This study examines the implications of a poor early course for the long-term prognosis of schizophrenia in a developing country setting. The data are drawn from a 15-year follow-up of two incidence cohorts in urban and rural Chandigarh, India. The cohorts were originally established as part of the World Health Organization (WHO) Determinants of Outcome of Severe Mental Disorders (DOSMeD) study. In this sample, we previously examined the long-term prognosis of a group of psychoses with acute onset and favourable early course (Reference Susser, Varma and MattooSusser et al, 1998). We now examine the long-term prognosis of psychoses at the other end of the spectrum of early course — that is, psychoses with a poor early course. We compare patients with a poor 2-year course (i.e. continuous psychotic illness at the 2-year follow-up) with patients with other 2-year course types with regard to long-term course and mortality.
METHOD
The methods of the DOSMeD are described elsewhere (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). Briefly, in defined catchment areas, investigators were to include over a 2-year period all first-contact patients presenting with a psychotic disorder to a helping agency. Patients ranged in age from 15 to 54 years. The Chandigarh sites were the only developing country sites in the DOSMeD study where coverage of the catchment areas was sufficient for the samples to be considered as incidence cohorts (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). Although both of these sites are in the same region of India, they represent different sociocultural contexts. The rural catchment area in Chandigarh is a green fertile region in Ambala District (Harayan State), which although more prosperous than many rural Indian locales, has a 56% literacy rate. Urban Chandigarh, on the other hand, is one of the most modern cities in India (for more information see Reference Day, Nielsen and KortenDay et al, 1987; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992; Reference Collins, Varma and WigCollins et al, 1999).
Patients were followed up and reinterviewed at 2 years as part of the DOSMeD study and at 15 years as part of another WHO-sponsored international study (Reference Sartorius, Gulbinat and HarrisonSartorius et al, 1996). At the 15-year follow-up, patient cohorts established in Chandigarh and a number of other sites in the DOSMeD and other WHO studies were reassessed using a comprehensive set of standardised instruments in addition to instruments used in the original DOSMeD study. The key instrument for rating the course of illness at the 15-year follow-up was the Life Chart Schedule (LCS; Reference Susser, Finnerty and MojtabaiSusser et al, 2000). An abbreviated form of this instrument, the Broad Rating Schedule (BRS; Reference Sartorius, Gulbinat and HarrisonSartorius et al, 1996), was used to rate the course of illness for deceased patients and patients lost after the 2-year follow-up.
Sample
Two hundred and nine patients were originally recruited into the urban and rural sites combined. Of these, 171 (82%) had a rating of course of illness at the 2-year follow-up. Ninety-one (53%) of the 171 were male and 80 (47%) were female; 118 (69%) were from the urban site and 53 (31%) from the rural site; the average age of these patients at baseline was 26.7 years (s.d.=9.4).
One hundred and eleven (65%) of the 171 patients could be interviewed directly at the 15-year follow-up using the LCS. Twenty-four (14%) of the 171 had died by that time; a rating of the course of illness up to the time of death was made using the BRS. For another 19 (11%) patients who could not be located for the 15-year follow-up interview, information on the course of illness for up to an average of 10.5 (s.d.=3.3) years was available. For these patients too, a rating of course of illness was made using the BRS. In summary, information on the long-term course of illness was available for 154 (90%) of the 171 patients. Long-term course information was not available for 17 patients. Five of these were located but refused a follow-up interview, and another 12 were lost to follow-up with no information on the course of illness after the 2-year follow-up.
The sample for examining the association of the 2-year course and mortality comprised all 171 patients for whom information on the 2-year course, vital status and time of death was available. Of these, 15 had a poor 2-year course and 156 had other course types. The sample for examining the association of the 2-year and the long-term course comprised 154 of the 171, namely those for whom information on the long-term course was available. Of these, 13 had a poor 2-year course and 141 had other course types.
Ratings of course
Course in the first 2 years of follow-up was assessed using ratings of pattern of course on the Psychiatric and Personal History Schedule (PPHS; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). The PPHS was administered by a mental health professional, often a psychiatric social worker or a psychiatrist who usually also interviewed a key informant. Ratings of pattern of course had excellent interrater reliability (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). The ratings included seven patterns of course in addition to continuous course (see Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). For the purpose of this study, a poor 2-year course was operationalised as a rating of continuous psychotic illness (no remission) with psychotic symptoms present most of the time. A poor 2-year course was contrasted with other 2-year course types that included all other course patterns.
Course of illness for subjects who participated in the 15-year follow-up was assessed using the LCS (Reference Susser, Finnerty and MojtabaiSusser et al, 2000) — a standardised instrument that provides detailed ratings on the course of illness in multiple domains, including residence, work, symptoms and treatment. The instrument was administered by a mental health professional, often a psychiatric social worker or psychiatrist. The LCS ratings have shown good interrater reliability (Reference Susser, Finnerty and MojtabaiSusser et al, 2000), with excellent reliability for course of illness ratings (κ=0.90). The course ratings covered the period since intake and included three course types in addition to the continuous course type. For the purpose of this study, poor long-term course was operationalised as a rating of psychotic over most of the period. If there were any remissions, these were brief (not longer than 6 months). A poor long-term course was contrasted with other long-term course types that included all other course patterns.
Ratings for the deceased and patients with partial follow-up were made using the BRS. The format of the items used for rating the course of illness on this abbreviated instrument was identical to that used in the LCS. All available information, including medical records and interviews with relatives (for deceased patients), were used to make these ratings.
Rating, time and cause of death
Rating of death and its time and cause were based on personal interviews with the patient's survivors and supplemented by a review of medical records, where available. No death register is available for this region.
Data analysis
Association of the 2-year course with the long-term course was examined in two steps. First the risk for poor long-term course was compared between patients with a poor 2-year course and those with other 2-year course types by computing relative risks. Next, to control for the effect of potential confounding variables, the association between 2-year and long-term course was assessed using logistic regression in which the long-term course was the dependent variable and the 2-year course was the independent variable. The following variables were also included in the model to control for their effects: gender, urban v. rural setting, narrow (S+) v. broad (Non-S+) definitions of schizophrenia (Reference Wing, Cooper and SartoriusWing et al, 1974; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992) and the interval between onset and intake into the study (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992).
Association of the 2-year course with mortality was examined by two different methods. First, mortality rates were compared among patients with a poor 2-year course v. other 2-year course types. Age-standardised mortality rate ratios and 95% confidence intervals were computed using the age distribution of the group with other 2-year course types as the standard. The numerator for computation of mortality rate was the number who died, and the denominator was the number of person-years. Patients who were followed up to 15 years contributed 15 person-years, and those who died or were lost to follow-up before the 15-year follow-up contributed up to the time of death or loss to followup (the time-point when the research team last had any information about the patient). The Epitab routine of the Stata 6.0 computer program for Windows (StataCorp, 1999) was used for computation of the age-standardised rate ratio. Next, Kaplan-Meier survival curves were used to display visually the mortality risk among patients with a poor 2-year course v. other course types. The log-rank test was used to assess the statistical significance of differences in the survival rates of the two groups.
RESULTS
Association of the 2-year course with the long-term course
As noted above, the sample for examining the association of the 2-year course and the long-term course comprised 154 patients — 13 with a poor 2-year course and 141 with other 2-year course types. Of the 13 with a poor 2-year course, 12 (92%) had a poor long-term course. Similarly, of the 141 with other 2-year course types, 128 (91%) had other longterm course types. Thus, a poor 2-year course was highly predictive of a poor long-term course (relative risk=9.3, 95% CI 5.5-15.7). Results of the logistic regression also showed that a poor 2-year course was highly predictive of a poor long-term course even after controlling for the potential effects of gender, urban/rural setting, narrow v. broad definitions of schizophrenia and the interval between onset and intake into the study (Table 1). Furthermore, with the variable of poor 2-year course in the model, none of the other predictor variables had a statistically significant coefficient. The adjusted odds ratio for the poor 2-year course was extremely large (93.9) because the outcome of interest (i.e. poor long-term course) was very common among patients with the exposure (i.e. poor 2-year course).
Table 1 The results of multiple logistic regression for examining the association of poor 2-year course with poor long-term course in 154 patients with schizophrenia in urban and rural Chandigarh, India. The variables of gender, urban v. rural setting, narrow (S+) v. broad (Non-S+) definitions of schizophrenia and the time interval between onset and intake into the study were also entered into the regression model to control for their effects
| Variables | Coefficient (β) | Standard error | Z test | P value | Adjusted odds ratio (95% CI) |
|---|---|---|---|---|---|
| Poor 2-year course | 4.5 | 1.1 | 4.0 | <0.001 | 93.9 (9.5-931.1) |
| Male gender | 0.5 | 0.6 | 0.8 | 0.41 | 1.6 (0.5-4.8) |
| Urban setting | -0.1 | 0.6 | -0.2 | 0.82 | 0.9 (0.3-2.7) |
| Narrow schizophrenia (S+) | -0.3 | 0.6 | -0.5 | 0.61 | 0.7 (0.2-2.5) |
| Interval between onset and intake ≥ 6 months | 0.3 | 0.7 | 0.4 | 0.72 | 1.3 (0.3-5.5) |
| Intercept | -2.3 | 0.6 | - | - | - |
Association of the 2-year course with mortality
As noted above, the sample for examining the association of the 2-year course with mortality comprised 171 patients — 15 with a poor 2-year course and 156 with other 2-year course types. Of the 15 with a poor 2-year course, 7 (47%) had died before the 15-year follow-up. Of the 156 with other course types, on the other hand, only 17 (11%) had died by that time. The difference in the proportion of patients who had died was statistically significant (χ2=14.5, d.f.=1, P<0.001). The age-standardised mortality rate ratio for patient groups with a poor 2-year course over the other 2-year course types was 9.4 (95% CI 3.8-23.7) (Table 2, column 7). As the age-specific mortality rate ratios reported in column 6 of Table 2 show, the increased mortality was evident in all age groups. After excluding suicides, the agestandardised mortality rate ratio was 8.7 (95% CI 3.0-25.4).
Table 2 Mortality rates according to the 2-year course type in 171 patients with schizophrenia in urban and rural Chandigarh, India. The age-standardised rate ratio was computed using the age distribution of the group with the ‘other course types’ as the standard

| Age range, years | Poor 2-year course | Other 2-year course types | Incidence rate ratio; rate for poor course/other course types | |||
|---|---|---|---|---|---|---|
| Number died/person-years | Crude rate per 10 000 per year | Number died/person-years | Crude rate per 10 000 per year | Crude (95% CI) | Age standardised (95% CI) | |
| 15-24 | 2/52 | 385 | 6/1023 | 59 | 6.6 (0.6-36.7) | - |
| 25-34 | 2/47 | 426 | 4/602 | 67 | 6.4 (0.6-44.7) | - |
| 35+ | 3/9 | 3333 | 7/287 | 244 | 13.7 (2.3-59.9) | - |
| Total | 7/108 | 648 | 17/1912 | 89 | 7.5 (2.6-18.9) | 9.4 (3.8-23.7) |
The increased risk of mortality among patients with a poor 2-year course is illustrated visually by Kaplan—Meier survival curves in Fig. 1. Similar to the incidence rate ratio, the log-rank test indicated a statistically significant difference in the risk of mortality for the two groups (test statistic=4.0, P<0.001).
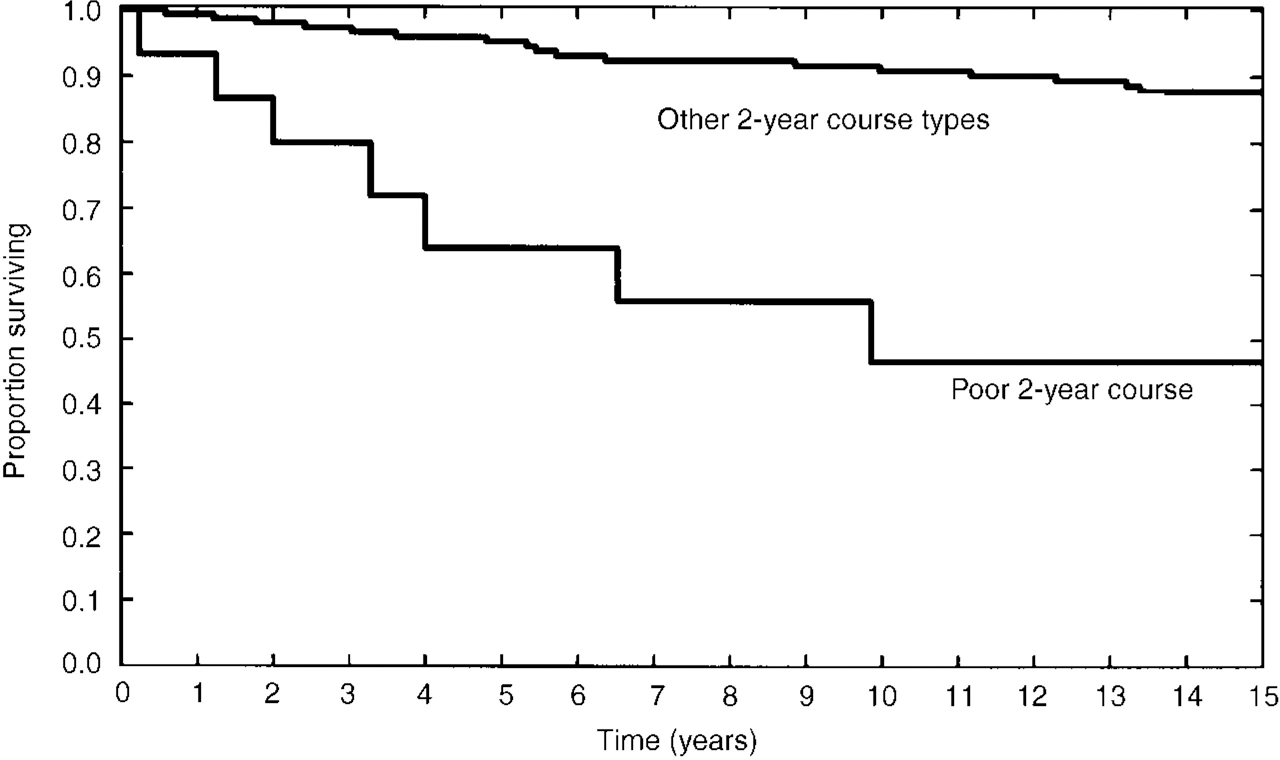
Fig. 1 Risk of death according to the 2-year course type in 171 patients with schizophrenia from urban and rural Chandigarh, India.
For subjects who died the median time to death was 4.8 years after intake (3.3 years for the group with the poor 2-year course and 5.4 years for the group with other 2-year course types). Out of the seven deaths among patients with a poor 2-year course, the specific causes of death in six patients were known. These were suicide (two cases), acute nephrotic syndrome superimposed on malnutrition (one case), infectious gastroenteritis superimposed on malnutrition (one case), respiratory arrest associated with asthma (one case) and viral pneumonia (one case). The specific cause of one death was not known but the available information indicated a natural cause.
Out of the 17 deaths among patients with other 2-year course types, the specific causes of death in 11 were known. These were suicide (three cases), traffic accident (one case), renal failure (one case), stroke (two cases), heart failure (one case), acute myocardial infarction (one case), septicaemia (one case) and heat stroke (one case). In five of the six remaining deaths for which the specific causes were not known, the available information indicated natural causes. In one case, it could not be ascertained whether death was due to a natural cause or suicide.
DISCUSSION
Previous studies from some developing country settings have suggested that on average there is a better prognosis for schizophrenia in such settings (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992; Reference WarnerWarner, 1994). None the less, in this developing country setting, we found that the subtype of patients with a poor 2-year course had a very poor prognosis in the long term. These patients tended to have a chronic course of illness and were at very high risk of premature death. Findings from this study have implications for the long-term course of schizophrenia and the mortality associated with this illness.
Long-term course
Of patients with a poor 2-year course, defined as a rating of continuous psychotic illness at the 2-year follow up, 92% had a poor course in long-term follow-up, which in most cases extended up to 15 years. This finding is consistent with the 13-year follow-up study in the Nottingham site of the DOSMeD project (Reference Harrison, Croudace and MasonHarrison et al, 1996), which reported a poor long-term prognosis for patients with continuous psychotic course at the 2-year follow-up. Although fewer patients in developing country settings compared to industrialised settings have a poor 2-year course (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992), this course pattern appears to be highly persistent across vastly different settings.
This finding might also have implications for aetiological research. The great diversity in the course and outcome of psychoses classified under the general rubric of schizophrenia is highly suggestive of aetiological heterogeneity (Reference Tsuang and FaroneTsuang & Farone, 1995). Findings from this study, as well as our earlier work (Reference Susser, Varma and MattooSusser et al, 1998) in which we examined the long-term course of psychoses with remitting course and acute onset, lend validity to the differentiation of some course patterns that are evident even in the early stages of illness.
Mortality
The high rate of mortality among patients with a poor 2-year course is alarming. Most studies of mortality in schizophrenia have been conducted in industrialised settings (e.g. Reference Simpson and TsuangSimpson & Tsuang, 1996; Reference BrownBrown, 1997; Reference Ringbäck Weitoft, Gullberg and RosenRingbäck Weitoft et al, 1998) and we were not able to locate any previous mortality studies in an incidence cohort from a developing country setting. In his 10-year follow-up study of a cohort of 101 patients in the Colombian site of the International Pilot Study of Schizophrenia, León (Reference León1989) reported only two deaths. However, that setting might be better classified as semi-industrialised (Reference Leff, Sartorius and JablenskyLeff et al, 1992). Furthermore, the cohort was not an incidence cohort and the duration of follow-up was shorter than in our study. Previous studies in industrialised settings generally compared subtypes or categories based on cross-sectional symptomatology and produced conflicting and overall weak effects (Reference Black, Warrack and WinokurBlack et al, 1985; Reference Wood, Evenson and ChoWood et al, 1985; Reference Allebeck and WistedtAllebeck & Wistedt, 1986; Reference Black and FisherBlack & Fisher, 1992). The magnitude of the effect for the schizophrenia subtypes in those studies was much smaller than the effect of early poor course of illness in the present study. Westermeyer et al (Reference Westermeyer, Harrow and Marengo1991) conducted one of the few studies that examined the relationship of early course with long-term mortality. In a 13-year follow-up study from Chicago, these authors compared the suicide rates of patients with chronic and sub-chronic v. acute and sub-acute schizophrenia, diagnosed according to the Research Diagnostic Criteria (Reference Spitzer, Endicott and RobinsSpitzer et al, 1978). All of the suicides in this group of patients occurred in the subgroup with a chronic or sub-chronic illness.
Implications for services
The high mortality rate among patients with a poor 2-year course raises questions about the adequacy of care for this group of patients. In at least two cases of death, the terminal illness was superimposed on malnutrition, indicating that the unmet needs of these patients for such basic necessities as food had contributed to their deaths. The better overall course and outcome of schizophrenia in developing countries should not distract us from the special needs of this small but highly vulnerable group of poor-prognosis patients. The endemic poverty of many developing country settings might affect this group of patients to a much greater extent than other patient groups (Reference Desjarlais, Eisenberg and GoodDesjaralais et al, 1995). Because long-term residential care is scarce or non-existent in most developing country settings, the burden of caring for these patients often falls entirely upon the shoulders of their families (Reference Susser, Collins and SchanzerSusser et al, 1996). A daunting challenge facing mental health professionals and policy makers in such settings is to recognise and accommodate the special needs of the families of poor-prognosis patients.
Some information was available on the course of medication treatment for 7 out of 15 patients with a poor 2-year course in the sample for examining the association of course with mortality. Of these, only three had received treatment for most or all of the follow-up period. These data raise concerns about the continuity of treatment in this setting for patients with a poor course of illness.
Limitations
The findings from this study need to be considered in the context of its limitations. First, not all of the members of the 2-year cohort could be interviewed for the 15-year follow-up. For the deceased patients and those who were lost to follow-up, the long-term course rating was based on a review of medical records and/or interview with relatives. Ratings based on these sources might not be as reliable as a direct and detailed follow-up interview. It is reassuring, however, that the findings with regard to the association of 2-year course with long-term course were similar for patients with a complete 15-year followup (data not shown).
Second, the term ‘developing country’ is often applied to settings with very different sociocultural, economic and care provision characteristics. Across these settings, one might expect differences with regard to association of short-term course with long-term course and mortality. Therefore, in generalising from this study to other developing country settings, great caution is called for. It is noteworthy, however, that we detected no meaningful differences between the urban and rural settings with regard to the association of short-term course with long-term course and mortality (data not shown). As noted earlier, urban and rural Chandigarh represent different sociocultural settings.
Third, in this setting, as in most other developing settings, no death register is available. Therefore, information on death, its timing and its cause was obtained from relatives and medical records, where available. Data obtained from these sources are less standardised than data from a death register, although perhaps more detailed.
Finally, the number of patients with a poor 2-year course was limited to 13 for examining the association of the 2-year with the long-term course and to 15 for examining the association of the 2-year course and mortality. Before replication in other studies with larger samples, the results of this study need to be interpreted with caution.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ In this developing country setting, similar to industrialised settings, a poor 2-year course is a strong predictor of poor long-term course.
-
▪ Patients with a poor 2-year course in this developing country setting are at much higher risk of mortality in the long term.
-
▪ Patients with a poor 2-year course comprise a highly vulnerable subgroup of individuals with schizophrenia who, in addition to psychiatric care, need food, shelter and medical care on a long-term basis.
LIMITATIONS
-
▪ For the deceased patients and those who were lost to follow-up, the long-term course rating was based on a review of medical records and/or interview with relatives, which might not be as reliable as interviewing the patients themselves.
-
▪ Developing countries vary considerably in sociocultural, economic and care provision characteristics. Therefore, the results of this study may not generalise to other developing country settings.
-
▪ Ascertainment of timing and cause of death was based on interviews with relatives and medical records, where available. Data obtained from these sources are less standardised than registry data.
ACKNOWLEDGEMENTS
This paper uses the data obtained during the Determinants of Outcome of Severe Mental Disorder (DOSMeD) project. The DOSMeD study was supported by the World Health Organization, the US National Institute of Mental Health (grant MH29969) and the collaborating research centres. The chief collaborating investigators at the 12 field research centres of this study were: E. Strömgren (Aarhus), K. C. Dube (Agra), C. León (Cali), N. N. Wig (1976-1980, Chandigarh), V. Varma (1980-1996, Chandigarh), D. Walsh (Dublin), A. Marsella (Honolulu), M. Katz (coordinator for the two US centres, Honolulu), M. Olatawura (Ibadan), R. A. Nadzharov and N. N. Zharikov (Moscow), R. Takahasi (1976-1984, Nagasaki), Y. Nakane (1984 to the present, Nagasaki), J. E. Cooper (Nottingham), L. Hanzlicek (1976-1981, Prague), C. Skoda (1982 to the present, Prague), L. C. Wynne and T. Gift (Rochester). At WHO Headquarters, Geneva, the study was coordinated by N. Sartorius (principal investigator) and A. Jablensky (co-principal investigator). Subsequently, follow-ups of the cohort were carried out with support from the Indian Council of Medical Research (ICMR). We thank the ICMR and the Chandigarh Postgraduate Institute of Medical Education and Research for technical help and financial support. We also thank the health administrations and the field staff of Chandigarh Union Territory and Raipur Rani Block, Ambala District, Haryana, for their help and cooperation in conducting this study. R.M.'s work was supported in part by Research Career Award K01-MH01754 from the National Institute of Mental Health, Rockville, MD, and by a National Alliance for Research on Schizophrenia and Depression Young Investigator Award. E.S.S.'s work was supported in part by Schizophrenia Research Centre Grant 5P20-MH50727 and the Lieber Centre.






eLetters
No eLetters have been published for this article.