We used data from a nationwide population-based register linkage study that included more than 4700 patients with mania/bipolar disorder who initiated lithium treatment and who were followed (in a historically prospective way) for up to 16 years. Early v. late intervention with lithium was defined in two different ways: start of lithium following first v. later contact for mania/bipolar disorder and start of lithium following a single manic/mixed episode v. a diagnosis of bipolar disorder. Regardless of the definition used, patients who started lithium early had significantly decreased rates of non-response to lithium compared with patients starting lithium later (first v. later contact: unadjusted analyses: P<0.0001; HR = 0.73, 95% CI 0.67-0.90, adjusted analyses: P<0.0001; HR = 0.83, 95% CI 0.76-0.91; single manic/mixed episode v. bipolar disorder: unadjusted analyses: P<0.0001; HR = 0.70, 95% CI 0.63-0.78, adjusted analyses: P<0.0001; HR = 0.75, 95% CI 0.67-0.84).
We defined lithium response in a rather rigorous way as per our prior study on predictors of excellent lithium response, Reference Kessing, Hellmund and Andersen12 as patients who continued with lithium monotherapy and did not get admitted to a psychiatric ward from a period half a year after initial start of lithium onwards. Defined in this way, excellent response to lithium monotherapy may reflect a ‘cure’ from further affective episodes following an upstart period of lithium, although subthreshold symptomatology may have occurred without resulting in a switch to or addition of another drug than lithium. Reference Kessing, Hellmund and Andersen12 This outcome measure includes two valid clinical robust indicators of lithium response: lithium prescribed in monotherapy and no need for psychiatric hospitalisation. We used survival analysis to take time at risk into consideration and with non-response to lithium monotherapy as the outcome since non-response is defined accurately in time (i.e. at a given date) in contrast to response.
Table 2 Distribution and effect of predictors of non-response to lithium following a diagnosis of a single manic or mixed episode v. a diagnosis of bipolar disorderFootnote a

| Start of lithium
following a diagnosis of a single manic or mixed episode |
Start of lithium
following a diagnosis of bipolar disorder |
Hazard
ratio (95 % CI) |
P | |
|---|---|---|---|---|
| n (%) | 410 (8.7) | 4304 (91.3) | ||
| Gender, % | ||||
| Male | 51.5 | 41.8 | 1 | <0.0001 |
| Female | 48.5 | 58.3 | 1.20 (1.12-1.27) | |
| Age at entry date, years: median (quartiles) | 46.7 (32.7-57.2) | 49.0 (37.5-59.3) | 1.02 (0.99-1.05) | 0.2 |
| Socioeconomic status, % | ||||
| Employed | 40.7 | 30.3 | 1 | |
| Unemployed | 7.8 | 8.6 | 1.22 (1.09-1.38) | |
| Early retired | 16.6 | 26.1 | 1.65 (1.51-1.79) | <0.0001 |
| Retired | 14.4 | 16.6 | 1.30 (1.14-1.47) | |
| Student | 7.1 | 3.4 | 0.86 (0.72-1.03) | |
| Missing | 0 | 0.1 | 0.62 (0.15-2.47) | |
| Other | 13.4 | 14.9 | 1.22 (1.10-1.34) | |
| Auxilliary diagnosis, % | ||||
| No auxiliary diagnosis | - | 1 | ||
| Psychiatric | 5.1 | 6.3 | 1.16 (1.03-1.32) | 0.02 |
| Substance misuse | 6.1 | 9.1 | 1.16 (1.04-1.29) | 0.008 |
| Somatic | 4.9 | 5.3 | 1.13 (0.99-1.30) | 0.7 |
a. Adjusted for all variables in the table.
Results in bold are significant.
Comparison with prior studies
As mentioned initially, no randomised trial or observational study has specifically compared response to lithium in early v. late intervention. Further, the review and meta-analysis by Kleindienst et al of predictors of response to lithium that included 1204 patients from 15 studies Reference Kleindienst, Engel and Greil11 concluded that for most potential predictors the evidence is not clear, owing to a number of shortcomings of the included studies. Regarding studies including data on the association between the number of prior affective episodes and response to lithium, shortcomings include: (a) small sample sizes (from 10 to 247 patients), Reference Kleindienst, Engel and Greil11 (b) relatively short follow-up periods (i.e. <2 years with a few exceptions of up to 5 or 7 years, and one study covering up to 27 years, however including 118 patients only), Reference Kulhara, Basu, Mattoo, Sharan and Chopra28 (c) selection bias, as most samples of patients are recruited from tertiary university specialised centres Reference Berghofer, Alda, Adli, Baethge, Bauer and Bschor29 and (d) high drop-out rates during follow-up. Since this review, two studies have analysed the association between the starting point of lithium treatment and response to lithium: one study found no effect of the latency between onset of illness and start of lithium treatment (n = 242), Reference Berghofer, Alda, Adli, Baethge, Bauer and Bschor29 and the other found that the response rate to lithium decreased with the number of prior episodes (n = 336). Reference Pfennig, Schlattmann, Alda, Grof, Glenn and Müller-Oerlinghausen30 It should be emphasised that none of the above-mentioned studies specifically compared or were designed to compare response rates among patients who had started lithium early v. patients who had started lithium later, which was the focus and aim of our study.
It should be noted that our estimates of excellent lithium response are rather conservative as we included all patients in the analyses using survival methods regardless of whether they in fact continued lithium treatment following half a year, as we wanted to calculate ‘intention to treat’ estimates, i.e. the response rates among all patients whom the clinician decided to treat with lithium and who tolerated lithium initially. Few long-term studies have reported the actual response rates among all patients initiated on lithium (intention to treat analyses). In fact, we have identified only one such study; Maj et al identified 78 (19.4%) of 402 patients who started lithium and had no affective episodes or were taking other psychotropic drugs in addition to lithium during a 5-year follow-up period Reference Maj, Pirozzi, Magliano and Bartoli31 (for more details see Kessing et al Reference Kessing, Hellmund and Andersen12 ). Similarly in our study, the proportion of ‘excellent lithium responders’ was rather low even for patients starting lithium early (start of lithium following first contact: 13.3% (95% CI 10.9-16.2) and start of lithium following a first manic/mixed episode: 13.2% (95% CI 10.2-17.2) at 5 years’ follow-up). The study included all patients with a bipolar diagnosis who purchased lithium at least twice within a half-year period, suggesting that these patients (initially) tolerated lithium (as they continued to purchase lithium following the intake of the first package of lithium (100 tablets)).
The identified predictors of non-response to lithium were similar to those identified in our prior study on predictors of excellent lithium response, Reference Kessing, Hellmund and Andersen12 using a slightly different design. A comparison with prior studies of predictors of lithium response have been provided in our previous study. Reference Kessing, Hellmund and Andersen12
Advantages of the present study
There are a number of advantages related to the study. The study includes data from a population-based and nationwide register linkage study on all patients with a diagnosis of bipolar disorder within psychiatric hospital healthcare settings (as in-patients or out-patients) who initiated lithium treatment during a study period of up to 16 years. Data from the Medicinal Product Statistics is close to 100% accurate and lithium is frequently used in Denmark. Reference Kessing, Hellmund and Andersen12 All treatment data were included for all out-patient settings (i.e. within psychiatric hospital out-patients, community psychiatric centres, private specialist practice and general practice). The register contains no data on the prescribed daily dose of lithium or lithium serum levels, although these are routinely monitored according to standardised clinical practice.
The design of the study helps to overcome the four pitfalls mentioned earlier: the study includes a large sample size; a long follow-up period; reduced risk of selection bias, as the study included all patients nationwide with a diagnosis of mania/bipolar disorder who subsequently initiated treatment with lithium; and no drop-out rate, as register data are routinely collected for all individuals in Denmark regardless of ongoing research projects such as the present study.
The hazard ratios, predictors, and 5- and 10-year risks of non-response to lithium were rather similar in the two models using two different definitions of early v. later intervention, strengthening our findings as they do not seem to be dependent on the definition of early intervention with lithium.
Limitations of the present study
The diagnoses in the Danish Psychiatric Central Register originate from different clinicians all over Denmark using ICD-10 criteria for bipolar disorder and are not standardised for research purposes. The ICD-10 criteria for bipolar disorder include bipolar type I as well as bipolar type II disorder, but do not discriminate between these two.
Our results could be a result of confounding factors if patients who started early with lithium had a more severe or a milder form of mania/bipolar disorder than patients who received lithium later. We find, however, no indications for such associations from the literature or from clinical experience. We adjusted the analysis of the association between the starting point of lithium intervention (early v. late) and non-response to lithium for a priori defined covariates (gender, age, socioeconomic status, bipolar index diagnosis, auxiliary somatic diagnoses, auxiliary diagnoses related to substance misuse, and auxiliary psychiatric diagnoses). All of these variables turned out to be significantly associated with intervention time (early v. late) as well as with lithium non-response, except age and somatic comorbidity. In this way, we believe that we have adjusted for important potential confounders within psychosocial factors, the diagnosis of mania/bipolar disorder itself and comorbidity.
Another important confounding factor, which is more difficult to take into consideration, could be that only patients with so-called ‘typical’ bipolar disorder received lithium early on, whereas patients with ‘atypical’ bipolar disorder with, for example, inter-episodic residual symptomatology, mood incongruent psychotic features or rapid cycling (e.g. Pfennig et al Reference Pfennig, Schlattmann, Alda, Grof, Glenn and Müller-Oerlinghausen30 ) may have received other mood stabilisers (e.g. atypical antipsychotics or anticonvulsants). This is a potential bias because patients with typical bipolar disorder may have an overall better outcome than patients with atypical bipolar disorder as found in some Reference Pfennig, Schlattmann, Alda, Grof, Glenn and Müller-Oerlinghausen30 but not all studies. Reference Calabrese, Rapport, Youngstrom, Jackson, Bilali and Findling32 It is difficult to know whether a tendency to prescribe lithium early for more typical bipolar disorder has been prevalent among Danish psychiatrists during the study period. Although Danish psychiatrists may have known that the initial opinion that people with rapid-cycling bipolar disorder are refractory to lithium treatment may not be correct, Reference Fountoulakis, Kontis, Gonda and Yatham33 this confounding factor or other residual confounding cannot be excluded when explaining our findings.
Excluding people who purchased lithium once - only in a period from the index purchase to half a year after this date - will include patients who are partially or minimally adherent. This exclusion criterion may result in a possible underestimation of the difference in lithium response between early and late starters of lithium.
Severity of illness and age at first contact/first manic or mixed episode
It should be noted that patients included in the study had more severe forms of bipolar disorder, leading to psychiatric hospital contact as in-patients or out-patients. For patients starting lithium early, the median age of 46.7 years at inclusion in the study was rather high, although with a substantial variation: 25% were below 34 years and 25% above 58 years of age at inclusion. There may be three major reasons for this high age at first contact/first manic or mixed episode. First, patients with a severe or more abrupt first manic episode resulting in hospital contact may have a higher age at onset than patients with milder first episodes. Second, there may be a delay in the diagnosis of bipolar disorder, as early episodes may be mistaken as transient psychosis, reaction to stress/adjustment disorder, or alcohol or other substance misuse, Reference Kessing34 so a proportion of the patients may have had prior episodes. Notably in the present sample, 59.8% of the patients had received an antipsychotic prior to starting lithium, with a median time from start of antipsychotic to index mania/bipolar diagnosis of 1.9 years (quartiles 0.4-5.1). Third, as many as half of patients with bipolar disorder present with a depressive episode or recurrent depression as first episode(s). Reference Kessing34,Reference Perugi, Micheli, Akiskal, Madaro, Socci and Quilici35 Accordingly, 74.2% of the patients received an antidepressant before starting lithium in the present study, with a median time from start of antidepressant use to mania/bipolar diagnosis of 3.3 years (quartiles 1.2-6.7). As expected, patients who had received an antidepressant prior to starting lithium had a higher rate of non-response to lithium (HR = 1.47, 95% CI 1.37-1.59, P<0.0001, adjusted analysis for covariates as in Table 1). Similarly, prior use of antipsychotics (HR = 1.31, 95% CI 1.23-1.34), P<0.0001, adjusted analysis) and anticonvulsants (HR = 1.56, 95% CI 1.42-1.71, P<0.0001, adjusted analysis) were associated with a higher rate of non-response to lithium.
In summary, the findings of the study may be generalised only to patients with more severe forms of mania/bipolar disorder who may have a later onset of illness, although we find it most likely that early intervention with lithium will also have advantages in younger samples. Thus, preliminary findings suggest that young adults with bipolar disorder may benefit even more than older adults from early intervention combining pharmacological treatment and group psychoeducation. Reference Kessing, Hansen, Christensen, Dam, Gluud and Wettersley10
Clinical implications
The evidence for a prophylactic effect of lithium has increased during recent years Reference Coryell7,Reference Geddes, Goodwin, Rendell, Azorin, Cipriani and Ostacher36-Reference Kessing, Hellmund and Andersen38 and treatment with lithium is now anticipated to get a revival in use. Reference Malhi39,Reference Ghaemi40 Accordingly, recent guidelines have made stronger recommendations for lithium as the only first choice for prophylactic treatment (e.g. Pfennig et al Reference Pfennig, Bschor, Falkai and Bauer41 ). In clinical practice it is a crucial decision when to start prophylactic treatment with lithium. We have no data from randomised trials to guide this decision. The present study is the first observational study to investigate the question, using Danish nationwide longitudinal register-based linkage data of all patients starting lithium following a diagnosis of mania/bipolar disorder. Although residual confounding cannot be entirely excluded, the results clearly suggest that early prophylactic intervention with lithium following first psychiatric hospital contact or following the first manic/mixed episode is associated with improved long-term response to lithium.







eLetters
No eLetters have been published for this article.