People with learning disability have greater health needs for physical and psychological conditions (Welsh Health Planning forum, 1992; Reference Beange, McEldoff and BakerBeange et al, 1995). Knowledge of excess morbidity is not reflected in an understanding of how this population accesses secondary care. This is particularly relevant with the shift towards deinstitutionalisation of learning disability services and the increasing emphasis on primary care as the gateway to health care (Reference KerrKerr, 1998). These trends have affected professional roles, with the disability psychiatrist passing the institutional health care function to primary care. While the institution closure programme reflected sociological and political imperatives, the impact on care provision has not been evaluated. In this paper we describe a learning disability population in terms of epidemiology and secondary care uptake for physical and psychological health. We will consider social and environmental factors which may influence secondary care and examine the impact of a learning disability hospital as a provider of psychiatric and medical services.
METHOD
Study population
The study population consisted of the resident population in the area that until April 1996 constituted South Glamorgan Health Authority, a health district with a population of 434 000 (1996 estimate). In April 1996, South Glamorgan Health Authority was incorporated into Bro Taf Health Authority.
Data sources and record linkage
Data were available for all in-patient admissions (1991-97), out-patient appointments (1991-96), attendances at accident and emergency departments (A&E) (1993-96) and mortality (1993-97) for the resident population of South Glamorgan. In addition, a learning disability register compiled by the local social services department and a long-stay learning disability hospital database were used to identify patients with learning disability.
These data underwent a process of record linkage in order to identify those records relating to the same individual patient and to identify those individuals with a diagnosis of learning disability. The principle and process of record linkage have been discussed previously (Reference Gill, Goldacre and SimmonsGill et al, 1993) and have been used in various studies (Reference Morgan, Currie and PetersMorgan et al, 1997; Reference Currie, Morgan and PetersCurrie et al, 1998). Briefly, partial identifiers (name, gender, date of birth, postcode and address) were combined and matched by using probabilistic algorithms. The discriminating power of each item was calculated and weighted for whether the identifier was common or comparatively rare. A composite matching score was then calculated.
Data for in-patient admissions were derived from the contract minimum data set required for all UK health authorities. Admissions are recorded as finished consultant episodes (FCEs), defined as an inpatient spell under the care of one hospital consultant. An FCE finishes with either a hospital discharge or a discharge to the care of another consultant. It is therefore possible for a single admission to generate multiple FCEs.
Identification of patients
Patients with learning disability were identified by: (a) inclusion on the social services district register; (b) an in-patient admission within the learning disability speciality or with a diagnostic code of mental handicap (ICD-9 317-319 or ICD-10 F70-79; World Health Organization, 1978, 1986); (c) an out-patient appointment in the learning disability speciality; (d) inclusion on a long-stay learning disability hospital data set.
Analysis
For calculations of period prevalence and relative risk, the age- and gender-stratified 1996 population estimate for South Glamorgan was used as a denominator. The numerator was the total number of patients identified with learning disability excluding those known to have died before 1 January 1997. No adjustment was made for migration to or from South Glamorgan. All hospital activity was calculated for the 1996 prevalent populations.
Patients with learning disability were classified into three groups. Those present on the long-stay learning disability hospital data set in 1996 were defined as the institutional population. Those who had been resident in the learning disability hospital (that is, admitted before 1991 with a length of stay in excess of 365 days) but discharged before 1996 were defined as the ex-institutional population, and those recorded as never resident in the learning disability hospital were defined as the community population.
Townsend index of social deprivation
By identifying each individual with learning disability, we were able to estimate the prevalence of learning disability in each district ward on the basis of 1996 population estimates derived from the 1991 census. These prevalence figures were standardised by age and correlated to the Townsend index of material deprivation using the Pearson correlation coefficient. The Townsend index has four key variables: proportion of population of working age unemployed; proportion of households without a car; proportion of households overcrowded (defined as households with more occupants than rooms); and proportion of households not owner-occupied. A Townsend score of zero reflects the average for the UK. A positive Townsend score indicates material deprivation, with higher scores representing higher degrees of deprivation. A negative Townsend score represents comparative affluence.
RESULTS
Prevalence
In 1996, the estimated resident population of South Glamorgan was 434 000. We identified 1595 patients with learning disability, a prevalence per 1000 of 4.1 for males and 3.2 for females. The prevalence for the City of Cardiff was 4.0 per 1000, while it was 2.7 for the semi-rural Vale of Glamorgan. Figure 1 shows the prevalence of learning disability plotted against age for both genders. There was a wide variation in prevalence with age, with peaks of 7.0 and 5.4 for males and females respectively in the age group 35-44 years. We identified 134 subjects (8.4%) as resident in long-term institutional care. Of the 1461 community patients, 76 (5.2%) were identified as ex-institutional patients discharged into the community after 1 April 1991.
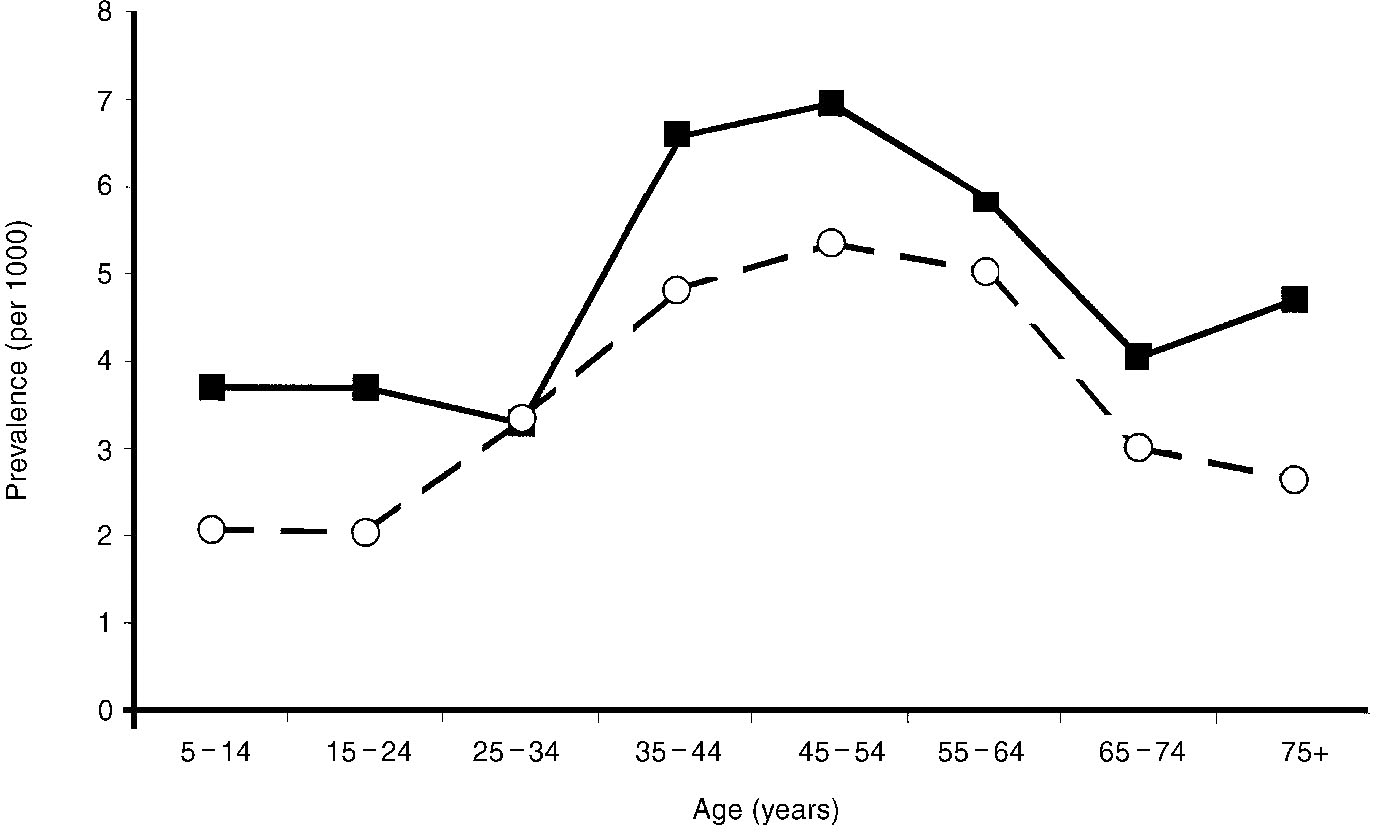
Fig. 1 Estimated period prevalence of learning disability by age and gender. -▪-, male; -○-, female.
Social deprivation
Figure 2 shows the relationship between social deprivation and prevalence of learning disability by district ward, after excluding those cases in long-term institutional care. There was a strong correlation between deprivation and prevalence (r=0.77, P <0.001). The correlations for three age bands were r=0.43 (0-24 years), r=0.80 (25-64 years) and r=0.38 (65 and over).
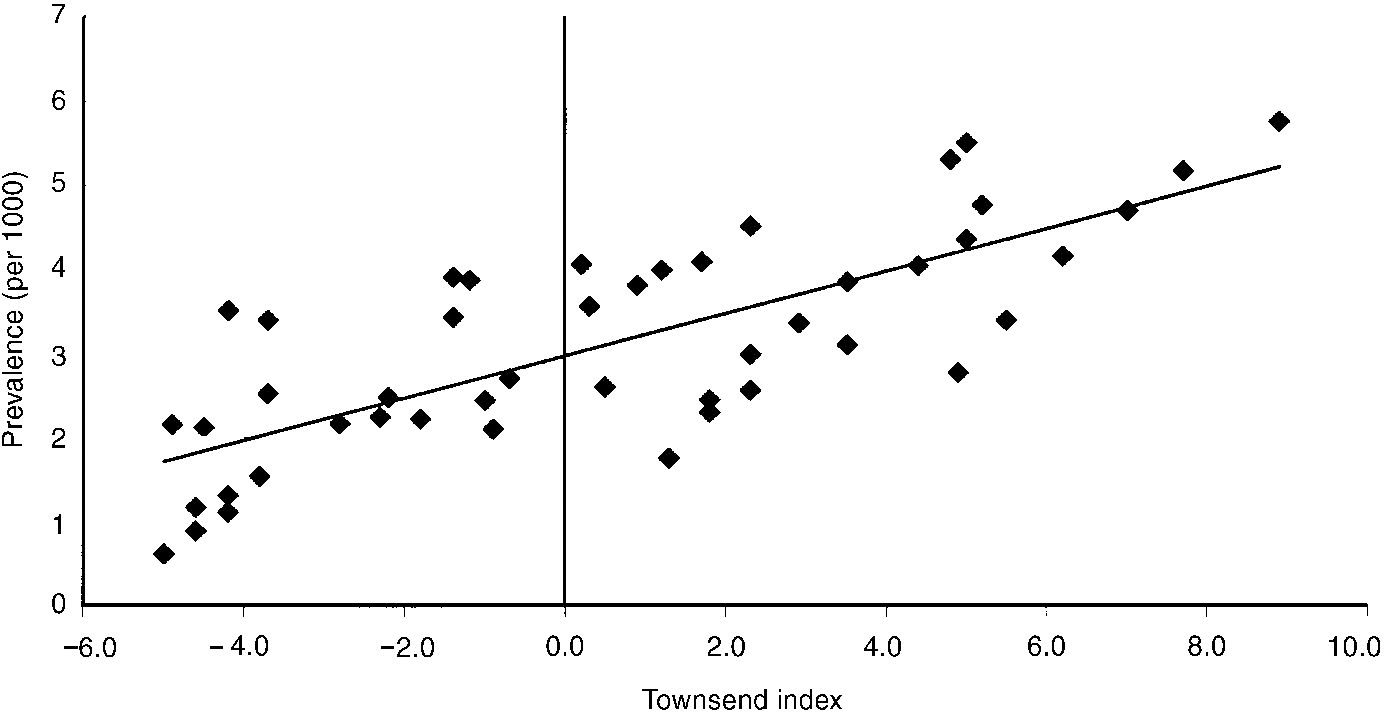
Fig. 2 Age-standardised prevalence of the learning disability by deprivation of district ward.
Acute in-patient activity
Between 1991 and 1997, there were 560 408 FCEs in the acute specialities. Of these, 2422 (0.43%) involved patients with learning disability. These patients consumed 0.43% of total bed-days. Mean length of stay for learning disability patients was 4.37 days, compared with 4.94 for the non-learning-disability population. The standardised admission ratios for patients with learning disability were 4.63 (95% CI 3.79-5.47) for dentistry specialities, 1.83 (95% CI 1.74-1.92) for the medical specialities and 0.64 (95% CI 0.59-0.69) for the surgical specialities. Admission rates for patients with and without learning disability are shown in Fig. 3. Table 1 shows a breakdown of admission rates and length of stay for the major medical and surgical specialities.
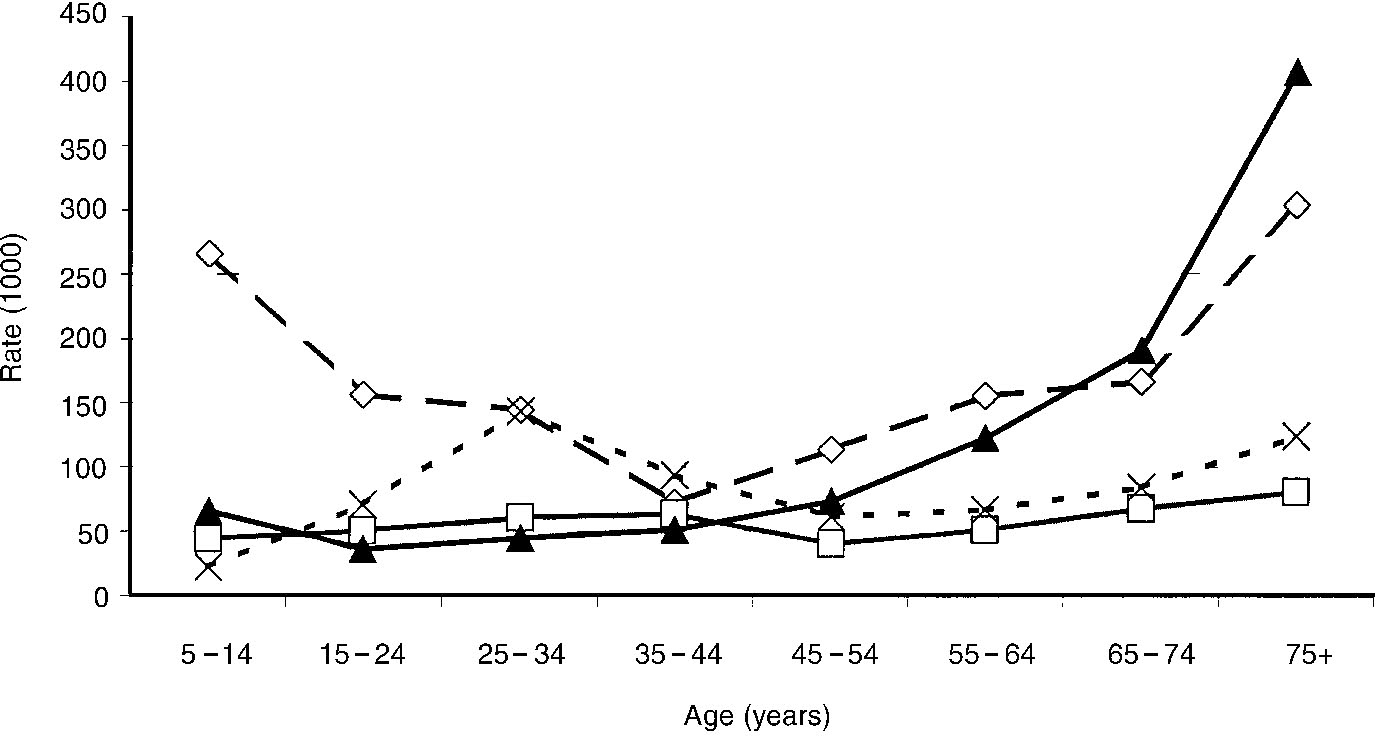
Fig. 3 Admission rate per annum for patients with and without learning disability for medical and surgical specialities. -⋄-, learning disability medicine; -□-, learning disability surgery; -▴-, non-learning disability medicine; -X-, non-learning disability surgery.
Table 1 Admissions and length of stay (LOS) for the main specialities for patients with and without learning disability

| Speciality | Learning disability patients | Non-learning-disability patients | ||
|---|---|---|---|---|
| Admissions | Mean LOS (days) | Admissions | Mean LOS (days) | |
| General surgery | 263 | 3.62 | 67 097 | 4.42 |
| Urology | 55 | 3.27 | 20 943 | 3.15 |
| Trauma and orthopaedic | 183 | 7.21 | 37 659 | 7.13 |
| Ear, nose and throat | 93 | 1.49 | 19 713 | 1.97 |
| Ophthalmology | 59 | 1.83 | 14 838 | 1.52 |
| Oral surgery | 118 | 1.49 | 7532 | 1.23 |
| Restorative dentistry | 10 | 0.00 | 87 | 0.36 |
| Paediatric dentistry | 138 | 0.02 | 8334 | 0.00 |
| Orthodontics | 0 | - | 70 | 0.00 |
| Neurosurgery | 17 | 10.59 | 2668 | 11.34 |
| Plastic surgery | 23 | 4.17 | 4127 | 5.74 |
| Cardiothoracic surgery | 8 | 26.00 | 1986 | 11.29 |
| Paediatric surgery | 50 | 2.32 | 7052 | 1.72 |
| Accident and emergency | 1 | 1.00 | 152 | 0.91 |
| Anaesthetics | 14 | 0.71 | 2848 | 0.10 |
| General medicine | 633 | 4.22 | 85 442 | 5.14 |
| Gastroenterology | 0 | - | 11 | 2.45 |
| Haematology | 186 | 1.54 | 20 912 | 1.07 |
| Clinical pharmacology | 0 | - | 4 | 12.25 |
| Rehabilitation | 6 | 33.33 | 1010 | 30.29 |
| Palliative medicine | 0 | - | 63 | 9.89 |
| Cardiology | 10 | 4.40 | 9325 | 3.67 |
| Dermatology | 32 | 9.22 | 10 996 | 2.42 |
| Thoracic medicine | 95 | 5.87 | 19 612 | 5.30 |
| Neurology | 16 | 29.13 | 2248 | 13.39 |
| Rheumatology | 0 | - | 1717 | 6.95 |
| Paediatrics | 385 | 3.99 | 39 531 | 2.80 |
| Paediatric neurology | 75 | 3.87 | 587 | 3.70 |
| Geriatric medicine | 81 | 18.06 | 31 077 | 25.82 |
| Obstetrics | 40 | 1.90 | 56 916 | 2.54 |
| Gynaecology | 49 | 1.88 | 52 837 | 1.66 |
| Obstetrics (antenatal) | 0 | - | 32 | 2.72 |
| GP maternity | 0 | - | 4878 | 2.01 |
| GP (other) | 14 | 11.14 | 3619 | 12.16 |
| Radiotherapy | 24 | 3.42 | 16 936 | 2.40 |
| Others/uncoded | 0 | - | 4871 | - |
| Total | 2678 | 557 730 | ||
Patients with learning disability registered in a long-term care institution and those always resident in the community had almost identical non-psychiatric admissions rates (239 and 240 per 1000 respectively). Those patients discharged from long-term institutional care had a higher admission rate (360 per 1000). The standardised admission ratio for those within institutional care compared with those in community care was 0.97 (95% CI 0.63-1.31). For emergency admissions this ratio was significantly reduced to 0.59 (95% CI 0.27-0.91).
The mean length of stay for institutional patients (2.1 days) was considerably lower than that of those in community care (5.3 days) and that of ex-institutional patients in community care (3.3 days). For emergency admissions, the respective figures were 2.9, 6.2 and 8.3 days.
Overall, total numbers of non-psychiatric hospital days per 1000 patients per annum were 492 for those in institutional care, 1270 for those in residential care and 1200 for the ex-institutional patients.
Psychiatric illness and activity
Of those patients we identified with learning disability, 263 (16.5%) were identified as having had a contact within secondary care (in- or out-patient) involving a primary or secondary diagnosis of psychiatric illness. Psychiatric comorbidity was more prevalent among the ex-institutional group (42.1%) than among those in institutional care (11.3%) or community care (15.6%).
Table 2 shows the admission rate per 1000 population for a primary ICD-10 diagnosis of psychiatric illness. Patients with learning disability accounted for 246 (1.37%) of all psychiatric in-patient admissions and 341 (0.8%) of all out-patient appointments.
Table 2 Prevalence and admission rates for psychiatric disorders for patients with learning disability
| ICD-10 code | ICD-10 chapter subheading | Patients (n) | Prevalence per 1000 | Average admission rate per annum per 1000 population |
|---|---|---|---|---|
| F00-F09 | Organic including symptomatic mental disorders | 15 | 9.4 | 2.0 |
| F10-F19 | Mental and behavioural disorders due to psychoactive substance use | 14 | 8.8 | 1.4 |
| F20-F29 | Schizophrenia, schizotypal and delusional disorders | 50 | 31.3 | 7.5 |
| F30-F39 | Mood (affective disorders) | 38 | 23.8 | 2.6 |
| F40-F49 | Neurotic, stress-related and somatoform disorders | 56 | 35.1 | 3.2 |
| F50-F59 | Behavioural syndromes associated with physiological disturbances and physical factors | 2 | 1.3 | 0.2 |
| F60-F69 | Disorders of adult personality and behaviour | 32 | 20.1 | 1.7 |
| F80-F89 | Disorders of psychological development | 46 | 28.8 | 1.5 |
| F90-F98 | Behavioural and emotional disorders with onset usually occurring in childhood and adolescence | 17 | 10.7 | 1.1 |
Mental handicap services
There were a total of 490 FCEs in the learning disability speciality with an admission dated after 31 March 1991. Of these, 198 involved patients resident in the long-stay institution. These admissions therefore represent either initial admissions or readmissions from an acute care provider. Patients who had previously been discharged from the long-stay learning disability institution generated 113 admissions, an annual admission rate of 212 per 1000 patients. This compares with an admission rate of 18 per 1000 for those community patients never resident in the institution. Mean lengths of stay for these two groups were 285 days and 114 days respectively.
DISCUSSION
Methodology
By using record-linkage techniques, we identified a population with learning disability in one health district. Such methods can be used for a wide range of disease groups, but their success depends on the likelihood of relevant patients coming into contact with the services from which the data are collected and on the accuracy and thoroughness of coding. By using a wide range of sources from both health and social services, we believe that we identified the large majority of the learning disability population. Our estimate of the prevalence of learning disability is higher than that previously reported for the City of Cardiff (Reference Humphreys, Lowe and BlundenHumphreys et al, 1981). This is due in part to the use of a wider range of health service data than in the previous study. Our figures are comparable with those recorded across a wide range of Western European and North American populations (Reference McClaren and BrysonMcClaren & Bryson, 1987). Our methods may have underestimated the prevalence of learning disability in the younger age groups. This is because one of our data sources (the learning disability data set) was for adults only, while another (the social services data set) was skewed towards adult patients. Our study may also have been less sensitive to mild or border-line learning disability defined by IQ.
Relationship with social deprivation
We report a positive correlation between prevalence of learning disability and social deprivation. This correlation may be explained largely by a concentration of social care homes within less affluent areas. However, the relationship is also apparent (although weaker) in the younger age groups where patients will be resident within the family home. This may indicate the presence of aetiogical factors associated with social deprivation that predict learning disability, although there must be doubt over the direction of causality. Caring for a patient with learning disability may involve financial hardships and consequent social drift. These areas demand further exploration.
Utilisation of non-psychiatric health services
Overall, patients with learning disability are not excessive users of non-psychiatric in-patient care in terms of number of admissions or length of stay, although there is considerable variation by speciality. Learning disability patients tend to use more medical beds than other patients but have less uptake within the surgical specialities. The first fact may reflect a greater prevalence of certain conditions such as epilepsy in the learning disability population, while the reduction in surgical care may be partly explained by reduced uptake of obstetric and gynaecological care (see Table 1). The lower mean length of stay, as compared with the general population, appears to be counter-intuitive in a population with high morbidity.
Patients in institutional care are likely to endure greater morbidity than those cared for in the community (Reference CorbettCorbett, 1979; Reference McGrother, Hauck and BhaumikMcGrother et al, 1996; Reference McDermott, Platt and KrishnaswamiMcDermott et al, 1997), yet this is not reflected in acute hospital usage. Overall admissions are similar, although length of stay for the hospital residents is significantly shorter. It seems likely that a degree of acute medical care is provided within these institutions, reducing the length of stay in other hospitals. Our data therefore provide evidence for a ‘hidden service’ provided by long-stay learning disability institutions that may be lost with the shift towards community-based care — a finding which appears to be contradicted by the experience of the ex-institutional patients, who also have fewer emergency admissions. However, this population is frequently readmitted, for considerable periods, into the long-stay learning disability hospital, which again may offer acute care.
Psychiatric comorbidity
The data on psychiatric comorbidity ‘dual diagnosis’ are interesting: 16.5% of the learning disability population have contacts coded for psychiatric diagnosis. While our figures are not synonymous with prevalence across the full range of diagnosis for severe psychiatric illness, which one would expect to lead to admission within a seven-year period, they represent a proxy for prevalence. In fact, our estimate of the prevalence of schizophrenia of 30.1 per 1000 compares with other published figures in the learning disability population (Reference Doody, Johnstone and SandersonDoody et al, 1998).
Psychiatric care contact is also influenced by this ‘institutional’ factor. This factor is striking in connection with admission to learning disability psychiatry, with high rates for the recently discharged institutional patients. Patients with a learning disability will continue to need acute psychiatric service following the closure of the institution.
The health care uptake of people with a learning disability is different from that of the general population. The spread of speciality contact appears to reflect the needs of this group. The presence of a learning disability institution had a significant influence on health provision; it remains to be seen whether other services will absorb this function after closure.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Social setting and deprivation are associated with varying health uptake for patients with learning disability.
-
▪ Institutional patients have a lower demand for non-psychiatric health services. The closure of institutions may create a vacuum of health care.
-
▪ Patients with learning disability have an increased uptake of medical and dental services but a reduced uptake of surgical specialities.
LIMITATIONS
-
▪ Our sample may have been skewed towards the older age groups.
-
▪ Routine data sources may be prone to inaccurate coding.
-
▪ No information concerning severity of learning disability was available.








eLetters
No eLetters have been published for this article.