Approximately half of the world's countries have been affected by war or open conflict in the past three decades. Reference Pettersson and Wallensteen1,Reference Marshall and Cole2 Most war casualties are civilians, Reference Bartov3 and the overwhelming majority of them live in low- and middle-income countries (LMICs). Reference Brundtland4 Post-traumatic stress disorder (PTSD) and depression are the most prevalent mental disorders in war-affected communities, and the prevalence rates of these conditions are significantly higher in such communities than in communities with no recent history of open conflict. Reference Steel, Chey, Silove, Marnane, Bryant and van Ommeren5,Reference Priebe, Bogic, Ajdukovic, Franciskovic, Galeazzi and Kucukalic6 This pattern applies to both adults and children, with more than 80% of the world's population of young people living in LMICs. PTSD is associated with mental and physical dysfunction, Reference Nemeroff, Bremner, Foa, Mayberg, North and Stein7 is chronic if untreated, Reference Morina, Wicherts, Lobbrecht and Priebe8 and contributes significantly to the burden of disease. Reference Kessler, Aguilar-Gaxiola, Alonso, Chatterji, Lee and Ormel9 As a result, mitigating the effects of trauma and adversity has become a major global public health issue. Reference Collins, Patel, Joestl, March, Insel and Daar10–Reference Belfer, Remschmidt, Nurcombe, Okasha, Sartorius, Remschmidt, Nurcombe, Belfer, Sartorius and Okasha12 The challenges for implementing evidence-based interventions in LMICs include insufficient mental health services, inadequately qualified practitioners to deliver interventions and impediments to adapting established interventions to the needs of LMIC contexts. Reference Morina, Rushiti, Salihu and Ford13 Numerous controlled trials of psychological interventions for mental health problems in children and youths following mass violence have been conducted in LMICs. A meta-analysis by Tol et al in 2011 that included four randomised controlled trials (RCTs) in children and adolescents exposed to mass traumatic events produced small effects on PTSD when psychosocial interventions were compared with waiting list or usual care. Reference Tol, Barbui, Galappatti, Silove, Betancourt and Souza14 These authors further concluded that the analysed trials had serious limitations in study design. Our aim was to survey the published literature on psychological interventions for children and young people in LMICs affected by mass violence to provide an updated meta-analytic review of the effects of psychological interventions on PTSD and depression symptoms.
Method
We defined the main structured research question describing the Population, Intervention, Comparison, Outcome and Study (PICOS) design in accordance with the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) group. 15 Our aim was to elucidate whether psychological treatment of children and adolescents improved war-related PTSD and/or depression symptoms compared with control conditions in RCTs.
Identification and selection of studies
Our inclusion criteria were that the study was conducted in an LMIC with survivors of mass violence who were 19 years old or younger, assignment to treatment conditions was random and at least 10 participants completed a psychological treatment aimed at reducing PTSD or depression (or both). No restriction was made as to intervention format, publication type, year of publication or publication language. A trial was excluded if the majority of participants were older than 19 years. If publications did not provide sufficient data for meta-analysis, the authors were contacted by email up to twice to retrieve these data. A trial was labelled as being conducted with survivors of mass violence if the conflict in question had taken place in a country that was listed as a war-affected country by the Uppsala Conflict Data Program. Reference Pettersson and Wallensteen1,16 This database defines wars as mass conflicts that generate 1000 or more battle-related deaths in one calendar year. We searched the PsycINFO, Medline and PILOTS databases to 9 July 2016. The following search terms were used in the fields ‘title’, ‘abstract’ and ‘key concepts’: posttraumatic stress OR PTSD OR depress* OR MDD AND genocide or war* OR prisoners of war OR mass violence OR mass conflict* OR post-conflict* OR political conflict* OR armed conflict* OR ethnic cleansing OR terrorism OR torture OR persecution OR civilian* AND treatment* OR intervention* OR therapy OR psychotherapy OR exposure OR trial. Additionally, reference lists of included publications and other relevant reviews were examined to retrieve additional studies.
Two authors (N.M. and M.M.) coded and extracted from each study the treatment target (PTSD or depression or both); number of participants; comparison group; type of outcome measure used (self-report measurement or structured interview); intervention format (individual or group); therapist (trained lay or professional therapist); type of intervention; number of sessions; country; and gender. If reported, scores of general function impairment were also coded and extracted. The pre-treatment, post-treatment and follow-up assessment mean and standard deviation scores and/or mean and standard deviation change scores for each outcome measure also were recorded. If mean age or gender proportions were not reported separately for each condition, the reported average data were used for all conditions.
Quality assessment
The Cochrane Collaboration's tool for assessing risk of bias was used for evaluating the quality of the studies regarding selection bias (random sequence generation and allocation concealment), detection bias, attrition bias, reporting bias and other sources of bias. Reference Higgins, Altman, Sterne, Higgins and Green17 Risk of bias in each domain was classified as low, high or unclear. Two raters independently rated all studies.
Coding of treatment characteristics
Treatment interventions were first coded as either ‘active treatment’ or ‘control group’. Next, active treatments were subdivided into trauma-focused cognitive–behavioural therapy (CBT), treatments mainly focusing on the memory of the trauma and/or its meaning; CBT without a main focus on the traumatic memory; multidisciplinary treatment (treatments including intervention techniques from different therapeutic approaches); classroom-based interventions for students; interpersonal psychotherapy; and meditation. Control conditions were subdivided into waiting-list or non-active controls and active control conditions. Active control conditions consisted of supportive counselling, creative play or treatment as usual (TAU). Finally, all active treatments were categorised according to whether they were delivered as individual or group treatment.
Statistical analysis
Intention-to-treat (ITT) samples were used when available (nine publications) and completer samples were used if ITT samples were not provided (nine publications). Given the limited number of controlled trials meeting our criteria, we found it informative first to compute within-group effect sizes for the impact of treatment on PTSD symptoms (i.e. change from pre-treatment to post-treatment and follow-up, respectively). However, as uncontrolled effect sizes do not account for the impact of time on symptoms, we viewed controlled effect sizes as more robust for assessing the efficacy of treatment effect. For uncontrolled effect sizes the post-treatment or follow-up mean was subtracted from the pre-treatment mean, and for controlled effect sizes the control group mean was subtracted from the treatment group mean at post-treatment or follow-up and divided by the pooled standard deviation. Subsequently, to obtain the effect size Hedges' g, the outcome was multiplied by a sample size correction factor J = 1-(3/(4d.f.−1)). Reference Lipsey and Wilson18 Subgroup analyses were conducted if a specific group of interventions consisted of at least four trials. As experimental conditions were mostly compared with waiting-list conditions, we separately analysed the overall effect of waiting-list control groups. Analyses were completed with Comprehensive Meta-Analysis version 3, using the random effects model to calculate effect sizes given the heterogeneity of the studies. Reference Borenstein, Hedges, Higgins and Rothstein19,Reference Field and Gillett20 Effect sizes may be conservatively interpreted with Cohen's convention of small (0.2), medium (0.5) and large (0.8) effects. Reference Cohen21 To test homogeneity of effect sizes we calculated the Q-statistic and the I 2 statistic which is an indicator of heterogeneity in percentages, with higher percentages indicating high heterogeneity. The risk of publication bias was assessed for the primary outcome measures through visual inspection of the funnel plot (for analyses including more than nine trials) and by examining the relation between effect and sample sizes, with relatively higher effect sizes of smaller studies being an indicator of publication bias. Reference Sterne, Sutton, Ioannidis, Terrin, Jones and Lau22 Furthermore, we calculated the likely number of missing studies using Duval & Tweedie's trim and fill procedure, Reference Duval and Tweedie23 which yields an estimate of the effect size after publication bias has been taken into account.
Results
In total 21 studies fulfilled our criteria (Fig. 1, Table 1). Nineteen studies were published in peer-reviewed journals, Reference Betancourt, McBain, Newnham, Akinsulure-Smith, Brennan and Weisz24–Reference Tol, Komproe, Jordans, Ndayisaba, Ntamutumba and Sipsma42 one was a book, Reference Khamis, Macy and Coignez43 and one a doctoral thesis. Reference Schauer44 All publications were in English. Nineteen publications reported on PTSD symptoms and 11 on depression symptoms. Most trials targeted both PTSD and depression (k = 10) and the remaining studies targeted either PTSD alone (k = 10) or depression (k = 1) alone. In total, 3444 treated participants and 1068 participants in a waiting-list condition were included in the analyses. In the 21 trials, 28 and 16 treatment arms targeted symptoms of PTSD and depression, respectively (Table 1). The difference between the number of trials and the number of interventions results from the fact that some trials assessed the efficacy of more than one active intervention. Active treatments were compared with waiting-list groups 13 and 8 times in relation to PTSD and depression symptoms, respectively. The number of participants per condition varied from 12 to 380, with a mean of 102.5 (s.d. = 91.0). The mean age of participants was 13.4 years (s.d. = 1.7) and half of the participants were female. Fifteen trials were conducted with children, four with adolescent participants and two with both groups combined. Of the trials focusing on both PTSD and depression, three reported treatment of PTSD as the major focus and additionally measured the efficacy of the intervention for depression among individuals with PTSD. Reference Ertl, Pfeiffer, Schauer, Elbert and Neuner27,Reference Schaal, Elbert and Neuner39,Reference Schauer44 The remaining seven had a general focus on treating war-related psychopathologic symptoms and focused on both PTSD and depression.
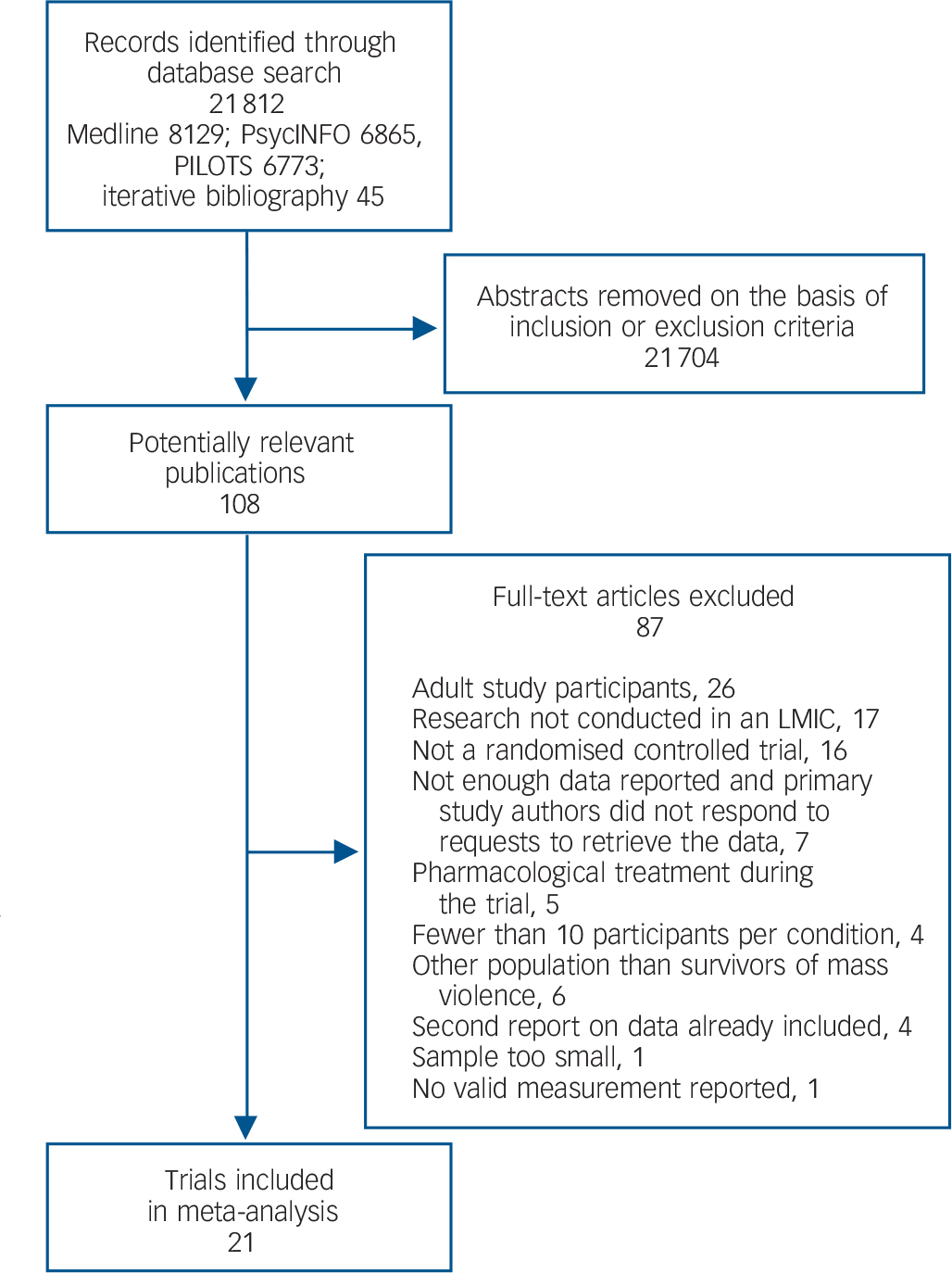
Fig. 1 Study selection process. LMIC, low- to middle-income country.
Table 1 Overview of included trials
| Study, type of treatment, number of sessions |
n used in pre- post analyses |
Country | Primary outcome | Follow-up (months) |
Modality | Age group | Treatment focus | Analysis | Diagnosis (%) at pre-treatment | |
|---|---|---|---|---|---|---|---|---|---|---|
| PTSD | Depression | |||||||||
| Betancourt et al (2014) Reference Betancourt, McBain, Newnham, Akinsulure-Smith, Brennan and Weisz24 | ||||||||||
| CBT (10 sessions) | 222 | Sierra Leone | UPID | 6 | Group | Adolescent, young adult |
General mental health including PTSD |
ITT | NR | NA |
| TAU (NR) | 214 | |||||||||
| Bolton et al (2007) Reference Bolton, Bass, Betancourt, Speelman, Onyango and Clougherty25 | ||||||||||
| IPT (16 sessions) | 105 | Uganda | APAI | NR | Group | Child | Depression only | ITT | NA | NR |
| CP (NR) | 105 | |||||||||
| WL | 104 | |||||||||
| Catani et al (2009) Reference Catani, Kohiladevy, Ruf, Schauer, Elbert and Neuner26 | ||||||||||
| TFCBT (6 sessions) | 16 | Sri Lanka | UPID | 6 | Individual | Child | PTSD only | ITT | 100 | NA |
| MED (6 sessions) | 15 | NR | ||||||||
| Ertl et al (2011) Reference Ertl, Pfeiffer, Schauer, Elbert and Neuner27 | ||||||||||
| TFCBT (8 sessions) | 29 | Uganda | CAPS | 12 | Individual | Adolescent | PTSD a | ITT | 100 | 24 |
| SC (NR) | 28 | |||||||||
| WL | 28 | |||||||||
| Gordon et al (2008) Reference Gordon, Staples, Blyta, Bytyqi and Wilson28 | ||||||||||
| MED (12 sessions) | 38 | Kosovo | HTQ | 3 | Group | Adolescent | PTSD only | Compl. | 100 | NA |
| WL | 40 | |||||||||
| Hermenau et al (2013) Reference Hermenau, Hecker, Schaal, Maedl and Elbert29 | ||||||||||
| TFCBT (6 sessions) | 15 | Congo | PSS-I | 6 | Individual | Child | PTSD only | Compl. | NR | NA |
| WL | 15 | |||||||||
| Jordans et al (2010) Reference Jordans, Komproe, Tol, Kohrt, Luitel and Macy30 | ||||||||||
| CBI (15 sessions) | 164 | Nepal | CPSS | NR | Group | Child | PTSD, depression | ITT | NA | NR |
| WL | 161 | |||||||||
| Khamis et al (2004) Reference Khamis, Macy and Coignez43 | ||||||||||
| CBI (15 sessions) | 380 | Palestine | IES | NR | Group | Child, adolescent | PTSD only | Compl. | NR | NA |
| WL | 284 | |||||||||
| Layne et al (2008) Reference Layne, Saltzman, Poppleton, Burlingame, Pasalic and Durakovic31 | ||||||||||
| CBI (18 sessions) | 66 | Bosnia | UPID | 4 | Group | Adolescent | PTSD, depression | Compl. | NA | NR |
| SC (18 sessions) | 61 | |||||||||
| McMullen et al (2013) Reference McMullen, O'Callaghan, Shannon, Black and Eakin32 | ||||||||||
| TFCBT (13 sessions) | 24 | Congo | UPID | 3 | Group | Child | PTSD only | Compl. | NR | NA |
| WL | 24 | |||||||||
| Murray et al (2015) Reference Murray, Skavenski, Kane, Mayeya, Dorsey and Cohen33 | ||||||||||
| TFCBT (16 sessions) | 131 | Zambia | UPID | NR | Individual | Child, adolescent | PTSD only | ITT | NR | NA |
| TAU (NR) | 126 | |||||||||
| O'Callaghan et al (2013) Reference O'Callaghan, McMullen, Shannon, Rafferty and Black34 | ||||||||||
| TFCBT (15 sessions) | 24 | Congo | UPID | 3 | Group | Child | PTSD only | ITT | 60 | NA |
| WL | 28 | |||||||||
| O'Callaghan et al (2014) Reference O'Callaghan, Branham, Shannon, Betancourt, Dempster and McMullen35 | ||||||||||
| MDT (8 sessions) | 78 | Congo | CRIES | 3 | Group | Child | PTSD only | Compl. | 16 | NA |
| WL | 80 | |||||||||
| O'Callaghan et al (2015) Reference O'Callaghan, McMullen, Shannon and Rafferty36 | ||||||||||
| TFCBT (9 sessions) | 26 | Congo | UPID | 6 | Group | Child | PTSD only | Compl. | 92 | NA |
| MDT (9 sessions) | 24 | |||||||||
| Peltonen et al (2012) Reference Peltonen, Qouta, El Sarraj and Punamaki37 | ||||||||||
| CBI (NR) | 108 | Palestine | CPTS-RI | NR | Group | Child | PTSD, depression | Compl. | 45 | 54 |
| WL | 64 | |||||||||
| Qouta et al (2012) Reference Qouta, Palosaari, Diab and Punamaki38 | ||||||||||
| MDT (8 sessions) | 242 | Palestine | CRIES | 6 | Group | Child | PTSD, depression | ITT | 64 | NR |
| WL | 240 | |||||||||
| Schaal et al (2009) Reference Schaal, Elbert and Neuner39 | ||||||||||
| TFCBT (4sessions) | 12 | Rwanda | CAPS | 6 | Individual | Adolescent | PTSD a | ITT | 100 | 80 |
| IPT (4 sessions) | 14 | Group | ||||||||
| Schauer (2008) Reference Schauer44 | ||||||||||
| TFCBT (6 sessions) | 24 | Sri Lanka | CAPS | NR | Individual | Child | PTSD a | Compl. | 100 | 29 |
| MED (6 sessions) | 22 | Unclear | ||||||||
| Tol et al (2008) Reference Tol, Komproe, Susanty, Jordans, Macy and De Jong40 | ||||||||||
| CBI (15 sessions) | 182 | Indonesia | CPSS | 6 | Group | Child | PTSD, depression | ITT | NR | NR |
| WL | 221 | |||||||||
| Tol et al (2012) Reference Tol, Komproe, Jordans, Vallipuram, Sipsma and Sivayokan41 | ||||||||||
| CBI (15 sessions) | 199 | Sri-Lanka | CPSS | 3 | Group | Child | PTSD, depression | Compl. | NR | NR |
| WL | 200 | |||||||||
| Tol et al (2014) Reference Tol, Komproe, Jordans, Ndayisaba, Ntamutumba and Sipsma42 | ||||||||||
| CBI (15 sessions) | 153 | Burundi | CPSS | 3 | Group | Child | PTSD, depression | ITT | NR | NR |
| WL | 176 | |||||||||
APAI, Acholi Psychosocial Assessment Instrument; CAPS, Clinician Administered PTSD Scale; CBI, classroom-based intervention; CBT, cognitive–behavioural therapy; CDI, Child Depression Inventory; compl., completers; CP, creative play; CPTS-RI, Child Post Traumatic Stress Reaction Index; CPSS, Child PTSD Symptom scale; CRIES, Children's Revised Impact of Event Scale; HTQ, Harvard Trauma Questionnaire; IES, Impact of Event Scale; IPT, interpersonal psychotherapy; ITT, intention to treat; MDT, multidisciplinary treatment; MED, meditation/relaxation; NA, not applicable; NR, not reported; PSS-I, Posttraumatic Symptom Scale – Interview; SC, supportive counselling; TAU, treatment as usual; TFCBT, trauma-focused cognitive–behavioural therapy; UPID, university of California – Los Angeles Posttraumatic Stress Disorder Reaction Index; WL, waiting list.
a. Depression was not reported as being a main treatment target.
Both structured clinical interviews and self-report scales were used as primary outcome measures. All primary outcome measures provided continuous data. With regard to the 20 trials assessing PTSD, structured clinical interviews were used in four trials and self-report scales in the remaining 16 trials. However, self-report measures were mostly administered as interviews rather than completed by the participant. For the assessment of depression, structural clinical interviews were used in four trials, self-report measures administered as interviews in five trials, and self-reports filled out by the participant in two trials.
Ten studies reported the number of participants fulfilling diagnostic criteria for PTSD at the pre-treatment assessment and four studies reported those with depression. With regard to PTSD, five trials reported that all participants had PTSD at pre-treatment assessment and five studies reported prevalence rates of 45–92% (see Table 1). For depression the reported prevalence among the four studies in question ranged between 21% and 80%. The number of treatment sessions implemented ranged from 4 to 18 (median 11.5, s.d. = 4.3). Trauma-focused CBT interventions were associated with a lower mean number of treatment sessions. In fact, all interventions with six or fewer sessions were trauma-focused CBT interventions conducted by the same group. Accordingly, the number of treatment sessions could not be used in subanalyses. Similarly, all but one of the trials of therapy conducted on an individual basis were conducted by the same group, and thus we refrained from comparing individual treatments with group treatments. The interventions were mainly conducted by non-psychotherapists who were trained for the purpose of the study, with only three trials making use of professionals to conduct the treatment. Reference Hermenau, Hecker, Schaal, Maedl and Elbert29,Reference Qouta, Palosaari, Diab and Punamaki38,Reference Schaal, Elbert and Neuner39 Interventions were mostly conducted in groups, with only six trials being implemented on an individual basis. Follow-up duration ranged from 3 months to 12 months. Given the limited number of included trials, all follow-up assessments regardless of the time of assessment were entered as one group in the meta-analysis.
Effects on PTSD
Uncontrolled effect sizes
Across all active interventions (k = 22) a large aggregated pre–post effect size was found: g = 1.15, 95% CI 0.82–1.48. With regard to uncontrolled effect sizes relating to the change from pre-treatment to follow-up, results showed large effect sizes across active treatments: g = 1.28, 95% CI 0.98–1.57, k = 16 (Table 2).
Table 2 Subgroup analysis (Hedges' g): within-group effect sizes
| Pre- v. post-treatment | Pre-treatment v. follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| k a | g | s.e. | 95% CI | k | g | s.e. | 95% CI | |
| PTSD | ||||||||
| Active intervention b | 22 | 1.15 | 0.17 | 0.82 to 1.48 | 16 | 1.28 | 0.15 | 0.98 to 1.57 |
| TFCBT | 9 | 1.75 | 0.37 | 1.02 to 2.48 | 6 | 1.91 | 0.44 | 1.05 to 2.77 |
| CBI | 6 | 0.32 | 0.24 | −0.16 to 0.80 | 4 | 0.98 | 0.21 | 0.57 to 1.39 |
| Other c | 7 | 1.20 | 0.23 | 0.75 to 1.65 | 6 | 1.19 | 0.29 | 0.62 to 1.75 |
| WL | 12 | 0.17 | 0.09 | −0.01 to 0.35 | 6 | 0.47 | 0.14 | 0.20 to 0.7 |
| Depression | ||||||||
| Active intervention | 12 | 0.30 | 0.12 | 0.08 to 0.53 | 8 | 0.52 | 0.15 | 0.22 to 0.82 |
| TFCBT | NA | NA | ||||||
| CBI | 5 | 0.24 | 0.11 | 0.02 to 0.46 | 4 | 0.48 | 0.13 | 0.23 to 0.73 |
| Other | 4 | 0.48 | 0.38 | −0.26 to 1.23 | NA | |||
| WL | 6 | −0.19 | 0.11 | −0.39 to 0.02 | 5 | 0.16 | 0.14 | −0.11 to 0.43 |
CBI, classroom-based intervention; NA, not applicable – number of trials too small (k<4) to conduct analysis; PTSD, post-traumatic stress disorder; TFCBT, trauma-focused cognitive–behavioural therapy; WL, waiting-list.
a. Number of treatment arms.
b. All active interventions excluding supportive counselling, creative play and treatment as usual.
c. Interpersonal psychotherapy, multidisciplinary treatment and meditation.
Controlled effect sizes
The aggregated between-group effect size comparing active treatments v. control conditions at post-treatment (k = 16) was medium: g = 0.57, 95% CI 0.27–0.88. The comparison between active conditions with waiting-list only (k = 12) produced a medium effect size: g = 0.53, 95% CI 0.25–0.81 (Fig. 2, Table 3). The aggregated between-group effect size comparing active treatments with control conditions at follow-up was small: g = 0.23, 95% CI 0.05–0.41 (k = 9). Four trials compared trauma-focused CBT with other active conditions at post-treatment (interpersonal psychotherapy, multidisciplinary treatment and meditation), Reference Ertl, Pfeiffer, Schauer, Elbert and Neuner27,Reference Hermenau, Hecker, Schaal, Maedl and Elbert29,Reference Layne, Saltzman, Poppleton, Burlingame, Pasalic and Durakovic31,Reference Schaal, Elbert and Neuner39 and results showed no difference between these interventions: g = 0.05, 95% CI −0.26 to 0.36. At follow-up only three studies compared trauma-focused CBT with other active conditions.
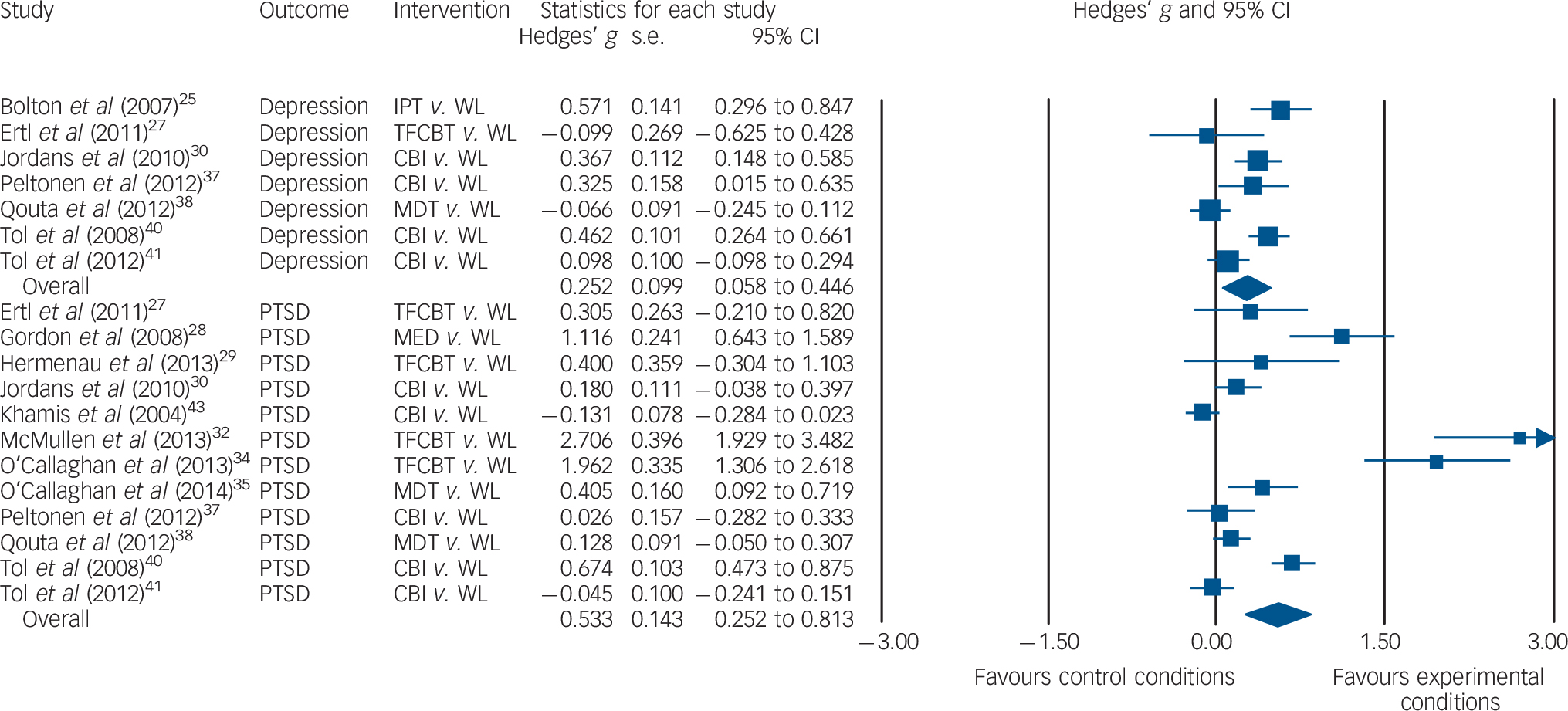
Fig. 2 Forest plot of controlled effect sizes comparing active treatments with waiting-list controls at post-treatment assessment. CBI, classroom-based intervention; IPT, interpersonal psychotherapy; MDT, multidisciplinary treatment; MED, meditation; PTSD, post-traumatic stress disorder; TFCBT, trauma-focused cognitive–behavioural therapy; WL, waiting list.
Table 3 Subgroup analysis: between-group effect sizes
| Post-treatment | Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| k a | g | s.e. | 95% CI | k | g | s.e. | 95% CI | |
| PTSD | ||||||||
| Active v. WL b | 12 | 0.53 | 0.14 | 0.25 to 0.81 | 6 | 0.27 | 0.13 | 0.02 to 0.52 |
| TFCBT v. WL | 4 | 1.33 | 0.58 | 0.20 to 2.46 | NA | |||
| CBI v. WL | 5 | 0.14 | 0.15 | −0.16 to 0.44 | NA | |||
| Other v. WL c | NA | NA | ||||||
| Depression | ||||||||
| Active v. WL | 7 | 0.25 | 0.10 | 0.06 to 0.45 | 5 | −0.02 | 0.06 | −0.14 to 0.10 |
| TFCBT v. WL | NA | NA | ||||||
| CBI v. WL | 4 | 0.31 | 0.09 | 0.14 to 0.48 | NA | |||
| Other v. WL | NA | NA | ||||||
CBI, classroom-based intervention; NA, not applicable – number of trials too small (k<4) to conduct analysis; PTSD, post-traumatic stress disorder; TFCBT, trauma-focused cognltlve–behavloural therapy; WL, waiting-list.
a. Number of treatment arms.
b. ‘Active’ comprises all active interventions excluding supportive counselling, creative play and treatment as usual.
c. ‘Other’ comprises interpersonal psychotherapy, multidisciplinary treatment and meditation.
Effects on depression
Uncontrolled effect sizes
Across all interventions (k = 12) a small pre–post effect size was found: g = 0.30, 95% CI 0.08–0.53. Uncontrolled effect sizes for changes in depression symptoms from pre-treatment to follow-up showed a medium effect size: g = 0.52, 95% CI 0.22–0.82 (k = 8).
Controlled effect sizes
The aggregated between-group effect size comparing active treatments with control conditions at post-treatment (k = 10) was small: g = 0.26, 95% CI 0.07–0.45. The comparison between active conditions with waiting-list only at post-treatment (k = 7) produced a small effect size: g = 0.25, 95% CI 0.06–0.45 (Fig. 2). At follow-up there was no difference between active treatments and control conditions: g = −0.02, 95% CI −0.11 to 0.08 (k = 7).
Heterogeneity
Heterogeneity was large for within-group effect sizes (PTSD: I 2 = 96.8, Q = 658.8, d.f. = 21, P<0.001; depression: I 2 = 91.0, Q = 122.9, d.f. = 11, P<0.001) as well as for between-group effect sizes (PTSD: I 2 = 94.7, Q = 284.5, d.f. = 15, P<0.001; depression: I 2 = 79.8, Q = 44.6, d.f. = 9, P<0.001), indicating substantial heterogeneity in effect sizes between studies. Table 2 shows the aggregated effect sizes for the different types of treatment included. However, given the relatively small number of studies in most categories, the power was judged to be inadequate for direct comparison of the different groups of treatments.
Effect on associated symptoms
Four publications reported the effect of treatment on functional impairment and the aggregated pre–post effect size in these trials was medium: g = 0.65, 95% CI 0.50–0.80. When active conditions were compared with waiting-list controls post-treatment, the aggregated effect size was small to medium: g = 0.36, 95% CI 0.26–0.49 (k = 4). At follow-up there was a small effect of active treatments compared with waiting-list controls: g = 0.18, 95% CI 0.06–0.30 (k = 4).
Publication bias
Inspection of the funnel plots depicting the uncontrolled effect sizes (pre- v. post-treatment) for PTSD and depression suggested the presence of asymmetry, as the direction of the effect of the smaller trials was towards the right. This indicates that non-significant trials might not have been published. A similar pattern applied to PTSD trials comparing active treatments with waiting-list conditions at post-treatment (as fewer than ten trials compared active treatments for depression with waiting-list controls, publication bias could not be assessed in this regard). Reference Sterne, Sutton, Ioannidis, Terrin, Jones and Lau22 The trim and fill procedure identified ten, two and seven studies to be missing regarding the uncontrolled effect sizes for PTSD and depression, and controlled effect size for PTSD, respectively. The produced imputed point estimates resulting from these three analyses were 0.34, 0.11 and 0.04, respectively.
Risk of bias in included trials
The intraclass correlation coefficient of the total score for all studies combined as rated by the two raters was 0.88 (95% CI 0.84–0.92), indicating good interrater reliability. The majority of the trials were rated as having low risk of bias in the domains random sequence generation (16 trials) and other bias (18 trials). The numbers of trials rated as having high or unknown risk in the specific domains were as follows: allocation concealment 10 trials, detection bias 11 trials, attrition bias 11 trials, reporting bias 17 trials. Altogether, the risk of bias was rated as low in 71% of cases. Furthermore, the trials did not differ substantially on risk of bias and thus this variable could not be included in subanalyses.
Discussion
Current published research indicates that psychological treatments may effectively treat PTSD in children and adolescents in LMICs. However, significant publication bias was found, and after adjustment for this bias the imputed uncontrolled and controlled effect sizes for PTSD were medium and small, respectively. Furthermore, the effects on depression were small, and here too publication bias was found. It is proposed that mass violence does not simply result in psychopathologic disorder emanating from the impact of war-related trauma but that mental health is also strongly affected by the subsequent social upheaval and other ongoing stressors. Reference Miller and Rasmussen45,Reference De Jong, Komproe, Van Ommeren, El Masri, Araya and Khaled46 Nevertheless, our findings indicated that treatments focusing on memories of the traumatic experience produced the largest effects on PTSD. However, this result is limited by the low number of trials and potential publication bias. Of the four trials comparing trauma-focused CBT with a waiting-list group, two reported very large effect sizes and two small effect sizes, which may indicate publication bias.
The low effect sizes for depression may be attributed to several factors. First, not all studies included depression measures and so the limited variance may have skewed this finding. Second, depression may be more resistant to change in LMICs because of the ongoing adversity that people often have to manage, which may engender feelings of helplessness and hopelessness. Third, a substantial proportion of the interventions were designed to address PTSD rather than depression, and so it may not be surprising that depression reduced to a lesser extent. In fact, the two studies that employed interpersonal psychotherapy – a treatment with good evidence as a psychotherapy for depression – showed a strong effect for depression. Reference Bolton, Bass, Betancourt, Speelman, Onyango and Clougherty25,Reference Schaal, Elbert and Neuner39 It should also be noted that patients allocated to waiting-list conditions enjoyed a reasonable effect size in reduction of PTSD symptoms at follow-up (0.47), a result also found in treatments in high-income countries. Reference Hesser, Weise, Rief and Andersson47
Limitations
We note some limitations to the treatments. First, approximately half the trials reported treatment completer data and the remainder reported ITT analyses; this heterogeneity in handling missing values raised difficulties in interpretation of results for a meta-analysis. Second, the variability in assessment by interview and self-report potentially leads to more heterogeneity in response as a result of measurement artefact. There were also limitations to our meta-analysis. The actual number of studies reviewed was small, making it difficult to conduct subanalyses of different groups. We also note the range of measures employed in different countries, which raises the potential problem of the lack of standardisation and suitability of measures across cultural contexts. Reference Kohrt, Rasmussen, Kaiser, Haroz, Maharjan and Mutamba48 Finally, we recognise that the focus on PTSD and depression ignored other important constructs in post-conflict settings, such as functioning.
Study implications
There is a need for caution about the capacity of these interventions to be implemented in LMICs at population levels. Publication bias might have led to an overestimation of the efficacy of interventions for mental health needs of young survivors of war. Furthermore, the mean number of treatment sessions prescribed by the treatment protocols was more than ten. This can be a significant barrier in LMICs because of difficulties for parents in transporting children to the site of intervention, civil conflict disrupting treatment access or priority being given to more immediate needs (e.g. working to assist family income). Further, many of the studies required considerable training of the providers of the treatment, as well as sustained supervision, to ensure that the intervention was delivered adequately. Reference Bolton, Bass, Betancourt, Speelman, Onyango and Clougherty25 A central tenet of global mental health is that an intervention needs to be both efficacious and capable of being scaled up to the point that it can be readily implemented in LMICs despite the limited resources of these countries. Reference Tol, Patel, Tomlinson, Baingana, Galappatti and Panter-Brick49 A major challenge for global mental health is to develop more low-intensity interventions that can still achieve reasonable effect sizes but simultaneously provide cost-effective solutions to LMICs. This would enhance the long-term and sustainable capacity to disseminate the interventions to large numbers of children in need.
Acknowledgements
This work was supported by a grant from the Netherlands Institute for Advanced Study (NIAS) given to N.M. The NIAS had no role in any aspect pertinent to the meta-analysis or the writing of the manuscript or the decision to submit it for publication. The corresponding author (N.M.) had full access to all the data and had final responsibility for the decision to submit for publication.








eLetters
No eLetters have been published for this article.