In Europe, employment rates of between 10% and 20% are reported for people with schizophrenia, Reference Marwaha, Johnson, Bebbington, Stafford, Angermeyer, Brugha, Azorin, Kilian, Hansen and Toumi1 yet people with severe mental illness want to work. Reference Crowther, Marshall, Bond and Huxley2 The effectiveness of the individual placement and support (IPS) model of supported employment at increasing this group's access to work has been demonstrated in North America. Reference Drake, McHugo, Bebout, Becker, Harris, Bond and Quimby3–Reference Latimer, Lecomte, Becker, Drake, Duclos, Piat, Lahaie, St-Pierre, Therrien and Xie6 Its effectiveness in European contexts has also been demonstrated by a recent six-centre randomised controlled trial, which found that IPS doubled patients' access to work. Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7 Patients with schizophrenia and those with less prior experience have been found to be less likely to obtain work, Reference Wewiorski and Fabian8 but the validity of these findings for the IPS model and in Europe has not been established. The impact of service and ‘process’ characteristics has never been tested.
We aimed to explore who among a group of patients with severe mental illness would do well in vocational services in terms of both obtaining and maintaining open, competitive employment, and which process and service factors would be associated with better outcomes. We therefore aimed to determine predictors of employment outcomes from among demographic and illness characteristics, early process factors and service features.
Method
Sample, setting and procedure
A randomised controlled trial was conducted in six European centres – London, Ulm-Günzburg, Rimini, Zurich, Groningen and Sofia – comparing IPS with usual high-quality vocational rehabilitation based on the ‘train and place’ model. Individual placement and support workers were trained for the study by the originator of the model and supervised centrally by a fortnightly telephone conference. The vocational service (control service) at each centre was the best alternative vocational rehabilitation service available locally, with a structured programme conducted mostly in day facilities (although mostly residential in Ulm). Each had to guarantee taking patients into the service within 2 months of randomisation.
Patients (n=312) were recruited if they had psychotic illness, were aged between 18 and the local retirement age, had been ill and had major role dysfunction for at least 2 years, were in the community, had not been in competitive employment in the preceding year and wanted to enter competitive employment. Randomisation was carried out centrally and stratified by centre, gender and work history (1 month or less of continuous open employment v. more than 1 month in the previous 5 years), replicating the original IPS study. Reference Drake, McHugo, Bebout, Becker, Harris, Bond and Quimby3
Patients were followed up for 18 months, with interviews at baseline (T 0) and 6, 12 and 18 months (T 1–T 3). Data were collected through interview on:
-
(a) vocational outcomes
-
(b) hospitalisation
-
(c) global functioning (Global Assessment of Functioning – Symptoms (GAF–S) and Disability (GAF–D)) Reference Endicott, Spitzer, Fleiss and Cohen9
-
(d) symptoms (Positive and Negative Syndrome Scale; PANSS) Reference Kay, Fiszbein and Opler10
-
(e) anxiety and depression (Hospital Anxiety and Depression Scale; HADS) Reference Zigmond and Snaith11
-
(f) social disability (Groningen Social Disability Schedule; GSDS) Reference Wiersma, de Jong, Kraaijkamp and Ormel12,Reference Wiersma, de Jong and Ormel13
-
(g) quality of life (Lancashire Quality of Life Profile – European Version; LQoLP–EU) Reference Oliver, Huxley, Priebe and Kaiser14,Reference Gaite, Vázquez-Barquero, Arrizabalaga, Schene, Welcher, Thornicroft, Ruggeri, vazquez-Bourgon, Perez Retuerto and Leese15
-
(h) self-esteem (Rosenberg Self-Esteem Scale; RSE) Reference Rosenberg16
-
(i) needs for care (Camberwell Assessment of Need – European short version; CAN–EU). Reference Phelan, Slade, Thornicroft, Dunn, Holloway, Wykes, Strathdee, Loftus, McCrone and Hayward17,Reference McCrone, Leese, Thornicroft, Schene, Knudsen, vázquez-Barquero, Lasalvia, Padfield, White and Griffiths18
Patients were also asked about the therapeutic relationship with their clinical keyworker or equivalent, using a measure (Helping Alliance Scale; HAS) Reference Priebe and Gruyters19 developed for community psychiatric patients (HAS–k), at baseline and each follow-up interview. They were also asked about the relationship with their vocational worker (IPS worker or named worker in the vocational service; HAS–v) at each follow-up interview. Job status was collected regularly from vocational staff, while data on therapeutic relationships (HAS) were collected from them using a modified version of HAS (HAS–p) at each follow-up point. Clinical diagnosis was confirmed by OPCRIT. Reference McGuffin, Farmer and Harvey20 The fidelity to the IPS model of both the IPS and the vocational services was assessed using the IPS fidelity scale Reference Bond, Becker and Drake21 at three time-points; further service characteristics were also collected at two time-points.
Being in remission was also tested. Patients were defined as being in remission if they met van Os et al's Reference van Os, Burns, Cavallaro, Leucht, Peuskens, Helldin, Bernardo, Arango, Fleischhacker, Lachaux and Kane22 criteria: that symptoms measured by PANSS (delusions, unusual thought content, hallucinatory behaviour, conceptual disorganisation, mannerism/posturing, blunted affect, passive/apathetic social withdrawal and lack of spontaneity and flow of conversation) were rated as absent, minimal or mild for a 6-month period (i.e. at two consecutive time-points).
The study's primary outcome was entering competitive employment (on the open market, paid at prevailing wages), operationalised as working for at least 1 day over the entire follow-up period, in replication of the original study. Reference Drake, McHugo, Bebout, Becker, Harris, Bond and Quimby3 Secondary vocational outcomes were the number of hours worked and the number of days employed (regardless of hours worked per week), all on an ‘intention to treat’ basis. For patients employed at any point during follow-up, job tenure (duration of longest job) was examined (presented separately below). For the present analyses, hours worked and days employed were found to be highly correlated (Spearman's rho=0.78), so days employed was not further analysed.
Statistical analyses
Three analyses were conducted. First, patient characteristics collected at baseline, including illness characteristics and the patient's reported relationship with their clinical keyworker, were tested as potential predictors of the employment outcomes. Second, early process factors, collected at patient level at the first follow-up interview (T 1), when the patient had been in the service for up to 6 months, were tested as potential predictors. Service allocation (IPS v. vocational service) was included as a possible explanatory variable in the early process models, despite the fact that the greater effectiveness of the IPS service had already been demonstrated. Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7 This was to ensure that it was not confounding any significant associations between other potential predictor variables and employment outcomes. It was not included in the patient characteristics models, as these variables were measured before randomisation. The impact of service as such is not the focus of the current paper. Finally, key characteristics of the services themselves were tested. As the latter were service-level factors, they were tested against the effectiveness of the IPS service at each international centre.
Patient characteristic predictors
A logistic regression analysis was conducted to determine patient characteristics predictive of entering competitive employment (working for at least 1 day). This was preceded by univariate analysis of baseline demographic, clinical and social functioning data based on evidence from the literature of factors that have a potential impact on employment outcomes. These included:
-
(a) age
-
(b) gender
-
(c) diagnosis (schizophrenia v. bipolar disorder)
-
(d) age at first contact with psychiatric services
-
(e) number of lifetime psychiatric admissions
-
(f) living situation
-
(g) immigrant status
-
(h) years of education
-
(i) prior work history and baseline global functioning (GAF–S, GAF–D)
-
(j) anxiety and depression (HADS–A and HADS–D respectively)
-
(k) symptoms (PANSS positive, negative and general scores)
-
(l) social disability (GSDS sub-scales and total score)
-
(m) quality of life (LQoLP sub-scales and total score)
-
(n) needs (CAN total number of needs, number of met needs and proportion of needs met for all five CAN sub-scales and the CAN total score)
-
(o) self-esteem (RSE).
Remission between baseline and T 1 and baseline therapeutic relationship with the clinical keyworker (HAS–k) were also tested. Univariate associations were analysed using χ2-tests for categorical predictors and unpaired t-tests for continuous predictors.
Variables significant at the 10% level were entered into the logistic regression. These analyses were carried out using SPSS for Windows version 14. Regression analyses modelling the number of hours worked and job tenure (employed patients only) against the potential predictors listed above were conducted using methods appropriate for count data. Reference Gardner, Mulvey and Shaw23 Zero-inflated Poisson regression, which is a mixture of a Poisson distribution and a degenerate distribution with point mass one at zero, Reference Hall24 was used for hours worked as this displayed a large frequency of zeros (59.0% of the data). Job tenure (n=122) was modelled using regression methods for over-dispersed Poisson-distributed data. For both outcomes, predictor variables univariately significant at the 10% level were then entered into a multivariate model. These analyses were performed with SAS for Windows Version 9.1, using PROC NLMIXED for the zero-inflated Poisson-distributed outcomes and PROC GENMOD for job tenure.
Early process predictors
Potential early process predictors of entering employment, hours worked and job tenure included the following variables at T 1 (the earliest point at which these could be measured): IPS/vocational service; number of meetings with the IPS/vocational worker; whether the patient received vocational training; patient-rated therapeutic relationship with the vocational worker (HAS–v); and vocational worker-rated therapeutic relationship with the patient (HAS–p). Time from baseline to entry into the service (0–2 months, 2–6 months and not in service at 6 months, or never taken into service) was also included as, despite the stipulation that this should be no more than 2 months, many patients were taken into the service much later. These potential explanatory variables were selected by a priori discussion in the research group. A regression model was fitted to investigate whether these variables at T 1 predicted the vocational outcomes after the appropriate univariate analyses. Patients who had not entered the service by 6 months would not have a vocational worker and were therefore excluded from the analyses, as their inclusion would create a non-random missing-value pattern for the patient- and professional-rated therapeutic relationship scores. Time to service entry was therefore also analysed univariately. The regression models were repeated without the variable IPS/vocational service, as this was known to be a powerful predictor of employment.
Service characteristic predictors of IPS effectiveness
Whether the greater effectiveness of the IPS service at some international centres was related to differences in their vocational services was explored using prospective meta-analyis. The dependent variable was the risk difference in the primary outcome (worked for at least 1 day) between IPS and vocational service groups for each centre (IPS effect sizes). The heterogeneity found was modelled using five centre-level service characteristics, chosen a priori. Each of these factors was a contrast between the IPS and vocational service in that centre. They comprised: the contrast in IPS fidelity between the IPS and vocational services; the difference in the proportion of patients entering the service within 2 months; the contrast in whether the services operated a named keyworker system or not; the difference in case-load size; and the contrast in whether the service required its patients to undertake particular steps before seeking employment.
Meta-analytic methods were used to explore the relationship between categorical variables and IPS effect size, and meta-regression methods for continuous variables, using Comprehensive Meta-Analysis Version 2.
Results
Sample
A total of 1036 people were referred to the study, of whom 728 participated in information meetings and 312 were recruited. Data on the primary outcome measure (entered competitive employment) were obtained for the whole sample. Of these, 252 (80.8%) completed the final follow-up interview. There were no differences between those who did not complete the final interview and those who stayed in the study in terms of baseline characteristics or withdrawal from IPS/vocational service. Details previously reported. Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7
The majority of the sample had a diagnosis of schizophrenia (80.3%) and were male (60.3%); 55.8% had worked for more than 1 month in the previous 5 years. Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7 The mean levels of global symptomatology and disability (GAF–S and GAF–D) were 55.3 and 53.8 (out of 100) respectively, ranging from 20 to 80. Positive, negative and general symptoms (as measured by PANSS) were 13.4 (range 7–33), 15.1 (range 7–35) and 31.3 (range 16–67) respectively, and levels of anxiety and depression (HADS) were 6.8 (range 0–19) and 6.2 (range 0–19) respectively. Social disability (GSDS) was moderate at 9.1 out of 21 (range 1–21); overall subjective quality of life (LQoLP) was 4.4 out of 7 (range 2.28–6.67); the level of need (CAN) was 6.0 out of 22 (range 0–16) and the proportion of needs rated as met was 67% (0–100).
The IPS services were more effective than the vocational services for every vocational outcome, with 85 IPS patients (54.5%) working for at least 1 day compared with 43 vocational service patients (27.6%) and IPS patients working for nearly four times as many hours (428.8 v. 119.1) over the 18-month follow-up period. Of those who worked, the duration of the longest held job was twice as long for IPS patients (214 days) as for vocational service patients (108 days). Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7
Of the 128 clients who worked, only 2 from each service had only worked for 1 day (the minimum threshold used for the primary outcome measure) and 95 had worked for more than 40 days. Just over half the IPS patients who worked (n=48; 56.5%) obtained the job before their T 1 interview, compared with 16 vocational service clients (37.2%).
Patient-level predictors
Patient characteristics as predictors of entering competitive employment
An association with having worked for at least 1 day at the level appropriate for inclusion in the logistic regression (P<0.1) was found for clinical diagnosis, work history, global disability, depression, satisfaction with job situation, satisfaction with financial situation, number of assessed social needs, proportion of social needs met and remission status. Logistic regression yielded a model in which previous work history and proportion of social needs met were significant predictors of entering employment (Table 1). Patients who had worked for more than 1 month in the 5 years prior to baseline were more than twice as likely to enter employment as patients who had not (OR=2.42, 95% CI 1.46–4.02), and a 33 percentage point decrease in social needs met (one fewer social need being met out of three) was associated with a 33% higher probability of working for at least 1 day (OR=0.99, 95% CI 0.98–1.00).
Table 1 Patient characteristics predictor models

| Predictors | OR (95% CI) | Regression coefficient (s.e.) | P |
|---|---|---|---|
| Predictors of working for 1 day (n=273) | |||
| Work history | 2.42 (1.42-4.12) | 0.001 | |
| Clinical diagnosis (schizophrenia/ schizoaffective disorder v. bipolar disorder) | 1.22 (0.58-2.55) | 0.606 | |
| GAF—D score | 0.99 (0.96-1.01) | 0.213 | |
| HADS—D score | 0.99 (0.93-1.06) | 0.814 | |
| LQoLP—EU: satisfaction with job situation | 0.85 (0.68-1.06) | 0.144 | |
| LQoLP—EU: satisfaction with financial situation | 0.94 (0.81-1.10) | 0.458 | |
| Number of social needs (CAN) | 0.87 (0.66-1.15) | 0.317 | |
| Proportion of social needs met (CAN) | 0.99 (0.98-1.00) | 0.038 | |
| In remission between baseline and T 1 | 1.83 (0.98-3.42) | 0.058 | |
| Predictors of hours worked (n=260) | |||
| Work history | 0.94 (0.274) | 0.001 | |
| LQoLP—EU: satisfaction with job situation | 0.18 (0.110) | 0.102 | |
| LQoLP—EU: satisfaction with financial situation | 0.03 (0.081) | 0.711 | |
| Proportion of social needs met (CAN) | 0.01 (0.003) | 0.062 | |
| Remission | 0.21 (0.008) | < 0.001 |
As remission was measured at T 1 (patients had to meet the clinical criteria at both baseline and T 1), by which time some patients had already entered employment, a sensitivity analysis was conducted excluding data from patients who entered employment before T 1. Remission was not associated with entering employment in this analysis.
Patient characteristics as predictors of time worked
Significant univariate predictors of the number of hours worked were work history, satisfaction with job situation and financial situation LQoLP sub-scales, CAN proportion of social needs met and remission status. Multivariate regression analysis yielded a model in which work history and remission status where significant predictors of the number of hours employed (P=0.001 and P<0.001 respectively). Patients who had worked for more than 1 month were likely to work for more hours, as were those in remission between baseline and T 1 (Table 1).
Early process predictors of entering competitive employment
For all patients, univariate analysis indicated that service allocation (IPS v. vocational service), time from baseline to entry into the service, and patient- and professional-rated therapeutic relationship were each associated with employment status at the level appropriate for inclusion in the logistic regression (P<0.1). There was a statistically significant correlation between patient- and professional-rated therapeutic relationship scores at T 1 (r=0.151), but this was not sufficiently large to necessitate the omission of one score from the logistic regression. Logistic regression generated a model in which service and higher HAS–v and HAS–p scores were significant predictors of entering employment (Table 2). The IPS patients were 2.6 times as likely to enter employment as vocational services patients (OR=2.57, 95% CI 1.18–5.64). The probability of working for at least 1 day was increased by 5% with a 1-point improvement in HAS–v score (OR=1.05, 95% CI 1.02–1.09) and by 6% with a 1-point improvement in HAS–p score (OR=1.06, 95% CI 1.03–1.10).
Table 2 Early process predictor models

| Predictors | OR (95% CI) | Regression coefficient (s.e.) | P |
|---|---|---|---|
| Predictors of working for 1 day (n=202) | |||
| Service (IPS v. vocational) | 2.57 (1.18-5.64) | 0.018 | |
| Time from baseline to entry into the service (< 2 months v. 2-6 months) | 0.00 | 0.935 | |
| HAS—v total score | 1.05 (1.02-1.09) | 0.005 | |
| HAS—p total score | 1.06 (1.03-1.10) | 0.001 | |
| Predictors of hours worked (n=191) | |||
| Service (IPS v. vocational) | 0.96 (0.042) | 0.022 | |
| Time from baseline to entry into the service (< 2 months v. 2-6 months) | 0.45 (0.599) | 0.451 | |
| HAS—v total score | -0.05 (0.018) | 0.009 | |
| HAS—p total score | -0.07 (0.019) | < 0.001 |
In order to explore the relationship between service allocation and therapeutic relationship, a model was tested including service, patient- and professional-rated therapeutic relationship and their possible interactions. A significant interaction was found between service allocation and patient-rated therapeutic relationship, indicating that for patient ratings the effect of the relationship was limited to the IPS group. A 10-point increase in HAS–v score was associated with IPS patients having a 7% higher probability of working for at least 1 day than vocational service patients (OR=1.07, 95% CI 1.00–1.14). There was no significant interaction between service allocation and professional-rated therapeutic relationship, indicating that the effect of the relationship held regardless of service.
When the analysis was repeated without service allocation (IPS v. vocational service), logistic regression generated a model in which only higher patient- and professional-rated therapeutic relationship scores were predictive of entering employment. A one-point improvement in HAS–v or HAS–p score was associated with a 6% increase in the probability of working for at least 1 day (OR=1.06, 95% CI 1.02–1.09 and OR=1.06, 95% CI 1.03–1.10 respectively).
A sensitivity analysis was conducted, testing therapeutic relationship against entering competitive employment excluding any patients who had entered employment before T 1. This again found therapeutic relationship (both HAS–v and HAS–p) to be significantly associated with working for at least 1 day.
Analysing time to service entry univariately, in order to include patients who had not entered the service by the 6-month follow-up, found that patients whose time to service entry was less than 2 months were significantly more likely to enter employment than those who had not entered the service by T 1 (OR=1.9, 95% CI 1.0–3.7, P=0.049).
Early process predictors of time worked
Early process predictors for number of hours worked included service allocation, patient- and professional-rated therapeutic relationship and time from baseline to service entry. Multivariate regression yielded a model in which service (P=0.022), HAS–v score (P=0.009) and HAS–p score (P≤0.001) were significant. The IPS patients were likely to work more hours. There was also a statistically significant negative association between therapeutic relationship ratings and hours worked, but the parameter estimates were of negligible magnitude and therefore not clinically meaningful (Table 2).
When service allocation was omitted from the analyses, the predictive model of number of hours worked indicated that patients with better therapeutic relationships (higher HAS–v (P=0.003) and HAS–p (P≤0.001) scores) worked for fewer hours, but the parameter estimates were again of negligible magnitude. In this model, patients with shorter time from baseline to service entry (P=0.027) tended to work for more hours.
When analysing time to service entry univariately, patients who entered the service within 2 months of baseline were likely to work for fewer hours (P=0.012) than those who had not entered it by T 1. Patients who entered the service between 2 and 6 months were more likely to work for more hours (P=0.007) than those who had not entered it by T 1.
Additional analysis of time to first job largely confirmed the findings for our primary outcome, with previous work history, better therapeutic relationship and having fewer social needs met predicting getting the first job more quickly.
Job tenure
For the subgroup of patients who worked during the follow-up period, job tenure was univariately associated with the following patient characteristics: gender, work history prior to baseline, global disability, negative symptoms, satisfaction with safety and number of social needs met. Multivariate regression generated a model in which only satisfaction with safety was a significant predictor of job tenure, with patients with scores on lower satisfaction with safety being likely to stay longer in employment (P=0.043). In the model of early process predictors, job tenure was univariately significantly associated with service allocation and time from baseline to service entry. Only service allocation was a significant predictor in the multivariate model (P=0.010) (Table 3). Job tenure did not differ significantly between patients who entered the service within 2 months, between 2 and 6 months, or had not entered it by T 1.
Table 3 Predictors of job tenure.

| Variables in model (n=121) | Regression coefficient (s.e.) | P |
|---|---|---|
| Patient characteristics model | ||
| Gender | 0.15 (0.154) | 0.325 |
| Work history | 0.27 (0.181) | 0.134 |
| GAF—D score | 0.01 (0.008) | 0.443 |
| PANSS—Negative | -0.02 (0.017) | 0.150 |
| LQoLP—EU: satisfaction with safety | -0.11 (0.057) | 0.043 |
| Number of social needs met (CAN) | 0.14 (0.100) | 0.151 |
| Early process predictor model (n=122) | ||
| Service (IPS v. vocational) | 0.65 (0.254) | 0.010 |
| Time from baseline to entry into the service (<2 months v. 2-6 months) | -0.20 (0.381) | 0.593 |
Service characteristic predictors of IPS effectiveness
Values for the five service variables chosen to be possible sources of heterogeneity are detailed in Table 4, where data are presented on the difference in the variable between the IPS and vocational services at each centre.
Table 4 Contrasts in key service characteristics between centres

| IPS fidelitya,b | Proportion entering service within 2 monthsa | Named keyworker systemc | Case-load sizec | Steps before job searchc | Risk difference | |
|---|---|---|---|---|---|---|
| London | 33.50 | 76.0 | Yes | No | No | 0.32 |
| Ulm | 28.00 | 100.0 | Yes | No | Yes | 0.12 |
| Rimini | 35.00 | 73.1 | No | Yes | Yes | 0.31 |
| Zurich | 36.50 | 76.9 | Yes | No | Yes | 0.38 |
| Groningen | 28.25 | 19.3 | Yes | Yes | No | 0.08 |
| Sofia | 30.25 | 18.5 | No | No | Yes | 0.41 |
| Test of heterogeneity, Q (P) | 3.04 (0.081) | 0.00 (0.996) | 1.24 (0.266) | 1.46 (0.227) | 1.17 (0.280) |
Table 4 also presents the Q-statistics and associated P-values for the five variables. Contrast in IPS fidelity was a significant source of heterogeneity at the 10% significance level. As the contrast in IPS fidelity between the IPS and vocational services increased, the difference in effectiveness increased; thus, when there was a greater contrast in IPS fidelity, there was a greater effect size in favour of the IPS service (Fig. 1). As Fig. 1 shows, Sofia was the only outlier, as implementation of the IPS model was high in contrast to the low fidelity value. The other four variables were not associated with the IPS service effect size.
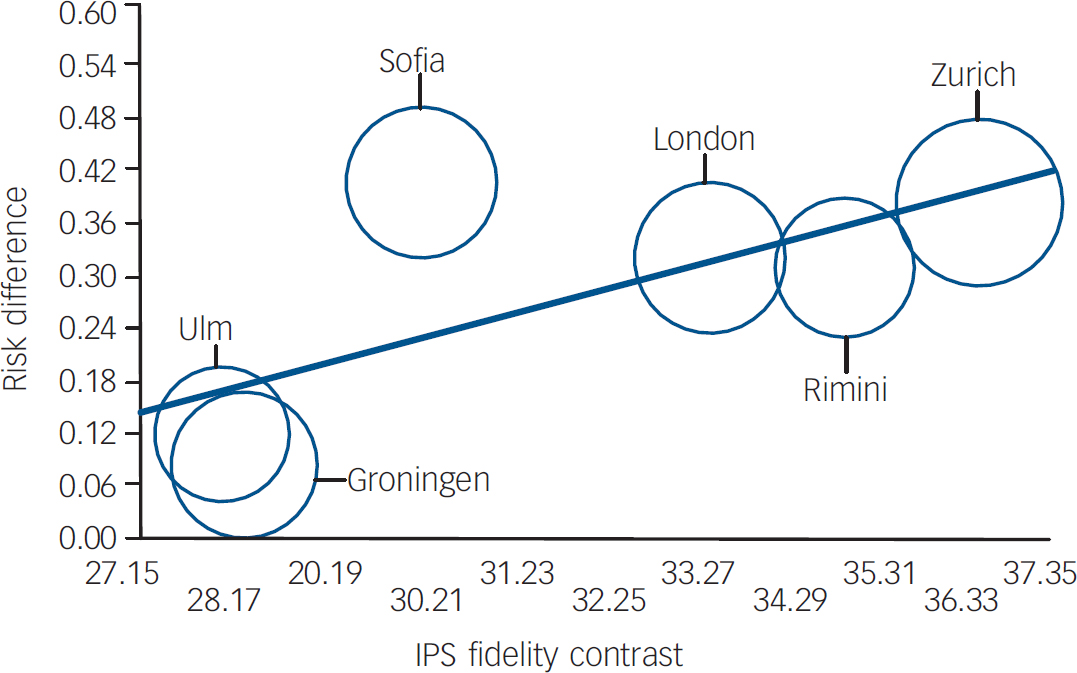
Fig. 1 Meta-regression of individual placement and support (IPS) fidelity contrast on risk difference. Data presented in Table 4 provide the coordinates of the bubble corresponding to each centre.
Discussion
Patient predictors of employment outcomes
Previous work history was the only patient characteristic predictive of all employment outcomes. Those who had worked for at least 1 month in the previous 5 years were more than twice as likely to enter competitive employment as those who had not; they obtained their first job more quickly and were also more likely to work for more hours. This confirms the findings of previous studies. Reference Wewiorski and Fabian8 Our measure of prior employment history was low (1 month's employment in 5 years), reflecting our replication of the original study, but nevertheless was strongly predictive.
In contrast with many studies, Reference Wewiorski and Fabian8 however, we did not find any association between age and employment outcomes; more unusually, no baseline clinical variables apart from remission were predictive. We thus did not replicate the finding that people with schizophrenia have worse employment outcomes than those with affective disorders. Nor did we replicate the evidence that negative rather than positive psychotic symptoms may be predictive of employment outcomes. Reference Green25 This may have been because of the narrower clinical spread of our sample (only 20% had bipolar disorder and the sample was fairly homogeneous in terms of having a psychotic disorder for at least 2 years). For our sample, previous work experience and being in remission (which our study was the first to assess) clearly had more impact than any other patient factor, with being in remission for the first 6 months of the study being univariately associated with getting a job and predicting working more hours. Remission was not predictive of getting a job, however, when excluding from analysis all those who obtained jobs in the first 6 months of the study, suggesting that although being in remission in the first 6 months was associated with getting a job during that period, it was not predictive of getting a job subsequently.
Although our primary outcome, entering competitive employment, was operationalised using a low threshold (worked for 1 day), in practice, very few patients (two from each service) worked only for 1 day. Moreover, with respect to time worked, our findings largely replicated the findings relating to the primary outcome.
Process predictors of employment outcomes
Process variables have rarely been considered in studies of supported employment, beyond levels of IPS fidelity. Although we only considered early process predictors, measured at 6 months, all the IPS patients and two-thirds (67.3%) of the vocational service patients had been taken into the services by then.
For those patients who had an IPS worker or named vocational worker, both patient- and professional-rated therapeutic relationship at T 1 were associated with working for at least 1 day, and this held even when those who found their jobs in the first 6 months of the study were excluded. For each increase of 5 points (out of 55) on the HAS at T 1, rated by either party, the likelihood of working increased by 30%. For professionals' ratings of the relationship, this association held regardless of service. For patients' ratings, however, the association only operated in the IPS group. That the relationship with the vocational worker was predictive of getting a job is consistent with the evidence that a good therapeutic relationship is associated with a range of positive clinical outcomes, Reference McGuire-Snieckus, McCabe, Catty, Hansson and Priebe26 but this has not been previously tested in relation to vocational interventions and outcomes to our knowledge. The measure of relationship used here, the HAS, was designed for community-based mental healthcare and assesses the patient's and professional's view of the qualities offered by the professional, such as understanding and commitment to helping the patient. Reference Priebe and Gruyters19 It has been validated against the more widely used Working Alliance Inventory. Reference Hovarth and Greenberg27,Reference Bale, Catty, Watt, Greenwood and Burns28 Its orientation is broadly client-centred Reference Catty, Winfield and Clement29 and it was readily adapted for use in the context of the patient–vocational worker relationship.
The other process factors tested were not associated with entering competitive employment, even when service allocation was omitted from the analysis. Shorter time to service entry, however, was associated with working for more hours, although only in the model omitting the service allocation variable. This was because time to service entry was confounded by service type, with IPS services being more likely to take patients on more swiftly: in fact, all but two IPS patients were taken into the service by T 1, whereas the vocational service patients were more evenly spread between the three categories.
For the subgroup of patients who obtained jobs, job tenure was predicted only by satisfaction with safety at baseline, with patients who felt safer having shorter job tenure. This may suggest that those feeling safer personally had less motivation to work, although this did not affect their likelihood of getting a job at all. The relationship with the vocational worker was not related to job tenure, suggesting that it helped patients with obtaining a job, but did not affect their ability to maintain it.
Motivation and dissatisfaction with life circumstances
It is generally agreed that motivation to work has a significant influence on whether people with severe mental illness gain competitive employment and an initial screen for motivation is common practice. Reference Drake, McHugo, Bebout, Becker, Harris, Bond and Quimby3 Macias et al, Reference Macias, DeCarlo, Wang, Frey and Barreira30 however, found that those with no interest in working did obtain work eventually and worked for as long as those who had had an initial interest, arguing against such an initial screen for motivation. Patients in the current study were screened for initial interest in work, so our cohorts did not exhibit a range of preferences. This is reflected in the fact that satisfaction with job situation at baseline, which effectively measured whether the patient was satisfied with not working, was not associated with employment outcomes. Nevertheless, there were several indications that dissatisfaction with aspects of their current circumstances, and thus a motivation to change them, may have been a factor in our study, although not tested systematically.
Having more of their social needs met at baseline made patients less likely to get a job. Thus, being more satisfied with social and intimate relationships seems to have given them less incentive to seek work. Similarly, having one more service need met (needs for information, transport, access to telephone and benefits), likely to reflect satisfaction with benefits, also doubled the likelihood of a patient withdrawing from the vocational service. Satisfaction with personal or neighbourhood safety had a comparable impact on job tenure, with those feeling less safe being more likely to hold onto their job for longer.
Findings on time to service entry, though based on univariate analysis only, also suggest an impact of motivation. These findings were driven by the vocational service patients, who entered the service over a longer period of time than did the IPS patients. Those taken into the service between 2 and 6 months after baseline worked for more hours than those not in the service at T 1, but those taken in even more swiftly actually worked for fewer hours. It may be that those taken into the service very swiftly had no opportunity to lose (or demonstrate) motivation, so although they were likely to get a job they eventually worked for fewer hours; those who waited longer to be taken into the service but did then engage with it, thus having to maintain their motivation over time, subsequently worked for more hours.
Although the function of employment as therapeutic or empowering for users of mental health services has been often suggested, Reference Harding, Strauss, Hafez and Lieberman31,Reference Rogers32 our findings provide some evidence that even within a group identifying themselves as wishing to work, specific personal circumstances and experiences of clinical services may actually be demotivating in seeking competitive employment.
Service characteristics and IPS effectiveness
Prospective meta-analysis methodology has been applied to the analysis of a similar multicentre trial of a complex intervention by Banks et al Reference Banks, McHugo, Williams, Drake and Shinn33 and was also used in the present study to explore how variation in effectiveness of IPS can be explained partially by socio-economic factors. Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7 The five centre-level service characteristics tested here were all expressed as the difference between the IPS and the vocational service at each international centre. The impact of a centre's IPS service having particularly high IPS fidelity might thus be counterbalanced by its vocational service being particularly close to the IPS service. Only IPS fidelity contrast explained the heterogeneity between centres with regard to the effectiveness of the IPS model, and this was the only trend (P=0.081). This is comparable to the findings of several studies that IPS fidelity is associated with its effectiveness. Reference Drake, McHugo, Becker, Anthony and Clark34,Reference Becker, Xie, McHugo, Halliday and Martinez35 The nature of the meta-analytic technique precluded also testing IPS fidelity per se.
Beyond fidelity
Although the importance of fidelity to the IPS model has been demonstrated in a number of studies, Reference Becker, Xie, McHugo, Halliday and Martinez35–Reference McGrew and Griss37 it does not account for all the variance in outcome in IPS studies. Reference Drake, Bond and Rapp38 Drake et al Reference Drake, Bond and Rapp38 have therefore argued that other features need to be considered, such as professional skills. The present study has begun to fill this gap in the literature by analysing process variables. Our finding that therapeutic relationship predicted getting a job suggests that building a relationship with the patient is one of the key skills involved in vocational services, with a demonstrable effect on vocational outcome. It is standard paractice for IPS workers to be deliberately recruited from professionals without prior mental health experience Reference Becker and Drake39 and anecdotally this lack of experience of the patient group was an initial hurdle for the professionals involved. Our findings suggest that targeting relational skills for working with this patient group would be a valuable focus for all vocational interventions.
Limitations
The study was powered on the comparison of IPS with vocational services, Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7 although the sample was sufficiently large for the analyses presented here. However, the number of predictors selected for inclusion in the multiple regression on the basis of univariate pre-testing means that some associations reported as statistically significant may, in fact, be spurious.
The prospective meta-analysis technique allowed inclusion of only five variables (number of centres minus one). This limited the number of variables we could explore, although it did allow for a more focused, hypothesis-driven analysis. In addition, early process variables were collected at T 1 rather than at a fixed interval from each individual patient's service entry.
The fact that the analysis of early process predictors had to be conducted with the subgroup of patients who could provide HAS data means that the impact of delay to entering the service on the whole patient group, including those who did not enter the service at all, could only be considered univariately. Patients who did not enter the service at all were not significantly less likely to work for at least 1 day, however. Reference Burns, Catty, Becker, Drake, Fioritti, Knapp, Lauber, Rössler, Tomov, van Busschbach and White7 Nor was delay entering the service found to be associated with the effectiveness of the IPS model when considered at the service level in the prospective meta-analysis.
Our findings closely parallel those of previous studies and therefore should be widely generalisable, but the motivation and focus that inevitably comes from participation in a research study cannot be ignored. Effect sizes are likely to be more modest in routine practice.
Acknowledgements
T.B. designed the study with W.R. and A.F.; it was run by T.B. and J.C. All authors were involved in the conduct of the study, interpreting the results and in revising and correcting the paper, which was drafted by J.C. and T.B. The analyses were led by S.W. All authors read and approved the final version of the manuscript.
Members of the Enhancing the Quality fo Life and Independence of Persons Disabled by Severe Mental Illness through Supported Employment (EQOLISE) Group are as follows: Tom Burns, Jocelyn Catty, Connie Geyer, Marsha Koletsi, Pascale Lissouba, Miles Rinaldi, Sarah White (London), Thomas Becker, Ulrike Ehiosun, Rana Kalkan, Reinhold Kilian (Ulm), Angelo Fioritti, Denise Manchisi (Rimini), Astrid Niersman, Jooske van Busschbach, Durk Wiersma (Groningen), Christoph Lauber, Wulf Rössler, Ingeborg Warnke (Zurich), Dimitar Germanov, Toma Tomov (Sofia), Adelina Comas, Claire Curran, Martin Knapp, Anita Patel (LSE).
This study was funded by a grant from the European Union, Quality of Life and Management of Living Resources Programme (QLRT 2001-00683). Thanks are due to Greg McHugo for methodological advice, to Deborah R. Becker and Miles Rinaldi for training the IPS Workers, and to the IPS Workers themselves: Alison Lewis (London), Wulf Dorn and Eva Marischka (Ulm), Donato Piegari (Rimini), Bettina Bartsch and Patric Meyer (Zurich), Anne Mieke Epema, Laureen Jansen and Bea Hummel (Groningen), and Petar Karaginev (Sofia).








eLetters
No eLetters have been published for this article.