Anxiety and depression are very common, and they can improve with cognitive–behavioural therapy (CBT). However, most cases are untreated. Therapists could help more patients by delegating repetitive treatment aspects to effective computer guidance. In open and randomised controlled trials (RCTs) people with anxiety and depression improved almost as much when guided mainly by certain computer-aided CBT systems as when guided entirely by a live therapist, and computer-aided CBT reduced the per-patient therapist time (e.g. Reference Osgood-Hynes, Greist and MarksOsgood-Hynes et al, 1998; Reference Kenwright, Liness and MarksKenwright et al, 2001; Reference Greist, Marks and BaerGreist et al, 2002; National Institute for Clinical Excllence, 2002; Reference Marks, Kenwright and McDonoughMarks et al, 2003; Reference Proudfoot, Goldberg and MannProudfoot et al, 2003). Open pragmatic evaluations complement RCTs as a guide to outcome in daily practice. The present one evaluates a primary care clinic's use of four computer-aided CBT self-help systems as ‘clinician extenders’ and not ‘clinician replacers’. It aimed to yield more patients treated effectively per therapist than is possible without computer-aided self-help by lessening patients’ use of therapists’ time.
METHOD
Design and mode of operation
A computer-aided self-help clinic was set up, the first to offer broad-spectrum computer-aided CBT in primary care. It was broad spectrum in that it used four different computer-aided systems and several modes of access for people with a variety of anxiety and depressive disorders. It operated for 15 months as an open pragmatic evaluation project within the West London Mental Health Trust and the Charing Cross Campus of Imperial College. It publicised its service in local general practitioner (GP) surgeries, community mental health centres, psychiatric out-patient clinics, local papers, Yellow Pages, voluntary organisations (e.g. Triumph Over Phobia– UK) and National Health Service (NHS) Direct.
The clinic accepted subjects who sent a completed screening questionnaire obtained with a pre-addressed envelope from a pack that the clinic sent to GP surgeries, other clinics and enquirers who phoned. Suitability criteria were: presence of an anxiety or depressive disorder; motivation to use self-help; and no substance misuse, psychosis or active suicidal plans. From the screening questionnaire staff judged referrals’ likely suitability for computer-aided CBT and offered them a 30-min screening interview by telephone or face to face at the clinic. Staff sent unsuitable patients a letter to this effect and copied it to their GP (unless they asked the clinic not to contact their GP). Diagnoses were obtained using a checklist summarising relevant ICD–10 (World Health Organization, 1992) diagnostic criteria.
How clinic patients used computer-aided CBT
Patients who were suitable at the screening interview were given an identification number allowing access to whichever of the clinic's four computer self-help systems most suited them: FearFighter for phobia/panic (Reference Kenwright, Liness and MarksKenwright et al, 2001; Reference Marks, Kenwright and McDonoughMarks et al, 2003); Cope for depression/anxiety (Reference Osgood-Hynes, Greist and MarksOsgood-Hynes et al, 1998); Balance for general anxiety/depression (Reference YatesYates, 1996); and BTSteps for obsessive–compulsive disorder (Reference Greist, Marks and BaerGreist et al, 2002). Patients knew that the information they gave their system was confidential to staff and could not be accessed without knowing the patient's identification number and password (many said they told the computer sensitive things they would not tell a human). Their system stored no personal identifiers such as names or addresses.
Patients were told that they could use their system as much as they wished. They were advised to use FearFighter (for phobia/panic), Cope (for depression/anxiety) or BTSteps (for obsessive–compulsive disorder) at least six times over 12 weeks. During office hours they had six brief scheduled therapist contacts by telephone or face to face for advice. Users of Balance (for general anxiety/depression) were asked to use it at least three times over 4 weeks (Balance is more basic than the three other systems) and to have three brief therapist contacts by telephone or face to face during that period.
Patients accessed FearFighter on a stand-alone personal computer (PC), mostly at the clinic or, rarely, on a stand-alone PC made available free at one internet café and one medical centre. When FearFighter became available on the internet some accessed it on a PC at home or elsewhere which was linked to the internet.
The clinic gave users of Cope and BTSteps, along with their identification number, self-help booklets to guide their free phone calls made from home to either Cope's or BTSteps's interactive voice response (IVR) system in a computer in Wisconsin, USA. Users could phone that computer from home around the clock for as long and as often as desired, and carried out their interviews by key presses on their telephone keypad. The computer faxed to the clinic weekly reports of patients’ telephone calls, their duration, the modules accessed and (for Cope patients) suicide risk – had this become high, which never happened, this would have been immediately faxed or phoned to the clinic.
Balance users accessed the system by a PC with a CD–ROM drive at home or at the clinic, at a GP surgery or, rarely, at a free internet café.
Clinic staff
The clinic was mainly run by two nurse therapists (L.G., M.K.) who, between them, totalled only one whole-time-equivalent clinician (because they spent much time on research, teaching and publicising the clinic's service), and an administrator/research assistant (R.C.). The research psychologist (D.M.-C.) had a mainly research rather than clinical role. The clinic was co-directed by two consultant psychiatrists (I.M.M., S.H.).
Outcome measures
Self-ratings were collected at pre- and post-treatment unless otherwise stated, and lower scores denoted normality/improvement:
-
• For all patients: Patient Global Impression of Improvement score (score range 0–6, at post-treatment; Reference GuyGuy, 1976), Work and Social Adjustment score (WSA; Reference Mundt, Marks and ShearMundt et al, 2002), Single-Item Depression Scale score (at pretreatment; Reference McKenzie and MarksMcKenzie & Marks, 1999), satisfaction (at post-treatment) rated on four questions (see Results), computer literacy (at pre-treatment) and motivation to do computer-aided CBT (at pre-treatment).
-
• For phobia/panic: Fear Questionnaire (Reference Marks and MathewsMarks & Mathews, 1979).
-
• For depression: Beck Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961) and the Hamilton Rating Scale for Depression (HRSD; Reference HamiltonHamilton, 1960).
-
• For generalised anxiety disorder: Beck Anxiety Inventory (BAI; Reference Beck, Epstein and BrownBeck et al, 1988).
-
• For obsessive–compulsive disorder: Yale–Brown Obsessive–Compulsive Scale (YBOCS; Reference Goodman, Price and RasmussenGoodman et al, 1989).
Data analysis
The sample's features are described. Univariate analyses of variance and chisquare tests compared patients who completed treatment with those who were unsuitable, refused or dropped out early. Paired sample t-tests were used for outcome analyses. Significance was set at 0.05 and all tests were two-tailed.
RESULTS
Patient flow
Over 12 months of intake the clinic received 355 screening questionnaires. Of these 355 patients, 149 (42%) obtained their screening questionnaire from a mental health professional, 101 (28%) from a GP and 105 (30%) by phoning the clinic after seeing advertisements in local newspapers, Yellow Pages, GP surgeries, etc. The referral rate was greatest in the last few months, as news of the clinic spread.
Of the 355 patients, 28 (8%) were unsuitable on the screening questionnaire (Fig. 1), the main reasons being: suicide risk (6), wanting face-to-face therapy (5), poor motivation (2), other diagnosis (7) and other reasons (8). The rest (327 referrals) were offered a screening interview with a clinician, of whom 61 (19%) did not attend and 266 (81%) did.
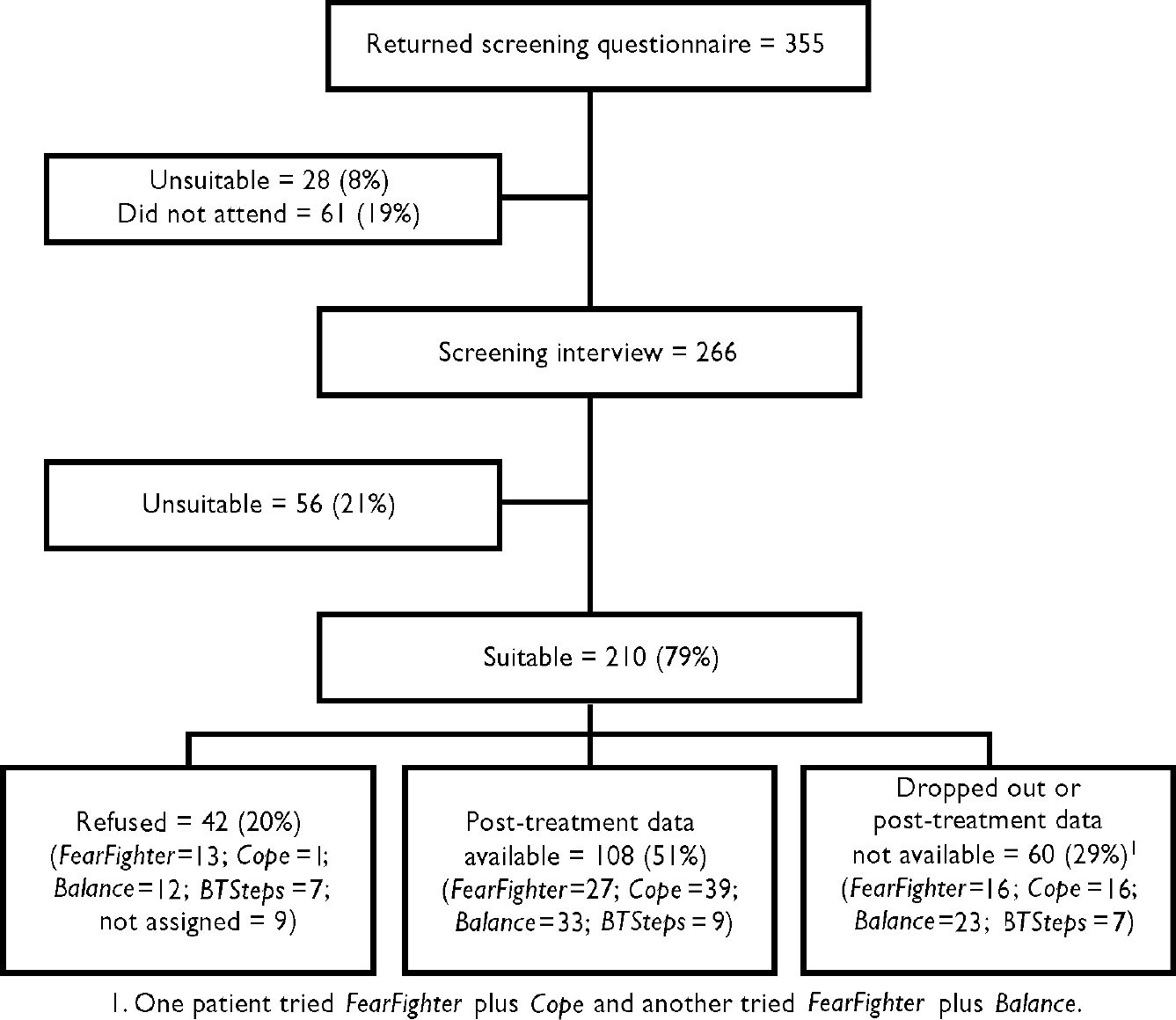
Fig. 1 Patient flow of the self-help clinic over 15 months.
Of the 266 who had a screening interview (Fig. 1), 210 (79%) were suitable for and offered computer-aided CBT and 56 (21%) were unsuitable. The main reasons for unsuitability were: no primary anxiety or depression (18), unsuited for CBT (13), work/social problems (8), poor motivation (6), suicide risk (5), living outisde the free catchment areas of the West London Mental Health Trust and the Hillingdon Primary Care Trust and without funds from an alternative NHS or private source (3), language problem (2) and wanting face-to-face therapy (1).
Refusal and dropping out
Of the 210 patients suitable at the screening interview, 42 (20%) refused computer-aided CBT and 60 (29%) dropped out early or gave no post-treatment data. Of the 39 patients who gave information, the main reasons for refusing or not completing the therapy included: hard to attend clinic/could not commit (13), the therapy was unhelpful (10), wanting face-to-face help (8), low motivation (8), offered help elsewhere (2) and problem improved (2). Those who were unsuitable, refused, dropped out and completed did not differ on initial severity.
Features of the referrals
Table 1 shows the pre-treatment features of all referrals, of those unsuitable at the screening interview, of suitable patients who refused or dropped out early and of those who completed the computer-aided CBT for all available variables: gender, age, socio-economic status, referral source, problem duration, medication, diagnosis and initial Single-Item Depression Scale score. There were no significant differences between these groups for any of the variables except diagnosis (see below). The greater initial depression of those who dropped out compared with that of those who completed the therapy was not significant on a Bonferroni correction for multiple tests. Some data are lacking for referrals who were unsuitable on the screening questionnaire and so either had no screening interview or did not attend it.
Table 1 Pretreatment features of the clinic's referrals over 12 months

| Variable | All referrals (n=355) | Unsuitable (n=56) | Completed (n=108) | Refused (n=42) | Not completed2 (n=60) |
|---|---|---|---|---|---|
| Gender: n (%) | |||||
| Male | 164 (46) | 28 (50) | 51 (47) | 18 (43) | 31 (52) |
| Female | 191 (54) | 28 (50) | 57 (53) | 24 (57) | 29 (48) |
| Age: years (s.d.) | 38 (13) | 36 (13) | 39 (12) | 38 (14) | 36 (11) |
| Socio-economic status: n (%) | |||||
| High professional | 15 (4) | 3 (5) | 7 (6) | 1 (2) | 1 (2) |
| Middle professional | 97 (28) | 17 (30) | 30 (28) | 15 (36) | 15 (25) |
| Low professional | 66 (19) | 12 (21) | 20 (18) | 5 (12) | 16 (27) |
| Manual worker | 41 (11) | 10 (18) | 9 (8) | 3 (7) | 4 (7) |
| Unemployed or student | 121 (34) | 12 (21) | 38 (35) | 15 (36) | 22 (37) |
| Unknown | 15 (4) | 2 (4) | 4 (4) | 3 (7) | 2 (3) |
| How screening questionnaire obtained: n (%) | |||||
| Directly from the clinic | 105 (30) | 15 (27) | 33 (31) | 14 (33) | 16 (27) |
| General practitioner | 101 (28) | 19 (34) | 28 (26) | 11 (26) | 18 (30) |
| Mental health professional | 149 (42) | 22 (39) | 47 (43) | 17 (40) | 26 (43) |
| Problem duration: years (s.d.) | 8 (10) | 9 (12) | 7 (8) | 11 (11) | 9 (10) |
| Medication: n (%) | |||||
| None | 148 (42) | 26 (46) | 43 (40) | 16 (42) | 24 (40) |
| Antidepressant | 171 (48) | 24 (43) | 60 (55) | 20 (48) | 30 (50) |
| Benzodiazepine | 46 (13) | 8 (14) | 14 (13) | 6 (14) | 6 (10) |
| Antipsychotic | 21 (6) | 6 (11) | 4 (4) | 2 (5) | 5 (8) |
| Beta-blocker | 16 (5) | 0 (0) | 6 (5) | 4 (10) | 3 (5) |
| Hypnotic/anxiolytic | 10 (3) | 1 (2) | 3 (3) | 4 (10) | 1 (2) |
| Anti-manic | 4 (1) | 0 (0) | 1 (1) | 0 (0) | 1 (2) |
| Unknown | 12 (3) | 2 (4) | 0 (0) | 3 (7) | 2 (3) |
| Primary ICD—10 diagnoses: n (%)1 | |||||
| Depression | 71 (21) | 5 (9) | 36 (33) | 8 (19) | 22 (37) |
| Phobia | 57 (17) | 4 (7) | 26 (24) | 14 (33) | 13 (22) |
| Generalised anxiety disorder | 35 (10) | 3 (5) | 19 (18) | 6 (14) | 7 (12) |
| Obsessive—compulsive disorder | 35 (10) | 11 (20) | 9 (8) | 8 (19) | 7 (12) |
| Reaction to stress/adjustment | 26 (8) | 5 (9) | 11 (10) | 2 (5) | 8 (13) |
| Mixed anxiety/depression | 6 (2) | 1 (2) | 3 (3) | 1 (2) | 1 (2) |
| Somatoform disorder | 6 (2) | 5 (9) | 0 (0) | 1 (2) | 0 (0) |
| Panic disorder | 3 (1) | 0 (0) | 1 (1) | 0 (0) | 0 (0) |
| Other | 27 (8) | 22 (39) | 3 (3) | 2 (5) | 2 (3) |
| Secondary ICD—10 diagnoses: n (%)1 | |||||
| None | 148 (44) | 42 (75) | 55 (51) | 23 (55) | 28 (47) |
| Depression | 26 (8) | 4 (7) | 14 (13) | 4 (10) | 4 (7) |
| Phobia | 24 (7) | 1 (2) | 9 (8) | 4 (10) | 10 (17) |
| Generalised anxiety disorder | 37 (11) | 0 (0) | 21 (19) | 7 (17) | 9 (15) |
| Obsessive—compulsive disorder | 8 (2) | 4 (7) | 4 (4) | 0 (0) | 0 (0) |
| Reaction to stress/adjustment | 5 (2) | 1 (2) | 0 (0) | 1 (2) | 3 (5) |
| Mixed anxiety/depression | 2 (1) | 0 (0) | 1 (1) | 0 (0) | 1 (2) |
| Somatoform disorder | 7 (2) | 1 (2) | 2 (2) | 0 (0) | 4 (7) |
| Panic disorder | 5 (2) | 0 (0) | 1 (1) | 2 (5) | 0 (0) |
| Other | 4 (1) | 3 (5) | 1 (1) | 1 (2) | 1 (2) |
| Single-Item Depression Scale score: mean (s.d.) | 4.9 (2.1) | 4.7 (2.1) | 4.7 (1.9) | 4.9 (1.9) | 5.3 (2.1) |
Of all 355 referrals, 191 (54%) were women and 121 (34%) were unemployed or students – the clinic was in a deprived area. Of the 139 patients who gave this information, 76 (54%) had a current partner and 52 (39%) had one or more children. At least 81% had completed basic education and 50% had a higher or further educational qualification.
Initial severity
The sample was very chronic with moderately severe problems. The mean problem duration was 8 years (s.d.=10) but it was over 10 years in about one-third of referrals; the mean score on the 0–8 Single-Item Depression Scale (Reference McKenzie and MarksMcKenzie & Marks, 1999; 0=hardly troubled by depression at all; 8=very severely disturbed/disabled) was 4.9 (s.d.=2), denoting moderate to severe depression. Work and social adjustment was moderate: a mean of 21 (s.d.=10) on the 0–40 WSA scale. Of 138 patients who gave this information, 54 (39%) had given up work or were on long-term sick leave because of their problem.
Current/past treatment
Of the 139 patients who gave data, about half (45%) were having current treatment from their GP or a mental health professional and about half were on psychotropic medication (Table 1). The vast majority (96%) had had past treatment for their problem; this had been CBT in only 20%.
Diagnoses
At the screening interview of 266 referrals, an experienced clinician made a primary and, if needed, secondary ICD–10 diagnosis (Table 1).
Primary diagnoses were (numbers of patients): 71, depression (40, recurrent depressive disorder; 22, depressive episode; 8, dysthymia; 1, other mood disorder); 57, phobia (3, agoraphobia; 16, agoraphobia with panic disorder; 17, social phobia; 21, specific phobia); 35, generalised anxiety disorder; 35, obsessive–compulsive disorder; 26, reaction to severe stress/adjustment disorder; 6, mixed anxiety/depressive disorder; 6, somatoform disorder; 3, panic disorder; 27, other.
Secondary diagnoses were made in 118 cases (44%): 26, depression (14, recurrent depressive disorder; 10, depressive episode; 2, dysthymia); 24, phobia (3, agoraphobia; 4, agoraphobia with panic disorder; 14, social phobia; 3, specific phobia); 37, generalised anxiety disorder; 8, obsessive–compulsive disorder; 7, somatoform disorder; 5, panic disorder; 5, reaction to severe stress/adjustment disorder; 2, mixed anxiety/depression; 4, other.
Compared with the suitable patients (Table 1), the 56 who were unsuitable at the screening interview had, as expected, significantly fewer primary diagnoses of depression, phobia, generalised anxiety disorder or obsessive–compulsive disorder and significantly more of the other primary diagnoses.
Computer literacy
Of the 135 patients for whom this information was available, 47 (35%) used computers most days at work, 16 (12%) ‘quite often’, 19 (14%) ‘often’, 41 (30%) ‘occasionally’ and 12 (9%) had never used computers before. Computer literacy did not differ between those in the unsuitable, refused, dropped out and completed categories or between FearFighter, Cope, Balance and BTSteps users, and did not correlate with outcome or satisfaction.
Clinical outcome
For all patients
For the 108 patients who had post-treatment data, clinical outcome on generic outcome measures appears in Table 2. Having been moderately disabled on the WSA at pre-treatment, post-treatment treatment the patients had improved significantly on the total WSA and each of its five items.
Table 2 Self-rated outcome: mean (s.d.) at pre- and post-treatment, 95% confidence intervals, percentage improvement and effect sizes for all patients with available post-treatment data (lower score=improvement)
| Scale | n | Pre-treatment | Post-treatment | Pre—post difference | Improvement %1 | Effect size2 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (s.d.) | Mean | (s.d.) | Mean | (95% CI) | Mean | (s.d.) | |||
| All (n=108) | ||||||||||
| Work and Social Adjustment (range: 0-40) | 107 | 20.6 | (9.6) | 14.7 | (9.5) | 5.9*** | (4.5 to 7.3) | 27.5 | (33.6) | 0.6 |
| Work (range: 0-8) | 86 | 4.2 | (2.7) | 3.5 | (2.5) | 0.7*** | (0.3 to 1.1) | 17.9 | (51.4) | 0.3 |
| Home Management (range: 0-8) | 90 | 3.5 | (2.2) | 2.4 | (2) | 1.1*** | (0.7 to 1.4) | 30.6 | (42.6) | 0.5 |
| Social Leisure (range: 0-8) | 90 | 4.8 | (2.3) | 3.2 | (2) | 1.7*** | (1.4 to 2) | 33.3 | (29.4) | 0.7 |
| Private Leisure (range: 0-8) | 90 | 3.9 | (2.3) | 2.6 | (2) | 1.3*** | (0.9 to 1.7) | 31.9 | (45.5) | 0.6 |
| Relationships (range: 0-8) | 90 | 4.1 | (2.3) | 2.8 | (2) | 1.2*** | (0.8 to 1.5) | 28.5 | (42.5) | 0.6 |
| FearFighter (n=27) | ||||||||||
| FQ Global Phobia (range: 0-8) | 25 | 5.6 | (1.7) | 3.2 | (1.6) | 2.3*** | (1.7 to 3) | 40.7 | (24.4) | 1.4 |
| FQ Total Phobia (range: 0-120) | 26 | 49.0 | (27.1) | 32.3 | (22.5) | 16.6*** | (12.1 to 21.2) | 39.9 | (24.8) | 0.6 |
| FQ Anxiety/Depression (range: 0-48) | 26 | 23.5 | (11.5) | 12.1 | (8.6) | 11.1*** | (7.6 to 14.6) | 47.3 | (25.7) | 1.0 |
| Work and Social Adjustment (range: 0-40) | 27 | 17.9 | (9.5) | 11.8 | (9.5) | 6.1*** | (3.9 to 8.3) | 36.4 | (39.0) | 0.6 |
| Cope (n=39) | ||||||||||
| Beck Depression Inventory (range: 0-63) | 23 | 27.4 | (9) | 16.2 | (7.1) | 11.2*** | (6.9 to 15.5) | 37.7 | (29.4) | 1.2 |
| HRSD (range: 0-51) | 30 | 16.8 | (5.2) | 13.3 | (6.2) | 3.5* | (0.9 to 6.1) | 15.2 | (41.9) | 0.7 |
| Work and Social Adjustment (range: 0-40) | 38 | 24.0 | (8.2) | 16.4 | (8.8) | 7.6*** | (4.6 to 10.6) | 29.4 | (31.1) | 0.9 |
| Balance (n=33) | ||||||||||
| Beck Anxiety Inventory (range: 0-63) | 30 | 20.7 | (11.9) | 13.4 | (9.3) | 7.3*** | (4.2 to 10.3) | 25.1 | (50.2) | 0.6 |
| Beck Depression Inventory (range: 0-63) | 28 | 22 | (10) | 15.6 | (6.8) | 6.3*** | (3.8 to 8.9) | 20.8 | (34.8) | 0.6 |
| Work and Social Adjustment (range: 0-40) | 33 | 20.0 | (9.6) | 16.0 | (9.8) | 4.0*** | (1.9 to 6.1) | 18.7 | (32.2) | 0.4 |
| BTSteps (n=9) | ||||||||||
| YBOCS Total (range: 0-40) | 9 | 23.2 | (7.4) | 14.0 | (8.1) | 9.2* | (1.6 to 16.7) | 35.7 | (42.5) | 1.2 |
| YBOCS Obsessions (range: 0-20) | 9 | 10.7 | (5.1) | 6.3 | (4.1) | 4.4* | (0.7 to 8.1) | 13.2 | (119.9) | 0.9 |
| YBOCS Compulsions (range: 0-20) | 9 | 12.4 | (3.5) | 7.6 | (5) | 4.7* | (-0.04 to 9.5) | 33.8 | (41.5) | 1.4 |
| Work and Social Adjustment (range: 0-40) | 9 | 17.2 | (12.4) | 12.1 | (10.2) | 5.1 | (-0.3 to 10.5) | 25.0 | (27.8) | 0.4 |
On the PGI scale at post-treatment (Table 3 and Fig. 2), 80% of patients rated themselves as better to some degree, 10% as unchanged and 9% as worse to some degree.
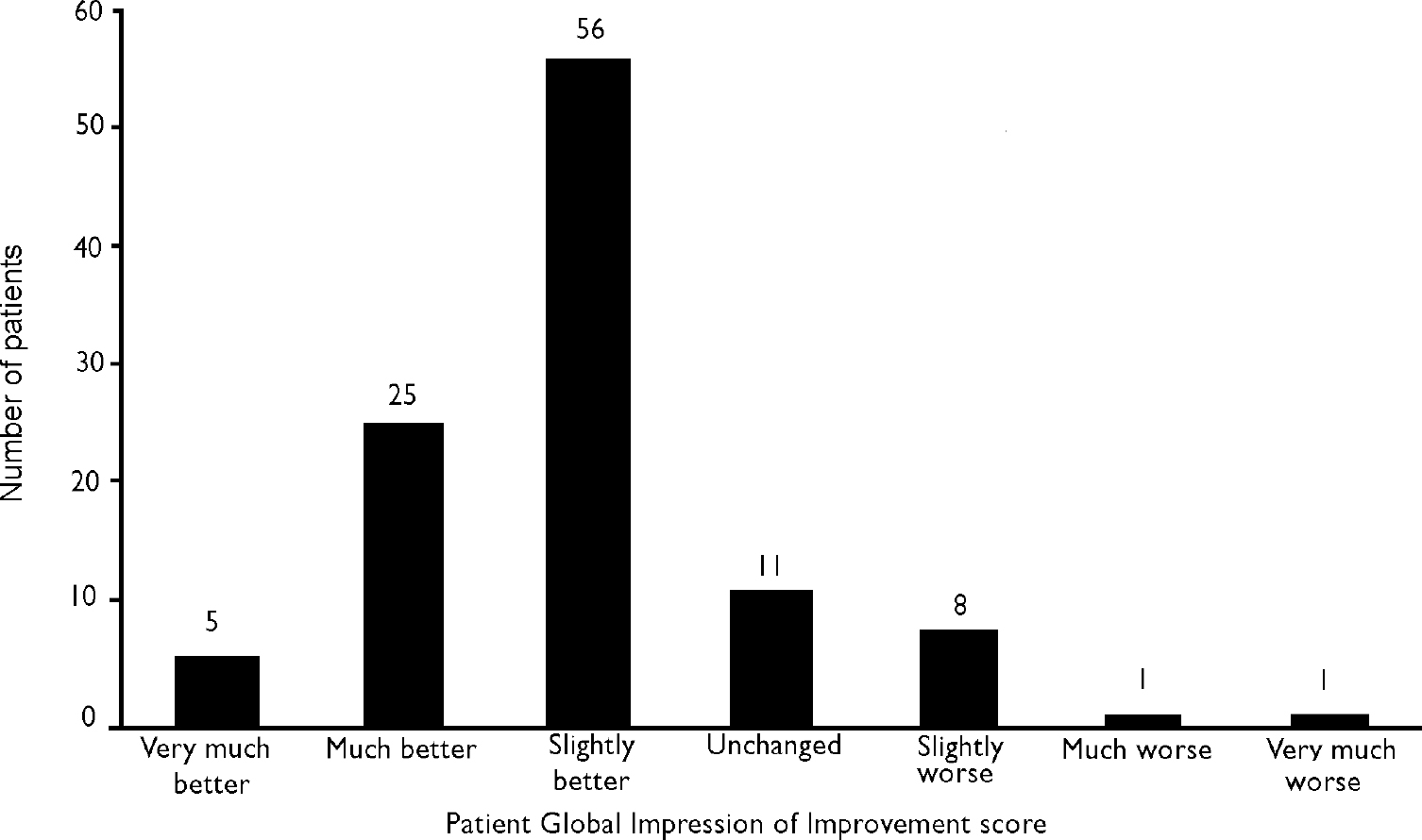
Fig. 2 Patient Global Impression of Improvement score at post-treatment (n=107).
Table 3 Patient Global Impression of Improvement scores self-rated at post-treatment
| All patients (n=107) | FearFighter (n=27) | Cope (n=39) | Balance (n=33) | BTSteps (n=9) | |
|---|---|---|---|---|---|
| Score (mean (s.d.)) | 2 (1) | 1.7 (0.6) | 2.4 (1.2) | 1.8 (0.7) | 1.3 (1.1) |
| Very much better (%) | 5 | 4 | 3 | 6 | 11 |
| Much better (%) | 23 | 22 | 21 | 15 | 67 |
| Slightly better (%) | 52 | 70 | 36 | 67 | 11 |
| Unchanged (%) | 10 | 4 | 18 | 9 | 11 |
| Slightly worse (%) | 8 | 0 | 18 | 0 | 0 |
| Very much worse (%) | 1 | 0 | 3 | 0 | 0 |
For users of each computer-aided CBTsystem
Separately per system, improvement on the WSA total score was significant for FearFighter, Cope and Balance users. Completers of each system also improved significantly from pre- to post-treatment on measures specific to their problem (Table 2). The clinically meaningful effect size of 0.8 or more was exceeded by FearFighter users on the Fear Questionnaire's global phobia and anxiety/depression scores, by Cope users on the BDI and the WSA and by BTSteps users on the YBOCS total score and the obsessions and compulsions sub-scores. Balance users did not attain this clinically meaningful effect size on any measure.
Patient satisfaction at post-treatment
For the 70 patients for whom full data were available, the mean ratings for the four questions of the satisfaction scale (each rated 0–8: 0=very good; 4=neutral; 8=very poor) were: technical aspects of their system, good to moderate (mean=3.1, s.d.=1.5); content and structure of their system, good to moderate (mean=2.7, s.d.=1.4); live support from a clinician, very good to good (mean=1.6, s.d.=1.5); clinic as a whole, good (mean=2; s.d.=1.5).
Patients were thus fairly satisfied with their computer-aided CBT system and even more satisfied with their live support and the clinic as a whole. In keeping with this, on how much of their treatment they would have preferred to have been guided by a therapist and how much by a self-help computer system (0–8 scale: 0=100% computer, 0% clinician; 4=50% computer, 50% clinician; 8=0% computer, 100% clinician) the mean rating was 4.9 (s.d.=2.2), suggesting a marginal preference for therapist over computer guidance. There were no significant differences in satisfaction or preference (therapist v. computer) between users of the different systems (data not shown).
Features of use of computer-aided CBT
A mean of 58 days (s.d.=49) elapsed from patients’ starting to ending the computer-aided CBT. Over that period they had a mean of 64 (s.d.=48) minutes of support from a clinician, of which 25 min (s.d.=23) were spent on extra treatment advice, 17 min (s.d.=15) on progress review, 16 min (s.d.=15) on general support, and only 6 min (s.d.=7) on technical support.
Table 4 shows patients’ use of each of the four computer-aided systems. Duration of use of Balance (the shortest and least interactive of the four) tended to be the shortest (P=0.1).
Table 4 Treatment duration, clinician support and mode of access for the completers of each computer-aided cognitive—behavioural therapy system
| FearFighter (n=27) | Cope (n=39) | Balance (n=33) | BTSteps (n=9) | |
|---|---|---|---|---|
| Treatment duration, days (mean (s.d.)) | 67 (22) | 65 (59) | 40 (51) | 63 (44) |
| Support time from clinician, minutes (mean (s.d.)) | ||||
| Total | 104 (25) | 46 (46) | 43 (36) | 81 (46) |
| Progress review | 20 (11) | 17 (17) | 12 (14) | 26 (15) |
| Extra treatment advice | 49 (19) | 14 (19) | 16 (14) | 24 (17) |
| General support | 23 (10) | 13 (15) | 11 (14) | 27 (19) |
| Technical support | 11 (7) | 3 (6) | 4 (6) | 4 (7) |
| Mode of access (n (%)) | ||||
| Self-help clinic | 16 (59) | 0 (0) | 18 (54) | 0 (0) |
| Home telephone | 0 (0) | 39 (100) | 0 (0) | 9 (100) |
| Home internet | 10 (37) | 0 (0) | 0 (0) | 0 (0) |
| Home personal computer | 0 (0) | 0 (0) | 13 (39) | 0 (0) |
| Other | 1 (4) | 0 (0) | 2 (6) | 0 (0) |
FearFighter patients had more general therapist support (P<0.001) than Cope and Balance patients and more extra treatment advice and technical support (both P<0.001) than users of the three other systems. Patients who used FearFighter at the clinic (n=17) needed significantly less technical support time than those who used it on the internet (n=10) in the first pilot test of the internet version (mean difference =–6.5; 95% CI –12.3 to –0.7; t=–2.3, d.f.=24, P=0.03).
About half of the patients had live support by telephone and half had support face to face at the clinic. The live support by telephone was given to users of the Cope and BTSteps IVR systems, of FearFighter on the internet and of Balance on a CD–ROM.
Patients’ known total time spent interacting with the computer were: FearFighter on a stand-alone PC (n=17), 266 min (s.d.=71) over a mean of five sessions (s.d.=1, range 2–7); Cope (n=39), 122 min (s.d.=83) spent on IVR phone calls over a mean of 11 calls (s.d.=8, range 0–34); Balance (n=23) for patients using it at the clinic, 100 min (s.d.=72) over two sessions (s.d.=2, range 0–9); BTSteps (n=9), 235 min (s.d.=151) spent on IVR phone calls over a mean of 32 calls (s.d.=26, range 5–69).
DISCUSSION
Effect on throughput and patient time per clinician
During the clinic's year of intake the full-time equivalent of one clinician dealt with 355 referrals, delegated most therapy tasks to computer-aided CBT and, apart from 30 min of screening, gave a per-patient overall mean of about 1 h of support over 12 weeks. Throughput per clinician at the clinic thus far exceeded the 50 referrals a year that CBT therapists screen and treat on average (Reference MarksMarks, 1985), although therapists vary greatly in their throughput. The clinic's patient mean of 1 h of support from a clinician is far below the mean of at least 8 h per clinician usually needed by these types of patient having CBT.
The clinic's greater throughput of patients per therapist with the help of computer-aided CBT and shorter patient time per clinician did not appear to sacrifice effectiveness. Individuals with anxiety and depression improved significantly and clinically meaningfully, and were fairly satisfied with computer-aided CBT despite a marginal preference for face-to-face care. When GPs nearby and a secondary CBT service recommended the clinic to many patients, this reduced the GPs’ referrals to secondary mental health services and slightly shortened the waiting list for face-to-face CBT in secondary care (Reference Kaltenthaler, Shackley and BeverleyKaltenthaler et al, 2002).
Patients who accessed the computer by telephone spent very similar total times calling the computer as in previous studies (Reference Osgood-Hynes, Greist and MarksOsgood-Hynes et al, 1998; Reference Kenwright, Liness and MarksKenwright et al, 2001; Reference Greist, Marks and BaerGreist et al, 2002): 2 h on Cope calls and 4 h on BTSteps calls.
Some of the outcomes in the present study can be compared with those in past studies of computer-aided CBT.
For FearFighter completers, pre- to post-FearFighter improvement and effect size (ES) on the Fear Questionnaire Global Phobia item were 41% (ES=1.4) of our sample compared with 54% (ES=1.3) in Kenwright et al (Reference Kenwright, Liness and Marks2001) and 38% (ES=1.7) in Marks et al (Reference Marks, Kenwright and McDonough2003). Our FearFighter users’ figures of 41% improved (ES=1.4) compared with figures for face-to-face CBT of 37% (ES=1.2) in Kenwright et al (Reference Kenwright, Liness and Marks2001) and 51% (ES=2.8) in Marks et al (Reference Marks, Kenwright and McDonough2003).
For Cope completers, pre- to post-Cope improvement on the Patient Global Impression of Improvement scale was a mean of 2.4 in our patients compared with 3.1 in Osgood-Hynes et al (Reference Osgood-Hynes, Greist and Marks1998), after correcting the latter's 1–7 range to our 0–6 range.
For BTSteps completers, pre- to post-improvement on the YBOCS was 40% (ES=1.2) in our sample compared with 23% (ES=1.3) in Greist et al (Reference Greist, Marks and Baer2002), and compared with 32% (ES=1.7) in patients who had had face-to-face CBT in Greist et al (Reference Greist, Marks and Baer2002).
Thus, the patients who completed computer-aided CBT in our study improved broadly comparably to completers in other studies which used the same systems and measures. Only in the RCT of Marks et al (Reference Marks, Kenwright and McDonough2003) did face-to-face care yield an appreciably better effect size than that of the computer-aided care in the present study.
Rates of non-attendance, unsuitability and non-completion
Of the self-referrals who were offered a screening interview, 19% did not attend. This is well below the 48% non-attendance rate for brief psychiatric screening of less-severe mental health problems (Reference Hamilton, Gordon and NajiHamilton et al, 2002) and an out-patient anxiety disorders clinic offering CBT (Reference Kenwright and MarksKenwright & Marks, 2003). Although we did not specifically measure this, we had the impression that rates of non-attendance were higher for patients already on a waiting-list for face-to-face CBT in secondary care.
The 79% suitability rate at screening interview was satisfactory. The combined rate of 20% who refused plus 29% of patients who began computer-aided CBT but gave no post-treatment data was higher than the equivalent for outpatients having CBT for anxiety disorders (Reference Marks, Blanes and McKenzieMarks et al, 1995). Non-completers had resembled completers on initial severity and other variables.
There is no ideal way to analyse patients who began computer-aided CBT but gave no post-treatment data (Reference EverittEveritt, 1998). It can be misleading to carry forward their baseline data on the assumption that outcome stayed frozen thereafter (Reference EverittEveritt, 1994). Assuming that none improved would ignore those who gave no data but said that after dropping out they continued the self-help they had learned and benefited from. Many non-completers did not answer repeated phone and postal requests for post-baseline ratings. Patients undergoing self-help at home with access to a live helpline had no incentive to attend the clinic or give ratings.
Cost-effectiveness
A rough cost comparison of computer-aided CBT with purely face-to-face CBT assumed the same throughput of patients managed per therapist using the computer-aided therapy as in the clinic, a £61/h cost of a CBT therapist (Reference Netten and CurtisNetten & Curtis, 2000) and the licence costs of computer-aided CBT used by the National Institute for Clinical Excellence (2002). Assuming administrative costs similar to those of the clinic and 15% overheads, the estimated per-patient cost advantage of computer-aided CBT over face-to-face CBT would rise from about 15% per patient for 350 patients a year to 41% per patient for 1350 patients per year. This advantage rises with volume savings as the number of patients rises, and discounts any value from computer-aided CBT at home giving patients immediate rather than delayed access to CBT, unrestricted access, easier disclosure of sensitive information, and removal of the need to travel to a therapist. This rough estimate of cost-effectiveness needs to be checked in a more formal study.
In contrast to its lower per-patient cost, the total cost of computer-aided CBT nationally might rise if previously untreated users sought the therapy in such numbers as to offset savings from lower per-patient costs. Sufficiently widespread dissemination of computer-aided CBT might eventually reduce demands on GP and secondary services and lessen medication use and chronicity.
Wider implications
Computer-aided CBT is developing rapidly. Patients can now help themselves entirely at home by accessing two of the four computer-aided CBT systems used by the clinic on the internet (patients without home internet access can use a link in public libraries, computer learning centres, internet cafés, etc.) and the other two by telephone. Those who get stuck during self-help can get support from a clinician on a live helpline.
As referrals can now be screened for suitability to engage in computer-aided CBT and supported by clinicians entirely by telephone while doing computer-aided CBT at home, self-help clinics could act as call centres for wide catchment areas. How many such centres would be needed to cover an entire country might be inferred from the experience of NHS Direct call centres.
Computer-aided CBT systems are ‘clinician extenders’, not ‘clinician replacers’. Because patients using these systems need screening and brief advice, training is needed to equip clinicians to work in this area. The training might take only 2 days per system and so be inexpensive. Trainees can work through each system systematically, posing as patients who have relevant problems (Reference McDonough and MarksMcDonough & Marks, 2002). The lack of such trained personnel is a barrier to the dissemination of computer-aided CBT.
The model suggested is stepped care, with computer-aided CBT self-help plus brief live helpline advice as a potential first port of call for most individuals with anxiety/depression. Those who fail to improve sufficiently with computer-aided CBT could go on to have entirely live clinician-guided help by telephone or face to face.
Some might benefit from posted self-help instructions (Reference Burgess, Gill and MarksBurgess et al, 1998) or self-help books, perhaps with access to a live helpline. Books may cost less than computer-aided CBT but they are less interactive and harder to modify and to disseminate on a large scale. It is also hard to track the progress of patients who are using books, whereas computer-aided CBT on the internet or a central IVR computer eases the audit of outcome on a mass scale.
Mental health inequalities might lessen with widespread access to computer-aided CBT self-help, given that almost two-thirds of the clinic's referrals came from the three lowest socio-economic groups and that initial computer illiteracy did not affect outcome.
Although the present study found that computer-aided CBT self-help at a single clinic supporting patients from a wide area was effective and acceptable, other models for implementation of the technology may work as well. Supporting patients on self-help systems full time may bore highly trained therapists (the clinic therapists spent only half of their time in patient contact). Computer-aided CBT could be integrated into existing therapist services, with clinicians perhaps dedicating 1 day a week to supporting patients doing computer-aided CBT who might otherwise wait months or years to get CBT in their service. A major obstacle to dissemination is the current reluctance of health service managers to fund computer-aided CBT. The clinic's time-limited funding came to an end. It can take a long time for socio-political processes to be worked through to make new technologies a routine aspect of health services.
Limitations
Although an open pragmatic evaluation like the present project may tell more about implementation issues than does an RCT, it cannot say how much of the patients’ self-rated improvement was due to the passage of time, contact with a service, CBT, computer-aided CBT or the brief help given by a clinician, nor is it known whether similar benefit might have accrued from offering an appropriate CBT self-help book plus access to a helpline. Also unclear is the potential effect of psychotropic medication, which about half of the patients were on at the start and had often been on for a long time; this is inevitable in any regular service.
Our study could not tell what proportion of all sufferers in the community might want computer-aided CBT as their first option in a stepped-care service instead of an immediate or a delayed interview with a live therapist by telephone or face to face. Nor could our study say whether costs might drop still further without impairing effectiveness if the brief advice given to computer-aided CBT users was from less-highly trained supporters (e.g. the new primary care health workers coming on stream) and if most screening was done via a questionnaire without a back-up live interview.
The amount of improvement should be regarded with some caution because of the high rate of refusal plus non-completion, even though completers and non-completers had been indistinguishable at the start.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ People with anxiety/depression can rapidly access effective cognitive–behavioural therapy (CBT) at home by doing mainly computer-aided self-help.
-
▪ Outcome with CBT self-help guided mainly by computer in regular care resembles that in controlled studies and that with purely clinician-guided care.
-
▪ Computer-aided CBT cuts clinicians’ per-patient time, and its cost advantage over purely clinician-guided CBT rises with the number of patients taking part.
LIMITATIONS
-
▪ The study was unrandomised and uncontrolled so any improvement might not be due to the intervention, and not many referrals completed each computer-aided CBT system.
-
▪ Computer-aided CBT still involves a clinician briefly screening and then supporting users, all of which can be done by telephone.
-
▪ Health authorities are wary of funding computer-aided CBT.
Acknowledgements
Funding was by the Hillingdon Primary Care Trust and London Research and Development Region. D.M.-C. was supported by a European Union Marie Curie Fellowship. STSolutions supported the use of Fearfighter, and Health Care Technology Systems supported the use of Cope and of BTSteps.









eLetters
No eLetters have been published for this article.