Chronic post-traumatic stress disorder (PTSD) is a common disorder that people may develop after exceptionally threatening and distressing events. Psychological treatments from various theoretical perspectives have been found to be effective for chronic PTSD in previous reviews (Reference Van Etten and TaylorVan Etten & Taylor, 1988; Reference Bradley, Greene and RussBradley et al, 2005). Some of the earlier reviews had to rely on uncontrolled trials as well as controlled ones, and on uncontrolled effect sizes. There are now sufficient numbers of randomised controlled trials of psychological treatments of chronic PTSD to allow a meta-analysis of effect sizes in such trials. We present a comprehensive systematic review and meta-analysis of randomised controlled trials assessing the efficacy of psychological treatments in reducing symptoms of chronic PTSD, and comparing the efficacy of different types of psychological treatment in reducing symptoms of this disorder.
METHOD
This review and meta-analysis derive from work undertaken in the preparation of PTSD treatment guidelines for the National Institute for Health and Clinical Excellence (NICE) in the UK (National Collaborating Centre for Mental Health, 2005). Further details of the protocol are published within the full guideline.
A systematic bibliographic search was undertaken to find randomised controlled trials of psychological treatments for PTSD from databases (EMBASE, Medline, PsycINFO and CINAHL) and the Cochrane Library, with each database being searched from inception to August 2004. Additional papers were found by hand-searching the references of retrieved articles, previous systematic reviews and meta-analyses of psychological treatments for PTSD. The search was restricted to papers with English-language abstracts. In addition, data from unpublished studies or papers in press were sought by contacting experts within the field.
Selection
Studies were only considered if PTSD symptoms were the main target of treatment, all participants had had PTSD symptoms for at least 3 months following a traumatic event, at least 70% of participants had a diagnosis of PTSD, and PTSD symptoms were measured using a recognised scale. To be included studies had to be of randomised controlled design, with adult (>16 years old) participants; the studies had to report at least pre-treatment and post-treatment measures, and retain at least 50% of the original sample at the post-treatment assessment. There was no restriction regarding type of traumatic event. The minimum duration of symptoms was 1 month. Early intervention trials that only included participants with recent onset of PTSD were not included and are considered in a separate review (further details available from the author upon request). The searching and selection were done by a team of systematic reviewers led by R.M. Any disagreements with regard to inclusion or exclusion of a study were resolved by discussion with the other authors.
Validity assessment
All published and unpublished papers were assessed against the following quality criteria: random sequence generation, concealment of allocation, masked assessment of outcomes, number of withdrawals, tolerability, adequate reporting of data and intention-to-treat analysis.
Data abstraction
Study details including the nature of the traumatic events, participants’ characteristics and type of intervention were entered into a Microsoft Access database (version 2000), the quality criteria were applied and outcome data for included studies were entered into Review Manager version 4.2.3 for Windows. The application of quality criteria and the accuracy of outcome data were double-checked by a second reviewer.
Study characteristics
An initial narrative synthesis was undertaken to describe the scope (participants, settings, intervention type, comparators, measures of effect), quality and outcomes of the studies. Three main efficacy outcomes were considered: one dichotomous outcome (retaining a diagnosis of PTSD) and two continuous outcomes (assessor-rated and self-reported severity of PTSD symptoms). Among the main outcomes, the primary outcome was clinician-rated severity of PTSD symptoms, although this was not present for all studies.
Quantitative data synthesis
Where possible, meta-analysis was used to synthesise data, including additional meta-analyses for anxiety and depression measures where available, and numbers leaving the study early, using Review Manager. Post-treatment data (or change scores if reported instead of post-treatment data) for the psychological treatment and control condition were entered in the Review Manager tables. Dichotomous outcomes (PTSD diagnosis and leaving the study early for any reason) were analysed as a relative risk number and were calculated on an intention-to-treat basis (i.e. a ‘once randomised always analyse’ basis). This makes the conservative assumption that all participants who ceased to engage in the study had an unfavourable outcome, e.g. they left because the treatment was not acceptable and still had a diagnosis of PTSD. Continuous outcomes were analysed as standardised mean differences (SMDs) to allow for ease of comparison across studies. It was not possible to obtain intention-to-treat data for most of the trials, and we therefore used completer data for all continuous outcomes.
For consistency of presentation all data were entered into Review Manager in such a way that negative effect sizes or relative risk numbers less than 1 represented an effect that favoured the active treatment compared with the waiting-list control. Data were pooled from more than one study using a fixed-effects meta-analysis except where heterogeneity was present, in which case a random-effects model was used as described below.
Heterogeneity
To check for heterogeneity between studies, both the I 2-test of heterogeneity and the χ2-test of heterogeneity (P<0.10) as well as visual inspection of the forest plots were used. The I 2 statistic describes the proportion of total variation in study estimates that is due to heterogeneity (Reference Higgins and ThompsonHiggins & Thompson, 2002). An I 2 of less than 30% was taken to indicate mild heterogeneity and a fixed-effects model was used to synthesise the results. An I 2 of more than 50% was taken as notable heterogeneity; in this case an attempt was made to explain the variation. If studies with heterogeneous results were found to be comparable, a random-effects model was used to summarise the results (Reference DerSimonian and LairdDerSimonian & Laird, 1986). In the random-effects analysis, heterogeneity is accounted for both in the width of confidence intervals and in the estimate of the treatment effect. With decreasing heterogeneity the random-effects approach moves asymptotically towards a fixed-effects model. An I 2 of 30–50% was taken to indicate moderate heterogeneity. In this case, both the χ2-test of heterogeneity and a visual inspection of the forest plot were used to decide between a fixed- and random-effects model.
In order to explore heterogeneity further, sensitivity analyses were performed to consider the influence of higher-quality methodology (this was done by considering studies that used masked assessment, and those that used an intention-to-treat analysis), studies that only included females and those that only included Vietnam veterans.
Clinical effectiveness
Where psychological interventions were compared against waiting-list control groups an effect size (SMD) of –0.8 or less (e.g. a larger negative number) was considered clinically meaningful for continuous variables (a ‘large’ effect size; Reference CohenCohen, 1988) and for dichotomous outcomes a relative risk of 0.65 or less (or greater than 1.54) was considered clinically meaningful. Where two active treatments were compared lower thresholds were set with an SMD of –0.5 or +0.5 for continuous variables (a ‘medium’ effect size), and for dichotomous outcomes a relative risk of 0.80 or less or 1.25 or greater was considered clinically meaningful. These thresholds came from discussions in the NICE Guideline Development Group in advance of undertaking the meta-analyses and were based on clinical experience and thresholds used in the literature (Reference *Schnurr, Friedman and FoySchnurr et al, 2003). In order to be considered clinically meaningful the value had to meet the threshold criterion and the 95% confidence interval had to be greater than the threshold. If the SMD and relative risk met the threshold criterion but the 95% CI included values in the non-clinically significant range, this was interpreted as limited evidence for an effect. Similarly, if the SMD or relative risk value was below the threshold, the 95% CIs were examined to determine whether the evidence was inconclusive (in case the 95% CI included numbers greater than the threshold) or whether it could be stated that there was evidence suggesting that an effect was unlikely (where the 95% CI was entirely outside the clinically meaningful range).
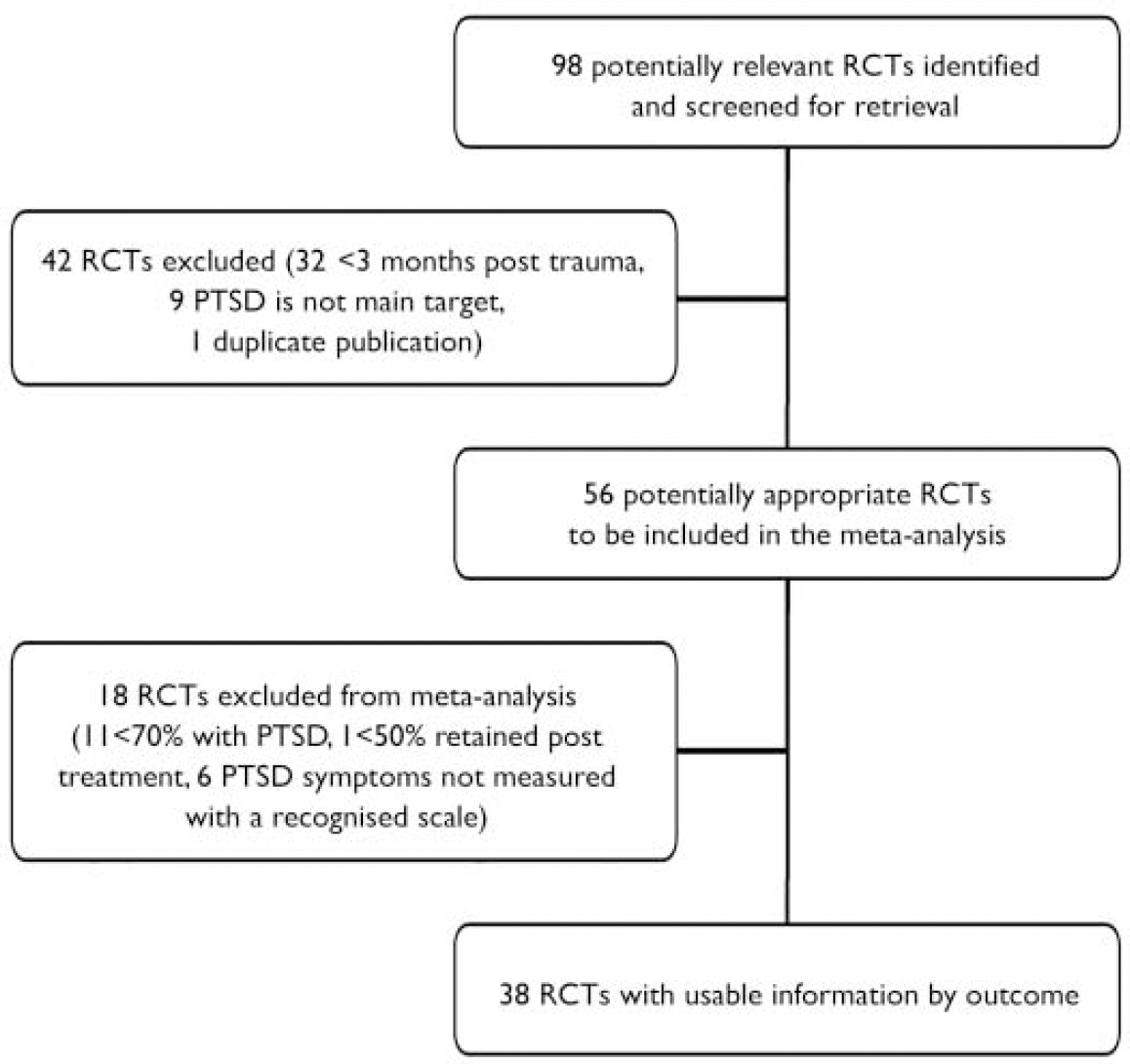
Fig. 1 Trial flow (PTSD, post-traumatic stress disorder; RCT, randomised controlled trial).
Psychological treatment categories
Five separate psychological treatment categories were defined (see Appendix). These came from discussions by the NICE Guideline Development Group in advance of undertaking the meta-analyses and were based on clinical experience and categories used in the literature (Reference Foa, Keane and FriedmanFoa et al, 2000).
RESULTS
Thirty-eight studies were included in the meta-analysis. Figure 1 shows the meta-analysis profile summarising trial flow.
Study characteristics
Details of the studies included appear in the data supplement to the online version of this article. Twenty-five studies compared trauma-focused cognitive–behavioural therapy (TFCBT) with waiting-list or other psychological interventions: Blanchard et al (Reference *Blanchard, Hickling and Devineni2003), Brom et al (Reference *Brom, Kleber and Defares1989), Bryant et al (Reference *Bryant, Moulds and Guthrie2003), Cloitre et al (Reference *Cloitre, Koenen and Cohen2002), Cooper & Clum (Reference *Cooper and Clum1989), Devilly & Spence (Reference *Devilly and Spence1999), Echeburua et al (Reference *Echeburua, de Corral and Zubizarreta1997), Ehlers et al (Reference *Ehlers, Clark and Hackmann2005), Fecteau & Nicki (Reference *Fecteau and Nicki1999), Foa et al (Reference *Foa, Rothbaum and Riggs1991, Reference *Foa, Dancu and Hembree1999), Gersons et al (Reference *Gersons, Carlier and Lamberts2000), Ironson et al (Reference *Ironson, Freund and Strauss2002), Keane et al (Reference *Keane, Fairbank and Caddell1989), Kubany et al (Reference *Kubany, Hill and Owens2003), Kubany et al (Reference *Kubany, Hill and Owens2004), Lee et al (Reference *Lee, Gavriel and Drummond2002), Marks et al (Reference *Marks, Lovell and Noshirvani1998), Paunovic & Ost (Reference *Paunovic and Ost2001), Peniston & Kulkosky (Reference *Peniston and Kulkosky1991), Power et al (Reference *Power, McGoldrick and Brown2002), Resick et al (Reference *Resick, Nishith and Weaver2002), Rothbaum et al (Reference *Rothbaum, Astin and Marsteller2005), Taylor et al (Reference *Taylor, Thordarson and Maxfield2003) and Vaughan et al (Reference *Vaughan, Armstrong and Gold1994). Twelve studies compared eye movement desensitisation and reprocessing (EMDR) with waiting-list or other psychological interventions: Carlson et al (Reference *Carlson, Chemtob and Rusnak1998), Devilly & Spence (Reference *Devilly and Spence1999), Ironson et al (Reference *Ironson, Freund and Strauss2002), Jensen (Reference *Jensen1994), Lee et al (Reference *Lee, Gavriel and Drummond2002), Marcus et al (Reference *Marcus, Marquis and Sakai1997), Power et al (Reference *Power, McGoldrick and Brown2002), Rothbaum (Reference *Rothbaum1997), Rothbaum et al (Reference *Rothbaum, Astin and Marsteller2005), Scheck et al (Reference *Scheck, Schaeffer and Gillette1998), Taylor et al (Reference *Taylor, Thordarson and Maxfield2003) and Vaughan et al (Reference *Vaughan, Armstrong and Gold1994). Seven studies compared stress management with waiting-list or other psychological interventions: Carlson et al (Reference *Carlson, Chemtob and Rusnak1998), Echeburua et al (Reference *Echeburua, de Corral and Zubizarreta1997), Foa et al (Reference *Foa, Rothbaum and Riggs1991, Reference *Foa, Dancu and Hembree1999), Marks et al (Reference *Marks, Lovell and Noshirvani1998), Taylor et al (Reference *Taylor, Thordarson and Maxfield2003) and Vaughan et al (Reference *Vaughan, Armstrong and Gold1994). Six studies compared ‘other therapies’ with waiting-list or other psychological interventions: Blanchard et al (Reference *Blanchard, Hickling and Devineni2003), Brom et al (Reference *Brom, Kleber and Defares1989), Bryant et al (Reference *Bryant, Moulds and Guthrie2003), Foa et al (Reference *Foa, Rothbaum and Riggs1991), Marcus et al (Reference *Marcus, Marquis and Sakai1997) and Scheck et al (Reference *Scheck, Schaeffer and Gillette1998). Four studies compared group cognitive–behavioural therapy with waiting-list or other psychological interventions: Classen et al (Reference *Classen, Butler and Koopman2001), Krakow et al (Reference *Krakow, Hollifield and Johnston2001), Schnurr et al (Reference *Schnurr, Friedman and Foy2003) and Zlotnick et al (Reference *Zlotnick, Shea and Rosen1997).
Two additional randomised controlled trials met inclusion criteria but differed in mode of delivery (Reference *Lange, Rietdijk and HudcovicovaLange et al, 2003; Reference *Neuner, Schauer and KlaschikNeuner et al, 2004), and one further trial compared two versions of TFCBT (exposure and cognitive therapy) with each other (Tarrier et al, Reference *Tarrier, Pilgrim and Sommerfield1999a ,Reference *Tarrier, Sommerfield and Pilgrim b ). These studies could not be included in the meta-analysis.
Quantitative data synthesis
Table 1 provides details of the quantitative data synthesis. It highlights that TFCBT and EMDR were better than waiting-list/control on most outcome measures. Stress management was better on some outcomes, and ‘other therapies’ appeared to be the least effective. Unfortunately none of the studies reported adverse effects and therefore it was not possible to analyse these. However, most studies did report withdrawal rates and these are included in Table 1.
Table 1 Summary of meta-analysis of comparisons of psychological treatments v. waiting list conditions

| Comparison | Clinician-rated PTSD symptoms | PTSD diagnosis (intent-to-treat) | Self-rated PTSD symptoms | Anxiety | Depression | Withdrawal rate |
|---|---|---|---|---|---|---|
| TFCBT v. waiting | T>W | T>W | T>W | (T>W) | T>W | (W>T) |
| list/usual care | 14 studies | 15 studies | 9 studies | 11 studies | 14 studies | 15 studies |
| n=649 | n=763 | n=428 | n=415 | n=625 | n=861 | |
| SMD=-1.40 | RR=0.44 | SMD=-1.70 | SMD=-0.99 | SMD=-1.26 | RR=1.42 | |
| (95% CI -1.89 to -0.91) | (95% CI 0.35 to 0.57) | (95% CI -2.17 to -1.24) | (95% CI -1.20 to -0.78) | (95% CI -1.69 to -0.82) | (95% CI 1.05 to 1.94) | |
| EMDR v. waiting | E>W | (E>W) | (E>W) | E>W | E>W | ? |
| list/usual care | 5 studies | 6 studies | 5 studies | 5 studies | 5 studies | 6 studies |
| n=162 | n=217 | n=156 | n=156 | n=160 | n=216 | |
| SMD=-1.51 | RR=0.49 | SMD=-1.13 | SMD=-1.20 | SMD=-1.48 | RR=1.21 | |
| (95% CI -1.87 to -1.15) | (95% CI 0.28 to 0.86) | (95% CI -2.13 to -0.13) | (95% CI -1.54 to -0.85) | (95% CI -1.84 to -1.12) | (95% CI 0.66 to 2.22) | |
| Stress management | (S>W) | (S>W) | ? | ? | ? | ? |
| v. waiting list/usual care | 3 studies | 4 studies | 1 study | 3 studies | 4 studies | 4 studies |
| n=86 | n=121 | n=24 | n=82 | n=109 | n=121 | |
| SMD=-1.14 | RR=0.64 | SMD=0.33 | SMD=-0.77 | SMD=-0.73 | RR=2.19 | |
| (95% CI -1.62 to -0.67) | (95% CI 0.47 to 0.87) | (95% CI -0.47 to 1.14) | (95% CI -1.23 to -0.31) | (95% CI -1.12 to -0.33) | (95% CI 0.71 to 6.73) | |
| Other therapies v. | ? | ? | (O>W) | (O>W) | ? | (W>O) |
| waiting list/usual care | 2 studies | 3 studies | 2 studies | 3 studies | 2 studies | 3 studies |
| n=72 | n=166 | n=132 | n=153 | n=72 | n=166 | |
| SMD=-0.43 | RR=0.79 | SMD=-0.61 | SMD=-0.48 | SMD=-0.25 | RR=3.82 | |
| (95% CI -0.9 to 0.04) | (95% CI 0.53 to 1.18) | (95% CI -0.98 to -0.24) | (95% CI -0.82 to -0.14) | (95% CI -0.71 to 0.22) | (95% CI 1.19 to 12.29) | |
| Group CBT v. waiting | ? | (GC>W) | ? | No data | No data | ? |
| list/usual care | 1 study | 1 study | 2 studies | 3 studies | ||
| n=97 | n=48 | n=71 | n=271 | |||
| SMD=-0.72 | RR=0.56 | SMD=-0.71 | RR=1.00 | |||
| (95% CI -1.14 to -0.31) | (95% CI 0.31 to 1.01) | (95% CI -1.2 to -0.22) | (95% CI 0.64 to 1.56) | |||
| EMDR v. TFCBT | (E=T) | ? | (E=T) | (E=T) | ? | ? |
| 6 studies | 7 studies | 7 studies | 4 studies | 7 studies | 8 studies | |
| n=187 | n=267 | n=206 | n=136 | n=206 | n=287 | |
| SMD=0.02 | RR=1.14 | SMD=-0.17 | SMD=-0.14 | SMD=-0.32 | RR=0.87 | |
| (95% CI -0.5 to 0.55) | (95% CI 0.70 to 1.85) | (95% CI -0.45 to 0.11) | (95% CI -0.48 to 0.20) | (95% CI -0.9 to 0.26) | (95% CI 0.58 to 1.30) | |
| TFCBT v. stress | ? | (T>S) | ? | (T=S) | ? | ? |
| management | 6 studies | 6 studies | 3 studies | 4 studies | 5 studies | 6 studies |
| n=239 | n=284 | n=127 | n=127 | n=161 | n=284 | |
| SMD=-0.27 | RR=0.78 | SMD=-0.37 | SMD=-0.12 | SMD=-0.25 | RR=1.17 | |
| (95% CI -0.71 to 0.16) | (95% CI 0.61 to 0.99) | (95% CI -0.74 to 0.01) | (95% CI -0.49 to 0.26) | (95% CI -0.57 to 0.08) | (95% CI 0.69 to 2.0) | |
| TFCBT v. other | (T>O) | (T>O) | (T>O) | ? | (T>O) | ? |
| therapies | 3 studies | 5 studies | 3 studies | 4 studies | 3 studies | 5 studies |
| n=120 | n=286 | n=176 | n=197 | n=120 | n=290 | |
| SMD=-0.81 | RR=0.71 | SMD=-1.18 | SMD=-0.47 | SMD=-0.65 | RR=1.14 | |
| (95% CI -1.19 to -0.42) | (95% CI 0.56 to 0.89) | (95% CI -2.32 to -0.03) | (95% CI -1.11 to 0.17) | (95% CI -1.03 to -0.28) | (95% CI 0.68 to 1.90) | |
| EMDR v. stress | ? | (E>S) | ? | (E>S) | (E>S) | ? |
| management | 2 studies | 3 studies | 3 studies | 2 studies | 3 studies | 3 studies |
| n=53 | n=84 | n=75 | n=45 | n=75 | n=84 | |
| SMD=-0.35 | RR=0.69 | SMD=-0.40 | SMD=-0.75 | SMD=-0.67 | RR=1.03 | |
| (95% CI -0.90 to 0.19) | (95% CI 0.46 to 1.04) | (95% CI -0.86 to 0.06) | (95% CI -1.36 to -0.13) | (95% CI -1.14 to -0.20) | (95% CI 0.37 to 2.88) | |
| EMDR v. other | No data | (E>O) | (T>O) | (T>O) | (T>O) | (O>T) |
| therapies | 1 study | 2 studies | 2 studies | 2 studies | 2 studies | |
| n=67 | n=124 | n=126 | n=127 | n=127 | ||
| RR=0.4 | SMD=-0.84 | SMD=-0.72 | SMD=-0.67 | RR=1.48 | ||
| (95% CI 0.19 to 0.84) | (95% CI -1.21 to -0.47) | (95% CI -1.08 to -0.36) | (95% CI -1.03 to -0.32) | (95% CI 0.26 to 8.54) | ||
| Stress management | (S>O) | ? | No data | ? | ? | ? |
| v. other therapies | 1 study | 1 study | 1 study | 1 study | 1 study | |
| n=25 | n=31 | n=25 | n=25 | n=31 | ||
| SMD=-1.22 | RR=0.58 | SMD=-0.51 | RR=-0.51 | RR=0.82 | ||
| (95% CI -2.09 to -0.35) | (95% CI 0.30 to 1.11) | (95% CI -1.32 to 0.29) | (95% CI -1.31 to 0.30) | (95% CI 0.2 to 3.46) | ||
| Group TFCBT | (GT=GC) | (GT=GC) | No data | No data | No data | (GC>GT) |
| v. group CBT | 1 study | 1 study | 1 study | |||
| (non-trauma-focused) | n=325 | n=360 | n=360 | |||
| SMD=-0.12 | RR=0.98 | RR=1.38 | ||||
| (95% CI -0.34 to 0.1) | (95% CI 0.83 to 1.16) | (95% CI 1.00 to 1.90) |
Sensitivity analyses
Masked assessment
The EMDR studies using masked assessment showed evidence favouring EMDR over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (three studies, n=120; SMD=–1.54, 1.54, 95% CI –1.95 to –1.12) similar to that in all EMDR studies (see Table 1). The TFCBT studies using masked assessment showed evidence favouring TFCBT over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (seven studies, n=308; SMD=–1.70; 95% CI –2.47 to –0.93) similar to that in all TFCBT studies.
Vietnam veteran studies
One EMDR study considered only Vietnam veterans. This showed less evidence favouring EMDR over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (one study, n=25; SMD=–0.97, 95% CI –1.81 to –0.13) than the other EMDR studies (see Table 1). One TFCBT study considered only Vietnam veterans using the primary outcome measure; this showed less evidence favouring TFCBT over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (one study, n=24; SMD=–0.22, 95% CI –1.03 to 0.58) than the other TFCBT studies.
Female studies
The EMDR studies including only female participants showed evidence favouring EMDR over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (two studies, n=57; SMD= –1.67, 95% CI –2.30 to –1.04) similar to that in all EMDR studies. The TFCBT studies including only female participants showed more evidence favouring TFCBT over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (six studies, n=358; SMD=–2.06, 95% CI –2.70 to –1.42) than all TFCBT studies.
Intention-to-treat analysis
None of the EMDR studies reported using an intention-to-treat analysis so this could not be assessed. The TFCBT studies using an intention-to-treat analysis showed more evidence favouring TFCBT over waiting-list on reducing the severity of PTSD symptoms (clinician-rated measures) (six studies, n=332; SMD=–1.82, 95% CI –2.76 to –0.89) than all TFCBT studies.
DISCUSSION
We identified 38 randomised controlled trials of psychological treatments for PTSD. Trauma-focused cognitive–behavioural therapy showed clinically important benefits over waiting-list or usual care on all measures of PTSD symptoms. In addition, there was limited evidence that it also has clinically important effects on depression and anxiety. The effectiveness of eye movement desensitisation and reprocessing was also generally supported by the meta-analysis, but the evidence base was not as strong as that for TFCBT, both in terms of the number of trials available and the certainty with which clinical benefit was established. Furthermore, there was limited evidence that TFCBT and EMDR were superior to supportive/non-directive treatments, hence it is highly unlikely that their effectiveness is due to non-specific factors such as attention. There was limited evidence for stress management and group cognitive–behavioural therapy, but ‘other therapy’ (supportive/non-directive therapy, psychodynamic therapies and hypnotherapies) that focused on current or past aspects of the patient's life other than the trauma or on general support did not show clinically important effects on PTSD symptoms, depression or anxiety. However, this might be due to the limited number of studies available and does not mean that these treatments were shown to be ineffective.
The treatments most supported by the review (individually delivered TFCBT and EMDR) are both trauma-focused psychological treatments that specifically address the patient's troubling memories of the traumatic event and the personal meanings of the event and its consequences. Direct comparisons of these two approaches did not reveal any significant advantages of one over the other, with respect to either treatment outcome or speed of therapeutic change (Reference *Taylor, Thordarson and MaxfieldTaylor et al, 2003).
Heterogeneity
There is clearly considerable clinical diversity within the studies considered. The separation of different active interventions into groups partially addresses their impact on clinical diversity, but not all trials within the same group used identical interventions. The differences were most marked in the ‘other therapy’ group, which had in common the absence of cognitive–behavioural techniques and trauma-focused work. There was also diversity in the TFCBT group, which included both exposure-only and trauma-focused cognitive therapy interventions.
Another source of heterogeneity was the quality of the studies. Sensitivity analyses of higher-quality and lower-quality studies were performed to explore this further. There was some limited evidence that higher-quality studies (those including masked assessment of outcome or intention-to-treat analysis) showed better outcomes than the lower-quality studies. This finding contradicts previous research (Reference Moher, Pharn and JonesMoher et al, 1998) that has found an association between poorer methodology and more favourable results for the intervention. It may reflect the fact that the better studies tended to be more recent and associated with refinement of techniques. They also included most of the female-only studies. The fact that female-only studies showed a better response to TFCBT than mixed studies and male-only studies is difficult to interpret. It may be that the female-only studies used more effective interventions, that the trauma of rape is more amenable than other traumas to effective TFCBT, or that for some undetermined reason women are more responsive to TFCBT than men. Interestingly, a similar superiority in female response has been found for pharmacological treatment of PTSD (National Collaborating Centre for Mental Health, 2005). The finding that studies including only Vietnam veterans produced worse responses to TFCBT and EMDR might have contributed to the female studies finding and also suggests that Vietnam veterans are a particularly difficult population to treat.
As with all psychological treatment trials, there are issues with the control group. The development of a psychological treatment placebo is difficult, if not impossible, as is masking of participants and therapists. In several of the waiting-list or usual care conditions it was apparent that some (usually poorly defined) treatment was going on. The main effect of this is likely to have made it more difficult for the active intervention to show itself to be superior to the control condition.
Tolerability
Unfortunately none of the studies reported adverse effects. It remains unclear whether no adverse effects occurred, or whether they were not described. This is a key short-coming in the trials identified. Most studies reported withdrawals by group. There are likely to be several different factors that determine withdrawal rates, including the tolerability of the intervention. There was limited evidence that TFCBT and other therapies fared worse than waiting-list or usual care on this outcome measure, but there was no significant difference in withdrawal rates in direct comparisons between any of the active treatments. The higher-quality TFCBT studies showed no difference in withdrawal rates when compared with waiting-list or usual care. Some people find it difficult to fully engage in psychological treatment because it requires a significant commitment of time and emotion. For some people with PTSD it may initially be difficult and overwhelming to disclose details of their traumatic events. It is also well recognised that some patients may be subject to initial adverse effects such as increased re-experiencing following exposure treatment (Reference Pitman, Altman and GreenwaldPitman et al, 1991; Reference Foa, Zoellner and FeenyFoa et al, 2002; Reference Hackmann, Ehlers and SpeckensHackmann et al, 2004). Withdrawal rates of up to 30% in some studies suggest that the active treatments were not always acceptable to those receiving them. It is possible that in these cases devoting several sessions to establishing a trusting therapeutic relationship and emotional stabilisation, before addressing the traumatic event, might lead to greater acceptability.
Limitations of the meta-analysis
Although this meta-analysis provides a systematic and comprehensive comparison of the different psychological treatments of PTSD, it is not without methodological problems. The randomised controlled trials analysed usually reported unadjusted means for the treatment conditions after therapy and at follow-up. Sample sizes were usually small, raising the chance that baseline differences present before treatment influenced scores after treatment. Indeed, some studies showed baseline differences between the study conditions that remained uncorrected in our analysis. However, across studies no systematic baseline difference existed, so the conclusions remain valid. Furthermore, the Review Manager program does not allow entering a score of 0 for both groups. Thus, the withdrawal rates reported are slight overestimates of the true rates.
Clinical implications
Our results suggest that trauma-focused psychological treatments (TFCBT or EMDR) are effective for chronic PTSD. Indeed, the effect sizes compare favourably with those found for cognitive–behavioural therapy in depressive and anxiety disorders (National Collaborating Centre for Mental Health, 2004; National Collaborating Centre for Primary Care, 2004). These treatments are normally delivered on an individual out-patient basis over 8–12 sessions. A course of trauma-focused psychological treatment should be offered to everyone with chronic PTSD. The results also suggest that not all chronic PTSD will benefit from these treatments; other approaches should then be considered, including extending the number of sessions, trying an alternative form of trauma-focused psychological treatment and the augmentation of trauma-focused psychological treatment with a course of pharmacological treatment. A recent meta-analysis has suggested that pharmacological interventions are unlikely to be as clinically effective as trauma-focused psychological interventions and should therefore be used as a second-line treatment (National Collaborating Centre for Mental Health, 2005).
Future research
Further well-designed trials of psychological treatments are required, including further comparison studies of one type of psychological treatment against another. There is a need for large-scale studies (phase 4) to find out whether the results will survive in real practice. Future trials should consider adverse events and tolerability of treatment in more detail. Our results suggest that several of the currently available treatments might benefit from modifications that would make them more acceptable to people with chronic PTSD and possibly also more effective. There is also potential for research concerning the direct comparison of psychological treatments with pharmacological treatments, the effectiveness of a combination of the two, and the implications of the high degree of comorbidity with other disorders for the choice of treatment.
APPENDIX
Psychological treatment categories
Treatments delivered on an individual basis that focused on the memory for the traumatic event and its meaning
-
1. Trauma-focused cognitive–behavioural therapy (TFCBT).
-
2. Eye movement desensitisation and reprocessing (EMDR).
Treatments delivered on an individual basis that do not place the main focus of treatment on the trauma
-
3. Stress management and relaxation.
-
4. Other therapies (including supportive therapy/non-directive non-directive counselling, psychodynamic therapies and hypnotherapy).
Treatments delivered in groups
5. Group cognitive–behavioural therapy.





eLetters
No eLetters have been published for this article.