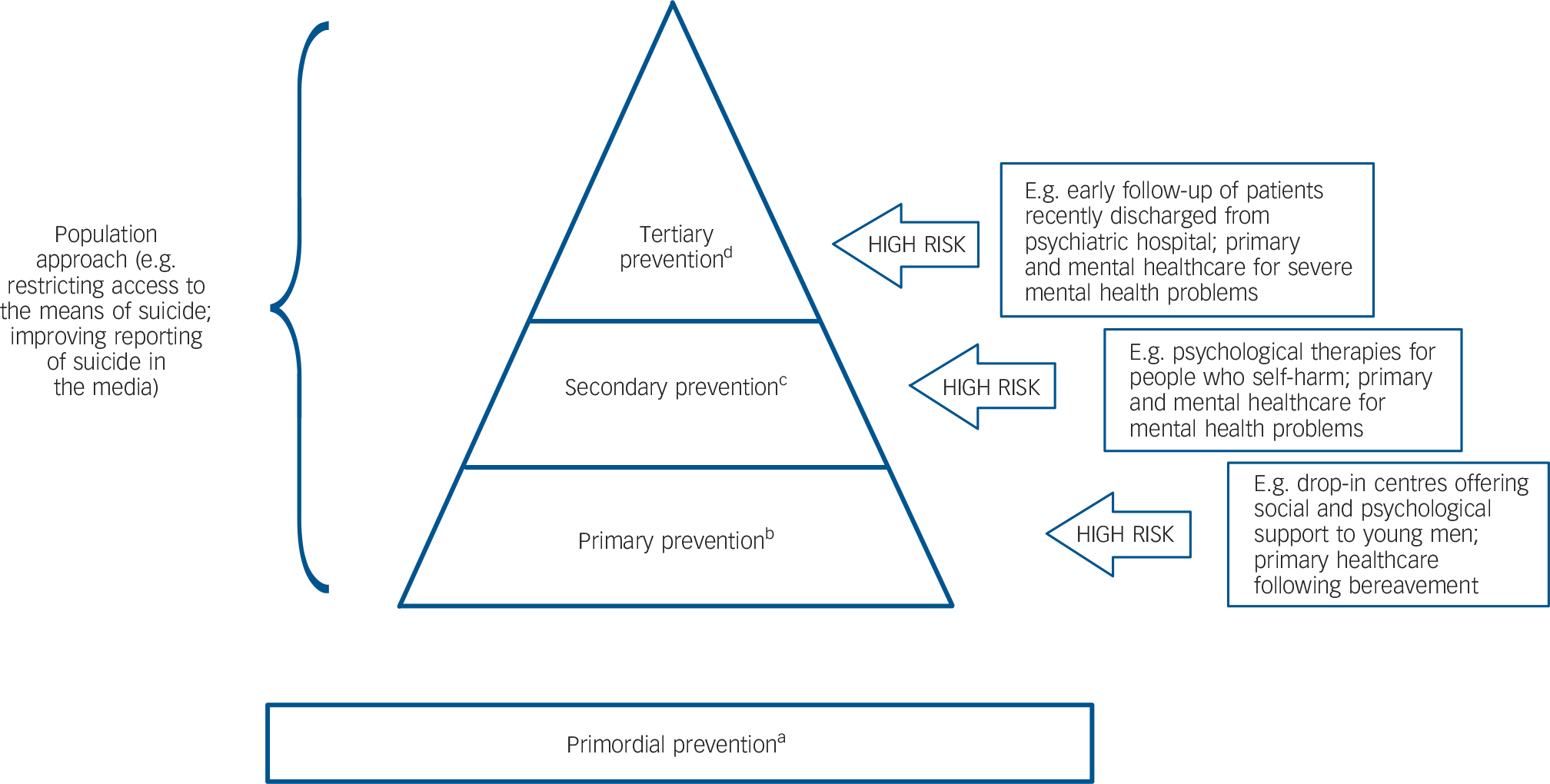
At a time when many high-income nations were beginning to promulgate suicide prevention strategies, a provocative paper demonstrated that focusing on high-risk groups would have much smaller impacts on national suicide rates than policies aiming to influence larger social or ecological forces (such as unemployment). Reference Lewis, Hawton and Jones1 Since then, despite further evidence favouring the population approach, Reference Gunnell and Frankel2–Reference Leitner, Barr and Hobby4 countries such as England, Denmark, Australia and the USA have adopted suicide prevention strategies that seek to combine broad population or universal approaches with complementary high-risk or targeted prevention interventions (Fig. 1). Many such strategies are in place despite a lack of evidence for the effectiveness of key components or for the effectiveness of all interventions acting in concert. The difficulties in evaluating such multilayered initiatives are those of evaluating any complex intervention: identification of the active component(s). Although synergies between interventions are theoretically possible, and highly desirable, these are difficult to demonstrate. Reference van der Feltz–Cornelis, Sarchiapone, Postuvan, Volker, Roskar and Grum5 Such emphasis on the high-risk approach is understandable in the context of pressures to respond to suicidal people encountered in clinical practice. This editorial considers the findings of a study by Gunnell et al (this issue), evaluating interventions to reduce suicide risk in recently discharged psychiatric patients, Reference Gunnell, Metcalfe, While, Hawton, Ho and Appleby6 and the implications of this for suicide prevention strategies.
The contribution of population and high-risk approaches
Population interventions aim to reduce population suicide rates by shifting modal behaviours and improving mental well-being across society as a whole. Reference Knox, Conwell and Caine7 This requires multi-agency, community-oriented work to address social and environmental conditions, employment opportunities, housing and family circumstances within groups held together by common links as well as geographical settings. Such broadly applied prevention efforts include diverse initiatives, for example: to reduce the availability and lethality of suicide methods; to improve detection of depression through educating primary care physicians; to stem the tide of substance misuse and dependence; and to influence media portrayals of suicide and mental illness. Targeted interventions address high-risk groups such as people with severe mental illness, people who self-harm, and specific occupational groups. Reference Lewis, Hawton and Jones1 Although targeted methods focus on relatively small groups (hundreds or thousands), universal methods aim at very large numbers (potentially measured in millions). The prevention paradox is that although suicide rates are lower in the latter group, universal approaches hold the potential to prevent a greater number of deaths. Furthermore, the majority of people who die by suicide – those from the general population – are only recognised posthumously as having been high-risk.
Successive reviews of evidence for the effectiveness of specific suicide preventive interventions have shown an even split between evaluations of high-risk and population approaches, but a clear dominance of population strategies over targeted interventions with respect to positive findings. Reference Gunnell and Frankel2–Reference Leitner, Barr and Hobby4,Reference Knox, Pflanz, Talcott, Campise, Lavigne and Bajorska8 A naturalistic study of a multilayered suicide prevention initiative in the US Air Force found reduced rates of suicide and other violence-related deaths after implementation. Reference Knox, Pflanz, Talcott, Campise, Lavigne and Bajorska8 This hybrid approach offered the potential to reduce suicide risk in a bounded, managed organisation, with the emphasis on universal approaches irrespective of risk. However, it remains uncertain whether such a programme, implemented within a strongly hierarchical organisation, can be applied to less defined communities. More recently, the high-risk approach has been bolstered by studies demonstrating its effectiveness in specific patient groups – those with clear clinical risk factors but representing relatively small numbers. Reference While, Bickley, Roscoe, Windfuhr, Rahman and Shaw9,Reference Fleischmann, Bertolote, Wasserman, Bolhari, Botega and Phillips10 Less encouraging findings have arisen when interventions targeting more loosely defined populations are evaluated. In Australia, the 1995–1997 National Youth Suicide Prevention Strategy (NYSPS) took a multilayered approach, funding interventions targeting young men (a high-risk group nationally) alongside broader health promotion initiatives. When evaluated, local NYSPS activity was found to have no impact on suicide rates in males (or females) aged 20–34 after controlling for the role of period effects (such as concurrent initiatives to address youth unemployment, and changes in labour force characteristics). Reference Page, Taylor, Gunnell, Carter, Morrell and Martin11
Gunnell and colleagues’ study Reference Gunnell, Metcalfe, While, Hawton, Ho and Appleby6 contributes to the evidence base by finding little impact of interventions to reduce the increased suicide risk in people recently discharged from psychiatric hospitals in England. These targeted interventions were introduced following the 2002 Suicide Prevention Strategy for England: pre-discharge joint case review; risk management plans covering the first 3 months; community follow-up within 7 days of discharge; and more rapid (<48 h) follow-up for patients thought to be at highest risk. The time series analysis of national data compared the periods before and after the introduction of the four interventions. Although finding some evidence for a reduction in admissions for self-harm during the 12 weeks after discharge, they found no evidence for a reduction in the risk of suicide over that period. This study raises important questions about the intended scope of suicide prevention interventions, and the role of the high-risk approach within any national suicide prevention policy.
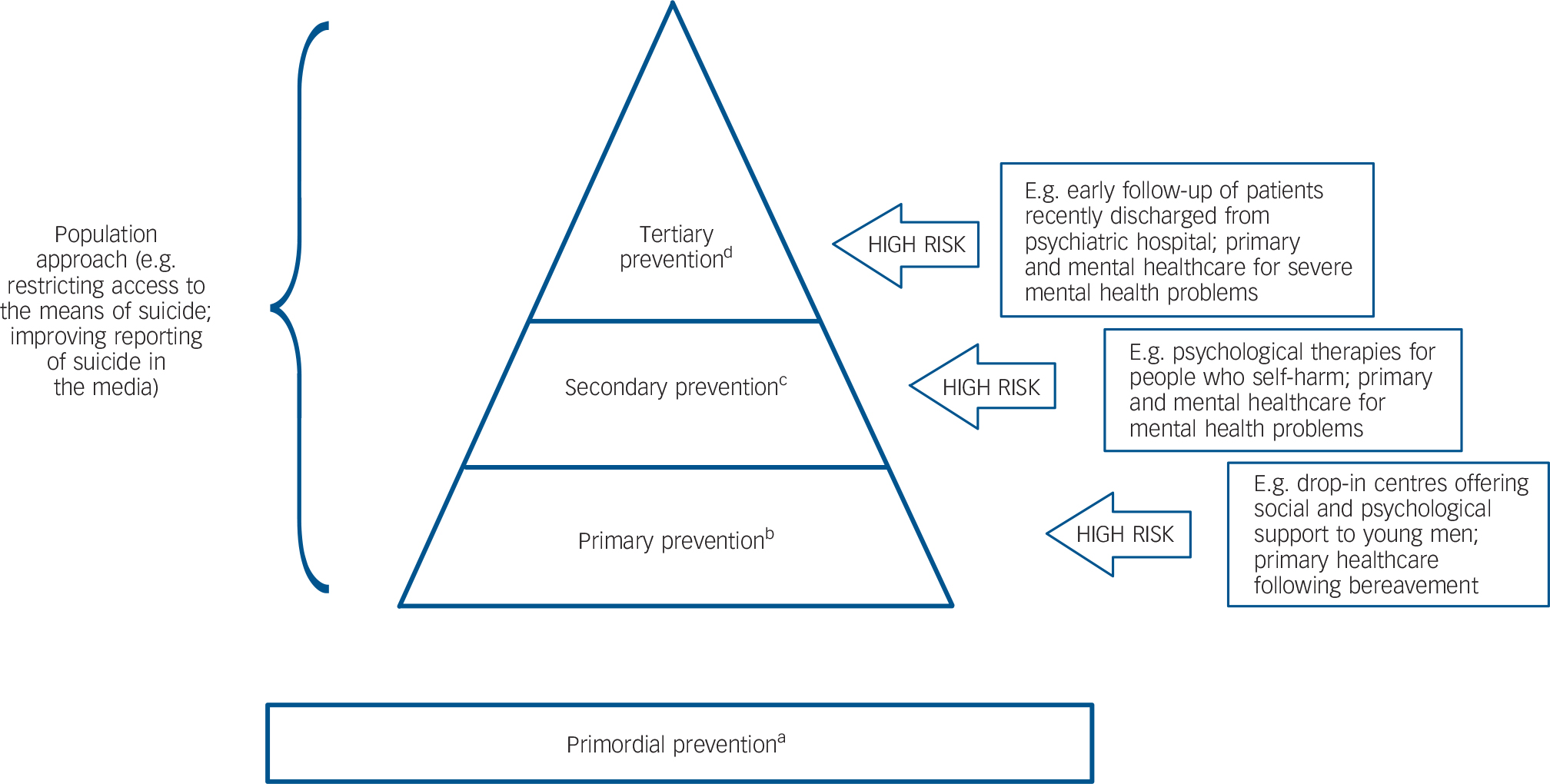
FIG. 1 The relationship of population and high-risk approaches to levels of suicide prevention.
a. Primordial prevention aims to prevent the emergence of risk factors for suicide. This level of prevention is essentially outside the remit of health services and involves establishing the socioeconomic and cultural conditions that promote mental health and well-being in a population.
b. Primary prevention includes interventions which prevent the onset of suicidal ideation. Examples include support following life events (job loss, bereavement, relationship breakdown), and the early detection of mental disorder together with its evidence-based management.
c. Secondary prevention detects early suicidal ideation or risk factors for suicide (e.g. hopelessness, substance misuse, physical illness) among those with and without mental illness.
d. Tertiary prevention involves risk minimisation for people with a history of self-harm and high levels of suicidal intent. This includes modifying continuing risk factors such as substance misuse and direct access to means.
Implications for policy makers
This evaluation of psychiatric discharge care arrangements Reference Gunnell, Metcalfe, While, Hawton, Ho and Appleby6 is published during an era of substantial cuts to NHS mental health services, and would appear to challenge the rationale for ongoing provision of care – as measured by reduced suicides. However, policy makers will need to consider alternative explanations for these findings, and also take into account the interventions’ wider benefits. The possibility of ecological fallacy arises, both in Gunnell et al's study Reference Gunnell, Metcalfe, While, Hawton, Ho and Appleby6 and in the Australian NYSPS evaluation. Reference Page, Taylor, Gunnell, Carter, Morrell and Martin11 In each setting the absence of an association with suicides at the group level may belie associations at the level of specific high-risk individuals. Although both studies accessed national-level routine data, neither was able to measure individual-level exposure to any components of the interventions investigated. Use of an alternative study design to evaluate the impact of introducing community follow-up within 7 days of psychiatric discharge in England and Wales has shown a significant reduction in suicides among recently discharged psychiatric patients. Reference While, Bickley, Roscoe, Windfuhr, Rahman and Shaw9 Again, the routine data used could only offer at best a measurement of mental health services’ implementation of recommendations as a proxy for exposure. Reference While, Bickley, Roscoe, Windfuhr, Rahman and Shaw9 All three studies Reference Gunnell, Metcalfe, While, Hawton, Ho and Appleby6,Reference While, Bickley, Roscoe, Windfuhr, Rahman and Shaw9,Reference Page, Taylor, Gunnell, Carter, Morrell and Martin11 highlight the methodological difficulties in evaluating high-risk interventions, namely measuring individual-level exposure, identifying control groups, and controlling for key potential effect modifiers and confounders, most notably concurrent population approaches. The low base rate of suicide creates the need for large numbers (approximately 45 000) Reference Gunnell and Frankel2 of high-risk individuals to be exposed to a targeted intervention if any effect is to be detected. Reference Perlis12 Although large samples (about 12 900 000) Reference Gunnell and Frankel2 are also required to investigate the impact of a means control policy, these are usually achievable using national-level routine data to measure changes in method-specific community rates of suicide and related self-harm injuries.
Beyond such methodological concerns it is also important to recognise the distinction between suicide prevention programmes and the provision of needed care. People unwell enough to have been admitted to a psychiatric hospital are likely to require post-discharge services. It may be unrealistic to expect those services to prevent suicide measurably. Nonetheless, their contribution to addressing well-being as well as mediators of suicide risk should also be recognised. This highlights the need for greater policy clarity over what should be the intended scope of any suicide prevention intervention. Although suicide prevention is highly desired, it may be more realistic to acknowledge that demonstrating such effects is beyond the scope of many studies. Showing benefits in terms of enhanced care leading to improved intermediate outcomes may be sufficient justification for spending valued resources, particularly in relation to powerful yet common risks such as depression.
Gunnell et al's study reported that post-discharge care was significantly associated with a reduction in self-harm admissions. Reference Gunnell, Metcalfe, While, Hawton, Ho and Appleby6 Many other suicide prevention interventions have demonstrated positive effects on intermediate outcomes such as suicidal behaviour, Reference Mann, Apter, Bertolote, Beautrais, Currier and Haas3,Reference Leitner, Barr and Hobby4 hopelessness, help-seeking, depressive symptoms and treatment uptake. Reference Mann, Apter, Bertolote, Beautrais, Currier and Haas3 Such studies, with their more achievable sample sizes, Reference Perlis12 strengthen the argument for assessing putative suicide prevention interventions using thoughtfully chosen surrogate outcomes (such as near-fatal suicide attempts), whether in structured trials or naturalistic studies of high-risk approaches. Large-scale research collaborations, meta-analyses and ecological analyses of aggregated data also provide an opportunity to measure the impact on suicides, acknowledging that a reduction in suicide mortality is the prized outcome.
Conclusions
We are still far from fulfilling policy makers’ wishes for a full set of true positive and true negative findings for each specific intervention proposed to prevent suicide: evaluated both singly and in combination, accounting for the mediating effect of socioeconomic forces, and accompanied in each case by cost-effectiveness analysis. Herein lies the justification for continuing to fund studies defining the impact of high-risk and universal suicide prevention interventions. Policy makers and researchers must recognise that these are radically different approaches, potentially complementary but not easily integrated without clear understanding of the great differences between seeking to improve a population's mental health (by minimising antecedent factors that ultimately contribute to becoming suicidal), and treating individuals with manifest psychiatric disorders. Without such clarity, as implied over a decade ago, Reference Lewis, Hawton and Jones1 it will be a daunting challenge to expand the evidence base for population or high-risk approaches. Addressing these uncertainties over what works, and in which combination, provides better assurances that investments in preventive efforts will reap rewards, and also that they will continue to be funded.



eLetters
No eLetters have been published for this article.