Common mental disorders are depressive and anxiety disorders which are typically encountered in community and primary care settings (Reference Goldberg and HuxleyGoldberg & Huxley, 1992). They are the leading mental health cause of disability in the global burden of disease (World Health Organization, 2001). Cross-sectional population-based studies consistently show that the poor and marginalised are at greater risk of having common mental disorders (Reference Patel and KleinmanPatel & Kleinman, 2003). Women are at greater risk, including in low- and middle-income countries; a review of the possible explanations for this found no evidence to support a hormonal or biological mechanism (Reference Piccinelli and WilkinsonPiccinelli & Wilkinson, 2000). Gender disadvantage and exposure to intimate-partner violence are key risk factors for common mental disorder in women (Reference Patel, Kirkwood and PednekarPatel et al, 2006). Surveys have also shown an association between reproductive and sexual complaints (such as the complaint of vaginal discharge) and common mental disorder (Reference Prasad, Abraham and AkilaPrasad et al, 2003; Reference Patel, Kirkwood and PednekarPatel et al, 2006). Other risk factors, reported principally from high-income countries, include chronic physical health problems (Reference Evans, Charney and LewisEvans et al, 2005), tobacco misuse and alcohol misuse (Reference Breslau, Schultz and JohnsonBreslau et al, 2005). In this paper, we describe the results of a longitudinal population-based study of women's health in Goa, India. We hypothesised that poverty, gender disadvantage, poor physical and gynaecological health and substance misuse were risk factors for the development of new episodes of common mental disorder.
METHOD
This was a population-based cohort study in the state of Goa on India's west coast, with a population of 1.4 million. The 1998–9 National Family Health Survey reported that Goa, together with some states such as Kerala, had some of the best health indicators in the country (International Institute for Population Sciences, 2001).
Sample
The study population comprised women aged 18–45 years living in nine villages of the catchment area of the Aldona Primary Health Centre (n=8595); 3000 women were randomly selected from the population registers maintained by the health department. The eligibility criteria for recruitment were age between 18 and 50 years (since the enumeration registers were up to 4 years old in some villages); residence in the area for the next 12 months; speaking one of the study languages (Konkani, English, Hindi, Marathi); and not being currently pregnant. If a randomly selected woman did not meet all these criteria, then the researcher was instructed to replace her using a priori criteria for identifying an eligible woman (Reference Patel, Kirkwood and PednekarPatel et al, 2006).
Recruitment and follow-up
Recruitment took place over a 19-month period from November 2001 to May 2003. Details of the recruitment procedure and data collection have been described in earlier publications (Reference Patel, Kirkwood and PednekarPatel et al, 2006). In brief, the mandatory requirements for participation were a face-to-face interview with a trained researcher, and the collection of vaginal or urine specimens for the diagnosis of reproductive tract infection. Participants who consented to a gynaecological examination also had their blood pressure, weight and height measured. All recruits who consented to participate and completed the recruitment procedures were reviewed at 6 and 12 months after recruitment. Thus, there were three rounds of data collection: at recruitment, and at 6 and 12 months (reviews).
Risk factors
Risk factors were assessed at recruitment. We conducted a semi-structured interview, which was a composite of items derived from existing interviews used in other studies of reproductive and mental health in Goa. The interview was evaluated in a pilot study; interrater reliability of key variables was moderate to high (kappas from 0.58 to 0.87). The data collected from these sources were organised in the following manner for the analyses of risk factors.
Socio-economic risk factors
Information on the participant's age, education, religion and marital status was collected. Economic status was measured by means of questions on type of housing, access to water and a toilet, household income, employment status, indebtedness and the experience of hunger due to lack of money to buy food in the previous 3 months.
Psychological factors
Two measures were used for psychological health. The Scale for Somatic Symptoms measures symptoms that are features of somatoform disorders. The scale elicits the experience of 20 common somatic symptoms in the previous 2 weeks (Reference Chaturvedi and SarmukaddamChaturvedi & Sarmukaddam, 1987), in four categories: pain-related symptoms such as headache and body ache; sensory symptoms such as hot or cold sensations and tingling; nonspecific symptoms such as tiredness and weakness; and symptoms of biological dysfunction such as poor sleep and constipation. Each symptom is rated on a Likert scale (0–2) of increasing severity. The scores of these four scales were summed to generate a somatoform disorder symptom score for each participant. The second measure was the Revised Clinical Interview Schedule (CIS–R), a structured interview for the measurement and diagnosis of common mental disorder in community and primary care settings (Reference Lewis, Pelosi and ArayaLewis et al, 1992). The CIS–R is the instrument for the UK national surveys of psychiatric morbidity, and has been widely used in developing countries, including India. The Konkani language version of the CIS–R administered in the present study had been previously followed in Goa (Reference Patel, Pereira and MannPatel et al, 1998). The interview consists of 14 sections, each covering specific symptoms such as anxiety, depression, irritability, fatigue, obsessions, compulsions and panic. The sum of the section scores generates a total score, a measure of non-psychotic psychiatric morbidity. Scores >11 signify case-level morbidity. In addition, interview data can be processed using the PROQSY software to generate ICD–10 diagnostic categories (World Health Organization, 1992).
Reproductive health factors
Participants were asked about pregnancies; numbers of pregnancies and their outcome were recorded, with more detailed history of pregnancy in the previous 12 months. Participants who were sexually active were asked about their experience of difficulty in conception in the previous 12 months. A menstrual history elicited the experience of irregular menstrual cycles and dysmenorrhoea in the previous 12 months. Participants were asked about their experience of five gynaecological symptoms (abnormal vaginal discharge, dysuria, lower abdominal pain, genital itching and dyspareunia) in the previous 3 months. Definitions of these symptom categories were derived from guidelines for reproductive health research (Reference Jejeebhoy, Koenig and EliasJejeebhoy et al, 2003).
Gender disadvantage factors
Questions covered five domains. The first domain was elicited as part of the socioeconomic factors, i.e. marital history; being widowed or divorced poses specific disadvantages for women in South Asia. In addition, being married or having had a pregnancy during adolescence (<20 years old) indicate restricted productive choices. The second domain covered the lifetime experience of verbal, physical and sexual violence by the spouse and concerns about the spouse's substance use habits. Violence experienced from any other person was elicited from all participants. The third domain covered the autonomy the woman had to make decisions regarding visiting her mother's or friend's home, seeing a doctor, keeping money aside for personal use, and having time to do things for herself; the responses to these four items (each scored 0–2) were combined to generate an autonomy score (range 0–8). The fourth domain enquired about the level of engagement, in the past 3 months, with four activities: religious activities, participation in a community or voluntary group, social outings to meet friends or relatives, and having friends or relatives visit her. The responses to these four items (each scored 0–4) were combined to generate a social integration score (range 0–16). The fifth domain consisted of items regarding support from family when faced with five different situations (good news, a personal problem, needing to borrow a small amount of money, feeling low and when ill). The responses to these five items (each scored 0–1) were combined to generate a family support score (range 0–5).
Physical health factors
Estimation of haemoglobin was based on a finger-prick sample of blood, using the Hemocue system (Reference Krenzischeck and TansecoKrenzischeck & Tanseco, 1996). Anaemia was evaluated as a categorical variable (absent, Hb≥11 g/dl; mild to moderate, Hb 8–10.9 g/dl; severe, Hb<8g/g/8 dl). The medical examination data collected from participants who consented to see the gynaecologist included weight, height and blood pressure. Body mass index (BMI) values were categorised (<17; 17–19; 20–24; and >25 kg/m2). Items of the WHO Disability Assessment Schedule (DAS; Reference Chwastiak and Von KorffChwastiak & Von Korff, 2003) that measure physical disabilities (standing for long periods, household responsibilities, walking a long distance, getting dressed, washing whole body, day-to-day work) were added to generate a physical disability score (range 6–17). The diagnosis of reproductive tract infection was established using gold-standard laboratory tests: polymerase chain reaction assay for chlamydial and gonococcal infections, culture for trichomonas vaginalis and Gram-stained slides for candidiasis and bacterial vaginosis (Reference Meehan, Wawer, Serwadda, Jejeebhoy, Koenig and EliasMeehan et al, 2003). The presence of other chronic health problems was based on self-report of the presence of a long-standing illness; participants were asked about the nature of the illness.
Outcome measures
The CIS–R data were processed using the PROQSY software to generate ICD–10 diagnoses. The primary outcome was the presence of an ICD–10 diagnosis equivalent to a common mental disorder, i.e. any anxiety or depressive disorder, at either of the reviews.
Analysis
Analyses of the risk factors of common mental disorders were carried out for participants who completed at least one review and who did not have a common mental disorder at recruitment. Logistic regression was used for all analyses, with incident case of common disorder as the outcome. First, univariate analyses were performed for each socio-economic risk factor; all those with P≤0.1 were included in a multivariate model. The factors with P≤0.1 in this multivariate model were retained for subsequent analyses. Next, the associations of risk factors in the other domains (gender disadvantage, mental health and reproductive and physical health) with common mental disorder were estimated. The factors with P<0.1 in univariate analyses were adjusted for the socio-economic factors identified above; those for which P remained below 0.1, together with the socio-economic factors, formed the final multivariate model. Analysis of obstetric risk factors and factors associated with spousal relationships were restricted to married participants. In the final model, which included all the women, variables with missing values had the values recoded as 9. For categorical variables with evidence of linearity, a P-value for trend is shown; otherwise the P-value shows the overall significance of the variable. Continuous variables such as age, household income, autonomy score, social integration score, family support score, physical disability, somatoform disorders score, CIS–R score, household size and income were converted to categorical variables (e.g. tertiles or quartiles) based on the distribution of scores. Reproductive tract infections were treated as a composite variable of any reproductive tract infection or any sexually transmitted infection (chlamydia, gonorrhoea, trichomoniasis). All significance tests are two-tailed.
RESULTS
Of the 3000 randomly selected women, 2494 consented to participate in the study (83.1%). Details of the recruited sample have been published elsewhere (Reference Patel, Kirkwood and PednekarPatel et al, 2006). At the first review (mean review interval 24 weeks, s.d. 1.4 weeks), 2316 participants completed the review procedure (92.9%). At the second review (mean review interval 52.2 weeks, s.d. 2.3 weeks) 2167 participants completed the review procedure (86.9%). There was no difference between participants who were reviewed and those who were lost to follow-up at either review on the following recruitment characteristics: education, household family income, CIS–R score, any reproductive tract infection or sexually transmitted infection, experiencing abnormal vaginal discharge, and self-reported chronic physical health problems. However, younger, unmarried participants were more likely to be lost to follow-up, because they had moved away from home for occupational, educational or marital reasons. Replacement participants had higher follow-up at both rounds (round 1: 94.2% v. 92.1%, P=0.05; round 2: 89.7% v. 85.2%, P=0.001). Language was also associated; migrants who were non-Konkani speakers had lower follow-up at both rounds, mainly because they had left the community. Follow-up at round 2 was lower among illiterate participants.
At least one review was completed by 2317 women, 151 of whom had a common mental disorder at recruitment; the analyses presented are thus based on the sample of 2166 women who completed at least one review and did not have a common mental disorder at recruitment. The study flow chart is shown in Fig. 1. A total of 39 participants had an incident common mental disorder; 31 were diagnosed as having mixed anxiety–depressive disorder and 8 as having depressive disorder. Thus the overall 12-month rate of new episodes of common mental disorder was 1.8% (95% CI 1.3–2.4%).
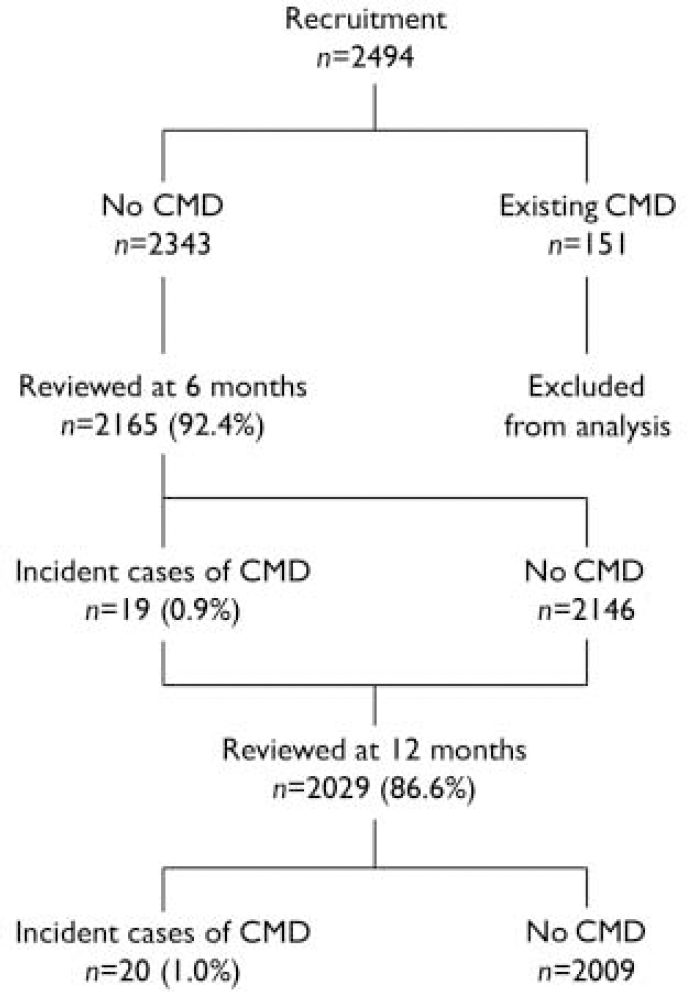
Fig. 1 Flow chart of participants in the study. CMD, common mental disorders.
Socio-economic risk factors
The baseline socio-economic factors most strongly associated with the risk for common mental disorders were related to deprivation and poverty, i.e. low level of education, low household income, lack of access to running water in the home, having experienced hunger and difficulties in making ends meet (Table 1). Compared with single women, married and divorced/widowed women were at significantly elevated risk. When these baseline factors were combined in a multivariate model, the following remained significantly associated with common mental disorders: being married (OR=6.52, 95% CI 1.6–27.3); being divorced or widowed (OR=6.04, 95% CI 0.8–44.3); higher total monthly household income (OR=0.37, 95% CI 0.1–1.1 for the highest quartile compared with the lowest); and the experience of difficulties in making ends meet (OR=2.82, 95% CI=1.4–5.6).
Table 1 Association of baseline socio-economic characteristics with common mental disorders (n=2166 unless otherwise stated)
| Baseline characteristics | Incident cases of CMD1 n (%) | Univariate OR (95% CI) | P |
|---|---|---|---|
| Personal demographic data | |||
| Age (years) | |||
| 18-24 | 4 (0.9) | 1 | |
| 25-29 | 8 (2.1) | 2.31 (0.7-7.7) | 0.17 |
| 30-34 | 6 (1.4) | 1.51 (0.4-5.4) | 0.52 |
| 34-40 | 11 (2.6) | 2.93 (0.9-9.3) | 0.07 |
| 40-50 | 10 (2.0) | 2.26 (0.7-7.2) | 0.17 |
| Participant type | |||
| Randomised selection | 23 (1.7) | 1 | |
| Replacement | 16 (1.9) | 1.09 (0.6-2.1) | 0.78 |
| Language | |||
| Konkani | 34 (1.9) | 1 | |
| Other languages | 5 (1.5) | 0.80 (0.3-2.1) | 0.65 |
| Education (years) | |||
| None | 7 (3.5) | 1 | |
| 1-9 | 21 (2.5) | 0.71 (0.3-1.7) | |
| 10-14 | 10 (1.1) | 0.32 (0.1-0.8) | |
| 15-23 | 1 (0.4) | 0.11 (0.0-0.9) | 0.0022 |
| Literate (read and write) | |||
| Yes | 31 (1.6) | 1 | |
| No | 8 (2.8) | 1.72 (0.8-3.8) | 0.17 |
| Ethnicity | |||
| Goan | 34 (1.7) | 1 | |
| Migrant | 5 (2.6) | 1.51 (0.6-3.9) | 0.40 |
| Religion | |||
| Hindu | 26 (1.6) | 1 | |
| Christian | 12 (2.6) | 1.64 (0.8-3.3) | 0.16 |
| Muslim | 1 (1.5) | 0.94 (0.1-7.0) | 0.95 |
| Occupation | |||
| Homemaker | 33 (2.3) | 1 | |
| Employed | 4 (0.9) | 0.38 (0.1-1.1) | 0.07 |
| Other | 2 (0.8) | 0.33 (0.1-1.4) | 0.13 |
| Marital status | |||
| Single | 2 (0.3) | 1 | |
| Married | 35 (2.3) | 6.67 (1.6-27.8) | 0.009 |
| Divorced/widowed/separated | 2 (3.3) | 9.84 (1.4-71.1) | 0.02 |
| Economic characteristics | |||
| Housing | |||
| Own home | 35 (1.8) | 1 | |
| Rented/other | 4 (1.9) | 1.04 (0.4-2.9) | 0.94 |
| Toilet access | |||
| In house | 12 (1.3) | 1 | |
| Outside house | 27 (2.1) | 1.60 (0.8-3.2) | 0.18 |
| Tap water in house | |||
| Yes | 11 (1.1) | 1 | |
| No | 28 (2.3) | 2.09 (1.0-4.2) | 0.04 |
| Per capita income, INR (n=2165) | |||
| <2000 | 23 (3.2) | 1 | |
| 2000-2999 | 7 (1.9) | 0.58 (0.2-1.4) | |
| 3000-4999 | 5 (0.9) | 0.28 (0.1-0.7) | |
| 5000+ | 4 (0.8) | 0.23 (0.1-0.7) | 0.0012 |
| Family in debt | |||
| No | 23 (1.6) | 1 | |
| Yes | 16 (2.2) | 1.38 (0.7-2.6) | 0.32 |
| Hunger in the past 3 months | |||
| No | 34 (1.6) | 1 | |
| Yes | 5 (5.3) | 3.37 (1.3-8.8) | 0.01 |
| Managing financially | |||
| No difficulty | 15 (0.99) | 1 | |
| Difficulty making ends meet | 24 (3.7) | 3.81 (2.0-7.3) | <0.001 |
Psychosocial risk factors
Baseline factors indicative of gender disadvantage, i.e. younger age at marriage, concern about the husband's substance misuse habits, and violence from others (typically in-laws for married women and parents for single women), were found to be strongly associated with common mental disorders in univariate analyses, but not after adjustment for socio-economic factors. Three types of marital abuse were elicited; none was associated with common mental disorders in univariate analyses; a composite variable of any marital abuse was also not associated with common mental disorders (OR=1.82, 95% CI 0.8–4.0). Baseline sub-case threshold psychological morbidity and symptoms of somatoform disorders at recruitment were associated with increased risk of common mental disorders, as were tobacco and alcohol use in the previous 3 months; these associations remained significant after adjustment for socio-economic factors (Table 2).
Table 2 Association of baseline gender disadvantage and mental health characteristics with common mental disorders (n=2166)
| Baseline characteristics | Incident cases of CMD1, n (%) | Univariate OR (95% CI) | P | Adjust OR2 | P |
|---|---|---|---|---|---|
| Age at marriage (n=1532) | |||||
| < 18 years | 6 (4.96) | 1 | 1 | ||
| 19-20 years | 9 (2.4) | 0.48 (0.2-1.4) | 0.52 (0.2-1.5) | ||
| 21-24 years | 14 (2.5) | 0.49 (0.2-1.3) | 0.67 (0.2-1.8) | ||
| 25+ years | 6 (1.2) | 0.24 (0.1-0.8) | 0.033 | 0.37 (0.1-1.2) | 0.23 |
| Husband verbal abuse (n=1533) | |||||
| No | 28 (2.1) | 1 | |||
| Yes | 7 (3.6) | 1.76 (0.8-4.1) | 0.19 | ||
| Husband physical abuse (n=1533) | |||||
| No | 32 (2.2) | 1 | |||
| Yes | 3 (2.5) | 1.11 (0.3-3.7) | 0.86 | ||
| Husband sexual abuse (n=1533) | |||||
| No | 33 (2.2) | 1 | |||
| Yes | 2 (4.9) | 2.27 (0.5-9.8) | 0.27 | ||
| Concerned about husband's habits (n=1533) | |||||
| No | 23 (1.9) | 1 | 1 | ||
| Yes | 12 (4.1) | 2.24 (1.1-4.6) | 0.03 | 1.69 (0.8-3.5) | 0.15 |
| Violence from others | |||||
| No | 34 (1.6) | 1 | 1 | ||
| Yes | 5 (4.8) | 3.04 (1.2-7.9) | 0.02 | 2.23 (0.8-5.9) | 0.11 |
| Social integration | |||||
| High | 16 (2.3) | 1 | |||
| Medium | 10 (1.4) | 0.60 (0.3-1.3) | 0.20 | ||
| Low | 13 (1.8) | 0.76 (0.4-1.6) | 0.48 | ||
| Autonomy in decision-making | |||||
| High | 10 (1.3) | 1 | |||
| Medium | 17 (1.8) | 1.37 (0.6-3.0) | 0.43 | ||
| Low | 12 (2.4) | 1.80 (0.8-4.2) | 0.17 | ||
| Support from family | |||||
| Low | 9 (2.4) | 1 | |||
| Medium | 14 (2.3) | 0.97 (0.4-2.3) | 0.94 | ||
| High | 16 (1.4) | 0.57 (0.2-1.3) | 0.19 | ||
| Somatoform symptom score | |||||
| 0-1 | 8 (1.1) | 1 | 1 | ||
| 2-3 | 2 (0.4) | 0.38 (0.1-1.8) | 0.23 | 0.32 (0.1-1.5) | 0.15 |
| 4-7 | 11 (1.7) | 1.47 (0.6-3.7) | 0.41 | 1.07 (0.4-2.7) | 0.88 |
| 8—max | 18 (5.1) | 4.62 (1.98-10.7) | <0.001 | 2.91 (1.2-6.9) | 0.01 |
| Psychological morbidity (CIS—R) scores | |||||
| 0 | 17 (1.2) | 1 | 1 | ||
| 1-2 | 3 (1.1) | 0.89 (0.2-3.0) | 0.77 (0.2-2.7) | ||
| 3-4 | 3 (1.4) | 1.12 (0.3-3.8) | 1.00 (0.3-3.5) | ||
| 5-8 | 9 (4.2) | 3.48 (1.5-7.9) | 2.74 (1.2-6.3) | ||
| 8-11 | 7 (8.6) | 7.57 (3.0-18.8) | <0.0013 | 5.37 (2.1-13.6) | <0.0013 |
| Tobacco use in last 3 months (n=2094) | |||||
| No | 31 (1.5) | 1 | 1 | ||
| Yes | 4 (9.3) | 6.68 (2.2-19.8) | 0.001 | 3.79 (1.2-11.6) | 0.02 |
| Alcohol use in last 3 months (n=2094) | |||||
| No | 33 (1.6) | 1 | 1 | ||
| Yes | 2 (5.6) | 3.61 (0.8-15.6) | 0.09 | 3.98 (0.9-18.0) | 0.07 |
Reproductive and physical health risk factors
Having had a pregnancy, younger age at first pregnancy and having had multiple pregnancies were all associated with common mental disorders in univariate analyses, but were not significant after adjustment for socio-economic factors. Gynaecological complaints (vaginal discharge, lower abdominal pain, dysuria and irregular menstrual periods) were associated with an increased risk and these associations remained evident after adjustment for socio-economic factors; 294 participants reported a long-standing illness or disability and 287 of them described the nature of this illness. The most common illnesses were cardiovascular diseases (101), diabetes (25) and spinal or back disorders (25). These, and physical disability at baseline, were significantly associated with common mental disorders after adjustments. However, none of the baseline biological markers of poor physical health (anaemia, reproductive or sexually transmitted infections, hypertension or low or high BMI) was associated with increased risk, either in univariate analyses or after adjustment (Table 3).
Table 3 Association of baseline reproductive and physical health characteristics with common mental disorders (n=2166)

| Baseline characteristics | Incident cases of CMD1, n (%) | Univariate OR (95% CI) | P | Adjusted OR2 | P |
|---|---|---|---|---|---|
| Obstetric baseline characteristics | |||||
| Ever pregnant | |||||
| No | 4 (0.6) | 1 | 1 | ||
| Yes | 35 (2.3) | 3.87 (1.4-10.9) | 0.01 | 0.91 (0.2-3.9) | 0.90 |
| Age at first pregnancy3 (n=1507) | |||||
| <20 years | 9 (4.3) | 1 | 1 | ||
| 20-29 years | 24 (2.1) | 0.47 (0.2-7.0) | 0.06 | 0.60 (0.3-1.3) | 0.21 |
| 30-39 years | 2 (1.5) | 0.34 (0.1-1.6) | 0.17 | 0.48 (0.1-2.3) | 0.36 |
| Pregnancy past year3 | |||||
| No | 32 (1.6) | 1 | |||
| Yes | 7 (3.0) | 1.86 (0.8-4.2) | 0.14 | ||
| Number of pregnancies3 (n=1507) | |||||
| 1 | 10 (1.5) | 1 | 1 | ||
| 2 | 22 (3.2) | 2.24 (1.0-4.8) | 0.04 | 1.90 (0.9-4.1) | 0.10 |
| 3+ | 3 (2.0) | 1.37 (0.4-5.0) | 0.64 | 1.14 (0.3-4.2) | 0.89 |
| Infertility in past year4 (n=1532) | |||||
| No | 31 (2.2) | 1 | |||
| Yes | 4 (3.0) | 1.39 (0.5-4.0) | 0.54 | ||
| Gynaecological symptoms | |||||
| Vaginal discharge | |||||
| No | 27 (1.4) | 1 | 1 | ||
| Yes | 12 (4.2) | 3.03 (1.5-6.0) | <0.001 | 3.49 (1.7-7.1) | 0.001 |
| Itching in genitals | |||||
| No | 31 (1.7) | 1 | |||
| Yes | 8 (2.6) | 1.60 (0.7-3.5) | 0.24 | ||
| Pain in abdomen | |||||
| No | 30 (1.6) | 1 | 1 | ||
| Yes | 9 (3.2) | 2.06 (0.96-4.4) | 0.06 | 1.92 (0.9-4.1) | 0.09 |
| Dysuria | |||||
| No | 31 (1.6) | 1 | 1 | ||
| Yes | 8 (4.2) | 2.77 (1.2-6.1) | 0.01 | 2.32 (1.0-5.2) | 0.04 |
| Dyspareunia (n=1533) | |||||
| No | 33 (2.3) | 1 | |||
| Yes | 2 (2.7) | 1.54 (0.4-6.5) | 0.56 | ||
| Irregular menses5 (n=1967) | |||||
| No | 7 (0.98) | 1 | 1 | ||
| Yes | 27 (2.1) | 2.22 (0.96-5.1) | 0.06 | 2.15 (0.9-5.0) | 0.08 |
| Menstrual cramps5 (n=1967) | |||||
| No | 12 (1.3) | 1 | |||
| Yes | 22 (2.1) | 1.59 (0.8-3.2) | 0.20 | ||
| Physical health indicators | |||||
| Haemoglobin, g/dl (n=2160) | |||||
| <8 | 1 (4.0) | 1 | |||
| 8-10.9 | 5 (1.4) | 0.33 (0.03-2.9) | 0.31 | ||
| 11+ | 33 (1.9) | 0.45 (0.1-3.5) | 0.45 | ||
| Any RTI (n=2073) | |||||
| Negative | 31 (2.1) | 1 | |||
| Positive | 6 (1.0) | 0.49 (0.2-1.2) | 0.11 | ||
| Any RTI (n=2073) | |||||
| Negative | 31 (2.1) | 1 | |||
| Positive | 6 (1.0) | 0.49 (0.2-1.2) | 0.11 | ||
| Any STI (n=2102) | |||||
| Negative | 35 (1.7) | 1 | |||
| Positive | 2 (2.3) | 1.33 (0.3-5.6) | 0.70 | ||
| Body mass index (n=1510) | |||||
| <17 | 3 (1.7) | 1 | |||
| 17-19 | 8 (2.5) | 1.47 (0.4-5.6) | 0.57 | ||
| 20-24 | 17 (2.5) | 1.49 (0.4-5.1) | 0.53 | ||
| 25+ | 5 (1.4) | 0.84 (0.2-3.6) | 0.82 | ||
| Systolic blood pressure (n=1556) | |||||
| ≤100 | 8 (3) | 1 | |||
| 101-120 | 19 (1.9) | 0.61 (0.3-1.4) | 0.25 | ||
| 121/140 | 5 (2.3) | 0.75 (0.2-2.3) | 0.62 | ||
| 141+ | 1 (1.7) | 0.55 (0.1-4.5) | 0.58 | ||
| Diastolic blood pressure (n=1556) | |||||
| <70 | 2 (2.4) | 1 | |||
| 70-79 | 20 (2.2) | 0.91 (0.2-3.9) | 0.89 | ||
| 80-89 | 10 (2.2) | 0.94 (0.2-4.4) | 0.94 | ||
| 90+ | 1 (1) | 0.40 (0.0-4.5) | 0.46 | ||
| Chronic physical illness (n=2157) | |||||
| No | 27 (1.4) | 1 | 1 | ||
| Yes | 10 (4.2) | 3.10 (1.5-6.5) | 0.003 | 2.96 (1.4-6.3) | 0.005 |
| Physical disability scores | |||||
| Low | 23 (1.2) | 1 | 1 | ||
| Moderate | 9 (3.8) | 3.08 (1.4-6.7) | 2.59 (1.2-5.7) | ||
| High | 7 (7.5) | 6.41 (2.7-15.3) | <0.0016 | 4.37 (1.8-10.7) | <0.0016 |
Final model
In the final multivariate model (Table 4), the following baseline factors were significantly associated with the onset of common mental disorders: abnormal vaginal discharge, low household income, having difficulty making ends meet, being married, divorced or widowed, smoking cigarettes or chewing tobacco in the previous 3 months, suffering from a chronic illness and sub-threshold psychological morbidity.
Table 4 Final multivariate model of association of socio-economic, reproductive and physical health risk factors with common mental disorders in women (n=2166)
| Baseline factor | Odds ratio | P |
|---|---|---|
| Abnormal vaginal discharge | 3.00 (1.4-6.4) | 0.004 |
| Chronic physical illness | 2.30 (1.0-5.1) | 0.04 |
| CIS—R score | ||
| 0 | 1 | |
| 1-2 | 0.51 (0.1-1.9) | |
| 3-4 | 0.71 (0.2-2.5) | |
| 5-8 | 1.81 (0.7-4.3) | |
| 8-11 | 3.10 (1.1-8.5) | 0.031 |
| Tobacco use in past 3 months | 3.23 (1.0-10.8) | 0.05 |
| Marital status | ||
| Single | 1 | |
| Married | 6.02 (1.4-25.6) | 0.01 |
| Widowed/separated/divorced | 6.23 (0.8-47.8) | 0.08 |
| Difficulties making ends meet | 2.39 (1.2-4.9) | 0.02 |
| Household per capita income, INR | ||
| < 2000 | 1 | |
| 2000-2999 | 0.58 (0.2-1.4) | |
| 3000-4999 | 0.36 (0.1-1.0) | |
| 5000+ | 0.41 (0.1-1.3) | 0.041 |
DISCUSSION
We report findings of the first (to the best of our knowledge) population-based cohort study of risk factors for common mental disorders from a low-income country. Our study reports specifically on risk factors for common mental disorders in women aged between 18 and 50 years, the demographic group at the highest risk. Our main findings were that economic difficulties, being married or divorced or widowed, gynaecological morbidity (particularly experiencing abnormal vaginal discharge) and self-reported chronic illness were independent risk factors; however, none of the objective measures of physical health, notably those reflecting nutritional status and reproductive and sexually transmitted infections, were associated with common mental disorders. Substance misuse, in particular current tobacco use, and subthreshold psychological morbidity at baseline, were also associated with increased risk. We propose a conceptual framework (Fig. 2) to explain the pathways from risk factors to common mental disorders in women. In this framework, distal socioeconomic factors are independent risk factors and also exert some of their effect through more proximal factors, notably poor reproductive health, substance misuse and chronic illnesses.

Fig. 2 Conceptual framework for pathways from risk factors to common mental disorders.
Social disadvantage and common mental disorders
All previous findings concerning risk factors for common mental disorders in low- and middle-income countries have been based on cross-sectional surveys, from which it is difficult to interpret causal relationships. Our design of a cohort study in which we excluded participants with a common mental disorder at baseline from the risk factor analysis demonstrates that economic deprivation is an independent risk factor for common mental disorders in women in our population. The likely mechanisms through which this association is mediated are diverse (Reference Patel and KleinmanPatel & Kleinman, 2003); for example, poorer women are more likely to suffer from adverse life-events, to live in crowded or stressful conditions, to have fewer occupational opportunities and to have chronic illnesses; all of these are recognised risk factors for common mental disorders. The fact that there is association between poverty and common mental disorders in countries which are extremely diverse in their economic strength suggests that relative poverty is arguably a key factor.
In view of the strong associations reported in cross-sectional surveys between domestic violence and common mental disorders (Reference Kumar, Jeyaseelan and SureshKumar et al, 2005; Reference Patel, Kirkwood and PednekarPatel et al, 2006), we were surprised that this was not an independent risk factor after adjustment for poverty and marital status in our longitudinal analysis. Several reasons may explain this; the rates of exposure to domestic violence were lower in our sample than those reported for women in India (Reference JejeebhoyJejeebhoy, 1998); and the association between domestic violence and poor mental health in surveys may be partly explained by recall bias, reverse causality or confounding by socio-economic deprivation. However, we did find a strong, and independent, association between being widowed, divorced or married and an increased risk for common mental disorder. We think that the most likely explanation for the association with being widowed or divorced is related to social isolation and stigma; and we suggest that the increased risk in married women is at least partly due to their having to cope with multiple roles and leading potentially more restricted lives in their marital homes.
Gynaecological morbidity and common mental disorders
Recent cross-sectional surveys have shown that psychological factors, including common mental disorders, are major risk factors (Reference Prasad, Abraham and AkilaPrasad et al, 2003; Reference Patel, Pednekar and WeissPatel et al, 2005) for abnormal vaginal discharge, one of the most common health complaints in women in South Asia. Gynaecological complaints are often culturally determined somatic idioms of distress for women facing severe social disadvantage and psychological distress (Reference Patel and OommanPatel & Oomman, 1999). Ethnographic studies in South Asia have reported that women typically attribute their gynaecological symptoms to tension in their lives and to symptoms of tiredness and weakness, which in turn are often associated with heavy physical work and social disadvantage (Reference Bang, Bang, Gittelsohn, Bentley and PeltonBang & Bang, 1994). Our study suggests that one mechanism for the association reported in cross-sectional analyses is that such symptoms, which may have a variety of aetiologies, lie along the pathway between long-term social and interpersonal difficulties and common mental disorder. The lack of association between biological indicators of reproductive health and common mental disorders suggests that the social contexts of gynaecological symptoms, including their possible impact on marital relationships, are the most plausible proximal mechanisms of association.
Other risk factors
Our study replicated the association of three well-defined risk factors for common mental disorder: sub-threshold psychological morbidity, tobacco use and chronic illness. A recent review confirms the high levels of comorbidity of physical and mental health problems and that this association is bidirectional (Reference Evans, Charney and LewisEvans et al, 2005). Several mechanisms may explain this association, including common biological pathways for some chronic diseases and common mental disorder, the adverse effects of treatments for chronic diseases and the impact of pain and disability associated with chronic diseases on mental health. The latter is the most likely pathway; the association between physical disability and common mental disorders was markedly attenuated after adjustment for chronic physical illness. Substance use, of both alcohol and tobacco, was associated with common mental disorder, and the association with tobacco use (smoked or chewed) remained significant after adjustment for socio-economic and other risk factors. This finding replicates similar reports from longitudinal studies in developed countries which have reported these associations (Reference Wagena, van Amelsvoort and KantWagena et al, 2005). Several mechanisms might be considered to explain this association, but the fact that the association has been reported for the first time in a non-Western setting where tobacco use among women is relatively rare (1.7%) and where most tobacco is chewed, points to the role of biological factors related to neuropharmacological effects of nicotine on neurotransmitter systems linked to depression (Reference Breslau, Peterson and SchultzBreslau et al, 1998). Other plausible mechanisms can also be considered, for example confounding by unmeasured life difficulties which predict both tobacco use and common mental disorder. Unsurprisingly, in our study current psychological symptoms were associated with the risk of common mental disorders, which may be partly an artefact resulting from the dichotomisation into case and non-case categories of scores measuring the symptoms of depression and anxiety, which are typically continuously distributed in populations.
Limitations and implications
We did not measure biological indicators for chronic illnesses. However, we were able to measure indicators for locally relevant exposures reflecting nutrition and reproductive health. The overall participation rate in the study was high and the attrition rate was relatively low, enhancing our confidence in the generalisability of the findings. However, there might have been a selection bias at recruitment such that women with physical health problems were more likely to participate. In using a categorical approach based on a diagnostic algorithm to define our outcome, we will have missed an unknown number of women with clinically significant symptoms of common mental disorder which did not meet ICD–10 case criteria, i.e. sub-threshold morbidity which may be associated with adverse impact and help-seeking (Reference Demyttenaere, Bruffaerts and Posada-VillaDemyttenaere et al, 2004).
The implications of our findings are that public health and clinical interventions aimed at reducing the burden of common mental disorders in women must target those who are poor and facing acute economic problems. It is plausible that community development activities which enhance women's education and attenuate the impact of poverty will promote mental health. Advocacy is needed by global and national health-policy makers to highlight the greater vulnerability of the poor to common mental disorder and strengthen the capacity of health services to address these disorders. Screening may help identify women with common mental disorders, particularly in clinical settings such as gynaecological or medical clinics, where women with gynaecological symptoms and chronic illnesses seek help. However, such screening programmes must be twinned with effective management strategies for common mental disorders. Reproductive and primary healthcare must incorporate a strong emphasis on the assessment of the mental health and social circumstances of women with gynaecological symptoms or chronic illnesses. The threshold for interventions for common mental disorders may need revision; women with sub-threshold symptoms, at the very least, need closer follow-up to improve early detection and management. Women who are using tobacco are also a high-risk group; interventions for early detection and treatment of common mental disorders should target women tobacco users. Further research is needed to identify the mechanisms through which some of the associations we have found are mediated; for example, what is the mechanism for the association between tobacco use and common mental disorders? Similarly, longitudinal studies examining the access and barriers to effective and affordable care for common mental disorders among poorer communities in low- and middle-income countries are needed; coping strategies which promote recovery and resilience may help identify mechanisms which promote mental health even in the context of economic adversity.
Acknowledgements
We are grateful to the Directorate of Health Services, Government of Goa, India, to the research team of the Stree Arogya Shodh Project which implemented this study in India and to the women who so willingly participated in this research.
This study was funded by a Wellcome Trust Career Development Fellowship in Clinical Tropical Medicine, to V.P.









eLetters
No eLetters have been published for this article.