The signs and symptoms of psychotic illness span a diverse range of phenomena in the domains of thought, emotion and behaviour. These different phenomena respond differently to treatment (Reference Johnstone, Crow and FrithJohnstone et al, 1978), implying distinguishable underlying pathophysiological processes. A scale for assessing response to treatment should have the following characteristics:
-
(a) the range of relevant phemomena should be covered by a set of items that are jointly exhaustive of these phenomena and yet mutually exclusive;
-
(b) distinguishable phenomena that are expected to respond differently to treatment should be covered by separate items;
-
(c) adequate interrater reliability should be achievable by a training programme that would be practical for use in multi-centre studies;
-
(d) the required interview should be tolerable to seriously ill patients;
-
(e) the scores should be sensitive to change.
We describe an investigation of interrater reliability, factor structure and sensitivity to change of a new scale for the assessment of the Signs and Symptoms of Psychotic Illness (the SSPI).
Existing instruments for assessing psychotic symptoms
Assessment instruments such as the Present State Examination (PSE; Reference Wing, Cooper and SartoriusWing et al, 1974) and the Comprehensive Assessment of Symptoms and History (CASH; Reference AndreasenAndreasen, 1986) provide a comprehensive coverage of the symptoms that occur in psychotic illnesses, but the length of interview required for these comprehensive scales makes them scarcely practical for use in treatment trials. The Brief Psychiatric Rating Scale (BPRS; Reference Overall and GorhamOverall & Gorham, 1962) has been used very widely in trials of antipsychotic treatment but the item composition does not reflect recent emphasis on the negative symptoms of schizophrenia. More recently, the Positive and Negative Symptom Scale (PANSS; Reference KayKay, 1991) was developed by extending the BPRS to provide more detailed coverage of negative symptoms of schizophrenia. However, several of the items of PANSS (e.g. impaired volition, impaired abstract thinking) include phenomena that embrace both impoverishment of mental activity and disorganisation of mental activity. In addition, the scoring guidelines for PANSS item N1 (blunted affect) indicate that incongruent affect might contribute to the score for blunted affect.
Furthermore, in both PANSS and BPRS a single phenomenon might contribute to the score for more than one item. For example, in the PANSS item suspiciousness, the highest score denotes beliefs of delusional intensity. A persecutory delusion might contribute strongly to PANSS scores for suspiciousness, delusions and unusual thought content. Similarly, a grandiose delusion might contribute to scores for grandiosity, delusions and unusual thought content, whereas a delusion of guilt might contribute to scores for guilt feelings, delusions and unusual thought content. As a consequence, alleviation of a persecutory, grandiose or guilty delusion might have a greater impact on the global score than the alleviation of some other psychotic symptom.
The Signs and Symptoms of Psychotic Illness scale
The SSPI comprises 20 items (Table 1). The first 19 items were designed to elicit the major signs and symptoms of psychotic illness. The majority of these were selected on the assumption that the signs and symptoms of psychotic illnesses represent at least five distinguishable pathological processes: depression, excitation, diminished psychomotor activity, disorganised psychomotor activity and reality distortion (Reference Liddle, Carpenter and CrowLiddle et al, 1994). Item 20 assesses insight.
Table 1 Intraclass correlation coefficients (ICCs) for items and total score (computed for the subsample of 63 cases) and the prevalence of item scores greater than unity in the four main diagnostic groups in the entire sample
| ICC | Prevalence (% of cases with item score > 1) | ||||
|---|---|---|---|---|---|
| Acute schizophrenia | Persistent schizophrenia | Schizoaffective disorder | Mania | ||
| Anxiety | 0.84 | 36 | 24 | 27 | 36 |
| Depression | 0.89 | 17 | 12 | 36 | 29 |
| Anhedonia | 0.75 | 43 | 55 | 64 | 7 |
| Elation | 0.83 | 10 | 5 | 45 | 79 |
| Insomnia | 0.87 | 16 | 7 | 36 | 64 |
| Somatisation | 0.69 | 17 | 45 | 18 | 36 |
| Delusions | 0.89 | 77 | 76 | 82 | 50 |
| Hallucinations | 0.87 | 52 | 67 | 36 | 29 |
| Impaired attention | 0.75 | 47 | 76 | 45 | 64 |
| Disorientation | 0.82 | 6 | 17 | 9 | 0 |
| Overactivity | 0.75 | 8 | 14 | 18 | 79 |
| Underactivity | 0.82 | 24 | 43 | 36 | 0 |
| Flat affect | 0.68 | 47 | 52 | 18 | 14 |
| Inappropriate affect | 0.78 | 19 | 24 | 9 | 7 |
| Pressure of speech | 0.71 | 8 | 12 | 18 | 57 |
| Poverty of speech | 0.80 | 27 | 40 | 0 | 0 |
| Thought form disorder | 0.80 | 59 | 50 | 45 | 50 |
| Peculiar behaviour | 0.69 | 20 | 31 | 9 | 43 |
| Hostility | 0.79 | 17 | 17 | 36 | 50 |
| Insight | 0.80 | 66 | 72 | 63 | 63 |
| SSPI total | 0.82 | ||||
To avoid the problem of some specific types of delusion contributing to the score for several different items, and thereby making a disproportionate contribution to global score, the SSPI has a single item for severity of delusions that contributes to the score for global severity. In addition, there is an optional delusion sub-scale, including items for specific types of delusions (guilty, grandiose, paranoic, Schneiderian) and for the mood incongruence of delusions. In situations in which the specific content of delusions is of interest, such as for the purpose of diagnosis or for measuring response to a treatment that might be expected to have a different effect on different types of delusions, the sub-scale item scores can be used. Similarly, a single score for severity of hallucinations contributes to the score for global severity, but there is a separate optional hallucination sub-scale that contains items for second person auditory hallucinations, Schneiderian hallucinations and mood incongruence of hallucinations.
Item content is defined in a glossary (available on request from the author) and item scores are assigned according to specified guidelines, on the basis of observed behaviour at interview and responses to questions regarding symptoms and behaviour during the past week. The interview is semi-standardised. There are 15 specified direct questions about symptoms and whenever these questions elicit evidence of psychopathology the interviewer asks further questions to establish the nature and severity of the phenomena. In addition, the interviewer conducts an inquiry into occupational activities, social function and the patient's understanding of the illness and its treatment. A brief test of attention and orientation is administered. The interview typically lasts 25 min. If there is reason for concern regarding the reliability of the patient's report of behaviour, a nurse or relative should be asked about level of activity and evidence of hostile or peculiar behaviour.
Severity of each item is rated in the range 0-4 (1, experiences or behaviour that are of questionable abnormality; 2, phenomena that are definitely abnormal but mild; 3, pathology of moderate severity that has a substantial impact on mental functioning; 4, severe psychopathology).
METHOD
Patients
A total of 155 patients were recruited, each suffering from acute or persistent psychotic illness diagnosed according to DSM-IV criteria (American Psychiatric Association, 1994) and receiving in-patient treatment or out-patient care from community mental health teams with a mandate to serve patients suffering from severe mental illness. Patients were classified as acutely ill if they had been admitted to hospital and/or suffered a decline in Global Assessment of Function (GAF; American Psychiatric Association, 1994) of 10 points or more in the preceding 4 weeks. Patients were classified as persistently ill if they had a GAF score of less than 51 and did not satisfy the criterion for acute illness. The study procedure was approved by the hospital and university research ethics review committees.
Interrater reliability
Interrater reliability was determined in two studies. Two novice raters participated in the first study: two trainee psychiatrists (K. K. and G. D.), each with 3 years of psychiatric clinical training, underwent an SSPI training programme that entailed the scoring of five video-recorded SSPI interviews and comparing their scores with those assigned by the senior investigator (P. F. L.) who had designed the scale. After completion of this training, K. K. and G. D. interviewed 32 patients. For each interview, one of the trainees acted as the interviewer while the other was a silent observer. At completion of the interview they each assigned SSPI scores without conferring. In the second study, K. K., G. D. and P. F. L. each scored video-recorded interviews of 20 patients. The intraclass correlations between the ratings by the three investigators were computed.
Factor analysis
To determine the factor structure of SSPI scores, factor analysis was performed on the scores for the 19 SSPI items (excluding insight) assigned at the initial interview of each of the 155 participating patients. Insight was excluded from the factor analysis because it was assessed in part on the basis of the patients' beliefs regarding their symptoms. Principal components with eigenvalues greater than unity were extracted, and these components were subjected to oblique rotation using the Promax procedure, employing SPSS for Windows, release 10.0.5 (1999). Scores for each subject for each factor were assigned by summing the item scores for all items with a loading greater than 0.6 in that factor. This simple procedure was adopted because a sum of relevant item scores can be compared readily between patients from different samples. Analysis of variance was employed to compare the factor scores in different diagnostic groups.
Sensitivity to change
To determine the sensitivity of SSPI scores to change in clinical state, longitudinal assessments were performed in 33 acutely ill patients. The SSPI scores were assigned shortly after admission to hospital and again either when the patient was judged fit for discharge from hospital or after a maximum of 6 weeks. In 22 of these cases, the overall severity of illness was assessed using the severity score of the Clinical Global Impression (CGI) scale (Reference GuyGuy, 1976) by the patient's attending physician on the day of each SSPI assessment. The correlation between change in SSPI global score and change in CGI severity score was computed.
RESULTS
Of the 155 participating patients 83 had acute schizophrenia, 42 had persistent schizophrenia, 11 had schizoaffective disorder, 14 had bipolar mood disorder currently manic, 1 had bipolar disorder currently depressed and 4 had other psychotic disorders. The mean age was 35 years (range 16-60 years) and the mean duration of illness since first recognition of psychotic symptoms was 11 years (range 2 months-37 years). There were 86 male patients and 144 of the patients were receiving antipsychotic medication at the time of first assessment. All patients tolerated the SSPI interview. The prevalence of scores of 2 or more (denoting definitely abnormal phenomena) for each item in each of the four main diagnostic groups (acute schizophrenia; persistent schizophrenia; schizoaffective disorder, and bipolar disorder, manic phase) is shown in Table 1.
Interrater reliability
There were no significant differences between intraclass correlation coefficients (ICCs) for any of the three possible pairs of raters, nor between the two studies. Therefore, the overall ICC values for each item and for the SSPI total score derived from both studies (63 subjects in total: 43 assessed by two raters and 20 assessed by three raters) were computed according to the procedure described by Bartko & Carpenter (Reference Bartko and Carpenter1976), as shown in Table 1. All coefficients for individual items indicate acceptable interrater reliability (ICC>0.68). For more than half of the individual items and for the SSPI total score, interrater reliability was excellent (ICC>0.80).
Factor structure
Principal component analysis revealed five principal components with eigenvalues exceeding unity. After rotation, five readily interpretable factors were obtained (Table 2). Underactivity, flat affect, poverty of speech and anhedonia loaded heavily in the first factor. This factor reflects the core negative symptoms similar to the symptom cluster previously designated as psychomotor poverty by Liddle (Reference Liddle1987). Overactivity, insomnia, elation and pressure of speech loaded heavily in the second factor. This factor reflects psychomotor excitation. Hostility also exhibited a substantial loading in this factor. Inappropriate affect, formal thought disorder and attentional impairment loaded heavily in the third factor. These are features previously identified as components of the disorganisation syndrome (Reference LiddleLiddle, 1987). Anxiety and depression loaded heavily in the fourth factor. In the fifth factor, delusions and hallucinations had loadings greater than 0.6, whereas somatic concern exhibited a modest loading. This fifth factor is similar to the reality distortion factor identified by Liddle (Reference Liddle1987).
Table 2 Factor loadings derived by factor analysis of the 19 signs and symptoms of the Signs and Symptoms of Psychotic Illness (SSPI) scale
| Anxiety/depression | |||||
| Anxiety | -0.02 | 0.03 | 0.10 | 0.85 | 0.08 |
| Depression | 0.21 | 0.14 | -0.12 | 0.73 | 0.08 |
| Psychomotor poverty | |||||
| Underactivity | 0.81 | -0.08 | -0.01 | 0.09 | -0.01 |
| Flat affect | 0.80 | -0.06 | -0.17 | -0.07 | -0.03 |
| Poverty of speech | 0.77 | -0.12 | -0.07 | -0.15 | -0.15 |
| Anhedonia | 0.75 | 0.00 | 0.24 | 0.27 | 0.06 |
| Psychomotor excitation | |||||
| Elation | -0.26 | 0.70 | 0.07 | -0.03 | -0.20 |
| Overactivity | 0.08 | 0.84 | 0.00 | -0.11 | 0.03 |
| Pressure of speech | -0.33 | 0.61 | 0.13 | -0.05 | 0.07 |
| Insomnia | -0.02 | 0.72 | -0.33 | 0.15 | -0.12 |
| Hostility | -0.03 | 0.59 | 0.02 | 0.32 | 0.00 |
| Peculiar behaviour | 0.37 | 0.40 | 0.13 | -0.46 | 0.24 |
| Disorganisation | |||||
| Inappropriate affect | -0.07 | -0.19 | 0.86 | 0.04 | -0.15 |
| Thought form disorder | -0.23 | -0.04 | 0.67 | -0.13 | 0.08 |
| Impaired attention | 0.19 | 0.15 | 0.65 | 0.05 | 0.02 |
| Disorientation | 0.39 | 0.03 | 0.41 | 0.08 | -0.07 |
| Reality distortion | |||||
| Delusions | -0.20 | -0.06 | -0.08 | 0.18 | 0.70 |
| Hallucinations | -0.06 | -0.14 | -0.09 | -0.10 | 0.84 |
| Somatisation | 0.09 | 0.04 | 0.07 | 0.15 | 0.51 |
| % of variance explained | 18 | 16 | 12 | 11 | 9 |
The five rotated factors were almost orthogonal. The only correlations between factors that exceeded 0.2 were a negative correlation of −0.21 between the psychomotor poverty and excitation factors and a positive correlation of 0.26 between the excitation and disorganisation factors.
Figure 1 shows the profile of factor scores for the four main diagnostic groups (acute schizophrenia; persistent schizophrenia; schizoaffective disorder; mania) included in the study. It can be seen that all five clusters of symptoms occur in all four diagnostic groups, although the mean severity of psychomotor poverty in mania is very low and is accounted for mainly by mild flattening of affect, which might be due to the effects of antipsychotic medication in a few cases. Analysis of variance indicated significant differences between the four diagnostic groups in severity of psychomotor poverty (F(3,146)=5.1,P=0.002), reality distortion (F(3,146)=3.1, P=0.03) and excitation (F(3,146)=28.3, P<0.001). The group differences in disorganisation (F(3,146)=0.32, P=0.81) and anxiety/depression (F(3,146)=0.62, P=0.6) were not significant. The differences between diagnostic groups were due largely to anticipated differences between patients with schizophrenia and patients with mania. Planned comparisons revealed that patients with mania had significantly less severe psychomotor poverty but more severe excitation than patients with either acute schizophrenia or persistent schizophrenia (P<0.005 for all comparisons). Furthermore, patients with mania had significantly less severe reality distortion than patients with acute schizophrenia (P=0.008) or persistent schizophrenia (P=0.006).
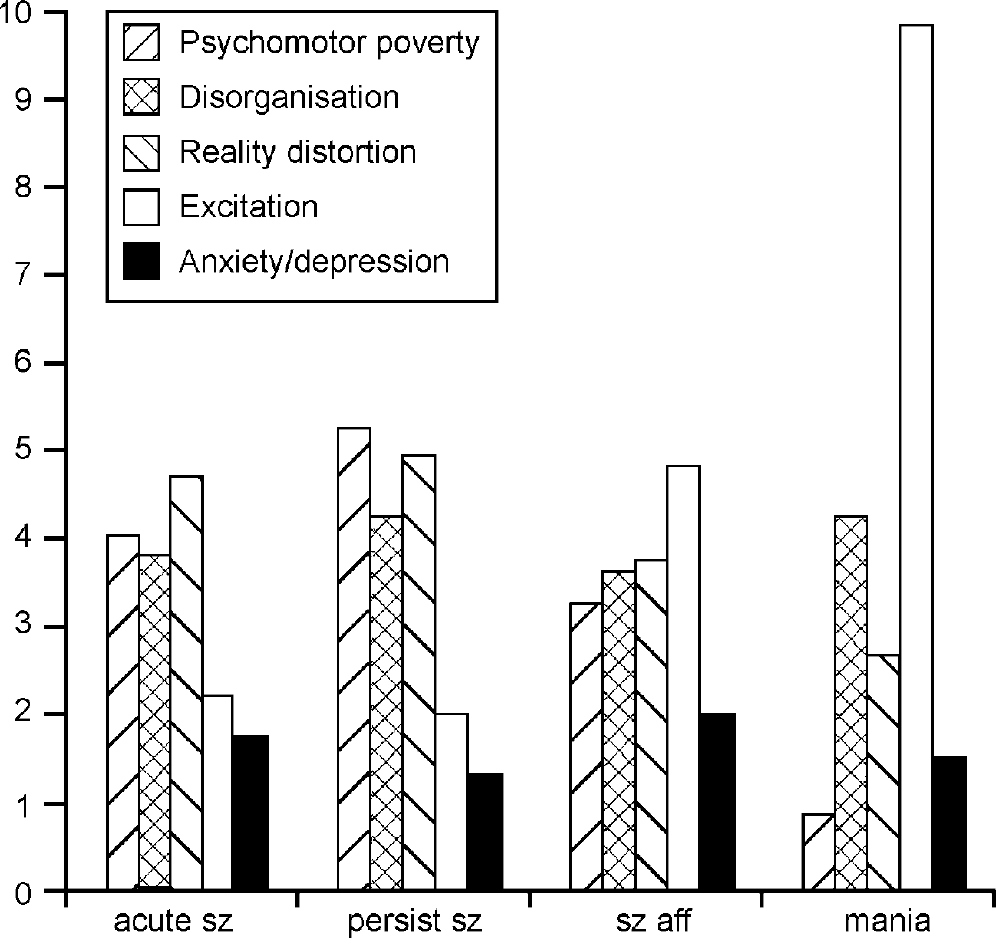
Fig. 1 Mean factor scores for each of the five factors in each of the main diagnostic groups: acute sz, acute schizophrenia; persist sz, persistent schizophrenia; sz aff, schizoaffective disorder; mania, bipolar disorder — manic phase.
Sensitivity to change
The 33 acutely ill patients participating in the longitudinal study included 22 with schizophrenia, 4 with schizoaffective disorder, 5 with bipolar disorder (manic phase) and 2 with other psychoses. Their mean age was 27.3 years (range 18-44 years) and the mean duration of illness was 4.5 years (range 0.2-23 years). There were 19 male patients. The mean duration between first and second assessments was 4.7 weeks (range 4-6 weeks). At the first assessment the mean global SSPI score was 19.5 (s.d.=8.3) and at the second assessment the mean global score was 9.2 (s.d.=5.9). The mean percentage reduction was 49.2% (s.d.=27.7). In the subset of 22 patients with CGI scores, the mean reduction in CGI score was 1.45 and the correlation between reduction in global SSPI score and CGI score was 0.67 (d.f.=21, P=0.001, two-tailed).
Of those patients with schizophrenia or schizoaffective disorder, the mean initial total SSPI score was 18.4 (s.d.=6.5), the mean reduction of SSPI score was 9.5 (s.d.=7.0) and the mean percentage change in SSPI was 48.7% (s.d.=27.4). The mean baseline CGI score was 4.3 (s.d.=0.96) and the mean reduction in CGI score was 1.55 (s.d.=1.04). Thus, assuming that the CGI provides a linear estimate of illness severity over the middle part of its range, a reduction of one point in the CGI score corresponds to a reduction of 6.1 units (or 31%) in the global SSPI score for those patients with schizophrenia or schizoaffective disorder.
The severity of all individual SSPI symptom items decreased from first to second assessment. However, for underactivity, flat affect, poverty of speech, somatisation and disorientation this reduction was not statistically significant. For anxiety, depression, anhedonia, attentional impairment, overactivity, pressure of speech, hostility, peculiar behaviour and impaired insight the reduction achieved a moderate level of significance (2.0<t<3.56; d.f.=32; P<0.05). For elation, insomnia, delusions, hallucinations, formal thought disorder and inappropriate affect the reduction was highly significant (t>3.56; d.f.=32;P<0.001).
Similarly, all factor scores decreased from the first to the second assessment (see Fig. 2). However, the decrease in psychomotor poverty exhibited only a trend towards statistical significance (t=1.96, P=0.058). The reduction in anxiety/depression was of moderate significance (t=2.6,P=0.013) but there were highly significant reductions in reality distortion (t=5.8, P<0.001), disorganisation (t=5.6, P<0.001) and excitation (t=4.2,P<0.001).
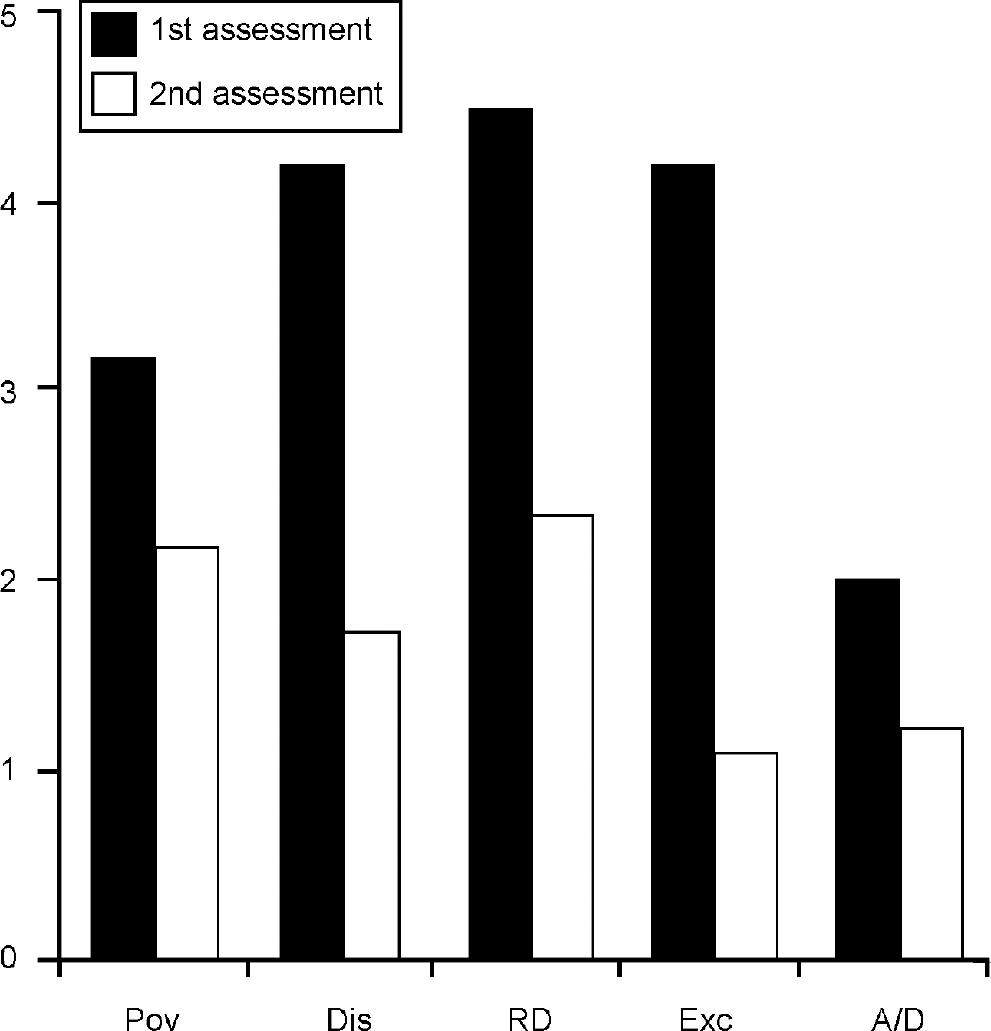
Fig. 2 The change in severity of each of the five symptom factors between the first and second assessment in the 33 acute cases in the longitudinal study: Pov, psychomotor poverty; Dis, disorganisation; RD, reality distortion; Exc, psychomotor excitation; A/D, anxiety/depression.
DISCUSSION
Acceptable interrater reliability for all individual SSPI items and excellent reliability for the total SSPI score were achieved after a relatively brief training programme based on five video-recorded cases.
Factor structure
The relationships between items, as revealed by factor analysis, reflect the clustering of symptoms predicted on the basis of recent studies (e.g. Reference van Os, Fahy and Jonesvan Os et al, 1996; Reference Wickham, Walsh and AshersonWickham et al, 2001). The factor that accounted for the most variance was that representing psychomotor poverty, reflecting the uniformly high correlations between the core negative symptoms that loaded strongly on this factor. The second factor representing psychomotor excitation accounted for a similar fraction of the variance. The third factor, disorganisation, reflected the moderately strong mutual correlations between formal thought disorder, inappropriate affect and attentional impairment. The fourth factor, anxiety/depression, reflected the moderately strong correlation between anxiety and depression (Pearson coefficient r=0.57, n=155, P<0.001). The factor accounting for the least variance was reality distortion, reflecting the fact that the correlation between the two cardinal components of this cluster — delusions and hallucinations — was of only modest strength but highly significant (Pearson coefficient r=0.35, n=155,P<0.001).
The factor structure of the SSPI is similar to the factor structure delineated by several studies of the PANSS (Reference Kay and SevyKay & Sevy, 1990; Reference Lindenmayer, Bernstein-Hyman and GrochowskiLindenmayer et al, 1995; Reference White, Harvey and OplerWhite et al, 1997). The most notable difference between the symptom factor structure of the SSPI and the PANSS is that the SSPI yields a disorganisation factor comprising inappropriate affect, formal thought disorder and attentional impairment, whereas the corresponding factor in analyses of PANSS items (labelled cognitive disorganisation) usually loads most heavily on impaired abstract thinking. However, the items loading on this PANSS factor are inconsistent between studies. One large study, of 1233 patients, did not identify a cognitive disorganisation factor at all, despite confirming the composition of the other four symptom clusters (Reference White, Harvey and OplerWhite et al, 1997). This inconsistency might be expected from the fact that several individual PANSS items embrace disorganised and impoverished mental activity within the one item. On the other hand, in the SSPI, PSE and CASH there is minimal confounding of phenomena reflecting disorganisation and impoverishment of mental activity within items. The symptoms loading on the disorganisation factor identified by analysis of SSPI items resemble those obtained from analysis of PSE items (Reference LiddleLiddle, 1987) and from analyses of CASH items (Reference LiddleLiddle, 1987; Reference Klimidis, Stuart and MinasKlimidis et al, 1993).
Although the factor composition closely reflects that predicted on the basis of recent studies, several unpredicted features are worthy of note. First, anhedonia loaded mainly on the psychomotor poverty factor and minimally on the anxiety/depression factor. The association between anhedonia and other psychomotor poverty symptoms might reflect, at least in part, the possibility that psychomotor poverty symptoms can be secondary to depression. It is probable that in a sample of patients with psychotic depression a stronger association between depression and anhedonia would be observed. Similarly, somatic concern exhibited a moderate loading on the reality distortion factor and a small loading on the anxiety/depression factor. Again, it is possible that a stronger association between anxiety/depression and somatic concern would be observed in a sample of patients with psychotic depression. However, somatic concern is moderately common in schizophrenia. A score of 2 or more was recorded in 26% of all patients with schizophrenia. Scrutiny of the video-recorded interviews indicated that the somatic concern was not considered to be of delusional intensity in any of these cases. None the less, the association between somatic concern and reality distortion suggests that the pathological process responsible for somatic concern in psychotic illnesses might share features in common with that responsible for delusions.
Sensitivity
The SSPI global score exhibited a substantial reduction from the initial to final assessment in the patients assessed longitudinally. This is likely to be due, at least in part, to the inclusion of five patients with mania and four with schizoaffective disorder in the sample. It is potentially informative to examine the relationship between change in global symptom severity assessed using the BPRS or PANSS, and change in global severity of illness measured with CGI, in published treatment trials. In a meta-analysis (Reference Tandon, Harrigan and ZornTandon et al, 1997) of treatment trials comparing the antipsychotic ziprasidone with placebo in patients with schizophrenia and schizoaffective disorder (with baseline mean CGI score of 4.8), the reduction in CGI after 4-6 weeks in the patients treated with ziprasidone was 0.54. The mean reduction in BPRS score was 13% and the mean reduction in PANSS score was 14%. Thus, for both BPRS and PANSS a reduction of approximately 25% in the global symptom score corresponds to a one-point decrease in CGI score (assuming a linear relationship in the middle of the CGI range). Because of the differences in patient samples, comparisons between studies should be interpreted with caution. None the less, the finding that in the patients with schizophrenia and schizoaffective disorder in this study a reduction of 1 unit in the CGI score corresponded to a 31% reduction in SSPI global score indicates that the sensitivity of the SSPI global score to change in illness severity is at least as high as that of the BPRS and the PANSS.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
• The global Signs and Symptoms of Psychotic Illness (SSPI) score provides a reliable and sensitive measure of severity of the symptoms of psychotic illness.
-
• Factor analysis confirms that at least five major clusters of symptoms occur in psychotic illness. These are psychomotor poverty, disorganisation, reality distortion, excitation and anxiety/depression.
-
• In acute cases, the severity of reality distortion, disorganisation, excitation and depression decreases significantly during 4-6 weeks of treatment.
LIMITATIONS
-
• On account of the bias towards recruitment of patients with severe mental illness, there were relatively few with affective psychosis, especially psychotic depression, and the reported factor structure cannot be generalised to include psychotic depression.
-
• Comparison of the sensitivity of the SSPI with other scales such as the Brief Psychiatric Rating Scale and Positive and Negative Symptom Scale must be interpreted cautiously because of differences in patient samples.
-
• The emergence of five factors does not rule out the possibility that other groupings of symptoms might usefully reflect shared aspects of the underlying pathological processes.







eLetters
No eLetters have been published for this article.