Natural disasters are increasing in frequency and impact, causing significant disruption and distress in many countries.Reference Leaning and Guha-Sapir1 McFarlane and NorrisReference McFarlane, Norris, Norris, Galea and Friedman2 define a disaster as a potentially traumatic event that is collectively experienced, has an acute onset and is time-delimited. Disasters may be attributed to natural, technological or human causes. Whether the cause of the disaster is important in distinguishing the extent of post-disaster psychopathology has been considered in a number of reviews. Neria et al Reference Neria, Nandi and Galea3 reported lower rates of post-traumatic stress disorder (PTSD) after natural disasters compared with human-made or technological disasters. Norris et al Reference Norris, Friedman, Watson, Byrne, Diaz and Kaniasty4 reported that the most severe levels of impairment occurred after disasters that resulted in the experience of mass violence. Utzon-Frank et al Reference Utzon-Frank, Breinegaard, Bertelsen, Borritz, Eller and Nordentoft5 reported increased prevalence of delayed-onset PTSD after military combat/deployment compared with other trauma groups. Bonde et al Reference Bonde, Utzon-Frank, Bertelsen, Borritz, Eller and Nordentoft6 reported increased rates of depression compared with controls after disasters and military deployment, but their data did not support specific findings for natural disasters. In contrast to all of these findings, Rubonis and BickmanReference Rubonis and Bickman7 reported that natural disasters caused significantly higher effect-size estimates than other disaster types. We therefore limited this review to disasters of natural causes to minimise heterogeneity.
Researchers commonly measure the extent of psychological distress and psychiatric disorders after natural disasters. Findings vary markedly between studies. Some report rates of psychiatric disorder as high as 60%Reference Cao, McFarlane and Klimidis8, Reference Sharan, Chaudhary, Kavathekar and Saxena9 and rates of PTSD as high as 74%,Reference Goenjian10 whereas others report non-significant differences between exposed and non-exposed populations for major depression, PTSD and other anxiety disorders,Reference Fergusson, Horwood, Boden and Mulder11 and for depressive disorders and alcohol misuse/dependence.Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12 It is probable that methodological factors contribute substantially to the variation in post-disaster effects. Previous reviews have highlighted methodological concerns, including the absence of longitudinal design, the failure to utilise appropriate controls and selective sampling techniques.Reference Rubonis and Bickman7, Reference Norris13, Reference Goldmann and Galea14
The failure to make comparisons with appropriate controls is a critical weakness that this review addresses. We restricted entry to studies that meet one of two key criteria: the measurement of pre-disaster rates of psychological distress or psychiatric disorder (to identify all studies that utilised a pre–post study design) and the measurement of rates of psychological distress or psychiatric disorder in a non-exposed control population (to provide an exposed/non-exposed comparison). In addition, we restricted this review to studies with representative samples to establish the psychological effects of natural disasters on exposed populations.
Method
This is a systematic review and meta-analysis. The study protocol was prospectively registered with PROSPERO, and can be accessed at https://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017056897 (registration number PROSPERO 2017 CRD42017056897). Study design and reporting is guided by the Meta-analysis of Observational Studies in Epidemiology guidelines (see Supplementary Appendix 1, available at https://doi.org/10.1192/bjp.2018.210 for details).Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie15
Screening, review, quality assessment and data extraction proceeded as per protocol. The study protocol proposed that multiple measures of psychological distress/disorder be aggregated to form a composite total for that study. Subsequent advice was that aggregating multiple measures was not feasible. As a consequence results are reported for psychological distress, psychiatric disorder (when measured as a whole) or individual psychiatric disorders.
Studies were eligible for the review if they measured the prevalence of psychological distress with validated scales or psychiatric disorder (defined as above the threshold for caseness according to validated scales). Studies were also eligible if they measured prevalence of PTSD, depression, anxiety or alcohol use disorder) with a validated diagnostic system. Only studies that compared measures to pre-disaster rates of disorder or distress, or a non-exposed control population were included.
Eligible samples were adult (defined by Ovid Medline as aged ≥19 years) populations representative of their catchment areas. Studies that used convenience samples or limited entry to those with the highest rates of adverse effects or the highest likelihood of these occurring were excluded. Populations not selected on the basis of disaster exposure such as immigrant groups were included if they were reflective of the sub-population from which they were sampled. Only studies that reported rates of psychological distress or psychiatric disorder more than 1 month after the onset of the natural disaster were included.
The study period was 1980 to March 2017 to coincide with the publication of the DSM-III and more reliable diagnostic systems. Potential studies were identified through a search of PubMed, EMBASE, and PsycINFO. The search strategy was guided by a research librarian and combined a search for natural disasters with a search for psychiatric disorders/psychological distress, using the Boolean classifier AND (see Supplementary Appendix 2 for details). In addition, review article references were scrutinised for possible studies and cross-referencing of included studies occurred to further identify studies for inclusion.
Two authors (B.B. and C.J.B.) independently reviewed the titles and abstracts after the initial search to identify papers for full-text review. They also reviewed the selected full-text articles to determine inclusion or exclusion into the next phase. Any initial disagreement was resolved by independent review with a third author (R.T.M.). Covidence,16 the programme recommended by the Cochrane Foundation to streamline systematic reviews, was used to assist and manage the screening process.
Eight authors were approached via email to clarify potential studies for inclusion and for unpublished data. Four authors responded: one provided an additional reference containing data for the meta-analysis, two provided unpublished data that could be included in the meta-analysis and the remaining author was unable to assist further. B.B. undertook data extraction with assistance from R.T.M. A data extraction sheet was designed and piloted for ten studies and then used with minimal refinement.
Quality assessment was guided by the use of a modified Newcastle–Ottawa Quality ScaleReference Wells, Shea, O'Connell, Peterson, Welch and Losos17 (Supplementary Appendix 3) and undertaken separately by B.B. and C.J.B., with differences resolved by discussion. A high rating was given if there were only minor weaknesses in one area, a medium rating was given if there were moderate weaknesses in one area or multiple minor weaknesses and a low rating was given if there were multiple moderate weaknesses or greater.
The studies that reported psychological distress or the presence of a psychiatric disorder were grouped based on study design (pre–post or exposed–non-exposed). A descriptive overview is provided for the data-sets that met the final inclusion criteria. Eligible studies that reported means and s.d. for continuous measures and odds ratios (or frequencies that enabled these to be calculated) for dichotomous measures contributed to the meta-analysis.
Random effects meta-analysis was undertaken with RevMan18 to aggregate studies with similar outcomes. The inverse variance method was used to calculate pooled standardised mean differences (SMDs) and 95% confidence intervals for continuous outcomes. For dichotomous measures, the Mantel–Haenszel method was used to calculate pooled odds ratios and 95% confidence intervals. The majority of the included outcome scales report increasing morbidity as scores increase. The short forms SF-12Reference Ware J, Kosinski and Keller19 and SF-36Reference Ware JE and Sherbourne20 are exceptions: the scores for these outcomes were subtracted from 100 (the maximum possible score) to scale them appropriately for meta-analysis. For studies that report outcome measurement at multiple time points, the outcome closest to 1 year post-disaster was chosen for meta-analysis purposes as this time point was felt to be most relevant for services and to clinicians. Heterogeneity among studies was tested by χ 2 tests and summarised as I 2. Sensitivity and meta-regression analyses were considered but there were insufficient studies with variables potentially explaining between study heterogeneity in the completed meta-analyses for these to be undertaken.
Results
Figure 1 provides a flow diagram of the screening and inclusion process. The databases search was completed on 3 March 2017 and revealed 1990 Medline abstracts, 1218 PsycINFO abstracts and 1343 EMBASE abstracts.
After de-duplication, authors B.B. and C.J.B. screened 2981 abstracts. This process resulted in 104 studies that were reviewed by authors B.B. and C.J.B. in full (including one study found by cross-referencing). Thirty-four studies required the use of a third author, R.T.M., to resolve whether they should be included. Forty-one studies were included for systematic review. These reported on 29 separate data-sets as some data-sets were published multiple times in separate studies. Supplementary Table 1 provides details of the included studies.
Fig. 1 Study identification flow diagram.
Twenty-one studies (reporting on 17 data-sets) evaluated psychological distress or psychiatric disorder after a natural disaster through a comparison with a non-exposed control population. Twenty studies (reporting on 12 data-sets) examined psychological distress or psychiatric disorder after a natural disaster through the use of a pre–post comparison.
The USA (14 data-sets) followed by Southeast Asia (four data-sets) were the most represented disaster locations. Disasters comprised tsunamis, floods, hurricanes earthquakes, wildfires, landslides, volcanic eruption and a typhoon. The timing of outcome measurement ranged from 1 to 48 months.
There were 27 097 participants represented in the exposed–non-exposed comparisons and 4221 participants were represented in the pre–post comparisons. The majority of studies used random or inclusive sampling techniques to evaluate adults exposed to the natural disaster of interest. Other studies evaluated sub-populations of interest not selected on the basis of disaster exposure. These included older adults,Reference Brown, Cherry, Marks, Jackson, Volaufova and Lefante21–Reference Bei, Bryant, Gilson, Koh, Gibson and Komiti23 residents of Scandinavia holidaying in Southeast Asia at the time of a major tsunami,Reference Heir, Sandvik and Weisaeth24, Reference Wahlstrom, Michelsen, Schulman and Backheden25 35-year-olds participating in an existing birth cohort study,Reference Fergusson, Horwood, Boden and Mulder11 college students,Reference Rotton, Dubitsky, Milov, White and Clark26–Reference Sattler28 veteransReference Dobalian, Stein, Heslin, Riopelle, Venkatesh and Lanto29, Reference Heslin, Stein, Dobalian, Simon, Lanto and Yano30 and immigrants.Reference Vu and Vanlandingham31 The study by Kessler et al Reference Kessler, Galea, Jones and Parker32 utilised a National Comorbidity Survey ReplicationReference Kessler and Merikangas33 sample from areas subsequently affected by Hurricane Katrina for pre-disaster measures and a post-hurricane survey offered to those who sought assistance from the Red Cross for the post-disaster measure. This methodology differs from the other studies with pre-disaster measures as they performed paired pre–post comparisons.
Thirteen studies (describing nine data-sets) reported psychological distress in an exposed–non-exposed control comparison. Eight data-sets reported statistically significant increases in psychological distress in the exposed population. The remaining study,Reference Rotton, Dubitsky, Milov, White and Clark26 reported non-significant findings for all measures of psychological distress.
Fifteen studies (describing seven data-sets) reported pre–post disaster measures of psychological distress. Four data-sets reported significant increases in psychological distress after the disaster and three studies did not report statistically significant change. Four data-sets reported data for psychological distress that could be used in an exposed–non-exposed control meta-analysis. The combined SMD was 1.10 (95% CI 0.23–1.96, P = 0.01, I 2 = 99%). Six data-sets reported data for psychological distress in a form that could be used in a pre–post disaster meta-analysis. The combined SMD was 0.32 (95% CI −0.06 to 0.7, P = 0.10, I 2 = 98%).
Figure 2 is the forest plot for the two study types demonstrating the overall effect for psychological distress after a disaster compared with a pre-disaster or non-exposed geographical control group. The combined SMD was 0.63 (95% CI 0.27–0.98, P = 0.005, I 2 = 98%), constituting a medium effect size.
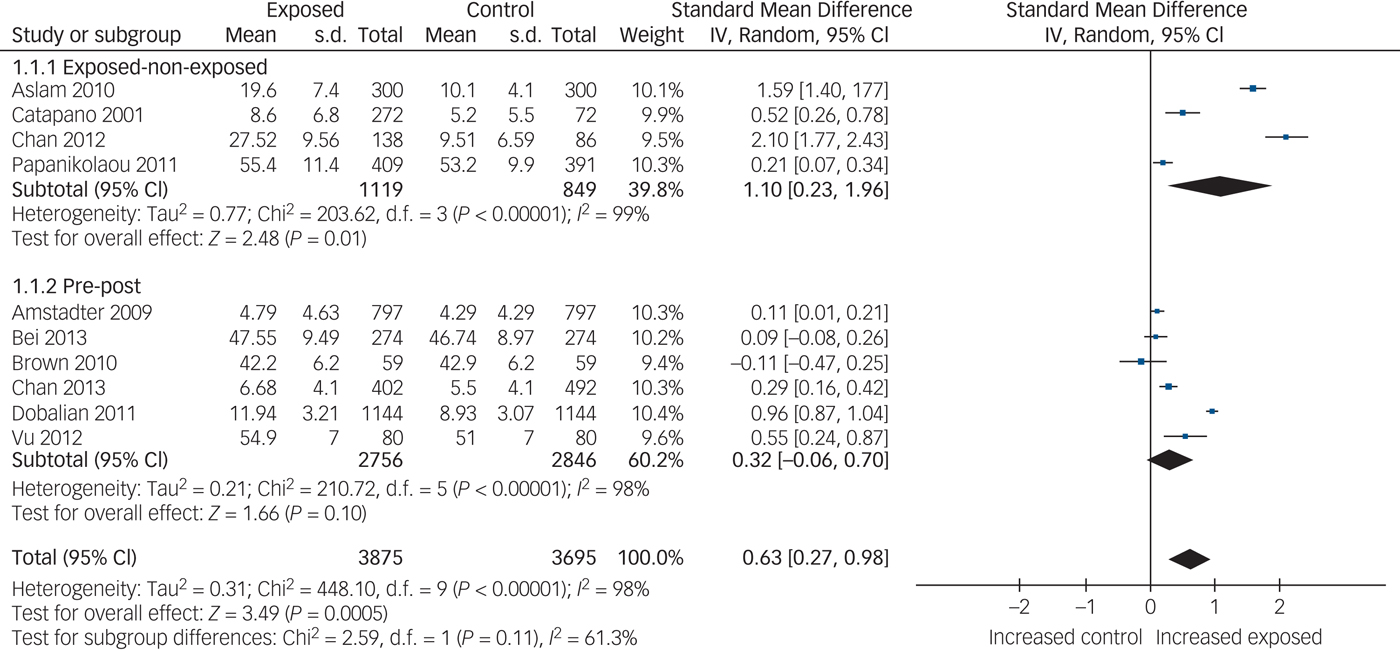
Fig. 2 Forest plot of psychological distress after natural disaster.
Seven studies (describing four data-sets) reported rates of psychiatric disorder with an exposed–non-exposed comparison. All reported statistically significant increases in psychiatric disorder for the exposed group compared with the control sample. Seven studies (describing two data-sets) measured psychiatric disorder with a pre–post disaster comparison. Both data-sets reported increased rates of psychiatric disorder after the disasters. Four data-sets reported data for psychiatric disorder that could be used for an exposed–non-exposed meta-analysis. The combined odds ratio was 2.14 (95% CI 1.58–2.90, P < 0.001). Two data-sets reported data for psychiatric disorder that could be combined for a pre–post comparison. The combined odds ratio was 1.44 (95% CI 0.98–2.11, P = 0.06).
Figure 3 is the forest plot for the meta-analysis of psychiatric disorder after a natural disaster combining the pre–post comparison and the exposed–non-exposed comparison. The combined odds ratio was 1.84 (95% CI 1.43–2.38, P < 0.001, I 2 = 76%). In this comparison, the overall percentage of psychiatric disorder in the exposed group was 38% compared with 26% in the non-exposed group.
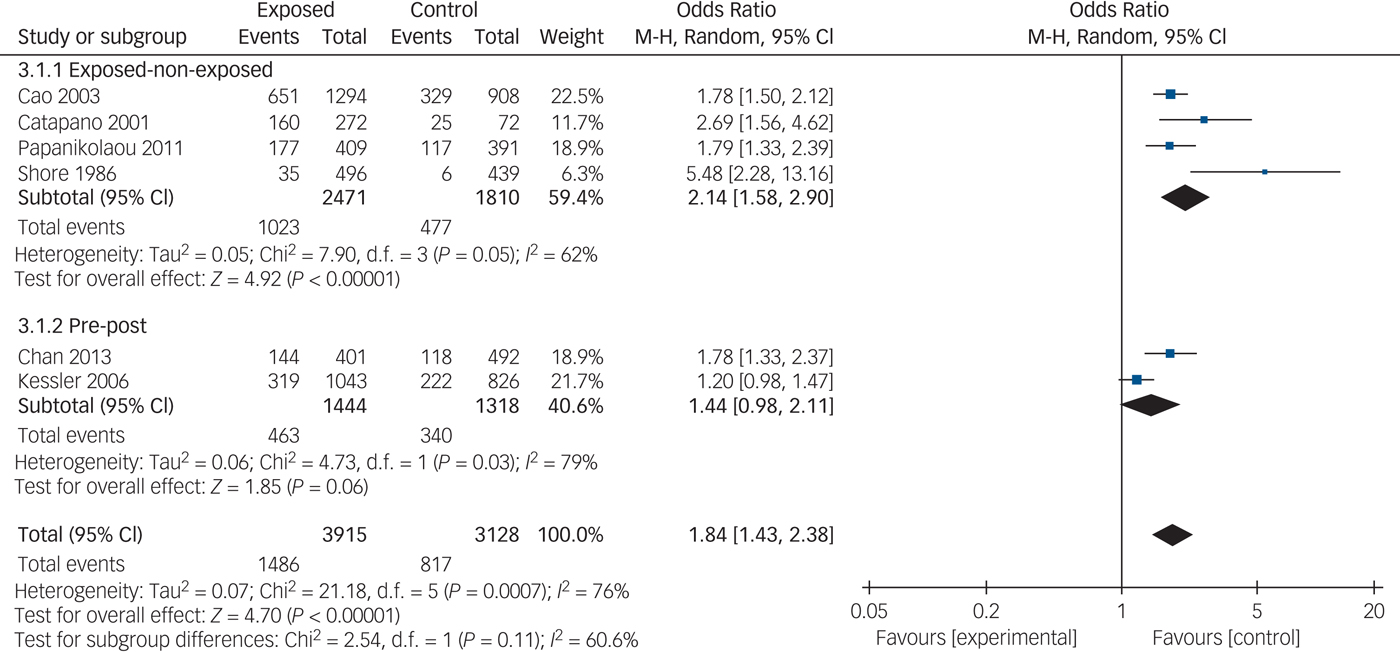
Fig. 3 Forest plot of psychiatric disorder after natural disaster. M-H, Mantel-Haenszel (see methods).
Nine studies (describing nine data-sets) evaluated PTSD through an exposed–non-exposed comparison. These studies did not specify that PTSD needed to be linked to the disaster being studied, meaning this was still a valid comparison. Eight of the nine studies reported increased rates of PTSD in the exposed group, although only five studies reported data that could be used in meta-analysis.
Three studiesReference Sattler28, Reference Aslam and Tarq34, Reference Bodvarsdottir and Elklit35 reported continuous data that could be aggregated with meta-analysis to report rates of PTSD in an exposed–non-exposed comparison. The SMD was 1.38 (95% CI 0.43–2.34, P = 0.004, I 2 = 97%), constituting a very large effect. Forest plots for this and subsequent meta-analyses are provided in the Supplementary Appendix 4. Two studiesReference Fergusson, Horwood, Boden and Mulder11, Reference Catapano, Malafronte, Lepre, Cozzolino, Arnone and Lorenzo36 reported dichotomous data for PTSD that could be combined by meta-analysis. The combined odds ratio was 5.96 (95% CI 0.25–142.54, P = 0.27, I 2 = 88%). Although this comparison was non-significant, the overall percentage experiencing PTSD in the exposed group was 10% compared with 2% in the non-exposed group.
Twelve studies (describing nine data-sets) compared depression in an exposed population with a non-exposed control population. Five of the nine data-sets reported significantly increased rates of depression in the exposed group. Five data-sets measured depression scores pre–post a natural disaster. Three data-sets reported significant increases in depression after the disaster whereas the others did not report a significant change.
Four data-setsReference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12, Reference Aslam and Tarq34, Reference Bodvarsdottir and Elklit35, Reference Chan, Xu, Huang, Wang, Zhao and Shum37 reported continuous measures of depression that could be aggregated with meta-analysis in an exposed–non-exposed comparison. The overall SMD for this comparison was 0.90 (95% CI 0.19–1.61; test for overall effect: Z = 2.48, P = 0.01, I 2 = 96%). Three studiesReference Bei, Bryant, Gilson, Koh, Gibson and Komiti23, Reference Nolen-Hoeksema and Morrow27, Reference Knight, Gatz, Heller and Bengtson38 reported continuous measures of depression that could be combined in a pre–post disaster meta-analysis. The overall SMD for this comparison was 0.10 (95% CI −0.04 to 0.23, P = 0.17, I 2 = 0%). When the two study types (pre–post disaster and exposed–non-exposed) were aggregated in a combined meta-analysis, the overall SMD was 0.55 (95% CI 0.04–1.06, P = 0.04, I 2 = 96%), constituting a medium effect size.
Two high-quality exposed–non-exposed data-setsReference Fergusson, Horwood, Boden and Mulder11, Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12 reported dichotomous measures of depression that were aggregated with meta-analysis (combined odds ratio 1.29, 95% CI 0.88–1.90, P = 0.20, I 2 = 0%). Although these findings were non-significant, the percentage experiencing depression in the exposed group was 11% compared with 7% in the non-exposed group.
Ten studies (describing seven data-sets) compared anxiety between an exposed group and control after a disaster. Four reported significant increases after the disaster and three did not. Three studies (describing three data-sets) measured anxiety pre- and post-disaster. One studyReference Phifer and Norris22 reported significant increases in anxiety, whereas the other two studiesReference Bei, Bryant, Gilson, Koh, Gibson and Komiti23, Reference Ullman, Newcomb, Cohen, Slomkowski and Robins39 did not.
Five studies (describing four data-sets),Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12, Reference Aslam and Tarq34, Reference Bodvarsdottir and Elklit35, Reference Chan, Xu, Huang, Wang, Zhao and Shum37, Reference Canino, Bravo, Rubio-Stipec and Woodbury40 reported data that could be aggregated with meta-analysis to compare continuous measures of anxiety between an exposed and control population. The combined SMD was 0.91 (95% CI −0.08 to 1.90, P = 0.07, I 2 = 98%), constituting a large effect size. Two high-quality exposed–non-exposed data-setsReference Fergusson, Horwood, Boden and Mulder11, Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12 reported dichotomous measures of anxiety that could be combined with meta-analysis. The combined odds ratio for the exposed group compared with the control was 1.33 (95% CI 0.91–1.93, P = 0.14, I 2 = 0%). Although this comparison was non-significant, the percentage experiencing anxiety in the exposed group was 13% compared with 7% in the non-exposed group.
Four studies (describing three data-sets) examined alcohol use after a disaster. Bravo et al Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12 reported non-significant increases in alcohol misuse/dependence after island-wide floods. Fergusson et al Reference Fergusson, Horwood, Boden and Mulder11 did not report significant change in alcohol misuse/dependence in their exposed group compared with non-exposed controls. Solomon et al Reference Solomon, Regier and Burke41 reported increased rates of alcohol misuse compared with a control population. The Fergusson et al Reference Fergusson, Horwood, Boden and Mulder11 and Bravo et al Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12 studies reported dichotomous measures of alcohol misuse/dependence that could be combined with meta-analysis. The combined odds ratio for the exposed group compared with the control was 1.17 (95% CI 0.76–1.79, P = 0.47, I 2 = 0%). Although this comparison was non-significant, the percentage experiencing alcohol misuse/dependence in the exposed group was 9% compared with 6% in the non-exposed group.
Supplementary Appendix 5 provides details of the quality assessment. Four studies were rated as high quality in the quality assessment. Two of the high-quality databases were pre–post in design and two were exposed–non-exposed databases. However, the two high-quality exposed–non-exposed databasesReference Fergusson, Horwood, Boden and Mulder11, Reference Bravo, Rubio-Stipec, Canino, Woodbury and Ribera12 could also take into account pre-disaster measures and are therefore a hybrid study design. Twelve databases received a medium-quality rating (six in each study type). The remaining databases were rated as low quality, according to the quality criteria.
We considered sensitivity and meta-regression analyses to examine for the possible effects of variables such as disaster type, disaster location and study type. However, even for the largest meta-analysis examining psychological distress there were five different disaster types, six broad localities and two study types, meaning a much larger numbers of studies would be required for this to be feasible.
Discussion
To our knowledge, this is the first systematic review and meta-analysis with a specific focus on methodologically sound studies measuring rates of psychological distress and psychiatric disorder after natural disasters. We report higher rates of psychological distress (combined SMD 0.63, 95% CI 0.27–0.98, P = 0.005) and higher rates of psychiatric disorder (combined odds ratio 1.84, 95% CI 1.43–2.38, P < 0.001) after natural disasters. Continuous measures of PTSD and depression are also significantly increased, whereas increases for anxiety and alcohol misuse/dependence are not significant.
Our findings can be considered alongside that of other meta-analyses evaluating psychopathology after disasters. Rubonis and BickmanReference Rubonis and Bickman7 reported a pooled effect size for all forms of psychopathology after disasters of 0.174. Bonde et al Reference Bonde, Utzon-Frank, Bertelsen, Borritz, Eller and Nordentoft6 reported an odds ratio of 2.28 for risk of depressive disorders after a natural disaster compared with a comparison group. Utzon-Frank et al Reference Utzon-Frank, Breinegaard, Bertelsen, Borritz, Eller and Nordentoft5 reported a baseline prevalence of PTSD after horrifying traumatic events of 19.7%, with a corresponding prevalence of delayed-onset PTSD of 5.6%. Therefore there is a clear signal that natural disasters result in increased psychopathology. However, direct comparisons between our study and the findings of these meta-analyses should not be made. The meta-analyses of Rubonis and BickmanReference Rubonis and Bickman7 and Bonde et al Reference Bonde, Utzon-Frank, Bertelsen, Borritz, Eller and Nordentoft6 included comparisons with groups with lesser degrees of exposure, whereas we required our comparator group to be a pre-disaster or non-exposed control. We did this to obtain the most accurate assessment of new morbidity in an affected community after a natural disaster. The meta-analysis of Utzon-Frank et al Reference Utzon-Frank, Breinegaard, Bertelsen, Borritz, Eller and Nordentoft5 was designed to report on the presence of delayed-onset PTSD after traumatic events. Although post-disaster rates of PTSD are provided, a non-exposed comparison group was not required and therefore an estimate of new morbidity after natural disaster cannot be made.
The magnitude of our findings is significant both statistically and clinically. Although many individuals experiencing psychological distress or psychiatric disorder may not seek formal help for their symptoms, this review documents a significant degree of new morbidity affecting disaster-exposed populations. This has clear consequences for those dealing with the aftermath of a disaster, including health professionals, health services and political leaders. Our study highlights the importance of mitigating strategies to minimise the adverse effects of disasters where possible.
A major finding from the meta-analyses is the high degree of heterogeneity between studies. With the exception of four meta-analyses (examining dichotomous measures of anxiety, depression, alcohol misuse/dependence and continuous measures of depression in a pre–post comparison), heterogeneity was very high. This suggests that disaster-specific and methodological factors explain the majority of the variation in outcome measurement, although the relative contributions of each could not be quantified by the study design.
However, we reduced methodological heterogeneity by restricting entry to studies that addressed previous methodological concern about lack of longitudinal design, lack of controls and selective sampling. We only included studies that used validated outcome measures and measured outcome more than 1 month post-disaster. Despite this, studies that entered the review used a large range of outcome measures and the timing of outcome measurement ranged from 1 to 48 months. This represents the main limitation to our study's findings, although the group of studies available for meta-analysis constituted a more homogenous subset. The variation in outcome measures and timing of outcome may have contributed to the between-study heterogeneity, although it is likely that other factors such as disaster type, severity, location, impact and response also influence outcome.
We also restricted entry to the review to studies that evaluated a broad range of exposure. Many post-disaster studies restrict attention to those with high degrees of exposure. Although this approach informs regarding disaster effects for those most severely exposed, we were interested in evaluating the effect on those with a range of exposures to clarify the effect of disasters on broader populations relevant to mental and public health services planning a post-disaster response.
Given the unpredictable nature of disasters, some degree of opportunism is always likely to be present in disaster research design. However, this review reinforces the importance of core epidemiological techniques and the use of longitudinal cohort studies and representative health surveys when undertaking high-quality disaster research. We recommend future disaster research always consider questions of appropriateness of comparators and representativeness of sampling in planning study design.
This systematic review and meta-analysis addresses concerns about absence of longitudinal design, failure to utilise appropriate controls and selective sampling in the disaster literature. High levels of heterogeneity point to disaster-specific effects being important in quantifying differences in outcome. They also highlight the possibility of health promoting initiatives and mitigating strategies to minimise post-disaster adversity. Despite variability in outcome, we report substantially higher rates of psychological distress, psychiatric disorder and specific diagnoses after natural disasters compared with control populations.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2018.210.





eLetters
No eLetters have been published for this article.