Major depression and borderline personality disorder are both characterised by distorted perception of the intentions of others, which leads to impaired social functioning. Reference Surguladze, Young, Senior, Brebion, Travis and Phillips1–Reference Daros, Zakzanis and Ruocco3 Mental state decoding – the ability to attribute mental states to social partners from perceivable social information such as tone of voice, body posture or facial expression – provides an important tool for maintaining social relations and cooperation. Human facial cues of the eyes provide one of the most important signals of mental states. Reference Baron-Cohen4 The Reading Eyes in the Mind Test (RMET) Reference Baron-Cohen4 is a test that matches semantic definitions of mental states to pictures of the eye region with emotionally valenced positive, negative or neutral expressions. This comprehensive method measures mental state decoding abilities in different disorders. Inaccurately inferring mental states from facial cues leads to distorted interpretations of other people's intentions, which can cause problems in social functioning. Previous studies analysing impaired mental state decoding abilities in depression and borderline personality disorder have produced contradictory results. Suggestions of specific links between distorted perception of the intentions of others and depression can be found in cognitive–behavioral, Reference Beck, Rush, Shaw and Emery5 psychodynamic Reference Blatt and Levy6 and mentalisation-based Reference Fonagy and Luyten7 theories. Some studies indicate that patients with depression exhibit impaired RMET performance, Reference Lee, Harkness, Sabbagh and Jacobson8–Reference Wang, Wang, Chen, Zhu and Wang11 whereas others found no conclusive evidence of this impairment. Reference Harkness, Sabbagh, Jacobson, Chowdrey and Chen12,Reference Kettle, O'Brien-Simpson and Allen13 This topic is further complicated by studies that suggest individuals with depression performed better on the RMET Reference Harkness, Sabbagh, Jacobson, Chowdrey and Chen12 and were more sensitive to negative social information than their healthy counterparts. Reference Wolkenstein, Schonenberg, Schirm and Hautzinger14
The mental state decoding performance in participants with borderline personality disorder has also produced contradictory results. One study reported patients with borderline personality disorder had impaired social interpretation relative to healthy controls according to RMET, but people with borderline personality disorder with co-occurring major depression were significantly more accurate in decoding mental states of negative stimuli. The same study indicated patients with both borderline personality disorder and major depression performed significantly better than patients with only borderline personality disorder on negative and neutral items as well as total score. Reference Fertuck, Jekal, Song, Wyman, Morris and Wilson15 Comorbid depression was shown to increase RMET accuracy Reference Fertuck, Jekal, Song, Wyman, Morris and Wilson15,Reference Unoka, Fogd, Seres, Keri and Csukly16 perpetuating the idea that depression in borderline personality disorder intensifies vigilance towards social information similarly to depression. Reference Harkness, Sabbagh, Jacobson, Chowdrey and Chen12,Reference Wolkenstein, Schonenberg, Schirm and Hautzinger14 No systematic review or meta-analysis assessing RMET performance in depression and borderline personality disorder, moderating effects of co-occurring depression, or other first and second axis disorders have been published. Consequently, a meta-analysis reviewing mental state decoding ability in people with major depression and borderline personality disorder is of the highest clinical and conceptual relevance. In the current study, a quantitative meta-analysis of the RMET performance of adults clinically diagnosed with borderline personality disorder and major depression was conducted. RMET performance was analysed using total score and negative, neutral and positive valences. Further, the impact of potential moderators such as demographic and clinical variables that affect the patient and healthy control groups were considered. Since comorbidity is a large factor in clinical outcomes, we also assessed comorbidity with borderline personality disorder as a determinant of RMET performance.
Method
Literature search strategy
Relevant articles were identified through a computerised literature search using PubMed, PsycINFO and MEDLINE Web of Science databases. Search terms included: “Reading in the Mind of the Eyes Test”, “Borderline Personality Disorder”, “Major Depression”, “Unipolar Depressive Disorder”, “Theory of Mind” and “Mental State Decoding”. The search was limited to articles that were published between 2000 and January 2014. Additionally, a manual review of each article was performed utilising cross-references from original articles and reviews. Eligible studies compared RMET performance in patients diagnosed with borderline personality disorder or major depression with healthy controls. The search yielded 31 studies that met the requirements. Studies to be included in the meta-analysis were reviewed by both authors and followed certain criteria: (a) they focused on RMET performance in adult patients with borderline personality disorder or adult patients with major depression compared with healthy controls, and (b) they provided data or statistical information that allowed for the calculation of an effect size.
Following inclusion criteria, 13 of 31 studies were included for meta-analysis. Reasons for exclusion of 18 studies included: (a) absence of control groups (n = 10), (b) control groups meeting clinical criteria for either bipolar disorder (n = 1) or oesophageal cancer (n = 1), (c) borderline personality disorder groups displaying characteristics of the disorder, but no clinical diagnosis (n = 1), (d) lack of statistical information for calculating effect size (n = 4) and (e) clinical groups of patients with a mean age under 18 (n = 1).
Only 7 of the 13 studies included reported RMET valence scores. Authors that did not report the relevant information were contacted, but either did not have the required information or failed to respond. One study provided valence scores for patients, but not for controls. Therefore, we performed two analyses: one on accuracy (n = 13) and one on valence scores (n = 7).
Moderator variables
Within the patient population, the following moderator variables were also coded: mean age at the time of testing; gender (i.e. percentage male); and comorbidity diagnosis. Symptom severity, additional demographic characteristics (ethnic background and education level) were considered, but ultimately were not reported enough in the studies.
For comorbidity diagnoses other than borderline personality disorder and major depression there were not enough data to examine meta-analyses differences on valence scores. Therefore, only analysis of RMET overall accuracy was undertaken for comorbidity of borderline personality disorder and any anxiety disorder, eating disorder, substance use disorder, and cluster A, B and C personality disorders. In the studies of patients with major depression, we sought to examine how comorbidity might affect this group; however, too few of the studies reported these data for us to use in our analysis. Thus, we only assessed how comorbidity influenced borderline personality disorder groups.
Statistical analyses
The meta-analysis was conducted with Comprehensive Meta-Analysis Version 2.0 software. Reference Borenstein, Hedges, Higgins and Rothstein17 Scores were standardised by calculating Cohen's d of studies comparing scores between patients with major depression or borderline personality disorder and healthy controls. Effect sizes were calculated based on the difference of two raw means divided by the pooled standard deviation and were classified as small (d = 0.2), medium (d = 0.5) or large (d≥0.8). Reference Cohen18 Cohen's d was calculated from reported means and standard deviations, univariate F-tests, t-statistics or P-values. Confidence intervals and Z-values of the effect sizes were used to assess statistical significance. The Cochran Q-statistic was used to examine homogeneity of the effect sizes across studies between clinical diagnoses of borderline personality disorder or major depression. Reference Hedges and Olkin19 When analysis of the Q-statistic revealed significant within-group heterogeneity, a random-effects model was used for the significance level. In addition to a visual funnel plot, methods for the evaluation of potential publication bias included those recommended by Begg & Mazumdar Reference Begg and Mazumdar20 and Egger et al. Reference Egger, Smith, Schneider and Minder21
When categorical domains exhibited significant heterogeneity, potential moderators were considered with the Q-statistic. The effects of demographic moderator variables such as age (for example mean age) and gender (such as percentage male) were analysed with meta-regression. Additional analysis comprised of comparison of studies by comorbidity.
Results
Overall RMET accuracy meta-analysis results
Analysis of effect sizes across differences in performance on patients with borderline personality disorder and patients with major depression revealed a moderate overall effect size (n = 13, d = −0.621, 95% CI −0.844<δ<−0.399) that was significantly heterogeneous (Q B(68.82) = 82.56, P<0.001) (Fig. 1). Given that the variability in effect sizes between patient and healthy comparison groups differed more than sampling error alone, analysis of the moderator variables was conducted.

Fig. 1 Overall meta-analysis accuracy scores for the Reading in the Mind of the Eyes Test.
Significance displayed in P-value scores. BPD, borderline personality disorder; MD, major depression.
Publication bias
There was no evidence of any publication bias possibility as indicated by non-significant Begg & Mazumdar rank correlation (P = 0.35) and Egger (P = 0.31) tests. Nevertheless, calculation of a fail-safe N revealed that a total of 112 ‘null’ studies would be needed to reduce the observed effect to 0.20. Thus, our meta-analyses are an accurate representation of the current literature on RMET performance in these populations.
Overall RMET valence scores
Analysis of effect sizes across differences in valence performance in patients with major depression and patients with borderline personality disorder revealed a moderate overall effect size (n = 21, d = −0.075, 95% CI −0.291<δ<0.056) that was significantly heterogeneous (Q B(71.43) = 74.49, P<0.001). Given that the variability in effect sizes between patient and healthy comparison groups differed more than from sampling error alone, analysis of the moderator variables was conducted.
Publication bias
Analysis for possible response bias revealed an asymmetric funnel plot and significant Begg (P = 0.001, 1-tailed) and Egger (P = 0.001, 1-tailed) tests, suggesting a potential publication bias in this literature. To address this, we calculated a fail-safe N, which revealed that 890 ‘null’ studies would need to be found and incorporated in the analysis to negate the presented effect. As such, the current data are felt to accurately represent the extant literature on RMET valence scores.
Moderator analysis
Borderline personality disorder v. major depression on overall accuracy
Moderator analysis comparing patients with borderline personality disorder with patients with major depression was significantly heterogeneous (Q B(12) = 44.437, P<0.001). Large effect sizes were seen in performance for patients with major depression (d = −0.751, 95% CI −0.991<δ<−0.511). The results for patients with borderline personality disorder were not significant (P = 0.51). Figure 2 visually depicts these results.
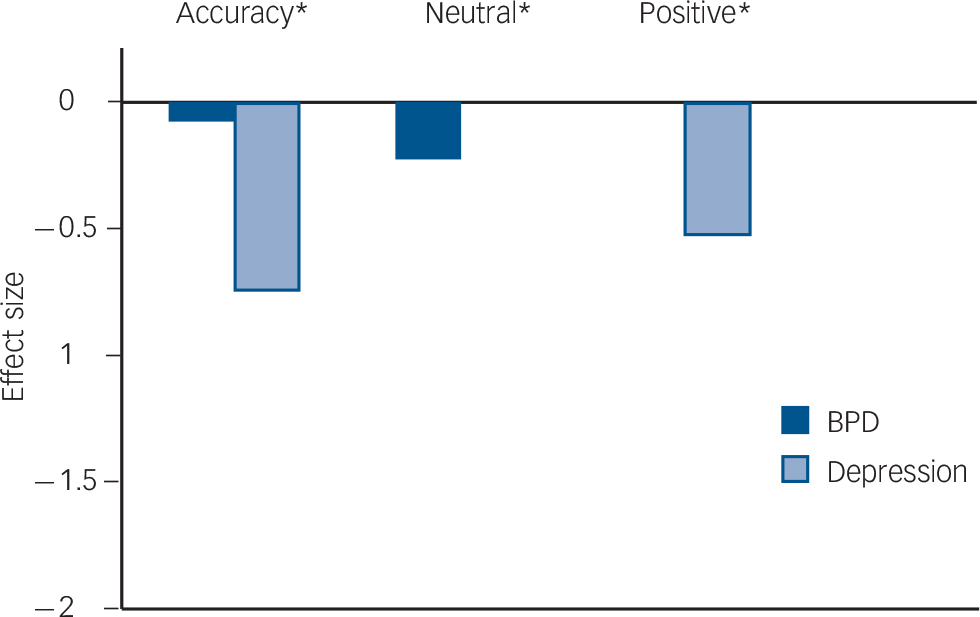
Fig. 2 Effect sizes for scores on the Reading in the Mind of the Eyes Test.
The borderline personality disorder (BPD) sample was worse than healthy controls on accuracy and neutral valence. The depression sample was worse than healthy controls on accuracy and positive valence. All negative valence scores were not statistically significant.
*Statistically significant at the 0.001 level.
Borderline personality disorder v. major depression on valence scores
For overall valence, patients with major depression (n = 21, d = −0.272, 95% CI −0.479<δ<−0.66) were significantly worse than those with borderline personality disorder and healthy controls. Both patients with major depression (Q B(18.86) = 73.50, P<0.001) and those with borderline personality disorder (Q B (47.83) = 70.76, P<0.001) showed significant heterogeneity for valence type. When comparing valence type, patients with major depression were significantly impaired on positive valence (d = −0.523, 95% CI −0.881<δ<−0.165). Conversely, patients with borderline personality disorder were significantly impaired on neutral valence (d = −0.230, 95% CI −0.460<δ<−0.001). Figure 2 visually depicts these results (see also Figs 3 and 4).
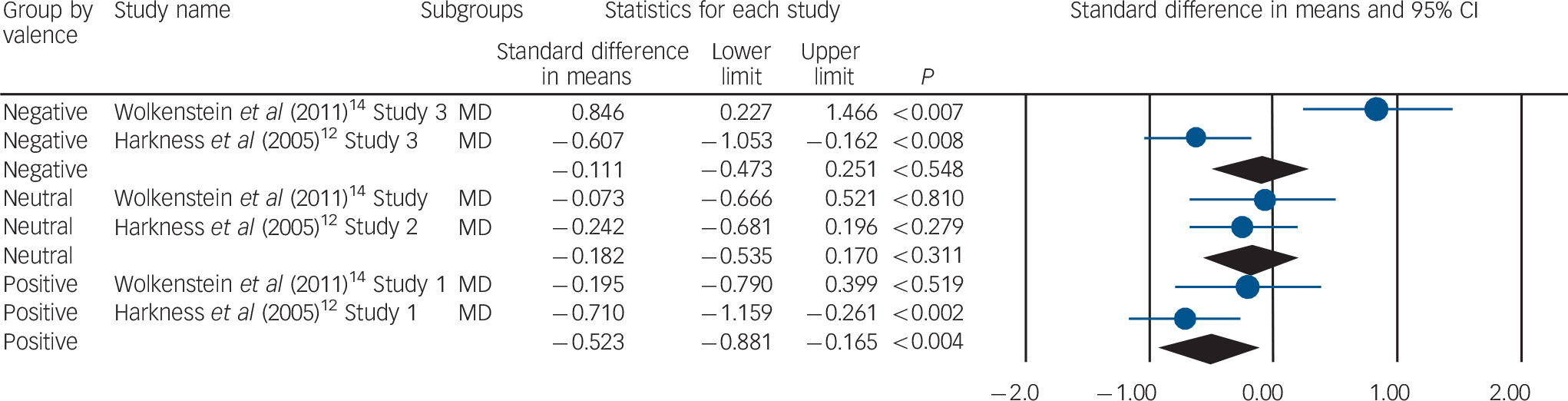
Fig. 3 Reading in the Mind of the Eyes Test meta-analysis valence scores in patients with major depression.
Significance displayed in P-value scores. MD, major depression.

Fig. 4 Reading in the Mind of the Eyes Test meta-analysis valence scores in patients with borderline personality disorder.
Significance displayed in P-value scores. BPD, borderline personality disorder.
Borderline personality disorder with major depression
Overall accuracy. Comorbidity of borderline personality disorder and major depression significantly affected the overall accuracy on the RMET (n = 5, Z = 3.45, P<0.0005). Patients with borderline personality disorder and major depression performed better than those with borderline personality disorder alone.
Positive valence scores. Those with borderline personality disorder and major depression performed better on the positive valence tasks of the RMET than patients with regular borderline personality disorder (Z = 2.79, P<0.005) (Fig. 5).
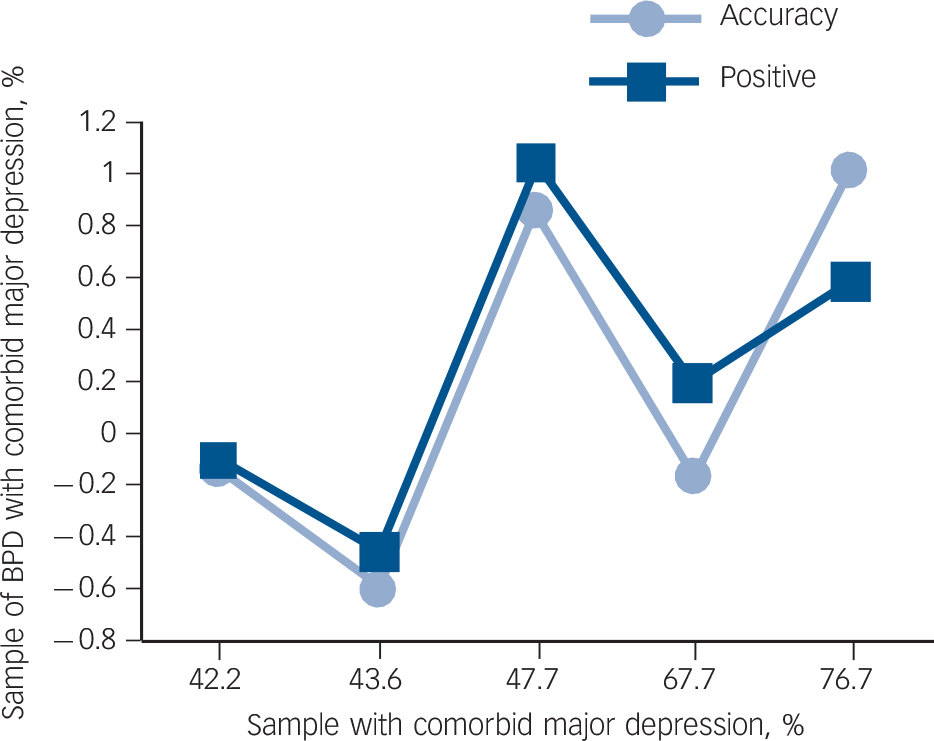
Fig. 5 Effects of comorbid depression on global accuracy and positive valence scores on the Reading in the Mind of the Eyes Test.
Borderline personality disorder (BPD) samples with a higher percent comorbid major depression performed significantly better than samples with a lower percent comorbid major depression.
Borderline personality disorder and other disorders
Any anxiety disorder. The relationship between comorbidity of borderline personality disorder and any anxiety disorder on overall RMET performance observed was not significant (n = 5, Z = 0.336, P = 0.75). The relationship between comorbidity of borderline personality disorder and any anxiety disorder for RMET valence was not significant (n = 15, Z = 0.56, P = 0.86).
Any eating disorder. The relationship between comorbidity of borderline personality disorder and any eating disorder in relation to performance on the RMET test was observed to be significant (n = 5 effects, Z = 1.13, P<0.005). Patients with a dual diagnosis of borderline personality disorder and any eating disorder performed better on the test than those with borderline personality disorder without any eating disorder. Valence showed no differences between comorbid borderline personality disorder and eating disorder (N = 15 effects; Z = 0.18, P = 0.93).
Any substance use disorder history. The relationship between comorbidity of borderline personality disorder and any substance use disorder history was not observed to be significant. (n = 5, Z = 0.486, P = 0.67). Valence results were not significant (n = 15, Z = 0.57, P = 0.83).
Any cluster A personality disorder. The relationship between comorbidity of borderline personality disorder and any cluster A personality disorder performance on the RMET was observed to be not significant (n = 4, Z = −2.28, P = 0.63). Valence scores were also not significant (n = 2, Z = −3.38, P = 0.83).
Any cluster B personality disorder. The relationship between comorbidity of borderline personality disorder and any cluster B personality disorder performance on the RMET was observed to be significant (n = 4, Z = −3.17, P<0.001). Patients with a dual diagnosis of borderline personality disorder and any cluster B personality disorder performed worse on the test than those with a borderline personality disorder without a cluster B personality disorder. This patient group also performed worse than healthy controls. Valence scores were not significant (n = 12, Z = −0.68, P = 0.32).
Any cluster C personality disorder. The relationship between a comorbidity of borderline personality disorder and any cluster C personality disorder performance on the RMET was observed to be significant (n = 4, Z = −3.01, P<0.001). Patients with a dual diagnosis of borderline personality disorder and any cluster C personality disorder performed worse on the test than those with borderline personality disorder without a cluster C personality disorder. This patient group also performed worse than healthy controls. Valence scores were not significant (n = 12, Z = −0.89, P = 0.12).
Demographic characteristics
Analysis of age composition among the samples reporting mean age revealed no significant differences for borderline personality disorder and major depression for accuracy (n = 11, Z = −0.26, P = 0.53). Analysis of gender composition of the samples reporting gender revealed that there were no significant differences for borderline personality disorder and major depression for accuracy (n = 9, Z = −1.81, P = 0.6).
Discussion
Main findings
The meta-analysis conducted extends the current literature on the RMET performance of patients with borderline personality disorder and patients with major depression. This meta-analysis was performed relative to healthy comparison controls and reviewed potential moderator variables that may influence RMET performance. To our knowledge this is the first meta-analysis to assess RMET performance differences among these patient populations. In addition, studies assessing either patients with borderline personality disorder or major depression have been limited by small sample size. Our study extends prior findings to a large sample for accuracy (n = 935) and an even larger one for valence (n = 1525).
Our meta-analysis results from 13 studies revealed a large overall effect size for global RMET accuracy performance. These results revealed patients with major depression and borderline personality disorder performed significantly worse than healthy controls. In addition, the overall effect was heterogeneous with differences in performance between patients with borderline personality disorder and those with major depression. Our moderator analysis revealed patients with major depression performed worse than those with borderline personality disorder. Literature has emphasised that patients with borderline personality disorder have vast impairments in mentalisation, Reference Fonagy and Luyten7 however our meta-analysis may elaborate on decreased mentalisation abilities in patients with major depression. Reference Harkness, Sabbagh, Jacobson, Chowdrey and Chen12,Reference Wolkenstein, Schonenberg, Schirm and Hautzinger14
In addition to accuracy, we assessed valence outcomes among patient groups. Only few studies reported included valence, but we were able to extract valence scores (n = 21) and examine within-patient valence differences. Overall valence scores showed significant differences, which allowed calculation of within-group valence analysis.
Major depression
The positive valence deficit in major depression indicates impairment in the processing of positive facial emotional cues. These findings are in line with previous studies of major depression and the processing of facial expressions with positive valence. Patients with major depression relative to healthy controls show reduced accuracy of processing happy facial expressions, reduced attention towards positive facial expressions, Reference Suslow, Junghanns and Arolt22 selective attention away from happy faces Reference Surguladze, Brammer, Keedwell, Giampietro, Young and Travis23 and a tendency to evaluate neutral and ambiguous expressions as less happy. Reference Donegan, Sanislow, Blumberg, Fulbright, Lacadie and Skudlarski24 Our results provide partial support for the hypothesis of a mood congruent impairment of mental state decoding in major depression, specifically that low positive affectivity and anhedonia is related to impaired ability to decode rewarding positive facial expressions. The neural basis of this social reward processing deficit may be related to the decreased activity in bilateral fusiform gyri and ventral striatum (right putamen) in response to happy faces. Reference Surguladze, Brammer, Keedwell, Giampietro, Young and Travis23 Further, these positive valence decoding impairments could affect interpersonal perception and could contribute to low self-esteem, social isolation and impairment.
Contrary to some previous findings Reference Harkness, Sabbagh, Jacobson, Chowdrey and Chen12,Reference Wolkenstein, Schonenberg, Schirm and Hautzinger14–Reference Unoka, Fogd, Seres, Keri and Csukly16 and negativity bias theory of depression in our meta-analysis we did not find more accurate decoding ability of facial expressions with negative valence. These results show that patients with major depression are not homogeneous regarding selective attention to negative emotional stimuli (negativity bias), and related higher accuracy in decoding negative facial expression. Further, RMET studies on major depression should report symptom profile and severity indexes to make possible the identification of subgroups with more and subgroups with less accurate negative mental state decoding abilities.
Borderline personality disorder
We found that patients with borderline personality disorder were overall significantly impaired in decoding mental states with neutral valence (such as reflective). Our findings are consistent with those of a meta-analysis on facial emotion recognition in borderline personality disorder; Reference Daros, Zakzanis and Ruocco3 patients with borderline personality disorder misattribute emotions to faces depicting neutral expressions. This emotionalising tendency may be related to the largely consistent findings of amygdala hyperactivity during facial emotion processing. Reference Donegan, Sanislow, Blumberg, Fulbright, Lacadie and Skudlarski24–Reference Minzenberg, Fan, New, Tang and Siever27 Further, this emotionalising tendency of affectively neutral expressions in borderline personality disorder can contribute to misunderstandings in social interactions, i.e. patients with borderline personality disorder may interpret neutral expressions as a threat. Reference Domes, Heinrichs, Rimmele, Reichwald and Hautzinger28
Findings relating to comorbidity
Our results showed that patients with borderline personality disorder and major depression comorbidity performed better on RMET accuracy and positive valence tasks than those with borderline personality disorder or major depression alone. As such, our findings represent a new informative clinical profile for people with comorbid borderline personality disorder and major depression. That is, regarding mental state decoding ability, borderline personality disorder with comorbid major depression is different from both borderline personality disorder and major depression alone. The RMET positive valence findings are in line with a meta-analysis Reference Daros, Zakzanis and Ruocco3 in which investigated studies with facial emotion recognition ability in borderline personality disorder from emotional stimuli at 100% intensity. In that meta-analysis it was found that people with borderline personality disorder with major depression have more intact positive emotional facial expression recognition ability than those with major depression alone.
One implication of our finding is that more accurate mental state decoding of RMET total accuracy and positive valence scores may represent an important feature of borderline personality disorder with major depression that might be useful for distinguishing between patients with both borderline personality disorder and with major depression from those with borderline personality disorder or major depression alone. It is important to note that comorbid major depression may reflect the depressive symptoms of borderline personality disorder at a more severe stage of their clinical trajectory and may not describe major depression as a distinct comorbid diagnostic entity. These results may point to the inability of structured diagnostic interviews based on the DSM-IV 29 system to differentiate between a major depressive episode and depressive symptoms of borderline personality disorder.
Patients with personality disorder and co-occurring eating disorder performed better on the test than those with borderline personality disorder without an eating disorder. We collapsed eating disorders into one group because most of the analysed studies reported them that way. Most of the previous studies found intact RMET performance in bulimia nervosa and RMET impairment in anorexia nervosa, Reference Russell, Schmidt, Doherty, Young and Tchanturia30,Reference Harrison, Sullivan, Tchanturia and Treasure31 with the exception of some other studies that found that RMET performance of those with anorexia nervosa was similar to that of healthy controls, Reference Kenyon, Samarawickrema, Dejong, Van den Eynde, Startup and Lavender32,Reference Adenzato, Todisco and Ardito33 and one where all subtypes of eating disorder were studied and found deficits only in bulimia nervosa and eating disorders not otherwise specified. Reference Medina-Pradas, Navarro, Lopez, Grau and Obiols34 Although in previous studies there were contrasting findings on RMET performance in different subgroups of eating disorder, our results revealed a subgroup of patients with borderline personality disorder and comorbid eating disorder with a relatively good RMET performance.
Our other important finding is that patients with borderline personality disorder who met DSM-IV criteria for any cluster B or any cluster C personality disorder performed worse on the RMET than those with borderline personality disorder but without this comorbidity. The comorbidity of these disorders with borderline personality disorder is considerable. Reference McGlashan, Grilo, Skodol, Gunderson, Shea and Morey35,Reference Grant, Chou, Goldstein, Huang, Stinson and Saha36 There are relatively few studies about RMET performance in people with personality disorder from these two clusters. Reference Richell, Mitchell, Newman, Leonard, Baron-Cohen and Blair37–Reference Schilling, Wingenfeld, Lowe, Moritz, Terfehr and Kother39 Our results point to potential mental state decoding impairment in these personality disorders, but we cannot exclude that the co-occurring symptoms of other personality disorder may reflect the severity of borderline personality disorder or dysfunctioning of personality in general and not the presence of distinct diagnostic entities. Future research should carefully consider the contributions of comorbid cluster B and C personality disorders to RMET performance in borderline personality disorder.
Limitations
The current study is characterised by some limitations. First, our analysis contained only studies that included a healthy comparison group. Further, studies were excluded if patients had mental health disorders not relevant to our study. Although this allowed for comparisons of the effect sizes between patient- and age-matched healthy comparison groups, it omitted studies that relied on normative data to calculate patients' RMET performance. Studies were also excluded if patients exhibited borderline personality disorder characteristics but were not diagnosed directly with borderline personality disorder. Meta-analyses were carefully conducted to prevent complications with the calculation of effect sizes on contrasting populations of controls, patients and with different clinical diagnoses. Moderator variable examination was limited as few studies reported education level and ethnicity. Also, the analysis was limited to cross-sectional studies only. Our analysis of the moderator effects of comorbidity may reflect symptom severity rather than the effects of multiple morbidities. Finally, our results are limited by the small number of studies for accuracy (n = 13) and for valence (n = 21). Both samples had little information on comorbidity, limiting our analysis.
Funding
The present publication was prepared within the framework of the TáMOP-4.2.2.C-11/1/KONV-2012-0008 (Social Renewal Operative Program) project titled ‘The application of ICT in learning and knowledge acquisition: Research and Training Program Development in Human Performance Technology’. The project was supported by the European Union and the co-financing of the European Social Fund.
Acknowledgements
The authors would like to acknowledge Dr Michael Borenstein, PhD, for his assistance in responding to meta-analysis-related questions.








eLetters
No eLetters have been published for this article.