There is no consensus on the position of electroconvulsive therapy (ECT) in current depression treatment protocols. For depression with psychotic features, ECT is the first-line treatment according to several guidelines,Reference Milev, Giacobbe, Kennedy, Blumberger, Daskalakis and Downar1–3 whereas others recommend antidepressant monotherapy4 or in combinationReference Ellis5 with antipsychotics. In clinical practice ECT is often used to treat patients with treatment-resistant depression. In a recent meta-analysis the response rate was 58% for patients with treatment-resistance depression and 70% for those without.Reference Haq, Sitzmann, Goldman, Maixner and Mickey6 Despite many studies on possible predictors of response to ECT, Kellner et al Reference Kellner, Greenberg, Murrough, Bryson, Briggs and Pasculli7 recently concluded that no useful clinical predictors have emerged. A possible explanation for this apparent lack of clinical predictors is the fact that many studies investigating predictors are underpowered to find an effect. Furthermore, heterogeneity between studies may mask the ability of a clinical variable to predict ECT response. Since many relatively small studies have been performed, meta-analysis may be useful to calculate effect sizes of possible predictors. A more accurate prediction of response and remission would be helpful to guide decision-making and preferably treat those patients likely to respond to ECT. This could substantially shorten depressive-episode duration.Reference Husain, Rush, Fink, Knapp, Petrides and Rummans8 To our knowledge, there have been no meta-analyses that look at prediction of response and remission separately. The difference between the two is, however, clinically relevant. Remission has become the gold standard for depression treatment, because patients who do not remit have a poorer prognosis than those who do. They have a greater chance of relapse and recurrence.Reference McIntyre and O'Donovan9
Method
Age, depression severity, psychotic and melancholic features were selected as potential predictors in this meta-analysis. They were selected because of their possible clinical relevance and because their role in the prediction of response and remission of depression after ECT is unclear. In an earlier meta-analysis,Reference Haq, Sitzmann, Goldman, Maixner and Mickey6 older age and psychotic features were weakly associated with greater ECT response rates, but heterogeneity was notable. Analyses of symptom severity and melancholic features were inconclusive as a result of study heterogeneity in the same analysis.
This meta-analysis was conducted and reported according to the PRISMA-P (preferred reporting items for systematic review and meta-analysis protocols) and MOOSE guidelinesReference Moher, Shamseer, Clarke, Ghersi, Liberati and Petticrew10, Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie11 (supplementary Table 1; available at http://dx.doi.org/10.1192/bjp.2017.28). Objectives and eligibility criteria were specified in advance and documented in a protocol (available from the authors on request).
Eligibility criteria
In order to obtain details of recent original studies on the predictive effect of age, severity of depression, melancholic and psychotic symptoms on the effectiveness of ECT (as it is currently practised) in patients with depression we applied the following eligibility criteria:
(a) studies assessing the effect of brief- or ultrabrief-pulse ECT on depression severity, published in or after 1995, articles are written in English;
(b) adults (>18 years of age) diagnosed with uni- or bipolar depression as confirmed by Research Diagnostic Criteria , DSM-III-R, DSM-IV, DSM-IV-TR, DSM-5 or ICD-10 criteria;
(c) presence of psychotic or melancholic symptoms as confirmed by a structured diagnostic or clinical interview;
(d) classification of patients as ‘responder/non-responder’ or ‘remitter/non-remitter’ based on scores on valid clinician-rated depression scales (Hamilton Rating Scale for Depression (HRSD) or Montgomery–Åsberg Depression Rating Scale (MADRS)) that were administered before and soon after the end of the ECT course;
(e) effect sizes (or raw data enabling calculation of the effect size) of single-response predictors were provided or could be obtained by contacting the authors.
Data sources and study selection
We searched Embase, Medline, Web of Science, Cochrane, PubMed publisher and Google scholar up to 17 February 2017. Articles published before 1995 were discarded. We chose to select studies from 1995 onward to get an overview of predictors of ECT as it is currently practised. The indication for, and practice of ECT has changed substantially over the years. This implies that including older studies means increased heterogeneity.
Combinations of the words depression, electroconvulsive therapy, response, remission and the four predictors (age, depression severity, psychotic and melancholic symptoms) were used. References from reviews and relevant articles were searched for additional studies. The titles and abstracts were screened for relevance. We selected articles in English. Searches were combined and duplicates removed. To maintain statistical independence of effect sizes, studies that reported on the same population were identified. When redundancy was obvious, the most comprehensive report with the largest sample size was used.
The inclusion of papers in the meta-analysis was evaluated separately by two independent researchers, the first (L.v.D.) and second author (S.v.d.A.). Disagreements were resolved via consensus. If no agreement was obtained, there was further discussion with two senior researchers (T.B. and D.S.).
Data-collection process
When reported results were insufficiently detailed but the remaining inclusion criteria were fulfilled, corresponding authors were contacted for clarification and re-contacted if necessary. Authors were contacted if an email address was available and the author had published in the past 10 years. If data on only response or remission were available, authors were contacted to ask if data on the other outcome measure could also be provided. In total, 62 authors were contacted, 21 of the responding authors provided us with the data necessary to use their study in the meta-analysis.Reference Bauer, Pfennig, Linden, Smolka, Neu and Adli12–Reference Huuhka, Anttila, Huuhka, Leinonen, Rontu and Mattila32
Data extraction
The information was independently extracted from each article by two investigators (L.v.D. and S.v.d.A.) using a data extraction sheet with the following data:
(a) study characteristics: year, country and design of the study, diagnostic classification and depression severity scale used;
(b) characteristics of the study sample: number of participants, percentage female participants, percentage of patients with psychotic symptoms, mean age of the participants, average episode duration and percentage with medication resistance;
(c) ECT related: the average number of ECT sessions, electrode position used;
(d) outcome measure: general response and remission rates, response and remission rates for patients with depression with and without psychotic symptoms, for patients with and without melancholic symptoms, average age (and s.d.) and depression severity score (and s.d.) for ‘responders/non-responders’ and ‘remitters/non-remitters’.
Quality assessment
There was a strict use of eligibility criteria to select studies for the meta-analysis. Diagnostic criteria had to be used and an objective measurement of response based on one of the clinician-rated depression scales was required.
Furthermore, two of the reviewers (L.v.D. and T.B.) independently assessed several other quality aspects of the included studies based on the GRADE methodReference Goldet and Howick33 and the Newcastle–Ottawa Quality Assessment ScaleReference Stang34 for cohort studies. The following three quality criteria were assessed:
(a) design of the study (pro- or retrospective);
(b) observational or interventional study;
(c) completeness of outcome data (more v. less than 20% drop-out).
Outcome measures
The primary outcome was remission, the secondary outcome was response. The use of continuous data would be a more sensitive method to detect differences. However, we chose to use remission as primary outcome measure because it is often used as such in clinical practice. Remission is associated with a lower full symptomatic recurrence rate compared with achieving treatment response.Reference McIntyre and O'Donovan9, Reference Trivedi and Daly35 In all the selected studies, response was defined as a reduction of at least 50% from the baseline HRSD or MADRS score. Remission was usually defined as a depression scale score equal to or below 7 (for HRSD-17) or 10 (for HRSD-21, HRSD-24 and MADRS).
Statistical analyses
The predictors were analysed separately with Comprehensive Meta-Analysis (CMA version 3). The effect size was analysed as an odds ratio (OR) for the dichotomous variables psychotic and melancholic symptoms. For age and severity of depression, the effect size was represented by the standardised mean difference (SMD). For each predictor, a random-effects model was computed since we expect the true effect to vary from study to study dependent on the composition of the study population.Reference Borenstein, Hedges, Higgins and Rothstein36 The Stata ‘metan’ package was used for part of the analyses on publication bias.
Without consideration of the study weights in the random-effects model, we calculated the average age of all ‘responders/non-responders’ and ‘remitters/non-remitters’. In the same way, response and remission percentages were calculated for those with and without psychotic and melancholic symptoms.
Publication bias
When there were ten or more studies in an analysis,Reference Higgins and Green37 funnel plots were used to visualise whether or not the effects found were dependent on the sample size.Reference Borenstein, Hedges, Higgins and Rothstein36 Publication bias was formally assessed with the Egger's test in CMA for age and depression severity given their continuous outcomeReference Egger, Davey Smith, Schneider and Minder38 and with the Harbord's test in Stata for the dichotomous predictors.Reference Harbord, Egger and Sterne39
Heterogeneity and sensitivity analysis
Heterogeneity was assessed using Cochran's Q-test and I 2 statistics. An I 2 statistic of 0–40% was interpreted as heterogeneity that might not be important, 30–60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity and 75–100% is considerable heterogeneity.Reference Higgins and Green37
Heterogeneity was further explored conducting sensitivity analyses. Therefore, we calculated the effect using fixed-effect and random-effects modelling and evaluated the effect of the modelling procedure on the overall effect per predictor. A substantial difference in the effect calculated by the fixed- and random-effects model will be seen only if studies are markedly heterogeneous.Reference Egger, Smith and Phillips40
Furthermore, we compared the overall effects based on potential clinical sources of heterogeneity such as the continent of origin (according to World Health Organization classification), the study population (average age and episode duration of the sample, the percentage of patients with psychotic features, percentage with medication resistance) and treatment parameters (length of ECT course and electrode position used). The effects were also compared based on the before mentioned study quality criteria.
Results
Selection of studies
After removal of duplicates and studies published before 1995 (Fig. 1), the literature search yielded 2193 potentially relevant articles. We excluded 1991 articles after review of titles and abstracts. The full texts of the 202 remaining studies were analysed; 171 of them did not meet eligibility criteria and were excluded, 2 articles were added through reference lists and 1 through cross-reference. In total, 34 articles were selected and used in this meta-analysis.Reference Bauer, Pfennig, Linden, Smolka, Neu and Adli12–Reference Huuhka, Anttila, Huuhka, Leinonen, Rontu and Mattila32, Reference Dannon and Grunhaus41–Reference Tominaga, Okazaki, Higuchi, Utagawa, Nakamura and Yamaguchi53 The interrater reliability was good, with an interrater agreement of 96.1% (kappa (κ) = 0.87, 95% CI 0.78–0.96).
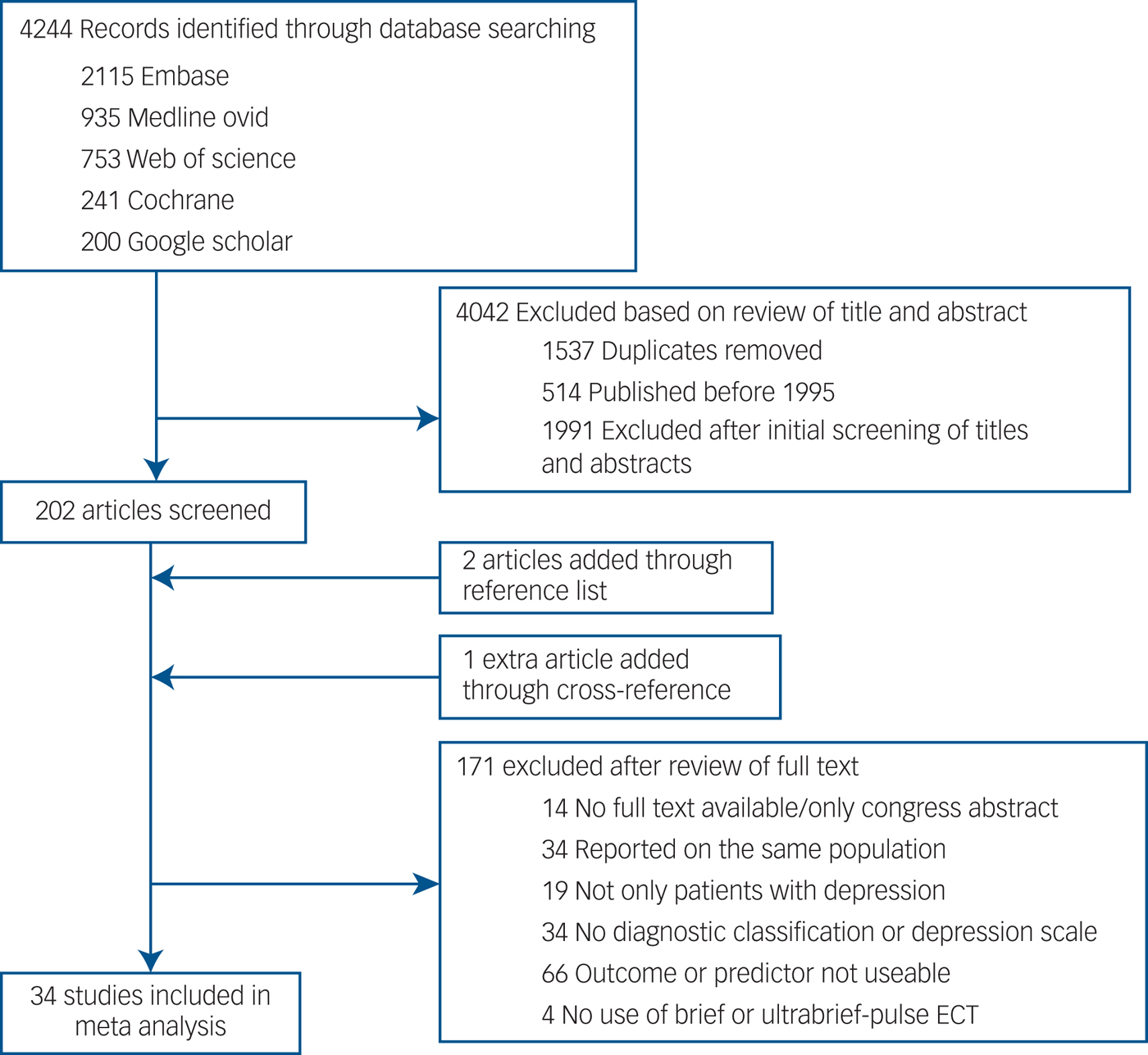
Fig. 1 Study selection.
Study characteristics
Overall, the selected studies reported on 3276 participants that received an ECT course (supplementary Table 2). More than half of the studies (52.9%) were carried out in Europe. A total of 25 studies included psychotic symptoms, 28 had data on age, 28 on depression severity and 7 on melancholic symptoms.
Studies had between 15 and 414 participants (on average 99 per study). The majority of the participants (64.3%) were women (range 27.0–77.8%) and 32.6% had psychotic symptoms (range 6.7–70.6%). Patients were on average 57.1 years of age (range of mean age was 33.1–74.8). Three studies reported on the same large sample, but on a different predictor.Reference O'Connor, Knapp, Husain, Rummans, Petrides and Smith19, Reference Fink, Rush, Knapp, Rasmussen, Mueller and Rummans31, Reference Petrides, Fink, Husain, Knapp, Rush and Mueller54 The data of the largest sample were used for the above calculations of study characteristics. One of the three was eventually excludedReference Petrides, Fink, Husain, Knapp, Rush and Mueller54 because data on psychotic symptoms were provided by the authors of the largest sample.Reference O'Connor, Knapp, Husain, Rummans, Petrides and Smith19
Results of the quality assessment can be found in the supplementary material (supplementary Table 3). There were 7 retrospective studies and 27 had a prospective design. In total, 26 studies were observational, 8 of them were interventional. Eight studies had a drop-out rate of more than 20%.
Psychotic symptoms
Remission
Data on the presence of psychotic symptoms and remission following ECT were provided in 21 studies. For remission, the OR under the random-effects model was 1.47 (95% CI 1.16–1.85, P = 0.001, I 2 = 36.6) (Fig. 2(a)). The remission rate for patients with depression and psychotic symptoms was 57.8%; for those without psychotic symptoms it was 50.9%.
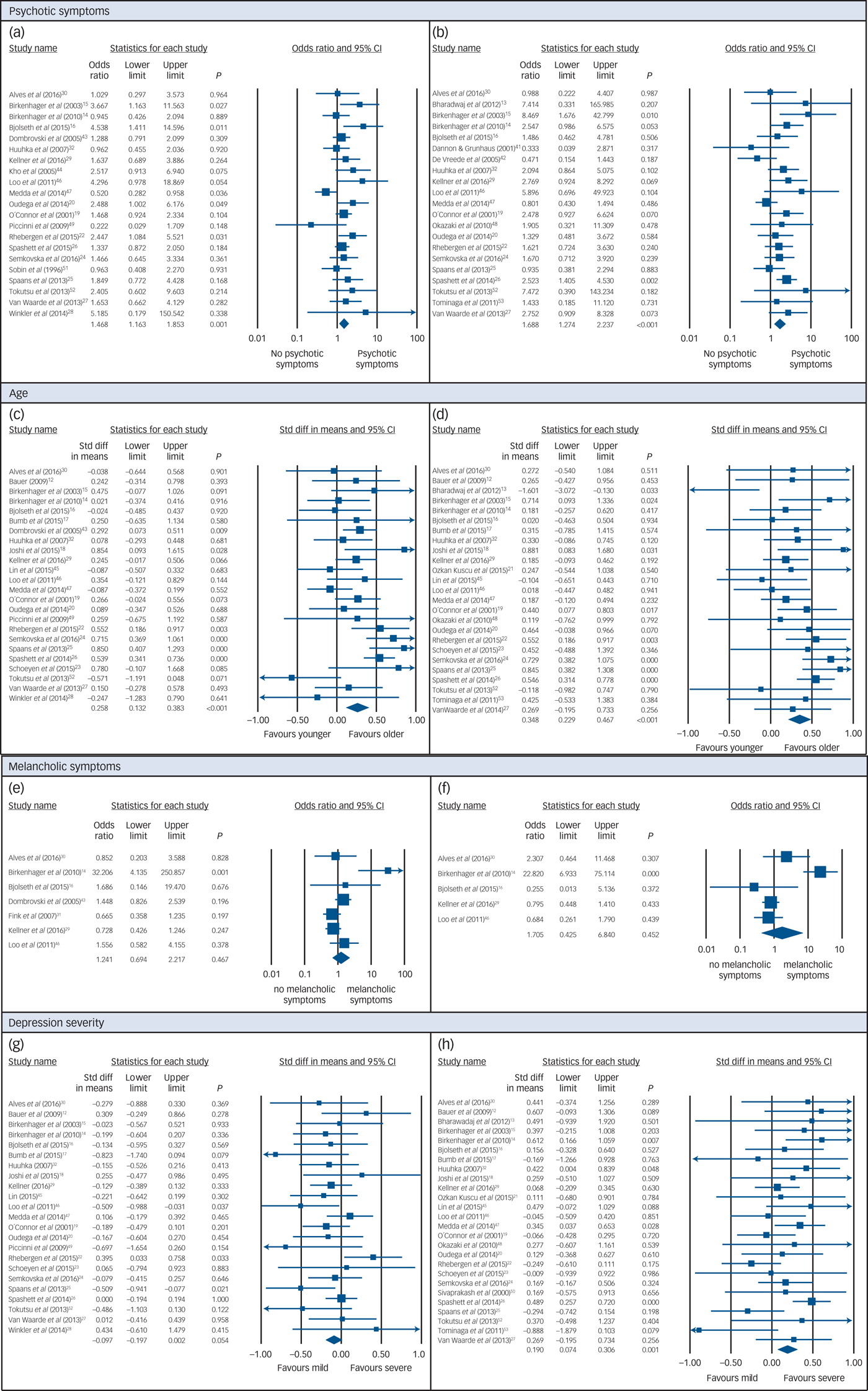
Fig. 2 Random-effects meta-analyses.
Response
Data on the presence of psychotic symptoms and response to ECT were provided in 21 studies. Psychotic features were positively associated with a higher ECT response rate under the random-effects model (Fig. 2(b)). The OR was 1.69 (95% CI 1.27–2.24, P < 0.001, I 2 = 25.8). The response rate for patients with depression and psychotic symptoms was 78.9% and for those without psychotic symptoms it was 70.6%.
Age
Remission
In total, 24 papers provided data on age and remission. Age was positively associated with higher ECT remission rates under the random-effects model (Fig. 2(c)). The SMD was 0.26 (95% CI 0.13–0.38, P < 0.001, I 2 = 53.4). The average age of those whose condition remitted was 59.7 years, compared with 55.4 years for those whose condition did not.
Response
Data on age and response to ECT could be extracted from 25 papers. Age was positively associated with a higher ECT response under the random-effects model (Fig. 2(d)). The SMD was 0.35 (95% CI 0.23–0.47, P < 0.001, I 2 = 29.7). The average age of those who responded was 58.2 years, compared with 54.9 years for those who did not respond.
Melancholic symptoms
Remission
There were seven studies that provided data on presence of melancholic symptoms and remission after ECT. The OR under the random-effects model was 1.24 (95% CI 0.69–2.22, I 2 = 63.9, Fig. 2(e)). The difference was, however, not significant (P = 0.467). The remission rate for patients with depression and melancholic symptoms was 62.9%, for those without melancholic symptoms it was 65.5%.
Response
Data on melancholic symptoms and response could be obtained from five studies. The OR under the random-effects model was 1.71 (95% CI 0.43–6.84, I 2 = 85.9, Fig. 2(f)). The difference was, however, not significant (P = 0.452) and there was considerable heterogeneity. The response rate for patients with depression and melancholic symptoms was 71.1% and for those without melancholic symptoms it was 64.7%.
Depression severity
Remission
Data on depression severity and remission could be extracted from 23 studies. Remission following ECT was less likely in patients with higher depression severity scores, although the effect was not significant under the random-effects model (SMD = −0.10, 95% CI −0.20–0.002, P = 0.054, I 2 = 29.7, Fig. 2(g)).
Response
In total, 26 studies reported on depression severity and response to ECT. A small but significant association was found between response and baseline symptom severity scores on the HRSD or MADRS, under the random-effects model (SMD 0.19, 95% CI 0.07–0.31, P = 0.001, I 2 = 28.1, Fig. 2(h)). Patients with higher scores were more likely to respond to ECT.
Publication bias
The funnel plots that could be generated revealed no obvious asymmetry (see supplementary Fig 1). Given the limited number of studies in the melancholia analyses, no funnel plots were generated for this predictor. According to Egger's and Harbord's test there was also no significant publication bias in all of these analyses (Table 1).
Table 1 Results of tests for publication bias

Heterogeneity and sensitivity analysis
A group of observational studies often shows considerable heterogeneity, regardless of the number of included studies. The Cochran's Q-test and I 2 statistics were used to quantify heterogeneity. There was evidence of moderate heterogeneity in all of the analyses that were done (Table 2), and substantial heterogeneity in the analyses on melancholic symptoms.
Table 2 Sensitivity analyses – results of random- and fixed-effect models and heterogeneity tests

n, total number of participants; OR, odds ratio (predictor present/predictor absent); SMD, standardised mean difference (‘responders’ – ‘non-responders’ or ‘remitters’ – ‘non-remitters’).
* P < 0.05, **P < 0.01, ***P < 0.001.
Heterogeneity was further explored conducting sensitivity analysis. Therefore, we calculated the effect using both fixed-effect and random-effects modelling and evaluated the effect of the modelling procedure on the overall effect per predictor. The difference between results of fixed- and random-effects analyses were small (Table 2), confirming that heterogeneity in our analyses was limited.
Besides that, we compared the overall effects based on the potential clinical sources of heterogeneity and study quality criteria (as discussed). Continuous variables were analysed with meta-regression, categorical variables were subjected to mixed-effects subgroup analysis. Studies were excluded from the analyses if data on the variable was not available. This can explain differences found in overall effects.
Psychotic symptoms
Age and medication resistance were clinical sources of heterogeneity in the remission analysis (Table 3). The predictive effect of psychotic symptoms was stronger in samples with older patients and those with lower levels of medication resistance. The results were not significantly influenced by the other potential clinical sources of heterogeneity (length of the ECT course, episode duration, electrode position and location of the study, supplementary Table 4).
Table 3 Tests of heterogeneity – results of meta- regression

* P < 0.05, **P < 0.01.
The study quality criteria had no significant influence on the results of the remission analysis (design of the study, drop-out and whether or not it was an observational study, supplementary Table 4). The length of the ECT course was a clinical source of heterogeneity in the response analysis. It was significantly related to the effect size, with longer courses corresponding to a greater predictive effect of psychotic symptoms on ECT response (Table 3). The results were not significantly influenced by the other potential clinical sources of heterogeneity (age, episode duration, therapy resistance, electrode position, location of the study) or the study quality criteria (design of the study, drop-out and whether or not it was an observational study, supplementary Table 4).
Age
The most important clinical source of heterogeneity in the analyses on the effect of age on response and remission after ECT, was the average episode duration (Table 3). SMDs were greater in studies with longer episode duration. Moreover, the predictive effect of age was significantly higher in studies that used right unilateral or variable electrode positions, compared with those only using bilateral ECT in the remission analysis (Fig. 3a).
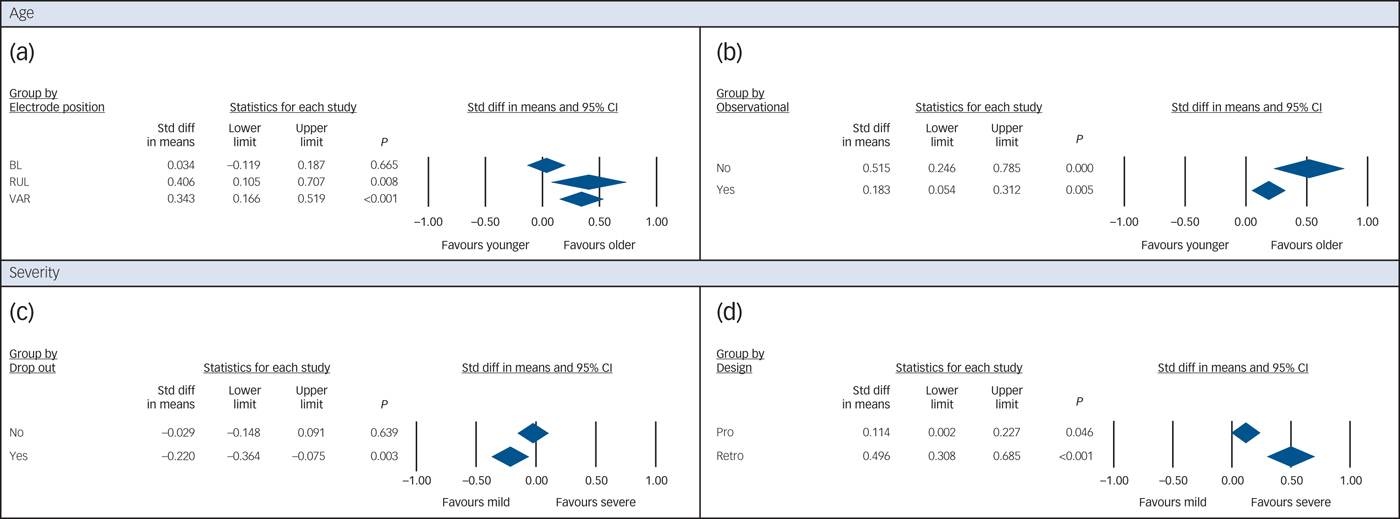
Fig. 3 Significant results of subgroup analyses.
In the remission analysis, the SMD was also influenced by whether it was an observational study, or an interventional study. Interventional studies found on average higher SMDs than observational studies (Fig. 3b). The results were not influenced by the other potential clinical sources of heterogeneity (psychotic symptoms, medication resistance, length of the ECT course, location of the study), or the other study quality criteria (design of the study and drop-out, supplementary Table 4).
In the response analysis, the results were not significantly influenced by the other potential clinical sources of heterogeneity (psychotic symptoms, electrode position, location of the study, medication resistance, length of the ECT course), or the study quality criteria (design of the study, drop-out and whether or not it was an observational study, supplementary Table 4).
Melancholic symptoms
Because of low patient numbers in part of the analyses and different definitions of the concept of melancholia, results of the response and remission analyses were considered to be inconclusive. Therefore, sensitivity analyses were not performed.
Depression severity
In the remission analysis, there was no significant influence of the potential clinical sources of heterogeneity (age, psychotic symptoms, episode duration, medication resistance, length of the ECT course, location of the study). Drop-out was a source of heterogeneity in the remission analysis (Fig. 3c). Studies with drop-out rates above 20% found that lower depression scale scores favoured remission after ECT. Those with limited drop-out found no effect at all of depression severity. There was no significant effect of the other study quality criteria (design of the study and whether or not it was an observational study, supplementary Table 4).
The results of the response analysis were not significantly influenced by any of the potential clinical sources of heterogeneity (age, electrode position, length of ECT course, episode duration, therapy resistance, location of the study). The SMD in the response analysis was influenced by the design of the study. Retrospective studies found remarkably higher SMDs than prospective studies (Fig. 3d). The results were not influenced by the other study quality criteria (drop-out and whether or not it was an observational study, supplementary Table 4).
Discussion
Main findings
This meta-analysis provides evidence for the superior efficacy of ECT in patients with depression with psychotic features, in older patients and in those with a more severe depression, whereas data on melancholic symptoms were inconclusive. This is an important finding, because identification of reliable predictors could contribute to more targeted patient selection, consequently increased ECT response and remission rates and limited episode duration.
We included 34 studies reporting on 3276 patients with a depressive disorder treated with ECT. There were relatively strict inclusion criteria to select only high-quality studies and, in contrast to previous meta-analyses on prediction of ECT efficacy, we made a distinction between data on response v. remission.
Presence of psychotic symptoms had an OR of 1.69 (P < 0.001) for response and 1.47 (P = 0.001) for remission. The SMD for older age was 0.35 (P < 0.001) in the response analysis, for remission it was 0.26 (P < 0.001). These are all rather small effect sizes.Reference Cohen55 When we look at the average age of patients whose condition remitted (59.7) and compare this with the age of those who did not remit (55.4), the difference is only 4.3 years. One could hypothesise that the age of 57 somehow resembles a turning point in remission following ECT. However, it is clear that not every person older than 57 will experience remission after treatment with ECT, just as remission will not occur in every patient with depression with psychotic symptoms. Therefore, age and psychotic symptoms are no waterproof predictors of ECT efficacy. They can, however, serve as one of several factors that can guide treatment decision-making.
A weaker association was detected between the severity of depression and response to treatment (SMD 0.19, P = 0.001). Depression severity was not associated with remission. This appears logical, since higher scores pre-ECT need a larger decrease than lower scores to attain remission.
Psychomotor disturbance is a key marker not only of melancholia but also of psychotic depression.Reference Parker56 Thus, those with depression with psychotic features often have melancholic symptoms. Consequently, the finding that depression with psychotic features is a predictor of ECT response and remission indirectly points to melancholic symptoms also having predictive potential. However, this does not result from our analysis. The few studies that reported on melancholic symptoms did not use the same definition of melancholia. Furthermore, one of the studies had a very low number of patients without melancholic features,Reference Bjølseth, Engedal, Benth, Dybedal, Gaarden and Tanum16 and another one had very low numbers of individuals who responded/remitted in patients without melancholic symptoms.Reference Birkenhäger, Pluijms, Ju, Mulder and van den Broek14 This resulted in very large confidence intervals and considerable heterogeneity. We conclude that this predictor is insufficiently investigated to draw solid conclusions on its predictive effect.
Several relevant factors have emerged from the heterogeneity analysis. Presence of psychotic symptoms was a stronger predictor of remission in older patients and in patients with limited medication resistance. Psychotic symptoms were a stronger predictor of response for those with a longer ECT course. A stronger predictive effect of psychotic symptoms in patients receiving a longer ECT course could mean that patients with depression with psychotic symptoms might benefit from longer ECT courses.
A limited episode duration is known to predict a good response to ECT.Reference Haq, Sitzmann, Goldman, Maixner and Mickey6 However, in studies with longer episode duration, the predictive effect of age on response and remission was stronger. This is remarkable, since we have no reason to expect that episode duration per se has an influence on the strength of the predictive effect of age. The value of the predictor age was also considerably higher in studies that used right unilateral or variable electrode positions in the remission analysis. As we look further, this result might be mediated by the location at which the study was performed. Age was a strong predictor of response and remission in studies carried out in the USA and Europe, and although the difference was not significant, the predictive effect was not that clear in studies carried out in Asia. An explanation could be that studies from Asia all use the standard bilateral electrode position, administer relatively short ECT courses and participants had a lower average age. The question therefore remains if the predictors that show a significant effect are relevant independent of the already known predictors and other confounders.
Besides the four predictors we investigated, there are several other potential clinical predictors that have been subject to previous meta-analyses. The predictive effect of the number of episodes, the age of onset, gender and a bipolar diagnosis on the efficacy of ECT appears to be non-existent.Reference Haq, Sitzmann, Goldman, Maixner and Mickey6 The lack of predictive value of a bipolar diagnosis was confirmed by a second meta-analysis.Reference Dierckx, Heijnen, van den Broek and Birkenhäger57 There was a significant influence of episode duration (SMD −0.43, P < 0.001; I 2 = 35%) on ECT response. The weighted mean episode duration for those who responded was 6.6 months and 14 months for those who did not respond. Medication failure was the second significant predictor (OR 0.57, P = 0.002; I 2 = 35%) for poorer ECT response, as mentioned in the introduction. This result was also confirmed by a second meta-analysis.Reference Heijnen, Birkenhäger, Wierdsma and van den Broek58
Data on known response predictors (episode duration and medication failure) and the percentage of patients with psychotic symptoms were not always provided and could therefore not always be accounted for in the current analyses. The results of the heterogeneity analyses therefore have to be interpreted with care.
The effect size of psychotic symptoms as predictor of response and remission was considerably higher than the effect found in a recent meta-analysis on ECT response prediction by Haq et al (OR = 1.34, P = 0.12).Reference Haq, Sitzmann, Goldman, Maixner and Mickey6 The same holds true for age (SMD 0.112, P = 0.25) and depression severity (SMD −0.022, P = 0.90). Differences between the meta-analyses were that, in our study response and remission rates were separated and strictly defined by HRSD or MADRS score. In addition, we retrieved unpublished data from 21 authors, contributing to a more complete analysis of those studies. To recapitulate, our study probably analysed a more homogeneous sample that facilitated detection of significant differences.
Strengths
There are several strengths to this comprehensive meta-analysis. To make sure we based our analysis on reliable data, we used relatively strict criteria for selection of studies (use of a diagnostic instrument and a validated clinician-rated depression scale). The second strength is the separate analysis for response and remission. This distinction enabled us to confirm the findings of one outcome criterion by a second one. Our findings lead to the conclusion that age and psychotic symptoms are stronger predictors of response than of remission. The fact that we contacted a number of authors for extra data contributed to a large sample to study and a more complete data analysis of studies concerned, limiting publication bias. Furthermore, it enabled us to find sources of heterogeneity.
Limitations
There are several limitations to our meta-analysis. Where strict selection criteria can be considered a strength, they can also be considered a limitation. As a consequence, a number of (often large) studies have been excluded. An example is a large Swedish study (n = 990)Reference Nordenskjöld, von Knorring and Engström59 that has only used Clinical Global Impression – Improvement scores and not a clinician-rated depression scale (HRSD or MADRS) to distinguish between individuals who responded and those that did not. The results of this study are, however, in line with our findings – a higher proportion of older patients responded (84.3%) as compared with younger ones (74.2%, P < 0.001) and patients with severe, depression with psychotic features had the highest response rate (88.9%) compared with patients with severe, non-psychotic depression (81.5%) and patients with mild/moderate depression (72.8%, P < 0.001). Furthermore, several seemingly suitable studiesReference Sackeim, Prudic, Devanand, Nobler, Lisanby and Peyser60, Reference Sackeim, Prudic, Nobler, Fitzsimons, Lisanby and Payne61 could not be used because they have not reported on the value of predictors for responders v. non-responders and could not provide us with these data.
As mentioned before, we did not only use data from studies that were designed specifically to look at the predictive effect of psychotic symptoms or one of the other predictors. Part of the data could be abstracted from studies with a different objective. Considering publication bias, this is an advantage. On the other hand, this is an extra source of heterogeneity between the studies. Different populations were studied, the studies had divergent designs, several depression scales and versions of these scales were used and the definition of remission can therefore not be exactly the same in every study. Moreover, ECT practice and patient selection for ECT differs all around the world.Reference Leiknes, Von Schweder and Høie62 We tried to minimise the impact of this heterogeneity by including some of these parameters in heterogeneity analysis to determine their effect on outcome.
Despite the fact that more effective forms of ECT exist,Reference Tor, Bautovich, Wang, Martin, Harvey and Loo63 we have chosen not to exclude studies that use ultrabrief-pulse ECT. Given its cognitive advantages it can be the preferred treatment for a subgroup of patients with depression. The predictor results of the studies that use only ultrabrief-pulse ECTReference Kellner, Husain, Knapp, McCall, Petrides and Rudorfer29, Reference Loo, Mahon, Katalinic, Lyndon and Hadzi-Pavlovic46 are in line with the overall results of our meta-analysis.
Clinical implications
Besides episode duration and treatment resistance, which are established predictors for the efficacy of ECT, age, depression severity and the presence of psychotic symptoms can also be of value in the ECT treatment decision-making process. Previous studies found a favourable response to ECT in patients with a short episode duration and limited treatment resistance. When episode duration is longer, age might be able to guide decision-making.
ECT could be suggested relatively early to those prone to respond or remit, thereby limiting depression duration and preventing a chronic trajectory of depressive symptoms. Other treatment options can first be considered for those with lower response and remission chances.
Research implications
We have used the general definition of melancholia in our meta-analysis. Another strategy could be to investigate psychomotor disturbance as measured by the CORE Assessment of Psychomotor Functioning or the score on HRSD retardation and agitation item scores as a more specific marker.Reference Parker and McCraw64 Observable psychomotor disturbance has been suggested as an essential criterion in making a diagnosis of melancholiaReference Snowdon65 and proved to be a predictor of ECT response in previous studies.Reference Hickie, Mason, Parker and Brodaty66, Reference Fink, Edward, Donald, Jules, Koukopoulos and Carroll67 For future projects, it could be valuable to incorporate measurement of the severity of psychomotor disturbance next to the general definition of melancholia so that the predictive effect of the presence of melancholia and more specific psychomotor disturbance can be evaluated.
Our analysis examined a lot of (often) small studies that report on two or three of the factors that are known to be relevant. Larger studies that report on all of the identified predictors (and the presence of personality disorderReference Rasmussen68) could be valuable to get a clearer view on the combined effect of several predictors.
A combination of these clinical variables with their biological underpinnings could further improve response and remission prediction and could serve as more objective tools to guide patient treatment matching.
Acknowledgements
We thank the authors mentioned in the Method section for sharing unpublished data. Besides that, we thank data specialist Wichor Bramer for the literature search.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2017.28.









eLetters
No eLetters have been published for this article.