Bipolar affective disorder is a chronic, severe mental disorder characterised by acute episodes of depressed, manic and mixed mood states. 1,2 Globally bipolar disorder affects 0.7% of the adult population, Reference Ferrari, Baxter and Whiteford3 and is associated with significant disability and cost owing to the severity and chronicity of the condition. Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine4,Reference Kleine-Budde, Touil, Moock, Bramesfeld, Kawohl and Rossler5 In 2010 the disorder accounted for 1.3% of years of life lost to disability globally, and was the fifth leading cause of disability among mental and substance use disorders. Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine4 Although pharmacotherapy is the recommended first-line therapy for manic, depressive and residual states, Reference Yatham, Kennedy, Parikh, Schaffer, Beaulieu and Alda6 medication adherence is typically poor, Reference Arvilommi, Suominen, Mantere, Leppamaki, Valtonen and Isometsa7 relapse rates are high, Reference Gitlin, Swendsen, Heller and Hammen8 and full remission is rare. 1 Psychosocial therapies are recommended as an adjunctive treatment to medications in many guidelines, 9–11 to reduce relapse to acute depression or mania, potentially through improved medication adherence, identification of early warning signs, self-management and family communication. Reference Miklowitz, Yatham and Kusumakar12 These psychosocial therapies have been evaluated through randomised controlled trials (RCTs) and meta-analyses with mixed results. Previous systematic reviews and meta-analyses were based on small numbers of studies, Reference Scott, Colom and Vieta13,Reference Lam, Burbeck, Wright and Pilling14 were limited to particular interventions (e.g. CBT only), Reference Lynch, Laws and McKenna15 did not cover key peripheral indicators of recovery and did not adjust for study characteristics such as the control groups. Reference Furukawa, Noma, Caldwell, Honyashiki, Shinohara and Imai16 The most comprehensive review and meta-analysis recently published produced significant positive effects for some psychosocial interventions; however, multiple analyses were undertaken, several of which included only one study and did not address study quality. Reference Jauhar, McKenna and Laws17,Reference Oud, Mayo-Wilson, Braidwood, Schulte, Jones and Morriss18 Importantly, the study did not use meta-regression to examine factors that might have influenced intervention efficacy. The purpose of our systematic review and network meta-analysis (NMA) was to address these previous limitations by employing the NMA approach to examine the efficacy of psychosocial interventions used for the adjunctive treatment of bipolar disorder in adults on relapse rates, depressive and manic symptoms, global functioning and medication adherence. Meta-regression techniques were used to identify factors related to the efficacy of this group of therapies. Unlike standard meta-analysis that can compare only two treatments at a time, NMA (also called mixed treatment comparisons) can assess the relative effectiveness of several interventions simultaneously even when the treatments have not been directly compared. It combines the evidence from studies directly comparing interventions (RCTs) with indirect information (comparisons made between RCTs through a common comparator such as treatment as usual). Reference Jansen, Fleurence, Devine, Itzler, Barrett and Hawkins19–Reference Cipriani, Higgins, Geddes and Salanti21 Using NMA addresses the issue of multiple testing found in previous meta-analyses as well as providing additional information in the form of indirect comparisons. The hypothesis was that network meta-analysis would improve the rigour of the results.
Method
Electronic peer-reviewed databases including Medline, PsycINFO and the Cochrane Library of Systematic Reviews accessed through EBSCOhost, as well as the clinical trial registries ClinicalTrials.gov, EU Clinical Trials Register, ISRCTN Registry, WHO International Clinical Trials Registry Platform and the Australian New Zealand Clinical Trial Registry were searched. We used search terms pertaining to bipolar disorder (e.g. bipolar disorder, cyclothymic personality) and psychotherapy (e.g. psychotherapy, behaviour therapy, brief psychotherapy, client centred therapy, cognitive behaviour therapy, emotion focused therapy, group psychotherapy, interpersonal psychotherapy, narrative therapy, psychotherapeutic counselling, solution focused therapy). Searches were limited to studies conducted among humans and published in the English language from inception of the databases to 31 January 2016. Full details of the search strategy are provided in online Table DS1. A review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO), registration number 2015:CRD42015016975. All identified publications were reviewed independently by two authors (E.S. and M.L.C.) against the selection criteria. Any discrepancies in the selection of articles were discussed among these authors to arrive at the final list of included studies.
We included randomised controlled trials that tested a psychosocial intervention against any comparator for the treatment of bipolar disorder (including types 1 and 2 disorder and cyclothymia in the acute or maintenance phase) among adults aged at least 18 years who were receiving regular mood-stabilising medication at intake. We included any intervention that comprised a psychosocial strategy alongside pharmacological treatment with the primary aim of improving bipolar disorder outcomes. We excluded studies where the sample age range included those younger than 18 years; where part or all of the sample were not receiving regular mood-stabilising medication; where the authors did not report outcomes related to changes in bipolar disorder outcomes; or where data were reported in a non-usable format (e.g. graphically) and usable data could not be obtained from the study authors. The rationale for excluding studies with people less than 18 years old related to the atypical presentation of bipolar disorder in youth, since it is unclear if a bipolar disorder diagnosis in young people is the same as in adults. Reference McClellan, Kowatch and Findling22 Studies that evaluated collaborative care were excluded since this approach not only involved psychosocial interventions but also changed the delivery of care to study participants.
Measures of treatment effect
All outcomes were derived from the primary end-point of each study or the longest follow-up time point. We extracted the number of participants meeting criteria for a manic or depressive episode (pooled) at follow-up as the primary outcome of relapse. Methods used to assess relapse included standardised clinical interviews yielding DSM or ICD diagnoses, predetermined cut-off points on depression or mania symptom scales, or admission to hospital. Intervention efficacy for the pooled outcome of depressive or manic relapse was assessed using a risk ratio (RR). We extracted the means and standard deviations of participants' scores on reliable and valid symptom rating scales for depression and mania, where lower scores equated to lower levels of symptoms. We also extracted means and standard deviations of participants' scores on reliable and valid measures of global functioning such as the Personal and Social Performance Scale and the Global Assessment of Functioning (GAF) scale, Reference Endicott, Spitzer, Fleiss and Cohen23 where higher scores equated to better functioning. In instances where the direction of a scale was reversed (higher scores equated to poorer functioning) we subtracted the mean from the maximum possible score on the scale if that was available, and if not multiplied the mean values by −1 to ensure all outcomes were in the same direction. Reference Higgins and Green24 Intervention efficacy was determined by calculation of a standardised mean difference (SMD) on these scales (measured using Hedges' g). We extracted the number of participants classified as being adherent to their regular psychiatric medication schedule, based on serum mood stabiliser concentrations above a pre-specified cut-off level or based on patient self-report (e.g. taking medication on at least 50% of the days since the preceding assessment) or reports from carers, family members or health professionals. Medication adherence was assessed using a risk ratio.
Risk of bias
Risk of bias was examined using the Cochrane Collaboration tool and techniques for assessing risk of bias. Reference Higgins and Green24 Two authors (M.L.C. and E.S.) independently examined each study and rated it as low risk (score 3), high risk (score 1) or ‘risk unable to be determined’ (score 2) for each domain. A total quality score was calculated as the sum of all components. A quality index with a value between 0 and 1 was calculated for each study by dividing the total quality score by the highest scoring study in the group. This index was then used in the quality effects meta-analysis described below.
Data extraction
Data were extracted independently by two of the authors (M.L.C. and E.S.). Each extracted data for half the studies and then cross-checked the entries for errors and consistency. Where studies reported outcomes for particular subgroups of the sample rather than for the control and intervention groups at an aggregate level, we calculated these values using the pooled variance and weighted mean. In instances where usable data were not reported in the manuscript, attempts were made to contact study authors for unpublished data.
Statistical analysis
Each of the five outcomes evaluated required a separate network meta-analysis which was conducted using MetaXL version 5.1, an Excel add-in developed by EpiGear International Pty Ltd. Reference Barendregt and Doi25 MetaXL implements the generalised pairwise modelling framework for network meta-analysis; this makes systematic indirect estimates of the input studies, followed by meta-analysis of all interventions compared with the common control. Reference Barendregt and Doi25 Whereas most meta-analyses use a random effects model, the primary analyses for this meta-analysis employed the inverse variance heterogeneity (IVhet) model, which uses the inverse variance study weights with a quasi-likelihood based variance structure for the pooled estimate to manage the potential underestimation of the statistical error due to heterogeneity. Reference Doi, Barendregt, Khan, Thalib and Williams26 We consider this superior to the random effects model because it addresses the known issue of underestimation of the statistical error with the random effects model. Reference Brockwell and Gordon27 A quality effects model was used as a sensitivity analysis since it favours larger and higher-quality trials and produces a conservative confidence interval for the pooled point estimate. Reference Doi, Barendregt, Khan, Thalib and Williams28 Effect sizes (Hedges' g) were specified as 0.2 small, 0.5 medium and 0.8 large. Reference Hedges and Olkin29
The assumption of transitivity, that the direct and indirect evidence are in agreement, underpins NMA. Reference Jansen, Fleurence, Devine, Itzler, Barrett and Hawkins19 Consistency, a statistical measure of transitivity, was assessed through computation of the H statistic which describes the relative excess in heterogeneity (Cochrane's Q) over its degrees of freedom. Reference Barendregt and Doi25 To explain any further causes of heterogeneity on the basis of study characteristics and characteristics of the intervention, we conducted weighted linear regression models using the Stata ‘regress’ command. Study-level weights were obtained from the IVhet meta-analyses, and were included in the regressions using the analytical weights option. Separate weighted regressions were conducted where the overall meta-analysis produced a significant result at the primary outcome time-point within each study, and thus were conducted for relapse rates, adherence rates, manic symptoms and GAF. Ratio data (including relapse rates and adherence rates) were natural log-transformed prior to analysis. We selected factors for the regression analysis a priori based on published research. The analysis examined the effect of intervention facilitator (clinician – psychiatrist or psychologist – v. trained therapist); intervention delivery format (group v. individually delivered); total intervention exposure time (in minutes); follow-up time-point (in months); any psychiatric comorbidity at baseline (anxiety, schizophrenia, suicidal ideation, antisocial personality disorder, substance use disorder or borderline personality disorder); phase of illness at baseline (euthymic v. acute); and bipolar disorder type at baseline (type 1 only v. types 1 and 2). The adjusted R 2 index was employed to quantify goodness-of-fit for each model. Statistical significance for all analyses was set at P<0.05.
Results
We identified 176 studies as potentially appropriate for inclusion in the meta-analysis (Fig. 1). There was 93% agreement between reviewers (κ = 0.84, P<0.05) for full-text articles meeting the inclusion criteria. Once data were extracted, 45 publications from 41 unique trials were suitable for the pooled analyses. Reference Ball, Mitchell, Corry, Skillecorn, Smith and Malhi30–Reference Zaretsky, Lancee, Miller, Harris and Parikh74 Thirty-eight studies were excluded owing to inappropriate study designs; 31 were excluded because of lack of appropriate results for the pooled analyses, such as group means and standard deviations at study end-points. Three trials evaluated interpersonal and social rhythm therapy (IPSRT) but only one provided outcome data that could be used in the pooled analyses, and this trial was conducted in people with type 2 bipolar disorder who were not taking medication at study entry; Reference Swartz, Frank and Cheng75 it was therefore determined not to be a trial of adjunctive therapy and excluded. A single attempt was made to contact 11 study authors where insufficient or unusable data were reported in the manuscript. Two responses were received, and one author provided additional data. However, that study was subsequently deemed not to fit the inclusion criteria as noted above and was excluded. Reference Swartz, Frank and Cheng75

Fig. 1 PRISMA flow chart of the study selection process
The 41 trials analysed in the meta-analysis contained data from a combined total of 3119 individuals and are described in online Table DS2. Gender was reasonably balanced with 57% of participants being female, and ages ranged from 18 years to 77 years (mean 38.8, s.d. = 10.7). Most studies recruited patients diagnosed with the broad inclusion criteria of bipolar disorder according to DSM criteria, which include type 1, 2 or cyclothymic disorder (33 trials, n = 2620). Reference Ball, Mitchell, Corry, Skillecorn, Smith and Malhi30,Reference Castle, White, Chamberlain, Berk, Berk and Lauder33–Reference Lahera, Benito, Montes, Fernandez-Liria, Olbert and Penn48,Reference Lauder, Chester, Castle, Dodd, Gliddon and Berk52,Reference Madigan, Egan, Brennan, Hill, Maguire and Horgan54,Reference Meyer and Hautzinger55,Reference Perlick, Miklowitz, Lopez, Chou, Kalvin and Adzhiashvili60,Reference Perry, Tarrier, Morriss, McCarthy and Limb61,Reference Reinares, Colom, Sanchez-Moreno, Torrent, Martinez-Aran and Comes63–Reference Scott, Garland and Moorhead66,Reference Simon, Ludman, Unutzer, Bauer, Operskalski and Rutter68–Reference Zaretsky, Lancee, Miller, Harris and Parikh74 Nearly half of the studies required patients to be euthymic at intake (20 trials, n = 1262). Reference Ball, Mitchell, Corry, Skillecorn, Smith and Malhi30,Reference Castle, White, Chamberlain, Berk, Berk and Lauder33,Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea and Benabarre35,Reference Costa, Cheniaux, Rosaes, Carvalho, Freire and Versiani37,Reference Depp, Ceglowski, Wang, Yaghouti, Mausbach and Thompson38,Reference D'Souza, Piskulic and Sundram40–Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine42,Reference Gonzalez Isasi, Echeburua, Liminana and Gonzalez-Pinto44–Reference Jones, Smith, Mulligan, Lobban, Law and Dunn46,Reference Lahera, Benito, Montes, Fernandez-Liria, Olbert and Penn48–Reference Lam, Watkins, Hayward, Bright, Wright and Kerr50,Reference Meyer and Hautzinger55,Reference Perich, Manicavasagar, Mitchell, Ball and Hadzi-Pavlovic59,Reference Reinares, Colom, Sanchez-Moreno, Torrent, Martinez-Aran and Comes63,Reference Smith, Griffiths, Poole, di Florio, Barnes and Kelly69,Reference Williams, Alatiq, Crane, Barnhofer, Fennell and Duggan73,Reference Zaretsky, Lancee, Miller, Harris and Parikh74
The majority of trials evaluated CBT (16 trials) and psychoeducation (12 trials) (Table 1). Another group of four trials clearly described the intervention as a combination of psychoeducation and CBT and were analysed as a separate subgroup. Three studies were included that evaluated family-focused therapy (FFT). A separate category of carer-focused interventions included data from five evaluations. A novel study evaluating psychoeducation combined with a mobile telephone application, Personalized Real-time Intervention for Stabilizing Mood (PRISM), was analysed as a separate group. The outcome measures that could be combined in meta-analysis varied across studies, with depression symptom scales being the most common outcome measure available from 25 trials, relapse (depression or mania) assessed in 24 trials, mania rating scales reported in 18, GAF scores from 14 and medication adherence from 11. Additional details of the studies used for the meta-analysis are presented in online Table DS2. The most common comparator was treatment as usual (TAU); eight trials contained active comparators. Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea and Benabarre35,Reference Depp, Ceglowski, Wang, Yaghouti, Mausbach and Thompson38,Reference Lauder, Chester, Castle, Dodd, Gliddon and Berk52,Reference Meyer and Hautzinger55,Reference Perlick, Miklowitz, Lopez, Chou, Kalvin and Adzhiashvili60,Reference Rea, Tompson, Miklowitz, Goldstein, Hwang and Mintz62,Reference Weiss, Griffin, Jaffee, Bender, Graff and Gallop72,Reference Zaretsky, Lancee, Miller, Harris and Parikh74
Table 1 Publications categorised by intervention groups and outcomes reported
| Intervention type and description | Publications | Outcomes available |
|---|---|---|
| Cognitive–behavioural therapy | ||
| In CBT therapists aim to work collaboratively with patients to understand the link between thoughts, feelings and behaviours, and to identify and modify unhelpful thinking patterns, underlying assumptions and idiosyncratic cognitive schemata about the self, others and the world. This category also includes ‘third wave’ CBT such as mindfulness exercises Reference Shinohara, Honyashiki, Imai, Hunot, Caldwell and Davies82 |
Ball et al (2006) Reference Ball, Mitchell, Corry, Skillecorn, Smith and Malhi30 | A, D, GAF, M, R |
| Cochran (1984) Reference Cochran34 | A, R | |
| Costa et al (2011) Reference Costa, Cheniaux, Rosaes, Carvalho, Freire and Versiani37 | D, M | |
| Gomes et al (2011) Reference Gomes, Abreu, Brietzke, Caetano, Kleinman and Nery42 | R | |
| Jones et al (2015) Reference Jones, Smith, Mulligan, Lobban, Law and Dunn46 | D, GAF, R | |
| Kirk & Gumley (2014) Reference Kirk and Gumley47 | D, GAF | |
| Lahera et al (2013) Reference Lahera, Benito, Montes, Fernandez-Liria, Olbert and Penn48 | D, GAF, M | |
| Lam et al (2000) Reference Lam, Bright, Jones, Hayward, Schuck and Chisholm49 | D, GAF, M, R | |
| Lam et al (2003), Reference Lam, Watkins, Hayward, Bright, Wright and Kerr50 (2005) Reference Lam, Hayward, Watkins, Wright and Sham83 | A, D, M, R | |
| Meyer & Hautzinger (2012) a Reference Meyer and Hautzinger55 | D, GAF,M, R | |
| Perich et al (2013) Reference Perich, Manicavasagar, Mitchell, Ball and Hadzi-Pavlovic59 | D, M | |
| Schmitz et al (2002) Reference Schmitz, Averill, Sayre, McCleary, Moeller and Swann65 | A | |
| Scott et al (2001) Reference Scott, Garland and Moorhead66 | D, GAF, R | |
| Scott et al (2006) Reference Scott, Paykel, Morriss, Bentall, Kinderman and Johnson67 | R | |
| Weiss et al (2009) a Reference Weiss, Griffin, Jaffee, Bender, Graff and Gallop72 | D, M | |
| Williams et al (2008) Reference Williams, Alatiq, Crane, Barnhofer, Fennell and Duggan73 | D | |
| Psychoeducation | ||
| Psychoeducation aims to provide information on the disorder and its treatment, as well as the social and family consequences of the disorder |
Cardoso et al (2015) Reference Cardoso, Mondin, Reyes, Zeni, Souza and da Silva32 | D, M |
| Castle et al (2010) Reference Castle, White, Chamberlain, Berk, Berk and Lauder33 | D, M, R | |
| Colom et al (2003), Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea and Benabarre35 (2009) a Reference Colom, Vieta, Sánchez-Moreno, Palomino-Otiniano, Reinares and Goikolea36 | A, R | |
| Dogan & Sabanciogullari (2003) Reference Dogan and Sabanciogullari39 | A, D, GAF | |
| D'Souza et al (2010) Reference D'Souza, Piskulic and Sundram40 | D, M, R | |
| Eker & Harkin (2012) Reference Eker and Harkin41 | A | |
| Javadpour et al (2013) Reference Javadpour, Hedayati, Dehbozorgi and Azizi45 | R | |
| Lin et al (2015) Reference Lin, Huang and Huang53 | D, M, R | |
| Perry et al (1999) Reference Perry, Tarrier, Morriss, McCarthy and Limb61 | R | |
| Sajatovic et al (2009) Reference Sajatovic, Davies, Ganocy, Bauer, Cassidy and Hays64 | D, GAF, M | |
| Simon et al (2005) Reference Simon, Ludman, Unutzer, Bauer, Operskalski and Rutter68 | R | |
| Smith et al (2011) Reference Smith, Griffiths, Poole, di Florio, Barnes and Kelly69 | D, GAF, M, R | |
| Combined CBT and psychoeducation | Gonzalez-Isasi et al (2010), Reference Isasi, Echeburua, Liminana and Gonzalez-Pinto43 (2014) Reference Gonzalez Isasi, Echeburua, Liminana and Gonzalez-Pinto44 | D, GAF, M |
| Lauder et al (2015) a Reference Lauder, Chester, Castle, Dodd, Gliddon and Berk52 | D, M, R | |
| Van Dijk et al (2013) Reference Van Dijk, Jeffrey and Katz70 | D | |
| Zaretsky et al (2008) a Reference Zaretsky, Lancee, Miller, Harris and Parikh74 | A, R | |
| PRISM | ||
| Psychoeducation and Personalized Real-time Intervention for Stabilizing Mood | Depp et al (2015) a Reference Depp, Ceglowski, Wang, Yaghouti, Mausbach and Thompson38 | D, GAF, M |
| Family-focused therapy | ||
| Family-focused therapy is based on the premise that aversive family environments affect the course of bipolar disorder. Treatment consists of psychoeducation, communication enhancement training and problem-solving training. These sessions included the person with bipolar disorder and family members to address the family dynamics that may affect the course of the disorder |
Miklowitz et al (2000), Reference Miklowitz, Simoneau, George, Richards, Kalbag and Sachs-Ericsson56 (2003) Reference Miklowitz, George, Richards, Simoneau and Suddath57 | D, R |
| Miller et al (2004) b Reference Miller, Solomon, Ryan and Keitner58 | A, R | |
| Rea et al (2003) a Reference Rea, Tompson, Miklowitz, Goldstein, Hwang and Mintz62 | R | |
| Carer-focused interventions | ||
| Carer-focused interventions used techniques such as psychoeducation, but included only the carer or family member. Note that the data extracted for the meta-analysis was based on the outcomes for the person with disorder not the carer/family member |
Bordbar et al (2009) Reference Bordbar, Soltanifar and Talaei31 | R |
| Madigan et al (2012) b Reference Madigan, Egan, Brennan, Hill, Maguire and Horgan54 | GAF | |
| Perlick et al (2010) a Reference Perlick, Miklowitz, Lopez, Chou, Kalvin and Adzhiashvili60 | D, M | |
| Reinares et al (2008) Reference Reinares, Colom, Sanchez-Moreno, Torrent, Martinez-Aran and Comes63 | A, R | |
| Van Gent & Zwart (1991) Reference Van Gent and Zwart71 | A, GAF | |
A, adherence; CBT, cognitive–behavioural therapy; D, depression symptom scales; GAF, Global Assessment of Functioning; M, mania rating scales; R, relapse.
a. Studies with an active comparator group.
b. Studies with more than one treatment group.
We assessed all included studies for risk of bias (see online Figs DS1 and DS2). Of the 41 included trials, reporting of random sequence generation and allocation concealment was mostly absent, and as such most studies were rated as unclear for these domains (27 and 21 studies respectively). Most studies either did not report masking of participants or reported that participants were actively aware of their treatment allocation, and thus 26 and 10 studies were rated respectively as unclear or at high risk of bias; however, masking of treatment allocation is acknowledged as being inherently difficult in studies of behavioural interventions. Reference Friedberg, Lipsitz and Natarajan76 Masking of outcome assessors was mostly done, and most trials (24) were rated as low risk for this domain. Similarly, most studies (24) were rated as low risk for attrition bias, as authors primarily conducted intention-to-treat analyses and reported low and equal attrition between treatment conditions. Although just over half of studies were classified as having a low risk of bias due to selective reporting (21 studies), more than a third were classified as high risk for this domain (15 studies), primarily where raw mean scores and standard deviations on symptom screening scales for depression and mania were not reported, or where raw numbers of participants meeting criteria for relapse were not reported or only displayed graphically. Most studies were classified as having a low risk of bias due to any other cause (31 studies); however, 8 studies were rated as having high risk of bias, mostly where the intervention and control groups were not equivalent on key measures of depression and mania at baseline (e.g. significant differences in mean scores on symptom screening scales).
The network diagram for the outcome of pooled manic or depressive relapse (online Fig. DS3) contained seven nodes: five psychosocial interventions and two control conditions. The carer-focused interventions were significantly more efficacious than TAU on the outcome of relapse with the IVhet model as shown in the forest plot (Fig. 2(a)): RR = 0.61, 95% CI 0.44–0.86). Only two trials of carer interventions (70 participants in total) were used in this analysis, but the quality of both was high. Family-focused therapy, psychoeducation and CBT were also associated with reduced risk ratios for relapse v. the control condition of TAU; however, these were not significant with the IVhet model or QE models (forest plots are shown in online Figs DS8–17). The network of interventions with depression symptom scale score outcomes (online Fig. DS4) included six psychosocial interventions and three control conditions. One trial compared a carer-focused intervention with an attention control condition, which meant it was disconnected from the network and therefore could not be analysed in the network meta-analysis. Reference Perlick, Miklowitz, Lopez, Chou, Kalvin and Adzhiashvili60 The SMD results presented in Fig. 2(b) indicate that although three of the psychosocial interventions (psychoeducation plus CBT, FFT and psychoeducation) and one of the control conditions (group drug counselling) decreased depression symptom scores compared with TAU, none had a significant effect. The combination of psychoeducation and PRISM significantly increased depression scores compared with TAU.
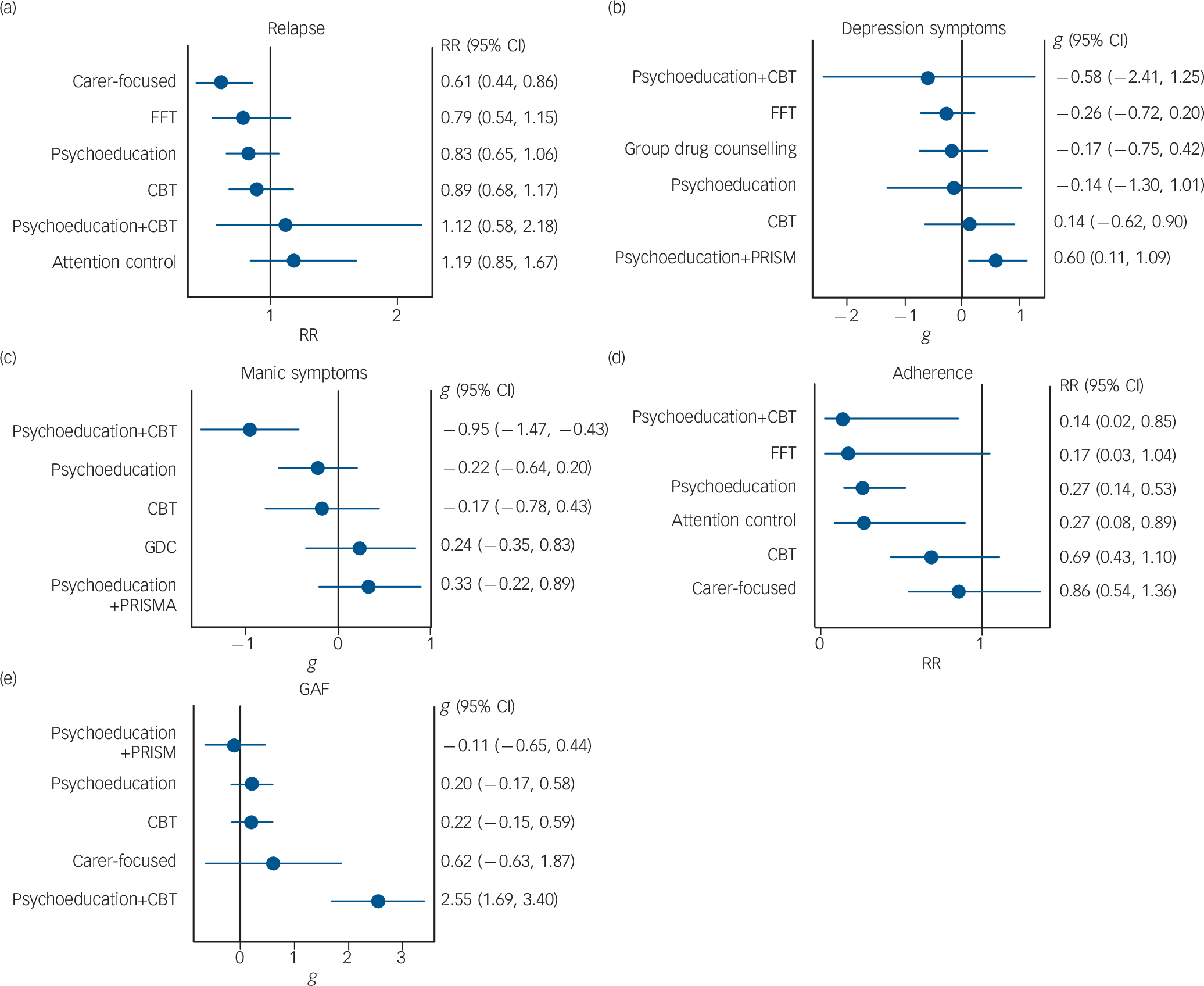
Fig. 2 Forest plots of network meta-analysis results (all v. treatment as usual). (a) Relapse: all treatments; (b) all depression symptoms; (c) all mania symptoms; (d) adherence to medication; (e) Global Assessment of Functioning. CBT, cognitive–behavioural therapy; FFT, family-focused therapy; GAF, Global Assessment of Functioning; GDC, group drug counselling; RR, risk ratio.
The network of interventions providing mania symptom scale score outcomes was similar to the depression network with the exception of lacking the FFT v. TAU branch (online Fig. DS5). The carer-focused intervention and attention control node was disconnected and thus could not be analysed as part of the network. Figure 2(c) shows that the combination of psychoeducation and CBT had a significant, large effect on reducing manic symptoms v. TAU (SMD = −0.95, 95% CI −1.47 to −0.43). This intervention was also superior to all other interventions included. The effect of psychosocial therapies on the risk of non-adherence are shown in Fig. 2(d) and the network diagram in online Fig. DS6. People who received the combination of psychoeducation and CBT were significantly less likely to report non-adherence to their bipolar medications than those receiving TAU (RR = 0.14, 95% CI 0.02–0.85). Psychoeducation alone was also associated with a significantly lower risk of non-adherence with bipolar medications (RR = 0.27, 95% CI 0.14–0.53) as was the attention control condition (RR = 0.27, 95% CI 0.08–0.89). The network of interventions with GAF outcomes contained six nodes (online Fig. DS7). Psychoeducation and CBT had a significant large effect on GAF scale scores compared with TAU (SMD = 2.55, 95% CI 1.69–3.40), as shown in Fig. 2(e). The network meta-analysis results for the depression, mania and GAF scales did not differ with the quality effects models (see online Figs DS8–17 for results using the alternative models). The weighted average H statistic for all the networks in this analysis was less than 3, indicating minimal inconsistency in treatment effects. The specific H values using the inverse variance heterogeneity model were relapse 1.06, depression symptom scores 2.14, mania symptom scores 1.26, adherence 1, GAF 1.11.
Meta-regression
Weighted regressions revealed that the risk of relapse was higher in studies where samples comprised participants with any comorbid psychiatric disorder at baseline, compared with studies where participants were required to have no existing comorbid psychiatric disorder to meet inclusion criteria: t(25) = 2.38, P = 0.03, adjusted R 2 = 16.3%; Table 2, online Fig. DS18). No factor was significantly associated with adherence rates. For symptoms of mania and GAF scores, studies with longer follow-up data collection had larger effect sizes than those collecting data only in the mid or short term: t(18) = 2.63, P = 0.02, adjusted R 2 = 25.8% for mania and t(15) = 5.19, P<0.01, adjusted R 2 = 65.0% for GAF scores (Table 2, online Figs DS19 and DS20). Additionally, effect sizes for improvements in GAF scores were smaller in studies where samples comprised participants diagnosed with type 1 and 2 disorder, compared with studies where samples were limited to people with type 1 only: t(15) = −3.03, P = 0.01, adjusted R 2 = 36.9% (Table 2, online Fig. DS21).
Table 2 Weighted regressions examining factors related to intervention efficacy at the longest follow-up assessment

| Relapse rate | Adherence rate | Manic symptoms | GAF | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
t
(d.f. = 25) |
P | Adj. R
2
(%) |
t
(d.f. = 12) |
P | Adj. R
2
(%) |
t
(d.f. = 18) |
P | Adj. R
2
(%) |
t
(d.f. = 15) |
P | Adj. R
2
(%) |
|
| Facilitator type a | 1.85 | 0.07 | 9.23 | 0.41 | 0.69 | −8.15 | −0.70 | 0.49 | −3.08 | 1.02 | 0.33 | 0.30 |
| Intervention delivery format b |
−1.64 | 0.11 | 6.63 | 0.09 | 0.93 | −9.92 | −0.61 | 0.55 | −3.83 | 1.18 | 0.26 | 2.77 |
| Total intervention exposure c |
0.84 | 0.42 | −1.71 | −1.50 | 0.18 | 13.38 | −0.77 | 0.46 | −3.26 | 1.02 | 0.34 | −0.49 |
| Follow-up length d | 0.83 | 0.41 | −1.28 | −1.56 | 0.15 | 11.46 | −2.63 | 0.02 | 25.83* | 5.19 | <0.01 | 64.98* |
| Psychiatric comorbidity e |
2.38 | 0.03 | 16.32* | 0.10 | 0.92 | −9.90 | 1.59 | 0.13 | 8.24 | −0.95 | 0.36 | −0.66 |
| Phase of illness f | 0.90 | 0.38 | −0.08 | 1.29 | 0.23 | 5.67 | 0.22 | 0.83 | −5.93 | 0.31 | 0.76 | −6.89 |
| Disorder type g | 1.64 | 0.11 | 6.61 | −1.40 | 0.19 | 8.02 | 0.92 | 0.38 | −0.95 | −3.03 | 0.01 | 36.95* |
Adj., adjusted; GAF, Global Assessment of Functioning.
a. Clinician (psychiatrist or psychologist) v. trained therapist.
b. Group v. individually delivered.
c. Total intervention exposure in minutes.
d. Length of final follow-up in months.
e. Patients with comorbid psychiatric disorders (anxiety, schizophrenia, suicidal ideation, antisocial personality disorder, substance use disorder or borderline personality disorder) at intake v. those without.
f. Euthymic state at intake v. acute phase.
g. Type 1 bipolar affective disorder v. types 1 and 2.
* P<0.05.
Discussion
To our knowledge this is the first network meta-analysis of psychosocial interventions used as adjunctive treatment for bipolar disorder, and the first meta-analysis to report pooled results for the outcomes of medication adherence and GAF for these interventions in people with this disorder. The study method addressed limitations in prior meta-analyses. The use of the IVhet and QE models as well as the addition of meta-regression increased the robustness of the findings. The results suggest that many psychosocial interventions lack high-quality evidence to support their efficacy as an adjunctive treatment to improve outcomes for people with bipolar disorder. Only the carer-focused interventions were associated with a significant reduction in the risk of relapse v. TAU. The effect for the carer interventions translates into a 39% relative risk reduction in relapse compared with TAU. However, the use of TAU as a control tends to inflate effect sizes compared with the use of active controls. Reference Furukawa, Noma, Caldwell, Honyashiki, Shinohara and Imai16 It is also important to note that only five RCTs evaluating carer-focused interventions could be included in this systematic review, suggesting a need for additional trials of this therapy in particular. Psychoeducation (delivered individually or in a group) as well as FFT and CBT showed trends toward improvement in the risk ratio but these results were non-significant under both IVhet and QE models. The lack of a significant effect on the risk of relapse for CBT was similar to the non-significant findings by Lynch et al. Reference Lynch, Laws and McKenna15 However, our analysis included five additional RCTs and was based on direct and indirect comparisons providing additional strength to the results. These results contrast with those of Oud et al, Reference Oud, Mayo-Wilson, Braidwood, Schulte, Jones and Morriss18 who found significant effects on depressive and manic relapses for group psychological interventions as well as for any relapse for individual psychological interventions at post-treatment and follow-up compared with TAU. The differences are probably due to differences in methodology (standard meta-analysis v. network) and the grouping of studies, since Oud et al had more groups with smaller numbers of studies per analysis.
None of the psychosocial interventions was found to have a significant effect in reducing depression symptom scale scores. Our analysis was based on the longest follow-up point and was similar to that of Oud et al, who showed that individual psychological interventions did not significantly reduce depression symptoms at follow-up assessments. Reference Oud, Mayo-Wilson, Braidwood, Schulte, Jones and Morriss18 Depressive symptoms in bipolar disorder are poorly addressed by both existing medication and psychotherapy strategies, reflecting the largest unmet need in the disorder. Reference Popp and Schneider77 Novel psychotherapeutic approaches to target depression and emotion regulation remain the next treatment horizon. Reference Cuijpers, Van Straten, Warmerdam and Smits78
The combination of psychoeducation and CBT demonstrated a significant large effect on reducing mania symptom scale scores compared with TAU as well as in comparison to all other comparators. This appears consistent with the significant but small effect that was seen in a previous meta-analysis for individual psychological interventions. Reference Oud, Mayo-Wilson, Braidwood, Schulte, Jones and Morriss18 However, other meta-analyses have not evaluated this combination of psychosocial interventions because the trials combining these two psychosocial therapies are recent, with the first trial published in 2008. Psychoeducation and the combination of psychoeducation and CBT were also found to significantly reduce the risk of medication non-adherence compared with TAU, which translates into a relative risk reduction for non-adherence of 86% v. TAU. Psychoeducation alone as well as the attention control comparator were also found to have a significant relative risk reduction of 73% compared with TAU. This appears to be the first meta-analysis to report these effects, but it should be interpreted prudently since the network of trials used in this analysis was limited. The combination of psychoeducation and CBT was also found to have a significantly large improvement in GAF scores compared with TAU as well as compared with psychoeducation, CBT, carer-focused interventions and psychoeducation plus PRISM. This result should be viewed cautiously since only one direct comparison of psychoeducation and CBT compared with TAU was included in the network of 15 trials for this analysis, and the result relies heavily on the indirect comparisons within the network.
The meta-regression results indicated that the risk of relapse was higher in studies comprising samples with psychiatric comorbidities, which has been described previously. Reference Otto, Simon, Wisniewski, Miklowitz, Kogan and Reilly-Harrington79,Reference Perlis, Ostacher, Patel, Marangell, Zhang and Wisniewski80 The greater improvements in mania symptoms and GAF at long-term follow-up relative to the short term may be indicative of increased efficacy of the interventions over time. The meta-regression of bipolar disorder type and GAF suggests that the psychosocial interventions have a greater benefit to global functioning in people diagnosed with type 1 bipolar disorder than for the group having a mix of type 1 and 2 diagnoses. This finding may be reflecting a similar mechanism to the higher risk of relapse among samples with psychiatric comorbidities, suggesting that psychosocial interventions may need to be tailored to specific manifestations of bipolar disorder and existing comorbidities, owing to the more severe course of illness associated with these disorders. Reference Mitchell81
Limitations and strengths
This analysis was limited by the number of RCTs available for inclusion and the data that could be pooled. Numerous potentially eligible studies could not be included owing to the lack of reporting of extractable data, including interventions testing IPSRT. The variety of outcomes assessed and the methods for assessing each outcome also limited the use of specific studies in these analyses. Consistency in the use of outcome measures would vastly improve the methodological rigour of the evaluations. The analysis was also limited by potential differences in the TAU control condition used in many of the trials. Although we have considered TAU to be a homogeneous control condition, there is the potential for variability within TAU due to physician knowledge of diagnosis, prescribing, referrals and use of treatment guidelines. Reference Mohr, Spring, Freedland, Beckner, Arean and Hollon51,Reference Popp and Schneider77,Reference Cuijpers, Van Straten, Warmerdam and Smits78 Given the small number of studies we were unable to undertake further analysis to explore this issue in detail.
Despite these limitations, these network meta-analyses strengthen treatment assessment and increase the precision of estimates through the combination of direct and indirect comparisons. The analyses examined the robustness of results under the inverse variance heterogeneity and quality effects models. They also included the assessment of peripheral improvements that are important to psychosocial functioning, including medication adherence and global functioning, which have not been included in previous reviews.
Study implications
Our results suggest that more research with a standard set of outcome measures similar to those used for trials of medications would greatly improve the rigour and comparability of the evaluations for future network meta-analyses. Given the differences in the resources required to deliver the interventions evaluated, additional cost-effectiveness assessments of the efficacious interventions from these network meta-analyses should be undertaken.
Our findings are important from both clinical and economic perspectives. From a clinical perspective, given the limited data available, this analysis suggests that psychosocial interventions should be offered to family members and carers since they significantly reduced risk of relapse in people with bipolar disorder. Psychoeducation should be offered to people with this disorder since the analysis found that it significantly reduced the risk of medication non-adherence. The combination of psychoeducation and CBT was also associated with significant decreases in the risk of medication non-adherence, reduced mania symptoms and improved global functioning and should be considered as an additional offering to people with bipolar disorder, particularly since it can be offered online. Reference Lauder, Chester, Castle, Dodd, Gliddon and Berk52 From an economic perspective these psychosocial therapies should be further evaluated to determine whether they are good value for money. Management of depression, however, remains the major unmet clinical need in the disorder.
Funding
This project was funded by the National Health and Medical Research Council (NHMRC grant ); E.S. and C.M. are supported by NHMRC Early Career Fellowships ( and respectively) and M.B. is supported by a NHMRC Senior Principal Research Fellowship . The views expressed in this paper are solely those of the authors and do not reflect the views of the NHMRC. The funder of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report.







eLetters
No eLetters have been published for this article.