Intimate partner violence (IPV) is associated with significant morbidity and mortality, especially among women, and its prevention is a global public health priority. 1 IPV includes emotional abuse, threatening behaviour and physical or sexual violence between current and former partners. 1 To date, research on IPV has predominantly focused on experiences of physical violence. Reference Feder, Ramsay, Dunne, Rose, Arsene and Norman2 In high-income settings, around 20% of women and 10% of men report lifetime IPV, with 5% and 3%, respectively, reporting past-year IPV. 3,Reference Smith, Osborne, Lau and Britton4 It is well established that IPV leads to mental health problems, including depression, post-traumatic stress disorder (PTSD) and suicide attempts. Reference Devries, Mak, Bacchus, Child, Falder and Petzold5–Reference Afifi, MacMillan, Cox, Asmundson, Stein and Sareen7 There is emerging evidence that this relationship is bidirectional – and that people (particularly women) with pre-existing mental disorders are at increased risk of subsequent IPV. Reference Devries, Mak, Bacchus, Child, Falder and Petzold5,Reference Trevillion, Oram, Feder and Howard8,Reference Oram, Trevillion, Feder and Howard9 However, little is known about their risk of different forms of IPV (especially emotional and sexual abuse), related health effects and help-seeking behaviour, or about the risk among men with mental disorders. Addressing this evidence gap is essential in guiding effective interventions in this vulnerable population.
Therefore, this study aims to examine the risk of recent IPV and related health burden and help-seeking behaviour among men and women with chronic (pre-existing) mental health problems in a nationally representative sample. We hypothesised that compared to people without chronic mental illness (CMI), people with CMI would be more likely to have experienced each type of IPV (emotional, physical and sexual IPV), and that victims with CMI would be (a) more likely to experience health problems and (b) less likely to seek help than victims without CMI.
Method
Data sources and study design
We used data from the 2010/2011 British Crime Survey (BCS). Reference Fitzpatrick and Grant10,Reference Chaplin, Flatley and Smith11 The BCS is an annual, nationally representative cross-sectional survey of crime victimisation in England and Wales. It is conducted by a private research company (BMRB), historically on behalf of the Home Office, and since 2012 on behalf of the Office for National Statistics. It comprises face-to-face interviews with all participants, and a self-completion module on domestic violence for participants aged 16–59 years only.
Sampling, interview procedures and participants
The 2010/11 BCS recruited a random nationally representative sample of people aged 16 years or older living in private residential households in England and Wales. The sampling strategy was complex, and included stratification (in order to achieve a socio-demographically representative sample for each police force area) and clustering (for further details please see Home Office Technical Reports Reference Fitzpatrick and Grant10 ). The widely used Postal Address File (the most complete record of private residential households) was used as the sampling frame. One adult was selected at random from each household, with no replacement in the case of non-participation.
Trained lay interviewers visited each selected household. Written informed consent was obtained from the selected adult after the study had been described. Each participant had a face-to-face computer-assisted interview conducted in a private setting in their home. This ‘main interview’ collected information on socio-demographics, past-year personal and household crime victimisation, and experiences of the criminal justice system. At the end of this interview, participants aged 16–59 years were additionally invited to consent to self-completion modules, which addressed domestic violence (including partner and family violence), sexual victimisation, stalking, drug-taking and drinking. These experiences were asked about in a self-completion questionnaire since they tend to be under-reported in face-to-face interviews. Reference Walby and Allen12 The participants were informed of the content and sensitive nature of the self-completion questionnaires, and re-assured of confidentiality. Participants could opt out of the self-completion modules if they were unwilling or unable to take part. Consenting participants were given a laptop and asked to read the questionnaires and enter the answers themselves, after which their answers were concealed. If they requested help from the interviewer with answering the self-completion module, questions on domestic and sexual violence were omitted.
In our study, we included all 2010/2011 BCS participants aged 16–59 years who completed the domestic violence module. We excluded those who had never had a partner, and those with missing data on partner violence (since partner violence was our primary outcome measure).
Measurements
The main exposure was CMI. This was defined as ‘any long-standing mental health condition, such as depression’, which has lasted for 12 months or more and which limits day-to-day activities; as reported by participants in the face-to-face interview. No further details about the nature of CMI were available in this survey. Analysis of a separate national survey (the 2007 Adult Psychiatric Morbidity Survey), which used a similar CMI measure to that used in the BCS, found that 3.3% (n = 213) had self-reported CMI, of whom 81% (n = 173) had common mental disorders (depression or anxiety disorders) and 7.5% (n = 16) had probable psychosis or a diagnosis of psychosis; 75% had visited a GP and 20% had received mental health care from secondary mental health care services in the preceding year (further details available from author on request).
The main outcomes were: any past-year IPV-defined as any emotional, physical or sexual abuse by a current or former partner in the past 12 months; and the separate forms of IPV: emotional, physical and sexual. These were assessed by asking a series of questions on specific abusive behaviour, as detailed below.
IPV definition
-
1 Emotional abuse: partner did any of the following
-
• Prevented them from having fair share of money
-
• Stopped them from seeing friends or relatives
-
• Repeatedly belittled them so they felt worthless
-
• Threatened to hurt them or someone close to them
-
-
2 Physical abuse: partner did any of the following
-
• Pushed them, held them down or slapped them
-
• Kicked, bit or hit them, or threw something at them
-
• Choked or tried to strangle them
-
• Threatened them with a weapon or threatened to kill them
-
• Used some other kind of force against them
-
-
3 Sexual abuse: partner did any of the following in a way that caused fear, alarm or distress
-
• Indecently exposed themselves to them
-
• Touched them sexually when they did not want it (e.g. groping, touching of breasts or bottom, unwanted kissing)
-
• Sexually threatened them (e.g. demanded sex when they did not want it or followed or cornered them in a sexually threatening way)
-
• Forced them to have sexual intercourse, or to take part in some other sexual act, when they made it clear that they did not agree or when they were not capable of consent
-
Since the definition of CMI for this study required a duration of more than 1 year, and the outcome of interest was IPV in the preceding year, the mental illness would by definition precede IPV (unless there was any measurement error).
Secondary outcomes were (a) health problems within the past 12 months ‘as a result of the abuse’, defined as: (i) physical illness or injury as a result of IPV (cuts/bruises/scratches/black eye/broken bones/internal injury/other physical injury/contracting a disease/becoming pregnant); (ii) mental/emotional problems as a result of IPV (difficulty sleeping/nightmares/depression/low self-esteem/attempted suicide); and (iii) attempted suicide as a result of IPV. (b) Help-seeking defined as telling one of the following three sources of help about IPV (i) informal network (family/relatives/friends/neighbours/work colleagues); (ii) health professionals (doctor/nurse/health visitor/counsellor/therapist); and (iii) other formal organisation (police/legal professional/government agency/helpline/specialist support service/voluntary organisation).
We estimated the prevalence and odds of each of the above outcomes among those with and without pre-existing CMI. We selected the following covariates as potential a priori confounders for any association between CMI and IPV, and between CMI and IPV-related health problems/help-seeking: gender, age, ethnicity (White/Black and minority ethnic), marital status (married/separated, divorced or widowed/ single), employment (employed, economically inactive, unemployed) and tenancy (homeowner, rents from private landlord, rents from local council). Reference Walby and Allen12–Reference Khalifeh, Hargreaves, Howard and Birdthistle14 We additionally adjusted help-seeking for presence of adverse health outcomes as a result of IPV. It is worth noting that some of these covariates (e.g. marital status, employment, tenancy) may be conceptualised as either confounders or mediators. We conducted our multivariate analysis in two steps, first adjusting for age and gender, and then adjusting for the additional covariates of ethnicity, marital status, employment and tenancy, such that the relative contribution of these two sets of covariates to the strength of the association between CMI and IPV could be examined.
Data analysis
We used the statistical software STATA version 12.0 SE (Stata Corporation, East College Station, TX, USA) for all analyses. We took the complex survey design into account (including clustering, stratification and population weights) using the STATA ‘svy’ suite commands. We estimated the population-weighted prevalence of IPV in those with and without CMI, and the prevalence standardised by age and gender (with the whole study sample as the reference population). Hypothesis tests were based on adjusted Pearson's tests (for bivariate analyses) or adjusted Wald tests (for multivariate logistic regression analyses). We tested for interactions between CMI and gender in relation to association with IPV. We stratified analyses for IPV prevalence and odds by gender.
Results
Response rate
The response rate for the 2010/11 BCS was 76% (n = 46 754 participants aged 16 years or more). Of those eligible for the questionnaire (n = 29 821 participants aged 16–59 years), 23 602 (79.1%) completed the module, 2297 (7.7%) refused and 3922 (13.2%) were unable to complete it without interviewer help (so they were not asked the domestic violence questions to maintain their safety).
Of the 23 602 participants who completed the domestic violence module, we included 23 222 in our study sample after excluding 374 (1.6%) who never had a partner and six (0.03%) who had no data on partner violence. Completion of the domestic violence module was less likely amongst those with CMI (68% v. 80%), and among those who were older, from ethnic minorities or unemployed (Fig. 1).
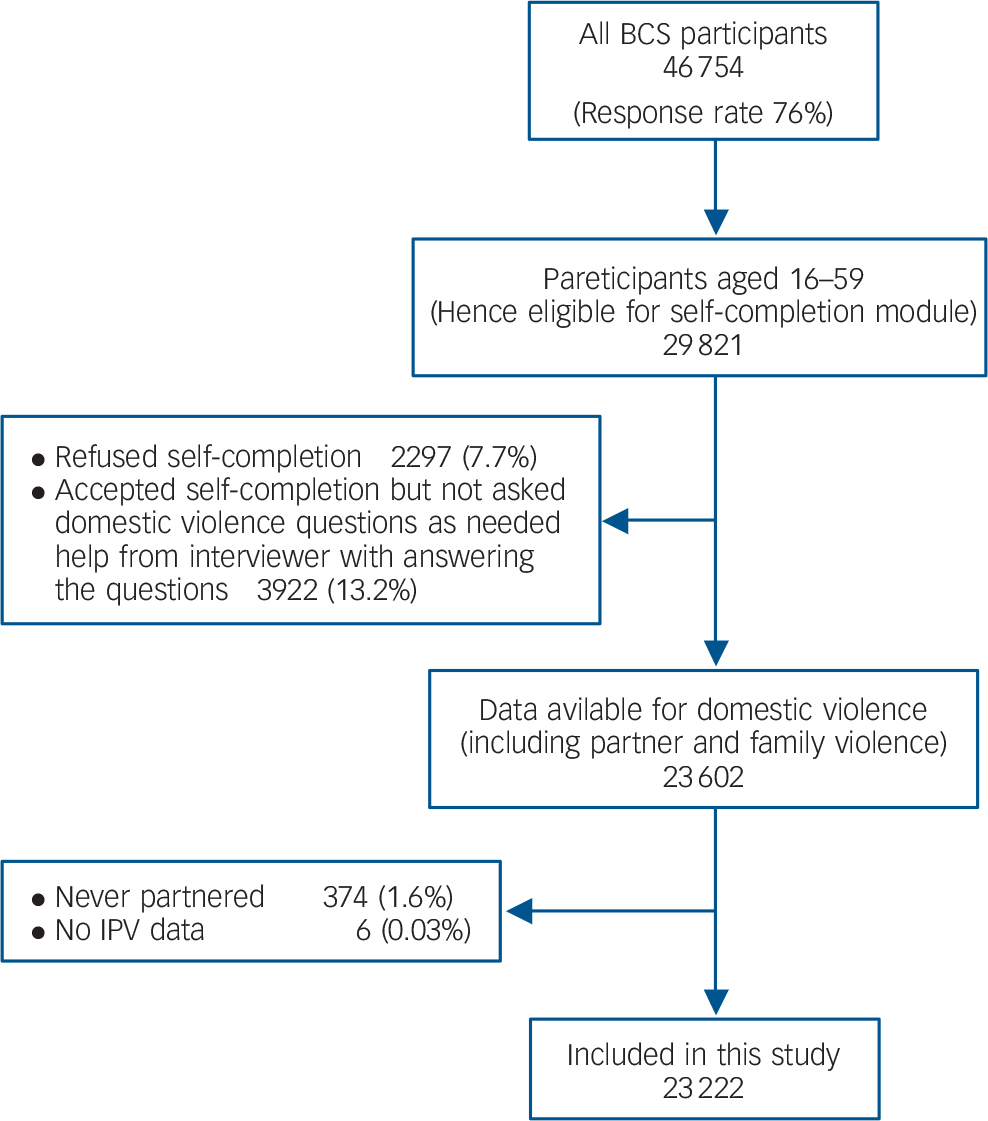
Figure 1 Sample flow
Prevalence of CMI and sample characteristics
The population-weighted prevalence of CMI was 2.4% (CI = 2.2%–2.7%; n/N = 692/23 222) with a prevalence of 2.7% (n/N = 442/12 731) and 2.1% (270/10 491) among women and men, respectively. Those with mental illness were more likely to be female, older, White, single, unemployed and to live in rented accommodation (see Table 1).
TABLE 1 Sample characteristics for those with and without mental illness
| Characteristic a | Chronic mental illness n = 692, % (n) |
No chronic mental illness n = 12 309, % (n) |
|---|---|---|
| Male | 39.0 (270) | 45.4 (10 221) |
| Female | 61.0 (422) | 54.6 (12 309) |
| White | 94.1 (650) | 91.3 (20 574) |
| Black and minority ethnic | 5.9 (41) | 8.7 (1950) |
| Missing | (1) | (6) |
| Married | 35.7 (247) | 58.6 (13 204) |
| Single | 39.6 (274) | 28.8 (6491) |
| Separated/divorced/widowed | 24.7 (171) | 12.6 (2828) |
| Employed | 27.2 (188) | 79.9 (17 957) |
| Economically inactive | 64.6 (447) | 15.7 (3523) |
| Unemployed | 8.2 (57) | 4.4 (991) |
| Missing | (0) | (41) |
| Owns house | 32.6 (225) | 64.7 (14 553) |
| Rents house from private landlord | 26.5 (183) | 21.7 (4881) |
| Rents house from Local Council | 41.0 (283) | 13.6 (3053) |
| Missing | (1) | (43) |
| Age: mean (s.d.) | 40.6 (10.4) | 39 (11.8) |
a. All characteristics differed between groups at the 1% significance level.
Prevalence and odds of past-year IPV
Among women, the population-weighted prevalence of past-year IPV was 20.0% (89/442) v. 5.3% (789/12 309) among those with and without CMI, respectively, and the age/gender standardised prevalence was 21.4% v. 5.6%, respectively (Table 2). Among men, the IPV population-weighted prevalence was 6.9% (21/271) v. 3.1% (356/10 221) among those with and without CMI, respectively, and the age/gender standardised prevalence was 10.1% v. 3.3%, respectively.
TABLE 2 Population-weighted and standardised prevalence of past-year IPV among those with and without chronic mental illness, by gender
| Men and women | Women | Men | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population-weighted prevalence (n) |
Standardised prevalence (95% CI) a |
Population-weighted prevalence (n) |
Standardised prevalence (95% CI) b |
Population-weighted prevalence (n) |
Standardised prevalence (95% CI) b |
|||||||
| CMI (n = 692) |
No CMI (n = 22 530) |
CMI | No CMI | CMI (n = 442) |
No CMI (n = 12 309) |
CMI | No CMI | CMI (n = 271) |
No CMI (n = 10 221) |
CMI | No CMI | |
| Any IPV | 14.6 (110) |
4.3 (1145) |
15.7 (11.4–20.1) |
4.5 (4.1–4.8) |
20.0 (89) |
5.3 (789) |
21.4 (16.1–26.7) |
5.6 (5.1–6.1) |
6.9 (21) |
3.1 (356) |
10.1 (3.4–16.7) |
3.3 (2.9–3.8) |
| Emotional IPV | 11.1 (90) |
3.3 (897) |
12.6 (8.6–16.6) |
3.4 (3.1–3.7) |
15.2 (73) |
4.4 (653) |
16.6 (12.2–21.1) |
4.7 (4.2–5.2) |
5.3 (17) |
2.0 (244) |
8.6 (2.2–15.0) |
2.2 (1.8–2.5) |
| Physical IPV | 6.1 (45) |
1.8 (486) |
7.1 (4.0–10.1) |
1.8 (1.6–2.1) |
8.1 (35) |
2.2 (344) |
9.9 (5.6–14.2) |
2.5 (2.1–2.8) |
3.2 (10) |
1.2 (142) |
4.3 (0.0–8.6) |
1.2 (0.0–1.5) |
| Sexual IPV c | – | – | – | – | 3.0 (13) |
0.4 (68) |
2.8 (1.3–4.4) |
0.49 (0.34–0.64) |
– | – | – | – |
a. Standardised for age and gender.
b. Standardised for age.
c. Sexual IPV is reported for women only as the absolute numbers in men with mental illness were too low (<5) for stable estimates.
The adjusted OR for any IPV among people with CMI was 2.9 (CI = 2.1–3.8), with a trend for higher relative odds among women (OR = 3.3, CI = 2.4–4.7) than men (OR = 2.0, CI = 1.1–3.7) (interaction term for mental illnes×female gender = 1.8, CI = 0.97–3.5, P = 0.06; Table 3). Among women with CMI, the adjusted relative odds for emotional, physical and sexual IPV were 2.8 (CI = 1.9–4.0), 2.6 (CI = 1.6–4.3) and 5.4 (CI = 2.4–11.9), respectively. Among men with CMI, the adjusted relative odds for emotional and physical IPV were 2.0 (1.0–4.4) and 3.0 (1.2–7.5), respectively. The absolute number of men with CMI reporting sexual IPV was too small for stable estimates.
TABLE 3 Odds ratios for past-year IPV among people with and without chronic mental illness, by gender
|
n among those with CMI |
n among those without CMI |
Age and gender-adjusted OR(95% CI) |
P-value | Fully adjusted OR
a
(95% CI) |
P-value | |
|---|---|---|---|---|---|---|
| Men and women | n = 692 | n = 22 530 | ||||
| Any IPV | 110 | 1145 | 4.0 (3.0–5.2) | <0.001 | 2.9 (2.1–3.8) | <0.001 |
| Emotional IPV | 90 | 897 | 3.7 (2.8–5.0) | <0.001 | 2.5 (1.8–3.6) | <0.001 |
| Physical IPV | 45 | 486 | 3.7 (1.6–2.6) | <0.001 | 2.6 (1.7–4.0) | <0.001 |
| Sexual IPV b | – | – | – | – | ||
| Women | n = 442 | n = 12 309 | ||||
| Any IPV | 89 | 789 | 4.7 (3.4–6.4) | <0.001 | 3.3 (2.4–4.7) | <0.001 |
| Emotional IPV | 73 | 653 | 4.0 (2.9–5.6) | <0.001 | 2.8 (1.9–4.0) | <0.001 |
| Physical IPV | 35 | 344 | 4.0 (2.4–6.7) | <0.001 | 2.6 (1.6–4.3) | <0.001 |
| Sexual IPV | 13 | 68 | 8.0 (4.1–15.6) | <0.001 | 5.4 (2.4–11.9) | <0.001 |
| Men | n = 270 | n = 10 221 | ||||
| Any IPV | 21 | 356 | 2.61 (1.5–4.6) | <0.01 | 2.0 (1.1–3.7) | 0.03 |
| Emotional IPV | 17 | 244 | 2.9 (1.5–5.5) | <0.01 | 2.0 (1.0–4.4) | 0.04 |
| Physical IPV | 10 | 142 | 3.0 (1.4–6.4) | <0.01 | 3.0 (1.2–7.5) | 0.02 |
| Sexual IPV b | – | – | – | – | ||
a. Final model included age, gender, ethnicity, marital status, housing tenure, employment status.
b. Sexual IPV is reported for women only, as the absolute numbers in men with MI is too small (<5) for stable estimates.
Health problems among IPV victims
Comparing health problems for victims with and without pre-existing CMI, the former were more likely to experience emotional/mental problems within the past year as a result of IPV (53% v. 30%; OR adjusted for socio-demographics = 2.2, CI = 1.3–3.8), with particularly high relative odds for attempted suicide as a result of IPV (13% v. 2%, aOR = 5.4, CI = 2.3–12.9; Table 4). The two groups were equally likely to experience physical injuries/illness following IPV (24%, P = 0.97).
TABLE 4 Prevalence and odds of health problems as a result of IPV among victims with and without chronic mental illness
| Problems as a result of IPV | Victims with CMI n = 109 % (n) |
Victims without CMI n = 1142 % (n) |
OR adjusted for age and gender (95% CI) |
Fully adjusted OR (95% CI) a |
P for fully adjusted OR |
|---|---|---|---|---|---|
| Any health problems | 57.9 (64) | 41.3 (493) | 1.9 (1.1–3.1) | 1.8 (1.1–3.0) | 0.02 |
| Physical injury/illness | 23.9 (23) | 23.7 (283) | 1.0 (0.5–2.0) | 0.9 (0.5–1.8) | 0.75 |
| Mental/emotional problems | 53.2 (60) | 30.5 (359) | 2.4 (1.5–4.0) | 2.2 (1.3–3.8) | <0.01 |
| Suicide attempts | 12.8 (14) | 2.2 (25) | 4.9 (2.1–11.1) | 5.4 (2.3–12.9) | <0.001 |
a. Adjusted for age, gender, ethnicity, marital status, employment, tenancy.
Help-seeking among IPV victims
Victims with and without CMI were equally likely to seek help from any source; 52% v. 51% among all victims (P = 0.91) and 69% v. 78% among victims who experienced health problems as a result of the abuse (P = 0.06; Table 5). However, victims with CMI were less likely to seek help from informal networks (OR adjusted for socio-demographics and health problems = 0.47, CI = 0.27–0.83) and more likely to seek help from health professionals (aOR = 2.7, CI = 1.3–5.1) than victims without CMI. Most victims sought help from more than one source, but 12% of victims with CMI (v. 1.5% of those without) sought help exclusively from health professionals (aOR = 6.9, CI = 2.6–18.3).
TABLE 5 Prevalence and odds of disclosure of IPV by victims with and without chronic mental illness
| Disclosed IPV to: | IPV victims with or without health problems as a result of IPV |
IPV victims with health problems as a result of IPV |
OR adjusted for age and gender (95% CI) |
Fully adjusted OR (95% CI) a |
P for fully adjusted OR |
||
|---|---|---|---|---|---|---|---|
| CMI n = 110 % (n) |
No CMI n = 1145 % (n) |
CMI n = 64 % (n) |
No CMI = 493 % (n) |
||||
| Anyone | 52.4 (57) | 50.8 (601) | 68.9 (44) | 77.8 (390) | 1.0 (0.6–1.6) | 0.6 (0.4–1.2) | 0.15 |
| Informal | 37.0 (38) | 45.0 (521) | 52.0 (31) | 70.4 (343) | 0.68 (0.40–1.1) | 0.5 (0.3–0.8) | <0.01 |
| Health professionals | 35.0 (42) | 13.4 (171) | 44.3 (34) | 25.6 (138) | 3.2 (1.9–5.5) | 2.7 (1.3–5.5) | <0.01 |
| Other formal | 23.3 (28) | 17.8 (231) | 39.0 (26) | 33.2 (174) | 1.2 (0.60–2.3) | 0.7 (0.4–1.3) | 0.27 |
| HP only | 11.8 (12) | 1.5 (24) | 12.5 (8) | 3.1 (20) | 7.0 (3.0–16.2) | 6.9 (2.6–18.3) | <0.001 |
a. Adjusted for age, gender, ethnicity, marital status, employment, tenancy and presence of health problems as a result of IPV.
Discussion
Key findings
In a large, nationally representative crime survey in England and Wales, and comparing people with and without CMI of more than 1 year's duration; the population-weighted prevalence of being a victim of any IPV in the past year was 20.0% v. 5.3% among women and 6.9% v. 3.1% among men. After adjusting for socio-demographics, we found that people with CMI were two to five times more likely to experience emotional, physical and sexual IPV as those without (with a trend for higher odds among women than men). The highest relative odds were found for sexual IPV against women; 30 in 1000 women with CMI reported sexual assault by a partner in the past year compared to 4 in 1000 of women without CMI (with adjusted relative odds of 5.4). Victims with CMI were twice as likely to experience mental or emotional problems and five times more likely to attempt suicide as a result of this IPV than victims without CMI. Whilst there was no difference in overall disclosure rates between victims with and without CMI, the former were half as likely disclose IPV to informal social networks, but twice as likely to disclose it to a health professional. Most victims disclosed their experiences of IPV to multiple parties, but around 10% of IPV victims with CMI (and 1.5% of those without) disclosed exclusively to a health professional.
Strengths and limitations
The strengths of this study include clearly defined hypotheses; a large adequately powered study; a nationally representative sample; and detailed measures of IPV impact and disclosure. The IPV measure used was one that was specifically developed for use in the BCS Reference Walby and Allen12 and has strengths and limitations. Its strengths include two features that are widely recognised as good practice in IPV/domestic violence research: (a) the use of specific behavioural questions on whether the respondent had experienced specific acts of violence over a well-defined time period, rather than more generic questions on whether they had experienced ‘abuse’ or ‘domestic violence; (b) the use of a self-completion questionnaire rather than interview-based questionnaire, which provides greater privacy, confidentiality and safety for the respondent. 3 Both of these features are associated with greater rates of disclosure, 3 with past Home Office research showing that respondents were five times more likely to disclose domestic violence when asked about this in the self-completion questionnaire than when asked about it in the interviewer-based questionnaire. Reference Walby and Allen12 Limitations of this IPV measure include (a) the lack of validation studies against other ‘gold standard’ IPV measures and (b) the lack of sufficient detail on the context, nature and frequency of violence which would allow a distinction between isolated acts of violence v. prolonged, severe and controlling violence. Reference Johnson15 Other strengths of this study include adjustment for important socio-demographic confounders. We carried out additional analyses on a separate national survey (the 2007 Adult Psychiatric Morbidity Survey-APMS), which used a similar CMI measure to that used in the BCS, Reference McManus, Meltzer, Brugha, Bebbington and Jenkins16 and which enabled us to indirectly assess the potential clinical characteristics of this group.
Study limitations include lack of details on the nature of the CMI within the BCS dataset, although the study definition meets internationally accepted definitions of disability, 17 and we indirectly assessed clinical characteristics of people with CMI using APMS data. There is potential for non-participation bias, since nearly 20% (N = 6219) of those eligible for the self-completion questionnaire did not complete the domestic violence module, either because they refused (8%) or because they were unable to complete the module without interviewer help (13%). Non-respondents were more likely to be older, unemployed and from an ethnic minority background. Some of these factors are associated with IPV risk, and so may lead to bias in the prevalence estimates. The domestic violence module was also less likely to be completed by those with versus those without CMI. Those with the greatest disability may be more likely to opt out of participating in the crime survey, and where they do participate they are more likely to opt out of the optional domestic violence module (since it increases participant burden). Greater disability is likely to be associated with greater IPV risk; therefore, we may have underestimated the relative risk for those with mental illness. It is possible that people with and without mental illness had differential recall or reporting of IPV, although there is some evidence that self-reported victimisation among people with mental illness is reliable. Reference Goodman, Thompson, Weinfurt, Corl, Acker and Mueser18 A limitation of cross-sectional studies is that it is often difficult to be certain of the direction of causality. In this study, the definitions of ‘CMI’ (duration more than 1 year) and ‘recent IPV’ (within the past year) mean that mental illness would have preceded ‘recent IPV’, except where there was measurement error due to reporting or recall bias. Nonetheless, the onset of IPV and CMI was not measured, and some participants may have experienced IPV before the onset of their mental illness (where IPV may have causally contributed to their CMI). The association found in this study between CMI and IPV could plausibly explained by two pathways: mental illness could be a risk factor for IPV and/or historical IPV could be a risk factor for both CMI and recent IPV. Both of these pathways are supported by a recent systematic review of longitudinal studies, which found evidence for a bidirectional causal relationship between common mental disorders and IPV. Reference Devries, Mak, Bacchus, Child, Falder and Petzold19 Findings are likely to generalise to other high-income settings, which tend to have similar prevalence and risk factors for IPV. 3
Findings in the context of past studies and implications
This is the first study to directly compare recent IPV (emotional, physical and sexual) among men and women with and without pre-existing mental illness. Reference Devries, Mak, Bacchus, Child, Falder and Petzold5,Reference Trevillion, Oram, Feder and Howard8,Reference Oram, Trevillion, Feder and Howard9,Reference Hughes, Bellis, Jones, Wood, Bates and Eckley20 Our findings on the prevalence and relative odds of any past-year IPV among women with mental illness are consistent with recent systematic reviews. Reference Devries, Mak, Bacchus, Child, Falder and Petzold5,Reference Trevillion, Oram, Feder and Howard8,Reference Hughes, Bellis, Jones, Wood, Bates and Eckley20 We extend previous findings by reporting an excess risk in men as well as in women with mental illness; and an excess risk for all forms of IPV, including emotional and sexual IPV. The findings on emotional IPV are important, since there is evidence that emotional IPV may lead to greater health problems than physical IPV, Reference Jewkes21–Reference Mechanic, Weaver and Resick23 whereas most research and clinical enquiry is focused on the latter. We found that the greatest relative odds were for sexual IPV against women, which were increased fivefold, with 3 in 100 women with CMI reporting past-year sexual violence by a partner. These findings suggest that health professionals should enquire about all forms of recent IPV, including emotional and sexual abuse, among people with CMI.
We report the novel finding that victims with pre-existing mental illness had an excess risk of psychological ill health (including suicide attempts) following IPV; consistent with findings on the greater psychological health impact of community violence against people with mental illness. Reference Khalifeh, Howard, Osborn, Moran and Johnson24 We also found that they were more likely to disclose IPV exclusively to healthcare professionals. These findings underline the key role that health professionals play in detecting IPV and supporting victims amongst this vulnerable population. The APMS analysis suggests that the majority of people with self-reported CMI have sought help from primary care, and about 20% have sought help from secondary health services in the preceding year, providing an opportunity for interventions by healthcare professionals. However, IPV is under-detected by primary care and mental health professionals, Reference Howard, Trevillion, Khalifeh, Woodall, Agnew-Davies and Feder25,Reference Ramsay, Rutterford, Gregory, Dunne, Eldridge and Sharp26 who report a lack of knowledge and preparedness to address IPV. Reference Rose, Trevillion, Woodall, Morgan, Feder and Howard27,Reference Nyame, Howard, Feder and Trevillion28
Complex interventions that include staff training and integration of advocacy workers within healthcare settings have been shown to improve detection of IPV and subsequent referral. Reference Feder, Davies, Baird, Dunne, Eldridge and Griffiths29,Reference Trevillion, Byford, Cary, Rose, Oram and Feder30 Recent NICE guidance on domestic violence 31 emphasises that identification of, and appropriate responses to, IPV among mental health service users should be part of good clinical practice; so mental health professionals should be trained to respond safely within well-defined care pathways. Reference Howard, Feder and Agnew-Davies32 This study found that women with CMI were particularly vulnerable to sexual violence, suggesting that training for mental health professionals should be tailored accordingly. However, there are still few studies on specific interventions for IPV in people with CMI. Reference Warshaw, Sullivan and Rivera33 Future research should focus on interventions to decrease the risk and impact of IPV among those with mental illness.
Funding
H.K. is supported by an MRC Population Health Sciences Fellowship (reference ). L.H. is supported by the National Institute for Health Research NIHR Research Professorship .
Acknowledgements
We acknowledge the CSEW Principal Investigator (Office for National Statistics), sponsors (Home Office, Ministry of Justice, Office for National Statistics), data collectors (TNS BMRB) and the UK Data Archive. The views expressed in this publication are those of the authors alone and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.









eLetters
No eLetters have been published for this article.